Topic 3 - Tissue Repair, Regeneration & Fibrosis
1/14
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
15 Terms

Acute tubular necrosis, oliguric phase
The cells of the brush border in the PCT are highly specialized, and have enormous resorptive capacity. When exposed to hypoxia, they rapidly become necrotic. The only cells in the body that are more sensitive to hypoxia are the cortical neurons of the central nervous system.
In this photomicrograph, note that the cells in the proximal tubules are destroyed (arrow), whereas the low cuboidal epithelial cells of distal tubules are preserved. When the proximal tubular cells are destroyed, the kidney shuts down, producing little urine, the so-called "oliguric" (little urine) phase of acute renal failure due to acute tubular necrosis. If the extracellular matrix (i.e., the basement membrane) of the tubule remains intact, the epithelial cells can regenerate.
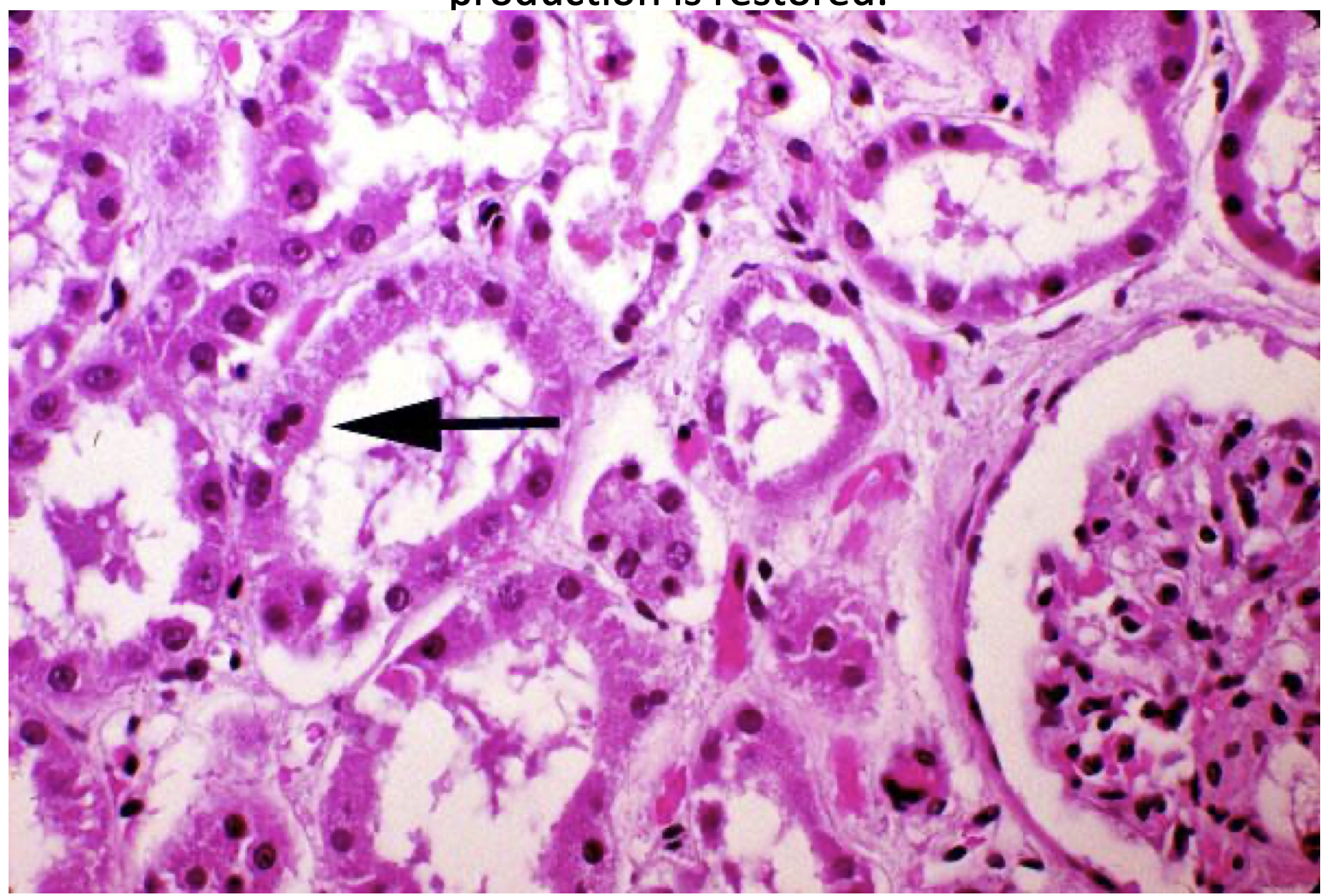
Acute tubular necrosis, regenerative (polyuric) phase
As the renal tubular epithelium regenerates, as the double nucleus (arrow) in this photomicrograph testifies to, the kidney begins to produce large amounts of very dilute urine. The is because the complicated brush border cells do not come back immediately, they are first replaced by low cuboidal epithelium, which does little in the way of resorption of water. Thus large quantities of dilute urine (polyuria) are produced by the patient. Eventually, the epithelium differentiates into the more complex brush border type, and normal urinary production is restored.
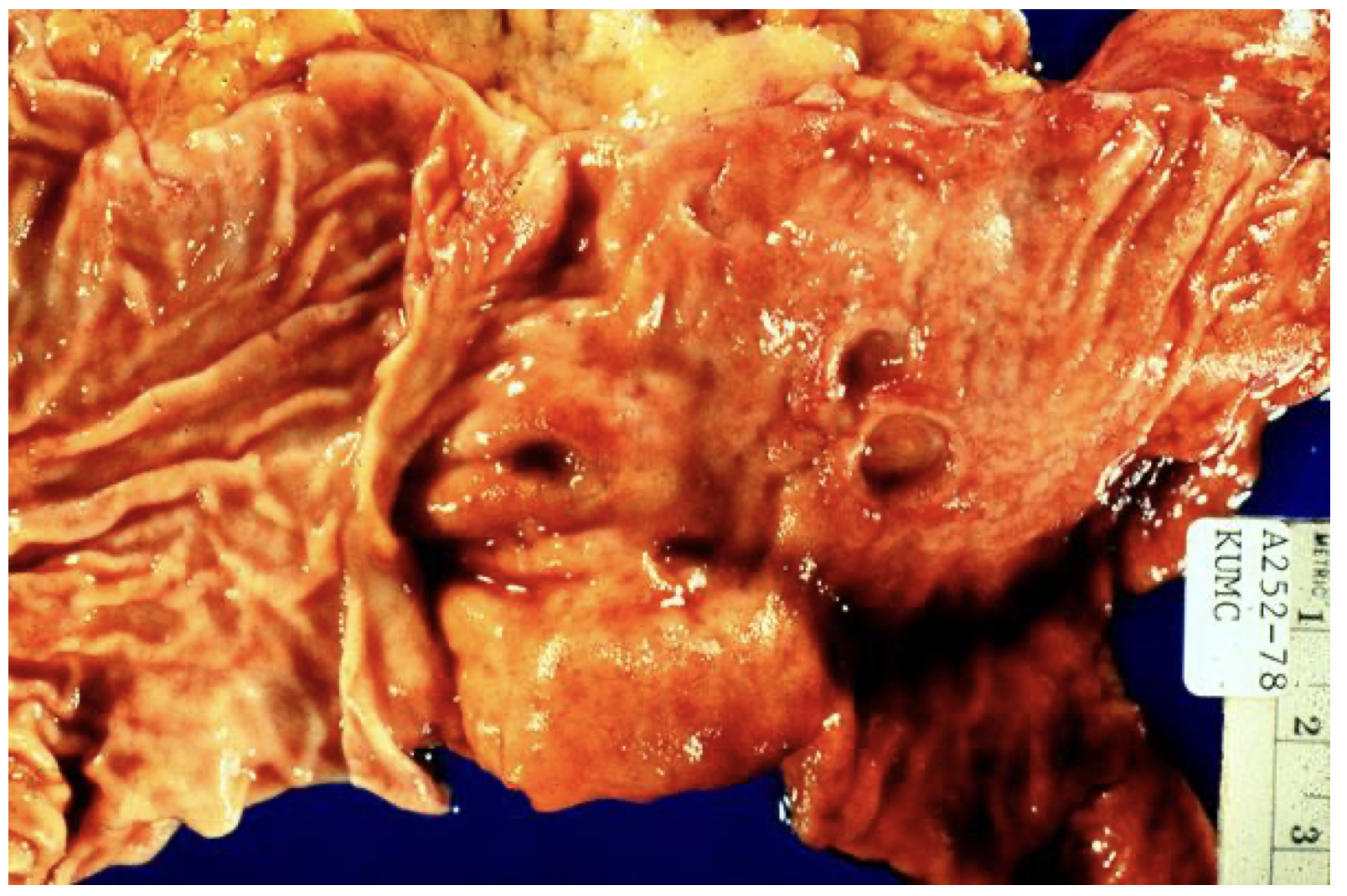
Duodenum, multiple peptic ulcers, gross
This gross photo was taken at the pylorus, with the stomach on the left and the duodenum on the right. Several ulcers are seen. If these become severe, they can perforate the bowel, and air could be seen under the diaphrams on an upright chest x-ray. This is a surgical emergency. The ulcers could also erode into the pancreas. The latest thinking is that ulcers may be infectious, caused by an organism called Helicobacter pylori.
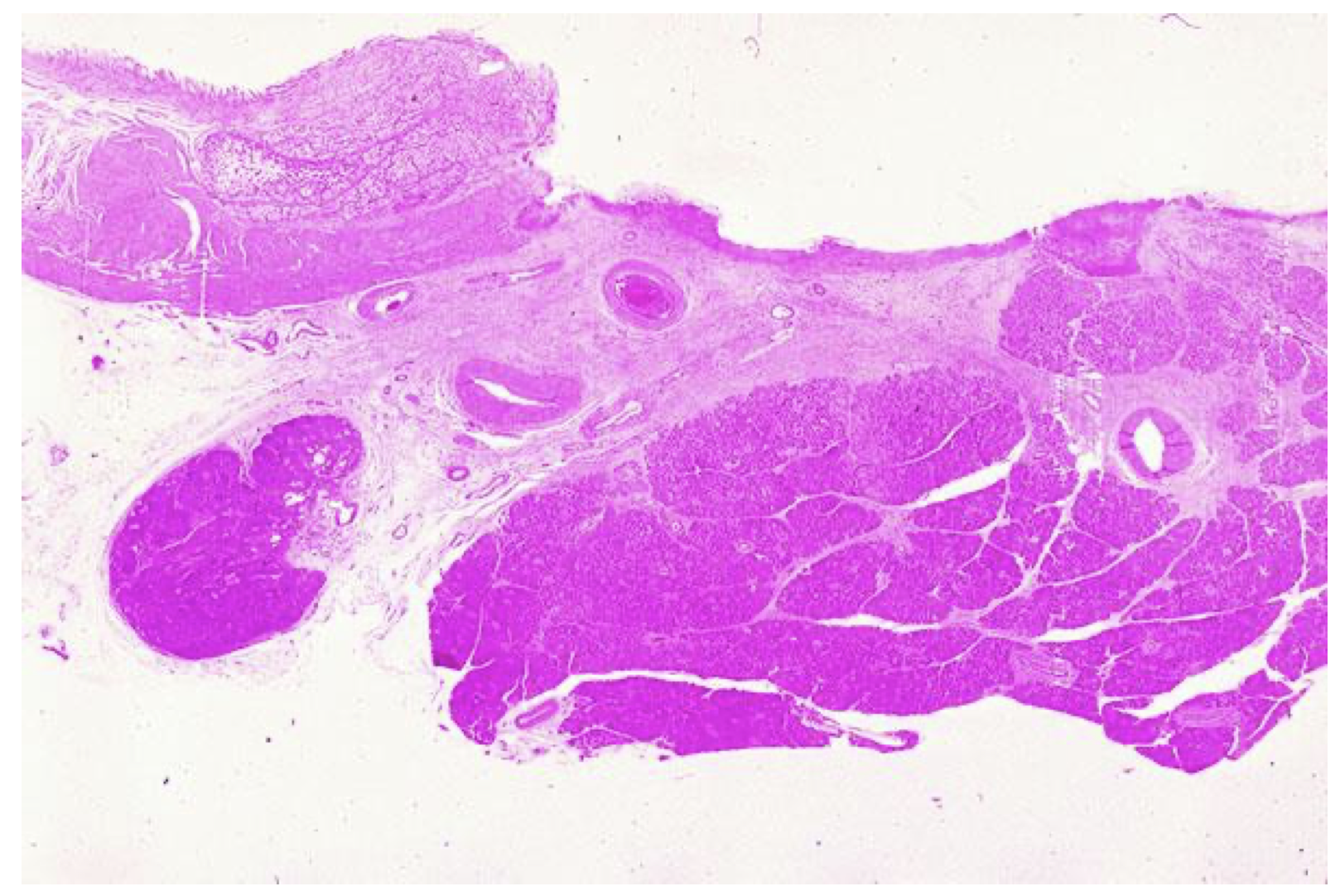
Duodenal ulcers, H/E microscopic slide, overview
normal epithelium on the left, which leads to a large ulcer. The ulcer can be seen to erode into the underlying pancreas. At the base of the ulcer, one would find RBCs, fibrin, and granulation tissue. A higher power view is available.
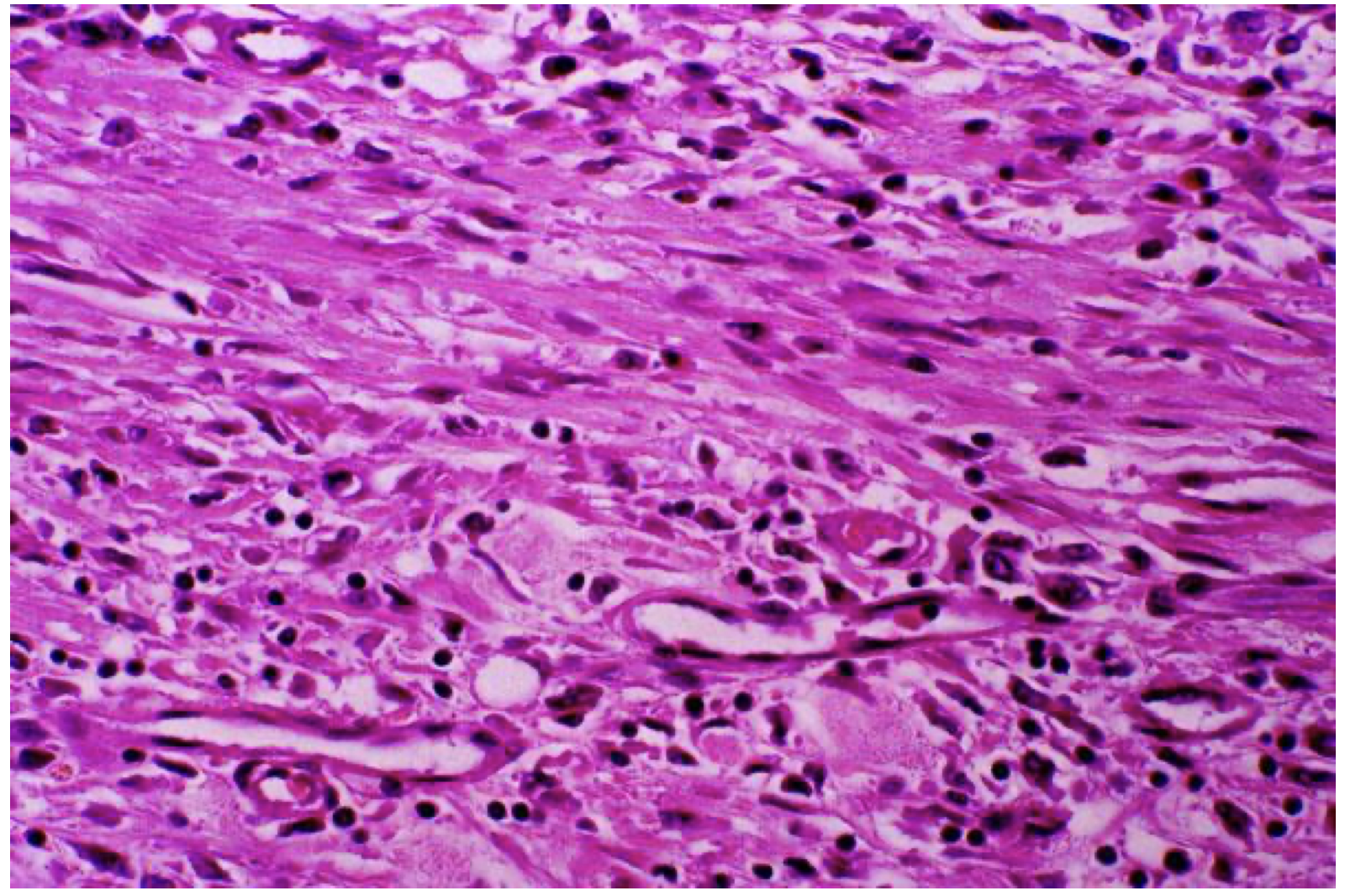
Granulation tissue, base of duodenal ulcer, H/E x 100
This photomicrograph shows the essence of granulation tissue: young, plump fibroblasts; collagen; chronic inflammatory cells; and angiogenesis, typified by young capillaries with swollen endothelial cells. If the chronic irritation is erradicated by treatment of the ulcer, the granulation tissue will slowly organize to form a mature scar, and the intestinal epithelium will regenerate over the top of it.

Keloid, photomicrograph, H/E, x25
A keloid is a hypertrophic scar, most common in those of African descent. Note that this section of skin shows melanin pigmentation in the basal layer, and exuberant collagen deposition. Large bands of collagen are seen deep in the dermis.

Ascites and umbilical hernia
This chronic alcoholic with cirrhosis developed portal hypertension. This increased pressure in the portal system is reflected by engorgment of abdominal veins, ascites (fluid in the peritoneal cavity), and umbilical herniation. Occasionally, fluid may also dissect into the scrotal sac.
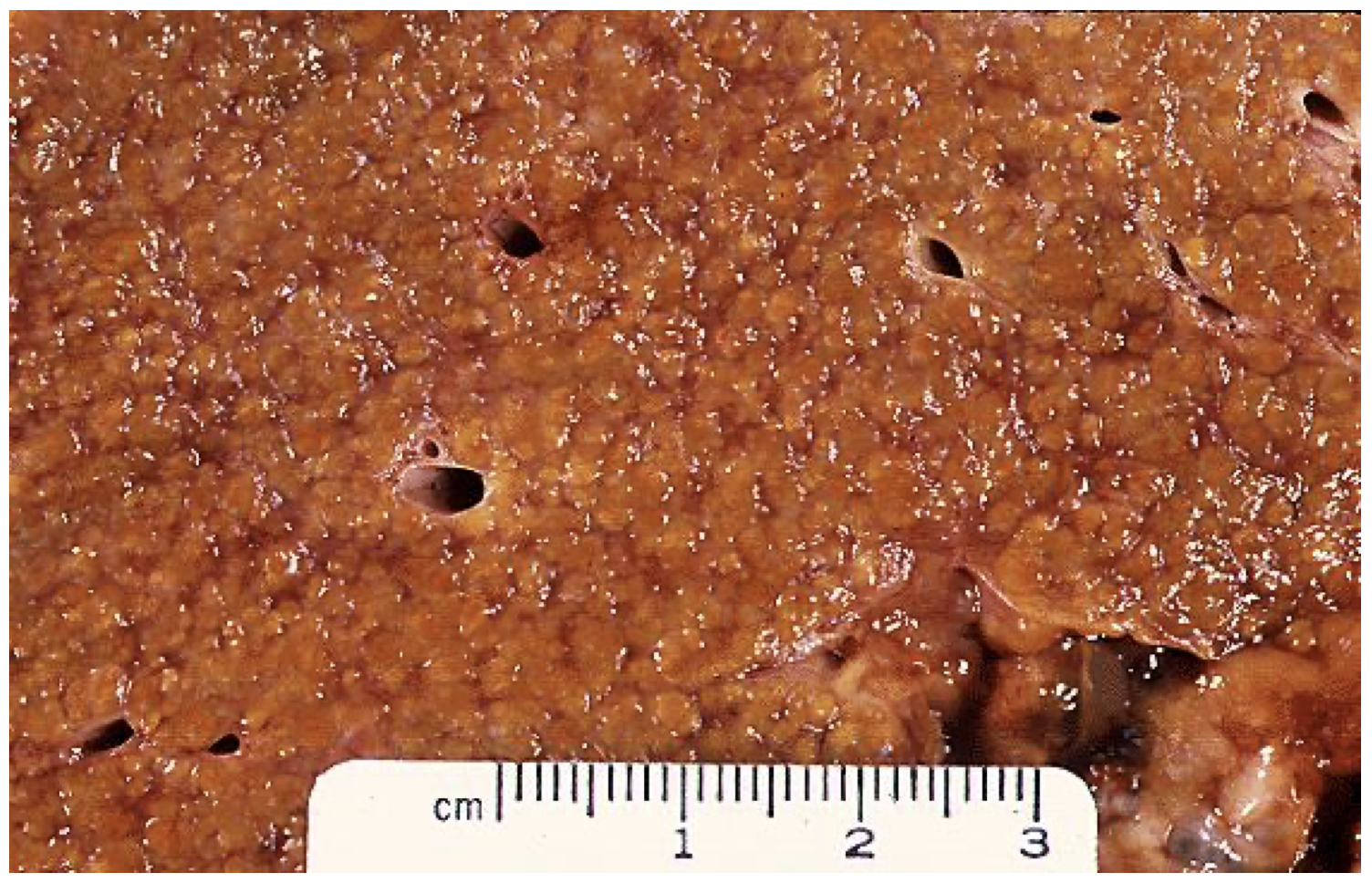
Cirrhosis, micronodular (alcoholic)
The cut surface of a liver with alcoholic cirrhosis demonstrates the fine nodularity common in alcoholic cirrhosis.
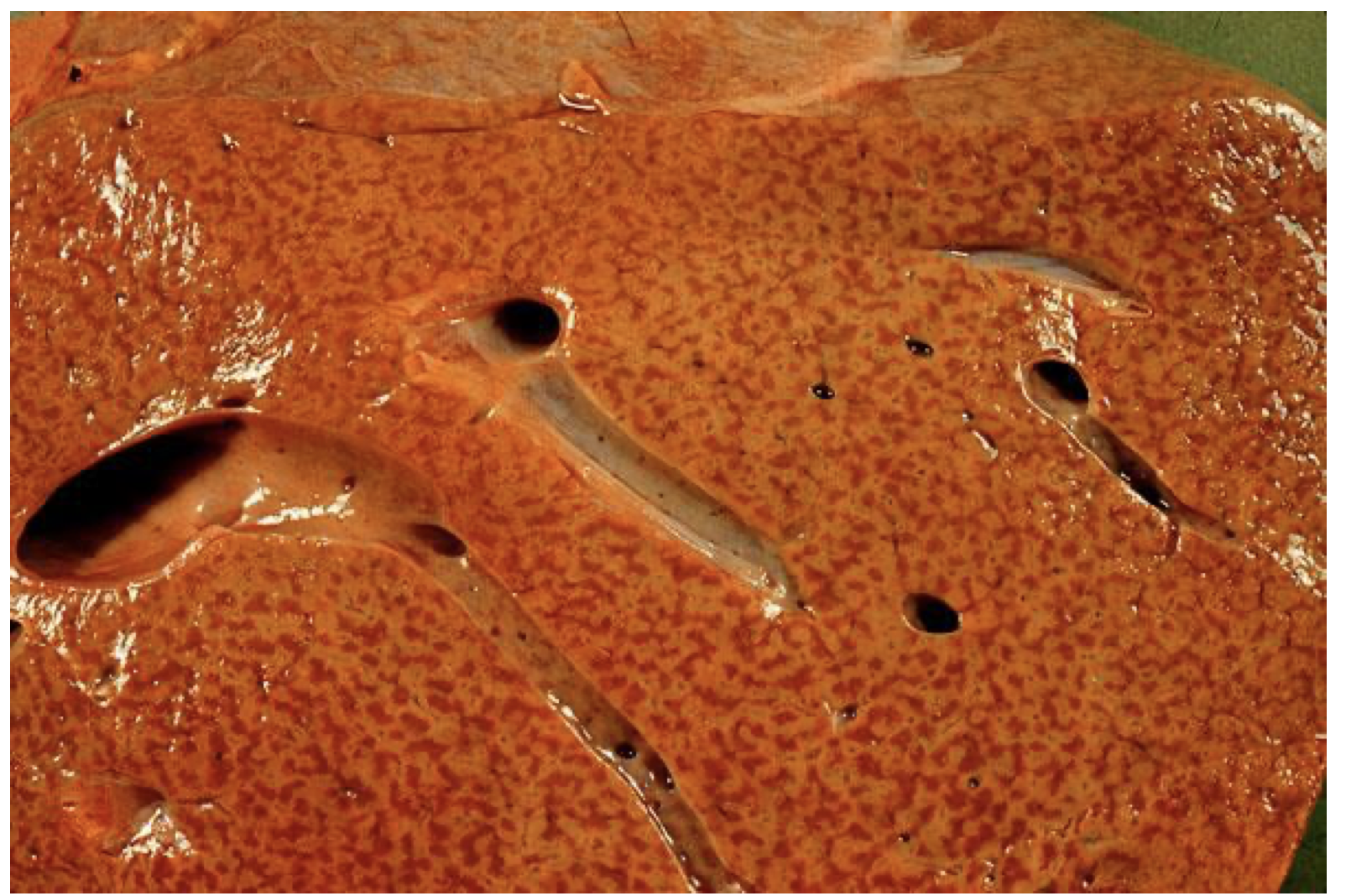
Chronic passive congestion, liver
Passive congestion of the liver occurs when there is right heart failure. The failure of the right ventricle causes the systemic circulation to back up behind it. In the liver, this manifests as centrolobular congestion, centered on the central vein. If the condition persists long enough, there may actually be necrosis of hepatocytes near the central vein. The repair process ensues, with resulting central fibrosis, or so-called "cardiac cirrhosis". The pattern of fibrosis is different from cirrhosis due to alcoholic liver disease, since fibrosis in that condition bridges from portal to portal.
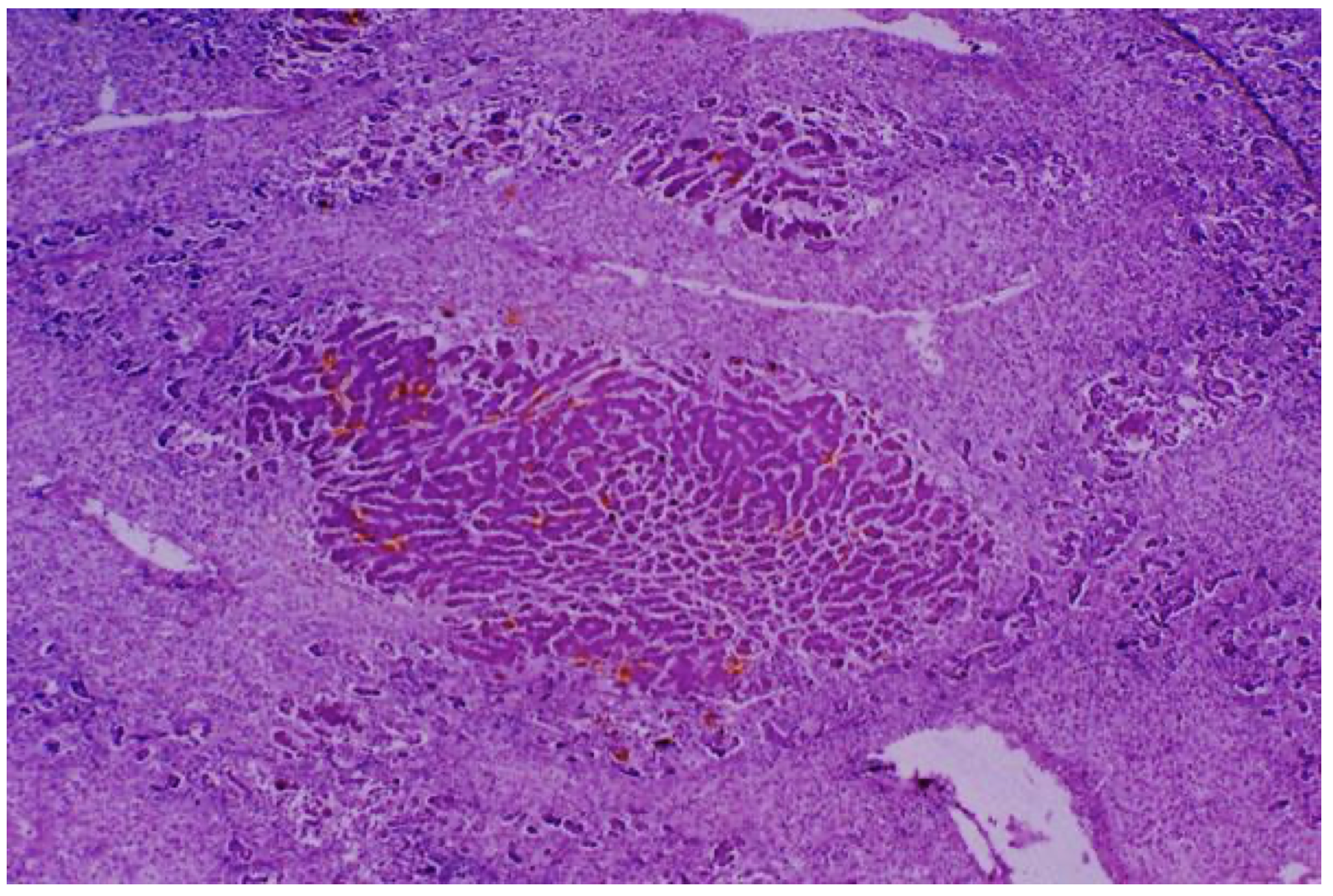
Chronic active hepatitis, photomicrograph, H/E x10
This scanning power photomicrograph shows the massive destruction that occurs with chronic active hepatitis due to hepatitis B or C virus. Most of the slide consists of areas of fibrosis, with a few remnants of viable hepatocytes.

Acute pyelonephritis, gross
In acute pyelonephritis, the infection generally ascends from the bladder, although it is possible to get hematogenous spread (rare). The infection ascends into the renal tubular system. Grossly, the kidney is red and swollen (inflamed), and yellow streaks can be seen in the medulla. These correspond microscopically to tubules filled with pus.

Chronic pyelonephritis, gross
The kidney is contracted from chronic inflammation and fibrosis. In pyelonephritis, scarring is often asymmetric, versus symmetrical scarring in vascular disease. Typically, reflux may be worse in one ureter vs. the other, whereas atherosclerosis affects both kidneys equally.
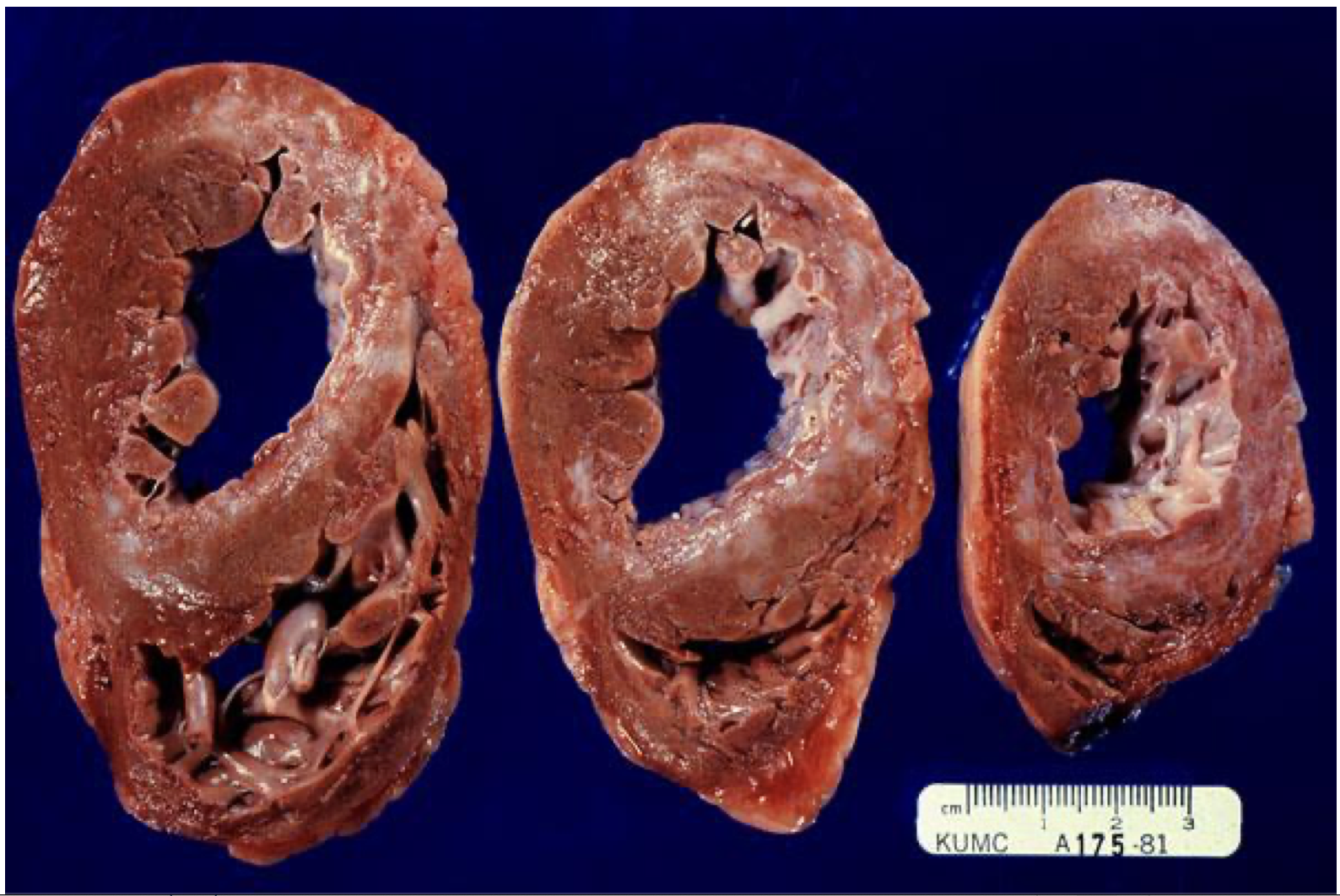
Heart, gross, fibrosis of healed infarcts
These cross-sections of heart show old infarcts, which appear gray or white grossly. Microscopically, they would consist of mature collagen.
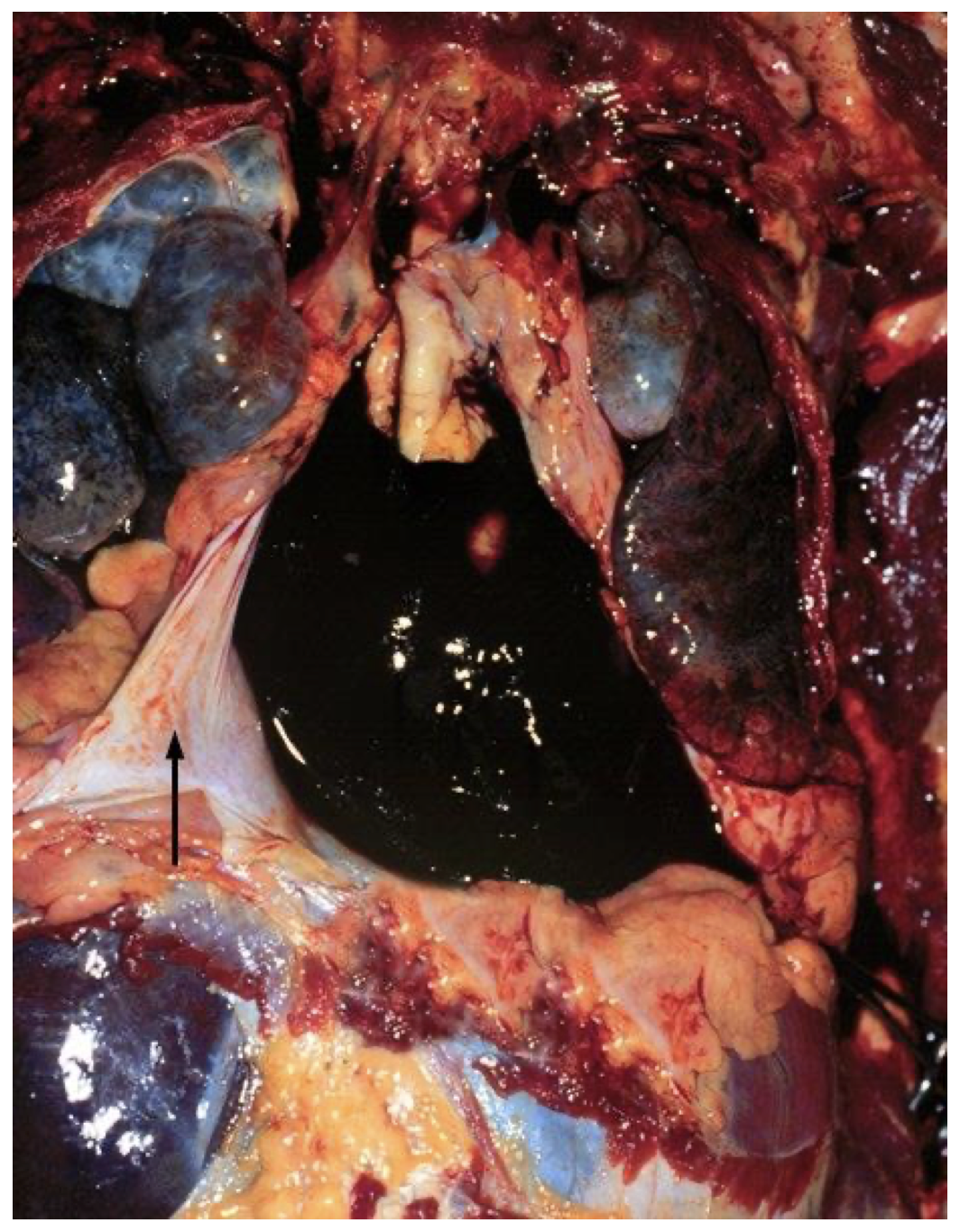
Rupture, left ventricle, with hemopericardium, gross, MI, day 6
This photograph of the chest cavity at autopsy shows reflected pericardium (arrow) and hemopericardium due to left ventricular rupture of an acute myocardial infarct. The infarct was about 6 days old.
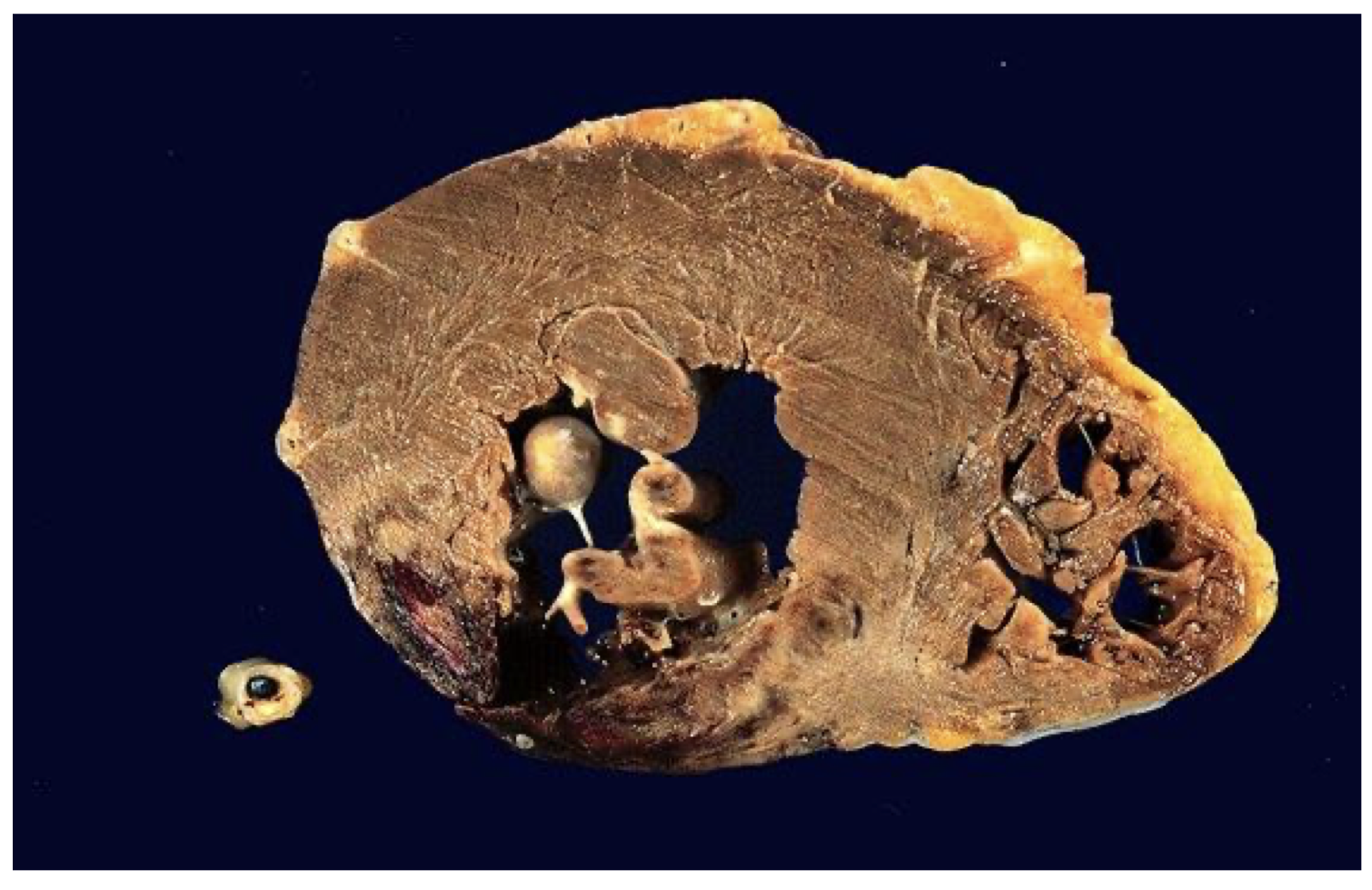
Rupture, left ventricle, with hemopericardium, gross, MI, day 6
This photograph shows a cross-section of left and right ventricle. The left ventricle has ruptured through the free wall on the lower left, to cause a hemopericardium, cardiac tamponade, and death. Typically, this occurs a week or more into the clinical course of a myocardial infarct, because macrophages have begun to digest infarcted debris, whereas fibroblasts have not yet completed their task of laying down collagen.