Microbiology Exam 5: Lesson 17-19
1/109
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
110 Terms
What is the outermost layer of the skin called?
Stratum corneum (keratinized outer layer)
How does the skin physically defend against pathogens and the ways pathogens can invade it?
Constant shedding of dead cells removes microbes; keratin provides a tough barrier.
Pathogens can invade through cuts, hair follicles, sweat glands, or breaks in the skin.
What are the main chemical defenses of the skin?
Antimicrobial peptides, sebum (low pH make skin inhospitable, toxic byproducts of fatty acid metabolism inhibit the growth of microorganisms ), sweat (acidic, salty), and lysozyme (breaks down peptidoglycan found in bacterial cell walls).
Also the skin’s natural microbial community that inhibits colonization by pathogens through competition.
Define Exanthem.
A skin rash arising from another focus of infection.
Define Enanthem.
A mucous membrane rash arising from another focus of infection.
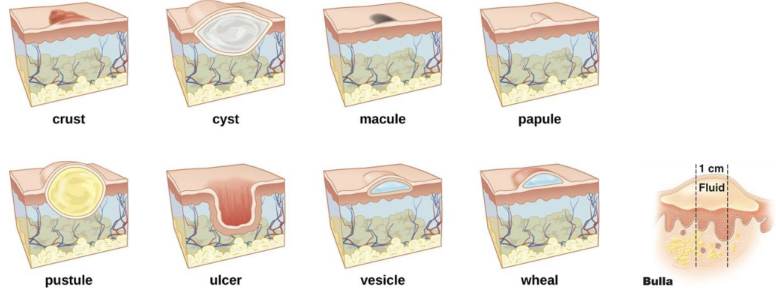
Types of skin lesions
Crust (dried exudate)
Cyst (enclosed sac)
Macule (flat discoloration)
Papule (raised bump)
Pustule (pus-filled lesion)
Ulcer (open sore)
Vesicle (fluid-filled blister)
Wheal (raised area from edema)
Bulla (large blister >1cm)
What are the main structures of the eye?
Sclera, cornea, iris, pupil, eyelid, conjunctiva, lacrimal apparatus.
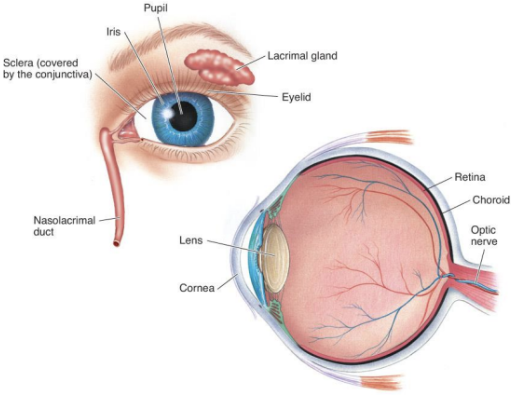
What are the eye’s main defense mechanisms?
Tears (contain lysozyme), blinking, and constant flushing action.
Define Conjunctivitis.
Inflammation of the conjunctiva (“pink eye”).

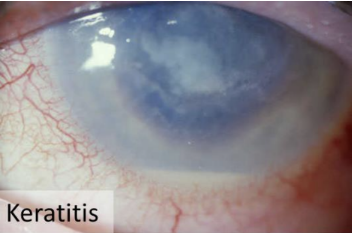
Define Keratitis.
Inflammation of the cornea.; may lead to blindless
Define Blepharitis.
Inflammation of the eyelid.
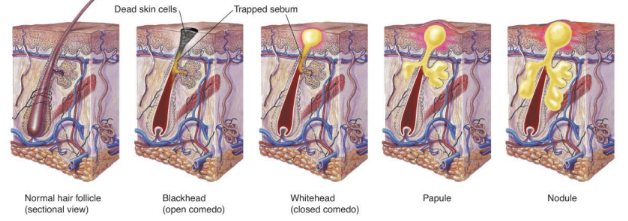
ACNE
Acne is the most common skin disease in the world
Chronic inflammatory condition involving
Propionibacterium acnes
Staphylococcus vs Streptococcus
Staphylococcus: Clusters, catalase-positive.
Streptococcus: Chains, catalase-negative.
What diagnostic tests are used to differentiate Staphylococcus vs Streptococcus
Catalase test: Staph = +, Strep = –.
Coagulase test: S. aureus = +, S. epidermidis = –.
Mannitol salt agar: S. aureus ferments mannitol (turns yellow). and no color change with S. epidermidis
Blood agar hemolysis: Alpha ( bacteria partially lyse red blood cells, Released hemoglobin converted to methemoglobin, Greenish-brown zone), Beta ( completely lyse red blood cells, released hemoglobin is destroyed, clear zone around the bacterial colonies), Gamma (No hemolysis, No visible change in the blood agar around the bacterial colonies) for Streptococci.
STAPHYLOCOCCI
Gram positive cocci
Staphylococcus epidermidis
Commonly found on the skin, mucous membranes, and respiratory tract.
can cause infections in immunocompromised individuals or when introduced into the body through medical devices
Staphylococcus aureus
Can be found in the nasal passages, skin, and gastrointestinal tract.
A more virulent pathogen that can cause a wide range of infections, including skin infections, pneumonia, sepsis, and food poisoning.
What is Folliculitis and a Sty?
Staphylococcus aureus infections
Folliculitis = infection of hair follicles. A sty is folliculitis of an eyelash.

What is a Furuncle and Carbuncle?
Staphylococcus aureus infections
Furuncle- A boil — a deep abscess filled with pus.
Carbuncle- A group of connected furuncles causing deeper inflammation.

Describe Impetigo (staphylococcal form).
Staphylococcus aureus infection
Bullous impetigo; Impetigo is a superficial bacterial infection that causes the skin to flake or peel large; a fluid-filled blisters caused by exfoliative toxin A. Common in newborns.

Describe Scalded Skin Syndrome
Staphylococcus aureus infection
Caused by exfoliative toxins A and B; skin peels off in sheets, mainly in newborns and infants.

Describe Toxic Shock Syndrome (TSS).
Staphylococcus aureus infection
Caused by toxic shock syndrome toxin-1 TSST-1 (superantigen); results in high fever, rash, low BP, multi-organ failure.
it is associated with tampon use surgical wounds and skin infections.

What is MRSA, and why is it clinically significant?
Methicillin-Resistant Staphylococcus aureus; resistant to β-lactam antibiotics, common in hospitals, causes hard-to-treat infections.
MRSA is especially troublesome in hospitals and nursing homes, where patients with open wounds, invasive devices, and weakened immune systems
Describe Impetigo (streptococcal form).
Streptococcus pyogenes Infection
Non-bullous form with honey-colored crusting; highly contagious spreads by contact (autoinoculation) ; common in older children and adults.

What is Erysipelas?
Streptococcus pyogenes Infection
Infection of upper dermis and superficial lymphatics; causes raised, well-demarcated red, swollen, painful area
Systemic symptoms: fever, chills

What is Necrotizing Fasciitis?
Streptococcus pyogenes Infection
Rapidly spreading “flesh-eating” infection of fascia caused by exotoxin A (superantigen); medical emergency. Has high mortality rate

What is Scarlet Fever?
Streptococcus pyogenes Infection
Complication of strep throat caused by erythrogenic toxin; causes sandpaper-like rash and strawberry tongue.
treated with penicillin or cephalexin

What are the key virulence factors of S. pyogenes?
M protein (prevents phagocytic), streptokinase (dissolves blood clots, aids spread), hyaluronidase (degrades connective tissue), streptolysins O and S (destroy red and white blood cells) , and erythrogenic toxin.
MACULOPAPULAR disease
Flat to slightly raised colored bumps
(measles (rubeola), Rubella (German Measles, Fifth Disease, Roseola, Scarlet Fever)
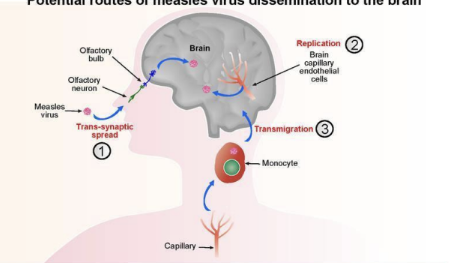
MEASLES (RUBEOLA)- Maculopapular rash disease
caused by Measles virus
Transmitted by respiratory route (droplets)
Starts on head → spreads to body; Macular rash and Koplik’s spots in mouth; high fever.
Prevented by MMR vaccination and supportive care

Rubella (German Measles) - Maculopapular rash disease
caused by Rubella virus
transmission by respiratory droplets
Symptoms- Maculopapular rash and fever
Congenital rubella syndrome is significant in pregnancy because it causes severe fetal damage
Prevented by vaccination and supportive care

Fifth Disease (Erythema Infectiosum) - Maculopapular rash disease
Produces a Mild Rash
caused by Parvoviridae, Parvovirus B19
transmitted by respiratory droplets
Symptoms include a fiery red (“slapped check”) rash on the cheeks and ears, and trunk. It disappears within a few days
Adults can experience symptoms similar to those of rheumatoid arthritis
treatment includes supportive care

Roseola - Maculopapular rash disease
Caused by Human herpesvirus 6 or 7.
Transmission of Roseolais most Likely respiratory route.
Symptoms of Roseola? High fever followed by rash; may resemble measles.
Treatment? Supportive care.
Scarlet Fever (rash type)- Maculopapular rash disease
caused by Streptococcus pyogenes (erythrogenic toxin).
Rash characteristics- Fine, red “sandpaper” rash and strawberry tongue.
Treatment- Penicillin or cephalexin.
Smallpox (Variola)- Vesicular Rash Disease
Variola virus (Poxvirus family).
Transmission? Respiratory droplets or contact with lesions.
Features of Smallpox rash include Deep, umbilicated pustules with thick yellow fluid; clustered on extremities.
Eradicated by vaccination (1980).

Chicken Pox and Shingles- Vesicular Rash Disease
Chickenpox caused by Varicella-zoster virus (VZV/HHV-3).
It is transmitted by respiratory droplets or direct contact. (highly contagious)
Clinical features include Vesicular rash, mostly on trunk; itchy; mild fever.
Prevention/Treatment- Live attenuated vaccine; antivirals if severe.
Shingles is caused by reactivation of latent VZV/ HHV-3
Features of Shingles rash include Painful vesicular rash along nerve pathways.
Prevention- Shingles vaccine (Shingrix) for adults 50+.
Treatment- Acyclovir or valacyclovir to shorten duration and reduce pain
Herpes Simplex (cold sores/fever blisters)- Vesicular Rash Disease
HSV-1 (primarily oral):
Infections: Cold sores/fever blisters (vesicles on lips), herpes gladiatorum (vesicles on skin), herpetic whitlow (fingers), herpes encephalitis
HSV-1 can remain latent in trigeminal nerve ganglia
Transmission: Direct contact, saliva
HSV-2 (primarily genital):
Infections: Genital herpes
Latency: Sacral nerve ganglia
Complications: Neonatal herpes (transmission during birth), herpes encephalitis
Transmission: Sexual contact, vertical transmission
Treatment: Acyclovir, valacyclovir, famciclovir (suppress replication, reduce symptoms, do not cure)
Viral latency
Latency: Virus remains dormant in host cells without active replication, but can reactivate later
Varicella-Zoster Virus (HHV-3):
Primary infection: Chickenpox (varicella)
Latency site: Dorsal root ganglia of spinal nerves
Reactivation: Shingles (herpes zoster) - typically in adults, immunocompromised, or elderly
Herpes Simplex Virus-1 (HSV-1):
Primary infection: Cold sores/fever blisters (oral herpes)
Latency site: Trigeminal nerve ganglia
Reactivation: Recurrent oral herpes lesions triggered by stress, UV exposure, illness
WARTS AND WART LIKE ERUPTIONS
Warts (Verrucae):
Causative agent: Human papillomaviruses (HPV) - over 100 types
Transmission: Direct contact, autoinoculation, indirect contact with contaminated surfaces
Types: Common warts, plantar warts, flat warts, genital warts
Treatment:
Cryotherapy, salicylic acid, imiquimod, or may resolve spontaneously.
Describe Molluscum contagiosum.
Caused by a poxvirus; spread by direct or sexual contact; causes smooth, firm, umbilicated lesions.
There is usually no treatment, mechanical removal can be performed (virus not eliminated)
Dermatomycoses (Tineas/Ringworm)
Causative agents: Dermatophytes (fungi that metabolize keratin)
Trichophyton, Microsporum, Epidermophyton species
Infect skin, hair, nails (wherever keratin is present)
Transmitted through direct contact with infected individuals, animals, or contaminated surfaces
Types by body location:
Tinea capitis: Scalp and hair
Tinea barbae: Beard area ("barber's itch")
Tinea corporis: Body/trunk ("ringworm") - circular, raised, red rings
Tinea cruris: Groin ("jock itch")
Tinea pedis: Feet ("athlete's foot") - blisters between toes
Tinea unguium (onychomycosis): Nails
Treatment: Topical or oral antifungals (azoles, terbinafine, griseofulvin)

CANDIDIASIS
caused by Candida albicans (yeast)
Occurs in skin and mucous membranes of genitourinary tract and mouth
Thrush: An infection of mucous membranes of mouth
Opportunistic. Predisposing factors:
Antibiotic use (suppresses normal bacterial flora)
Diabetes (elevated glucose)
Immunosuppression (HIV/AIDS, chemotherapy, corticosteroids)
Pregnancy (hormonal changes)
Moisture and occlusion
Topical treatment with miconazole or nystatin

PITYRIASIS VERSICOLOR
Endogenous skin infection that occurs in warm, humid climates
Caused by Malassezia species (lipophilic yeast)
Hypopigmented or hyperpigmented patches
Treated with antifungal creams or shampoos (Head and Shoulders with antifungal zinc pyrithione)
SPOROTRICHOSIS
Caused by Sporothrix schenckii (dimorphic fungus)
Subcutaneous nodules along lymphatic channels
"Rose gardener's disease" - from thorn pricks
SCABIES
caused by Sarcoptes scabiei
Transmitted through direct skin contact, contaminated bedding/clothing
symptoms:
Burrows in the skin to lay eggs
Linear burrow pattern is pathognomonic (highly characteristic of a disease)
Intense itching (worse at night)
Treatment with topical insecticide (permethrin, lindane)
PEDICULOSIS (LICE)
Caused by Pediculus humanus
Transmitted through direct contact, sharing of personal items
Symptoms:
Itching, visible lice or nits (eggs) on hair shafts
Types
P. h. capitis (head louse)
P. h. corporis (body louse)
P. h. pubis (“crabs”)
Treatment with topical insecticides (permethrin, malathion), nit removal
LEISHMANIASIS
caused by Leishmania species (protozoan)
Spread by the bite of infected sandfly
• Cutaneous form: skin ulcers/lesions at bite site
Treated with antimonial drugs, amphotericin B
Describe Trachoma.
Chronic eye infection caused by Chlamydia trachomatis; transmitted by direct contact or flies; causes scarring and blindness.
Leading infectious cause of blindness worldwide.
Treatment: Azithromycin, tetracycline
What parasitic infections affect the eyes?
Onchocerciasis (River blindness): Onchocerca volvulus (nematode/roundworm) spread via blackfly.
Acanthamoeba keratitis: From contaminated water/contact lenses.
Loiasis: Loa loa transmitted by deerfly; worms migrate under conjunctiva.
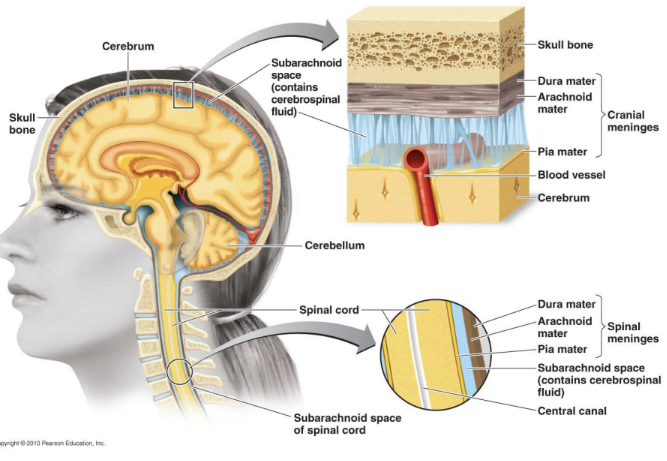
What is the Central Nervous System (CNS) and the three layers of the meninges that protect?
The CNS consists of the brain and spinal cord, responsible for processing and integrating information.
Dura mater – tough outer layer
Arachnoid mater – middle layer with CSF in subarachnoid space
Pia mater – delicate inner layer adhering to brain tissue
What is the blood-brain barrier (BBB) and its function?
Separation of circulating blood and the brain extracellular fluid (BECF) in the central nervous system (CNS)
Function: Protects brain from pathogens and toxins in bloodstream
Structure: Tight junctions between blood vessel cells act as selective filter
Clinical Problem:
Limits immune cell access
Limits antibiotic penetration
Once pathogens cross BBB → difficult to treat
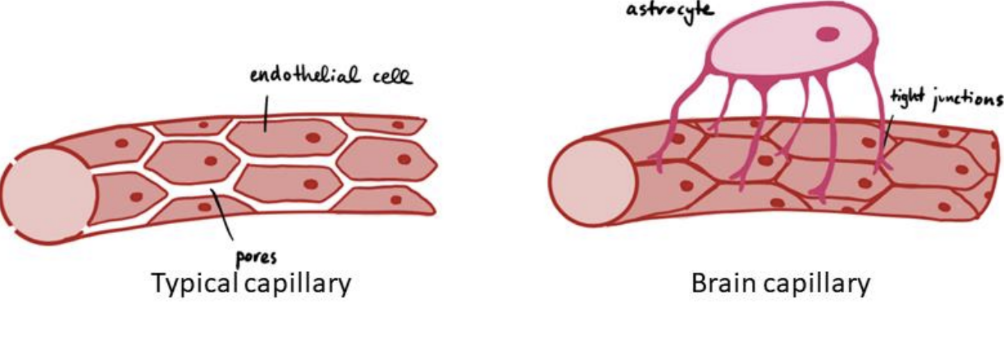
How can some bacteria like Borrelia and Treponema cross the BBB?
They are spirochetes with internal flagella that allow corkscrew-like movement through the barrier.

How does meningitis differ from encephalitis?
Meningitis: Inflammation of meninges.
Encephalitis: Inflammation of brain tissue.
What is meningoencephalitis?
Inflammation of both the meninges and the brain.
What are the three main bacterial species that cause meningitis?
Neisseria meningitidis (meningococcal meningitis)
Streptococcus pneumoniae (pneumococcal meningitis)
Haemophilus influenzae type b (Hib meningitis)
All 3 species can cross the blood-brain barrier, inflaming the meninges
All vaccine-preventable
How is bacterial meningitis transmitted and what are the characteristic symptoms?
Transmitted by droplet (respiratory secretions).
Symptoms include Fever, headache, stiff neck (classic triad)
, nausea, vomiting, altered mental state, and sometimes convulsions or coma.
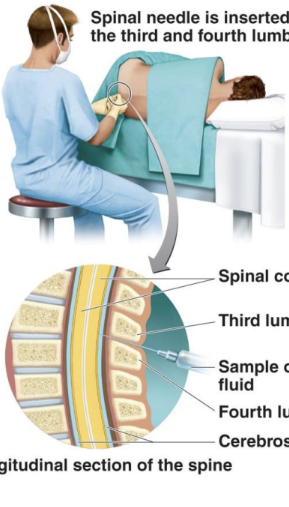
What body fluid is sampled to diagnose and what diagnostic methods are used to confirm bacterial meningitis?
Cerebrospinal fluid (CSF) obtained via lumbar puncture.
to confirm CSF analysis, Gram stain, latex agglutination test, culture. (CSF appears cloudy in bacterial infections) are used.
What rash is characteristic of Neisseria meningitidis (meningococcal meningitis) infection?
Petechial rash (purple/red skin spots from blood vessel invasion)

What is the causative agent of listeriosis and how is it transmitted?
caused by Listeria monocytogenes.
Transmitted through contaminated food — cold cuts, soft cheeses, unpasteurized milk, and fecal-contaminated foods.
Why is Listeria monocytogenes associated with refrigerated foods and who are at high risk for it?
It can grow at refrigerator temperatures (~4°C), unlike most foodborne pathogens.
Pregnant women (can cross placenta), elderly, and immunocompromised individuals.
What is the causative agent of tetanus and how is it acquired?
caused by Clostridium tetani.
acquired through deep puncture wounds contaminated with soil or feces ("Rusty nail" = deep wound + soil = anaerobic environment)
Tetanospasmin released from dead cells blocks
relaxation pathway in muscles
Muscles cannot relax, causing spastic paralysis (rigid, "lockjaw")
Muscle spasms so severe bones can break
Prevention by vaccination with tetanus toxoid ((DTaP, Tdap) and booster (dT)
Treatment with tetanus immune globulin

What is the causative agent of botulism?
Caused by Clostridium botulinum
Intoxication comes from ingesting botulinum toxin (Home-canned vegetables, garlic in oil, fermented fish, and honey (infants).
Botulinum toxin blocks release of neurotransmitter acetylcholine
Muscles cannot contract, causing flaccid paralysis (limp, droopy)
What are the three types of botulism?
Food-borne – ingestion of preformed toxin
Infant – toxin formed in intestines (floppy baby syndrome)
Wound – infection of wounds, often in IV drug users
What preventive measures help avoid botulism?
Proper canning (121°C), nitrites in sausages, avoiding honey in infants, and not eating from swollen cans.
tetanus vs botulinum toxin on muscles.
Tetanus toxin: Prevents relaxation → spastic paralysis.
Botulinum toxin: Prevents contraction → flaccid paralysis.
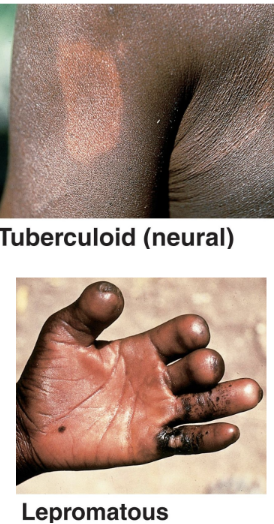
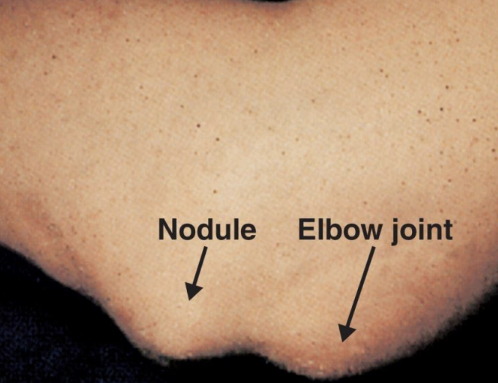
LEPROSY (HANSEN'S DISEASE)
Caused by Mycobacterium leprae
Acid-fast rod that grows best at 30°C
Core body temperature: 37°C (98.6°F)
Cooler body parts are affected (Fingers, toes, nose, ears, skin surface). This is WHY extremities are damaged
Grows in peripheral nerves and skin cells
Transmission requires prolonged contact with an infected person
Low infectivity (95% naturally immune)
Incubation: 3-5 years
What are the two forms of leprosy?
Tuberculoid (neural): Loss of sensation in skin areas
Strong immunity, few bacteria, localized lesions, nerve damage, better prognosis
Lepromatous (progressive): Disfiguring nodules over body
Weak immunity, many bacteria, disfiguring nodules (“Leonine facies”), worse prognosis.
How does viral meningitis compare to bacterial meningitis?
Aseptic meningitis is Milder, self-limiting (7–10 days), no bacteria in CSF (“aseptic”), caused by enteroviruses or herpesviruses.
Treatment: Supportive care only
Can viral encephalitis result from both primary and secondary infections?
Yes. Primary = virus directly invades CNS (HSV, arboviruses, rabies).
Secondary = reactivation or complication (measles → SSPE, human coronaviruses).
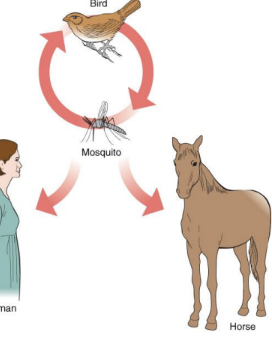
ARBOVIRAL ENCEPHALITIS
Caused by arthropod-borne viruses that belong to several families
transmitted by mosquito bites; mosquitoes transmit virus from infected birds to humans.
ex: West Nile virus, Eastern/Western equine encephalitis viruses.
-Fever, headache, confusion, seizures, paralysis, or coma.
Those who recover may have paralysis and mental disorders
No treatment or vaccine but can be prevented by Mosquito control, protective clothing, repellent
Poliomyelitis (Polio)
caused by Poliovirus
transmitted through Ingestion of contaminated water or food.
Initial symptoms: Sore throat and nausea
Virus enters CNS → destroys motor neurons
Flaccid paralysis (limbs, trunk)
Bulbar polio: Respiratory paralysis (can be fatal)
Prevention: vaccination (enhanced-inactivated form)
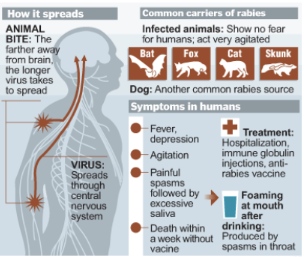
Rabies
Transmitted through bites from infected animals (bats, raccoons, foxes, skunks, coyotes).
Symptoms: (once CNS affected) Agitation, depression, hydrophobia,hallucinations; once symptoms appear, nearly 100% fatal.
post-exposure vaccination for rabies is possible it needs Long incubation period (up to 1 year) allows time for immune response before virus reaches brain.
Wound cleaning, rabies immune globulin (RIG), and 4-dose vaccine series over 14 days.
*must start before symptoms. after symptoms it is too late because the virus is in the CNS
PRION DISEASES
Misfolded proteins (no DNA or RNA). contain no nucleic acids and are resistant to normal sterilization.
EX:
Humans: Creutzfeldt-Jakob disease (CJD), Kuru
Animals: Mad cow disease, sheep scrapie
Symptoms: Rapid dementia, muscle weakness, ataxia, always fatal.
Primary Amoebic Meningoencephalitis (PAM)
caused by Naegleria fowleri.
acquired by Amoeba in warm freshwater (lakes, ponds, hot springs) enters via nose and travels up olfactory nerve.
outcome: Rapidly fatal (>97% mortality); causes destruction of brain tissue; death in 7–14 days.
prevented by Avoid submerging head in warm freshwater, use nose clips, maintain proper pool chlorination.
Which diseases are transmitted by droplets?
Bacterial meningitis, viral meningitis, some encephalitis cases.
Which diseases are transmitted by food?
Listeriosis, botulism, polio.
Which disease are transmitted by animal bites?
Rabies
Which disease are transmitted by mosquitoes?
Arboviral encephalitis (West Nile, Equine).
Which are transmitted by contaminated water?
Polio, Naegleria fowleri (PAM).
Which nervous system diseases can be prevented by vaccination?
Meningitis (Neisseria, Streptococcus pneumoniae, Hib)
Tetanus
Polio
Rabies (pre/post-exposure)
What are the basic components of the cardiovascular system?
The heart, blood vessels (arteries, veins, capillaries), and blood.
What are the basic components of the lymphatic system and function?
Lymph vessels, lymph nodes (fixed macrophages, B cells, and T cells) , spleen, thymus, tonsils.
Transporting lymph, filtering pathogens, and housing immune cells for defense.
What are the defenses of the cardiovascular and lymphatic systems?
5,000–10,000 WBCs per microliter of blood; lymphocytes for specific immunity and phagocytes for nonspecific defense.
Very few microbes can survive in the blood with so many defensive elements
What is the normal biota of the cardiovascular and lymphatic systems?
None—these systems are normally sterile.
Define bacteremia.
Presence of bacteria in the bloodstream.
Define viremia.
Presence of viruses in the bloodstream.
Define fungemia.
Presence of fungi in the bloodstream.
Define septicemia.
Persistent pathogens or toxins in the blood causing illness.
What is sepsis?
Systemic inflammatory response syndrome (SIRS) due to infection.
characterized by an elevated heart rate , high respiratory rate , abnormal white blood cell count and elevated or lowered body temperature, i.e. under 36 °C (97 °F) or over 38 °C (100 °F).
What is severe sepsis?
Sepsis with decreased blood pressure.
What is septic shock?
Sepsis with uncontrollable low blood pressure leading to organ failure.
What is lymphangitis?
Inflammation of lymph vessels associated with septicemia and septic shock.

What is endocarditis?
Inflammation of the inner lining of the heart (endocardium).
Fever, fatigue, joint pain, edema, weakness, anemia, and abnormal heartbeat.
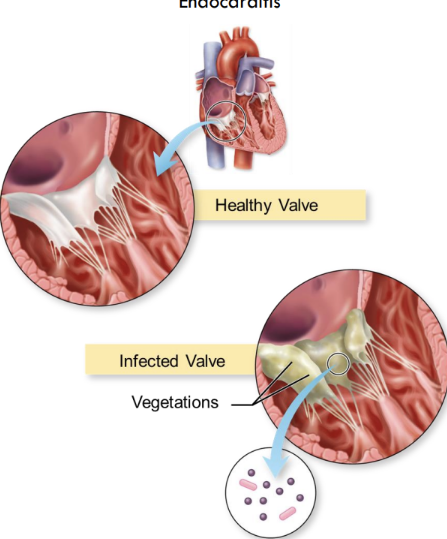
Acute Endocarditis
caused by Staphylococcus aureus (most common), Streptococcus pyogenes, S. pneumoniae, Neisseria gonorrhoeae.
transmitted through Parenteral entry (IV drug use, surgery, injury).
Subacute Endocarditis
Almost always preceded by some form of damage to the heart valves or by congenital malformation
caused by Low-pathogenicity bacteria such as Streptococcus mutans and Staphylococcus epidermidis.
Rheumatic Fever
caused by Streptococcus pyogenes.
Autoimmune complication of S. pyogenes infection causing inflammation of the heart valves, joints, and kidneys.
Puerperal Sepsis (childbed fever)
Infection of the reproductive tract following childbirth, leading to septicemia.
caused by Streptococcus pyogenes.
transmitted through contact with contaminated hands of healthcare workers during delivery.
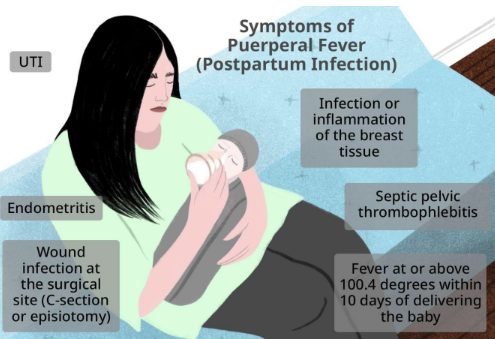
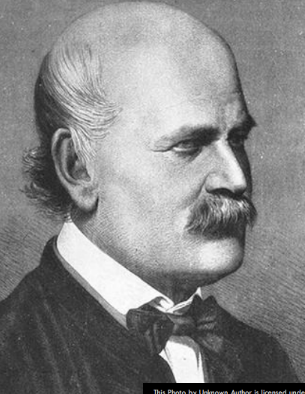
who and Why is Ignaz Semmelweis significant?
Ignaz Philipp Semmelweis (July 1, 1818 – August 13, 1865) was a Hungarian physician described as the "savior of mothers", who discovered by 1847 that the incidence of puerperal fever could be drastically cut by the use of hand disinfection
He introduced handwashing with chlorinated lime in 1847, drastically reducing maternal deaths from puerperal fever.
PLAGUE
Causative agent: Yersinia pestis, gram-negative rod
Reservoir: Rats, ground squirrels, and prairie dogs
Vector: Xenopsylla cheopis (rat flea)
TYPES/MANIFESTATIONS of plague
Bubonic: Bacterial growth in blood and lymph causing painful, swollen nodes called buboes.
Septicemic: Causes fever, chills, extreme weakness, shock, and bleeding into the skin and organs, which can turn skin and other tissues black
Pneumonic: Leads to rapidly developing pneumonia with symptoms like chest pain, shortness of breath, and coughing.
Most serious form and the only one directly spread from person to person through infectious droplet

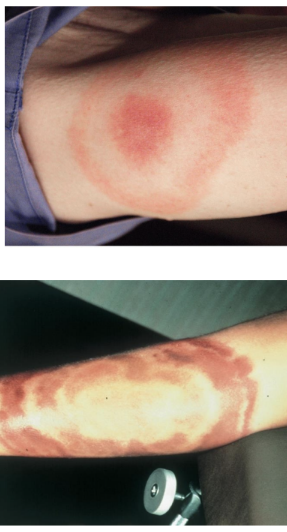
Lyme Disease
Causative agent: Borrelia burgdorferi
Reservoir: Deer, small mammals.
Vector: Ticks
First symptom: Bull's-eye rash
Second phase: Irregular heartbeat, encephalitis
Third phase: Arthritis
Lymphatic Filariasis
Caused by the parasitic roundworm Wuchereria bancrofti
Transmitted by mosquitoes
Larvae infect the lymphatic system
They damage vessels and glands
After years of infestation, arms, legs, and scrotum swell and distort, a.k.a. elephantiasis, lymphedem
