PAEA OBGYN EOR Topics
1/334
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
335 Terms
1. G2 P1001
2. G4 P1111
3. G3 P2103
1. currently pregnant, 1 term delivery, 1 living child
2. currently pregnant, 1 term delivery, 1 preterm delivery, 1 abortion/miscarriage, 1 living child (cannot tell if it is term or preterm child by formula)
3. currently pregnant, twins at term, 1 at preterm, 3 living children
G (# pregnancies)
T (# term deliveries at 37 weeks or more including stillbirths)
P (# preterm deliveries at 20-37 weeks)
A (abortions <20 weeks including miscarriages)
L (# living children)
a previable fetus is defined as
<24 weeks old (varies w/ guidelines)
what are the routine test during the first prenatal visit?
blood pressure, blood type & Rh, CBC, UA (glucose & protein), random glucose, HBsAg, Hep C, HIV, syphilis, rubella titer, VZV titer, pap, sickle cell & CF screening
diagnosis of pregnancy can be detected by serum B-hCG at ____ days after conception and by urine B-hCG at ____ days after conception
serum B-hCG: 5 days after conception
urine B-hCG: 14 days after conception
how is estimated date of delivery (EDD) determined?
Naegele's Rule: from 1st day of LMP
1. subtract 3 mos, add 7 days, add 1 year
2. add 9 mos & 7 days
ex: LMP started 8/7/16 = EDD: 5/14/17
when estimating gestational age on US what measurements can you use?
1. crown rump length (CRL)
2. biparietal diameter
3. head circumference
4. abdominal circumference
5. femur length
what physical exam and lab tests should be performed on initial visit of a pregnant patient?
full physical exam, BP, pelvic exam w/ pap smear (unless done in last 6 mos), G/C Cx's, bimanual exam to check size of uterus and help estimate # weeks into pregnancy, US if unsure of LMP to date # weeks
labs: CBC (r/o anemia), blood type & Ab screen + Rh status, RPR, HBSAg, rubella Ab screen, VZV Ab screen if no h/o chickenpox, UA w/ Cx, blood glucose, HIV, sickle cell/CF screen, PPD in high risk pts, screening for aneuploidy offered (inc or dec free B-hCG, PAPP-A low w/ down syndrome, inc nuchal translucency @10-13 weeks US)
what are the screening tests for aneuploidy (including down syndrome)? when are they performed?
ALL offered around 10-13 weeks
1. free B-hCG (high or low can be indicative of abnormalities)
2. PAPP-A (usually low w/ DS)
3. nuchal translucency (inc thickness on US)
4. if any above + can be offered chorionic villus sampling (or if they have any RF for aneuploidy such as advanced maternal age/AMA, previous child w/ chromosomal abnmlity, abnml US, prior pregnancy losses) but inc r/o spontaneous abortion w/ procedure
*amniocentesis offered around 15-18 weeks w/ same indications as CVS (both can diagnose chromosomal abnormalities and have risk of spontaneous abortion)
the uterus softening at 6 weeks is what sign?
Ladin's sign
the uterine isthmus softening after 6-8 weeks gestation is what sign?
Hegar's sign
bluish coloration of the cervix & vulva around 8-12 weeks is what sign?
Chadwick's sign
a palpable lateral bulge or softening of the uterine cornus (where uterus meets fallopian tubes) at 7-8 weeks gestation is what sign?
Piskacek's sign
cervical softening of the cervix and vulva around 8-12 wks
Goodell's sign
what are the # weeks in each trimester?
1st tri: 1-12
2nd tri: 13-27
3rd tri: 28-birth
what should be checked at routine first trimester visits?
BP, weight, urine dipstick, measurement of uterus/fundal height, auscultation of fetal heart sounds at 10-12 weeks (nml 120-160)
what week should the uterus/fundal height measure above the pubic symphysis? midway between pubic symphysis/umbilicus? at umbilicus? 2-3cm below xiphoid process?
-above the pubic symphysis? 12 wks
-midway between pubic symphysis/umbilicus? 14-16 wks
-at umbilicus? 20 wks
-2-3cm below xiphoid process? 38 wks
after 20 weeks gestation, the fundal height should measure +/- ____cm from the # of weeks
+/- 2 cm
when are fetal heart tones audible with doppler US? what rate is nml?
10-12 weeks (end of 1st trimester) at 120-160 bpm
what is the quad screen test for? what are the tests? when is it performed?
-to screen for trisomy 21 (down syndrome), trisomy 18, and NTD like spina bifida
-tests: alpha-feto protein, B-hCG, estradiol, and inhibin-A
-performed at 15-20 weeks
-can be performed w/ 1st trimester screening - called "integrated screening"
what would you expect with the quad screen if a baby had down syndrome?
a-FP: low
B-hCG: high
estradiol: low
inhibin-A: high (always high in chromosomal abnormalities)
when can a fetus be detected by pelvic US?
5-6 weeks
what would you expect with the quad screen if a baby had a neural tube defect?
a-FP: high
B-hCG: N/A
estradiol: N/A
inhibin-A: high (always high in chromosomal abnormalities)
what would you expect with the quad screen if a baby had trisomy 18?
a-FP: low
B-hCG: low
estradiol: low
inhibin-A: high (always high in chromosomal abnormalities)
the anatomy ultrasound (checking for amniotic fluid level, fetal viability, growth, and anatomy) is performed at how many weeks?
18-22 weeks
when is gestational diabetes screened for? what is the screening test & BS limit? what is the diagnostic test and & BS limits?
-24-28 weeks
-glucose loading test (GLT): 50g given and serum glucose checked 1 hr later- failed if BS ≥140
-glucose tolerance test (GTT): fasting BS checked (≥95) then 100g glucose given and BS checked at 1 hr (≥180), 2 hr (≥155), 3 hr (≥140); failure = at least 2/4
when is "quickening" aka fetal movement felt?
16-20 weeks
how often are OB visits scheduled?
Q4 weeks first 2 trimesters, 1-28 wks
Q2 weeks 28-36 wks
Qwk 36-birth
what tests/physical examinations should be performed at third trimester visits?
-repeat Ab titers in unsensitized Rh(-) mothers followed by RhoGAM @ 28 weeks & w/I 72 hrs of childbirth
-group B streptococcus screening @ 32-37 weeks via vaginal-rectal Cx
-H/H @ 35 weeks
-biophysical profile/BPP if there are complications: (5 variables: fetal breathing, fetal tones, amniotic fluid levels, NST (nonstress test), & gross fetal movements - 2 pts each)
-non-stress testing: baseline fetal HR 120-160
-Leopold maneuvers to determine fetal presentation, or US if cannot determine (can do external cephalic version if breech presentation)
-after 37 weeks sweeping membranes offered at weekly visits to help induce labor
In high risk individuals what tests are run again in the third trimester? prophylactic tx?
-G/C Cx
-if + HSV, prophylactic acyclovir initiated at 36 weeks
-if + GB strep, IV PCN given when presenting in labor
what are the hematologic effects of pregnancy?
-dilutional anemia (plasma vol inc by 50% but RBCs only inc by 20-30%)
-WBC increases (especially during stress of labor- ppl confuse this with sepsis)
-platelets dec
-hypercoagulable state (inc thromboembolic events d/t Virchows triad- venous stasis, endothelial damage, hypercoagulability & inc in factors VII-X and fibrinogen)
-iron deficiency anemia (d/t inc demand on hematopoiesis)
nonstress testing is reactive when?
-2 or more accelerations in 20 minutes
-fetal HR inc 15 or more bpm from baseline lasting 15 or more seconds
what are the effects of pregnancy on the heart and BP?
-CO increases by 30-50% (first in SV then in HR and a dec in SVR)
-BP decreases slightly (so if there is an inc be suspicious of preE/eclampsia)
dyspnea of pregnancy occurs in 60-70% of pts and is d/t
dec PaCO2 levels, inc tidal volume, decrease TLC
what GI changes occur in pregnancy?
N/V (>70%), delayed gastric empyting & dec gastroesophageal sphincter tone (= GERD), dec motility of lg bowel (= constipation)
what kidney changes occur in pregnancy?
-50% inc in GFR
-the kidneys inc in size and the ureters dilate (cause of inc r/o pyelonephritis)
what are the effects of pregnancy on the endocrine system?
-hyperestrogenic state (produced by placenta)
-placenta also produces hCG (doubles Q48 hrs in early pregnancy peaking at 10-12 wks) which maintains corpus luteum early on
-corpus luteum produces progesterone which maintains uterine lining
-human placental lactogen is produced by placenta and responsible for nutrient supply to fetus but can cause a diabetogenic state (bc insulin antagonist)
-prolactin greatly increases
-inc in T3/4 while fT4 and TSH remain minimally changed
what are the effects of pregnany on the msk system?
-change in center of gravity = low back strain
-carpal tunnel syndrome is common
what are the effects of pregnancy on the dermatologic system?
-spider angiomatas
-palmar erythema
-hyperpigmentation of nipples, umbilicus, abdominal midline (linea nigra), perineum, face (melasma)
approximately what increase in calories is recommended in nml BMI pregnant patients? what amount of weight gain is recommended in underweight, nml, and overweight patients?
300 cal per day (500 cal when breastfeeding)
-underweight: 28-40 lb
-nml: 20-30 lb
-overweight: 15-25 lb
what nutritional requirements requirements besides caloric intake increase during pregnancy?
-protein
-iron (IDA common in pregnancy)
-folate (prevent NTD)
-calcium
-other vitamins and minerals
what is the most common fetal position inside the womb during the third trimester? what are other potential positions?
-MC: cephalic (vertex)
-breech (butt or legs down)
-transverse
-oblique
during the first stage of labor what are the most common positions of the fetal head? how can you tell what position is presenting?
-OA (occiput anterior best- where baby comes out face down), LOA, ROA
-OT and OP are considered malpositioned
-palpate the anterior and posterior fontanelles (anterior is bigger and more central)
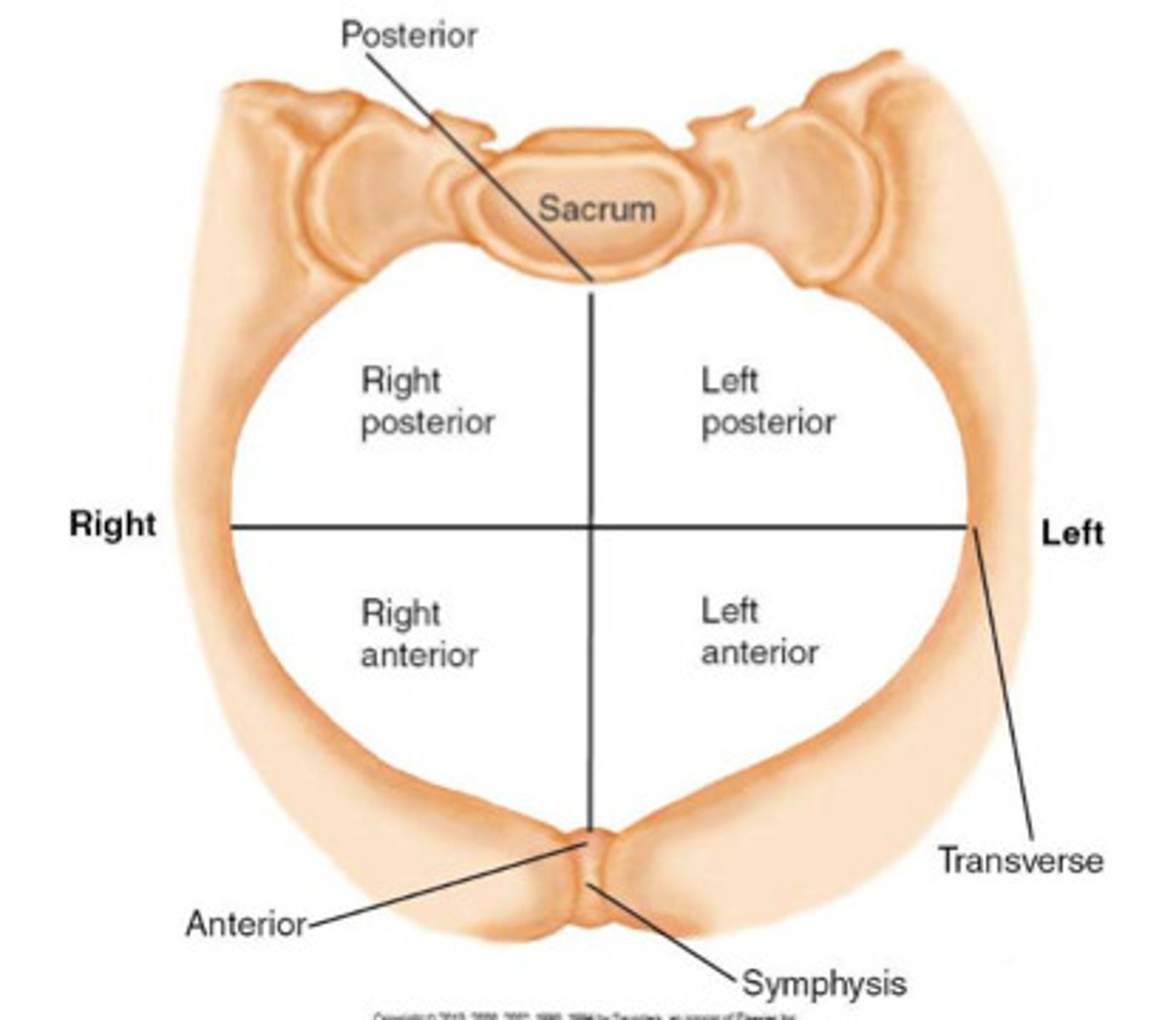
in persistent OT & OP fetal head positions during labor what is the management to prevent prolonged labor or need for c-section?
-manual rotation to OA (can use forceps or vaccuum as well)
-if unable to rotate can attempt vaginal delivery with forceps or vaccuum in OP position (50% delivery rate) but not OT (rare vaginal delivery)
-if all else fails- do c/s
fraternal twins are ____zygotic whereas identical twins are ____zygotic
fraternal: dizygotic (2 ova fertilized by 2 different sperm)
identical: monozygotic (1 ova fertilized by 1 sperm that divides after fertilization) - inc r/o fetal transfusion syndrome and discordant fetal growth
what are the maternal complications of multiple gestations?
-preterm labor
-spontaneous abortion
-preeclampsia
-anemia
-placenta previa
-cervical incompetence
-gestational diabetes
-postpartum hemorrhage
what are the fetal complications that can occur in multiple gestation?
-intrauterine growth restrictions (small for gestational age/SGA)
-placental abnormalities
-breech presentation
-umbilical cord prolapse
-preeclampsia
what labs will be elevated in multiple gestation?
-B-hCG
-human placental lactogen (HPL)
-materal serum a-fetoprotein (MSAFP)
APGAR score is performed at ___ & ___ minutes after birth; again at ___ if abnormal
1 & 5 min postpartum; again at 10 min if abnormal
a baby is born crying with a pink body but blue extremities, HR of 157, grimaces feebly on stimulation, flexes arms/legs and resists extension; what is the APGAR score?
8

what is the difference between contractions of pregnancy and Braxton-Hicks contractions?
Braxton-Hicks are not associated with cervical dilation
what are the cardinal movements of labor?
1. engagement
2. flexion
3. descent
4. internal rotation
5. extension
6. external rotation
7. expulsion
what are the stages of labor?
-stage I: onset of labor (true regular ctxs w/ cervical dilation until full dilation (10 cm); latent phase: cervix effacement with gradual dilation; active phase: rapid cervical dilation (usually beginning at 3-4 cm)
-stage II: time from full cervical dilation to delivery of fetus; passive phase: complete dilation to active maternal expulsion efforts; active phase: from active maternal expulsion efforts to delivery of fetus
-stage III: postpartum until delivery of placenta; avg 5 min but can be b/t 0-30 min
-stage IV: 1-2 hrs postpartum that mother is watched/evaluated for complications
what are the 3 signs of placental separation postpartum?
1. gush of blood
2. lengthening of umbilical cord
3. anterior-cephalad mvmt of uterine fundus (becomes globular and firmer) after placenta detaches
cervical examination of a pregnant patient in labor is done by what 5 criteria that make up the Bishop score?
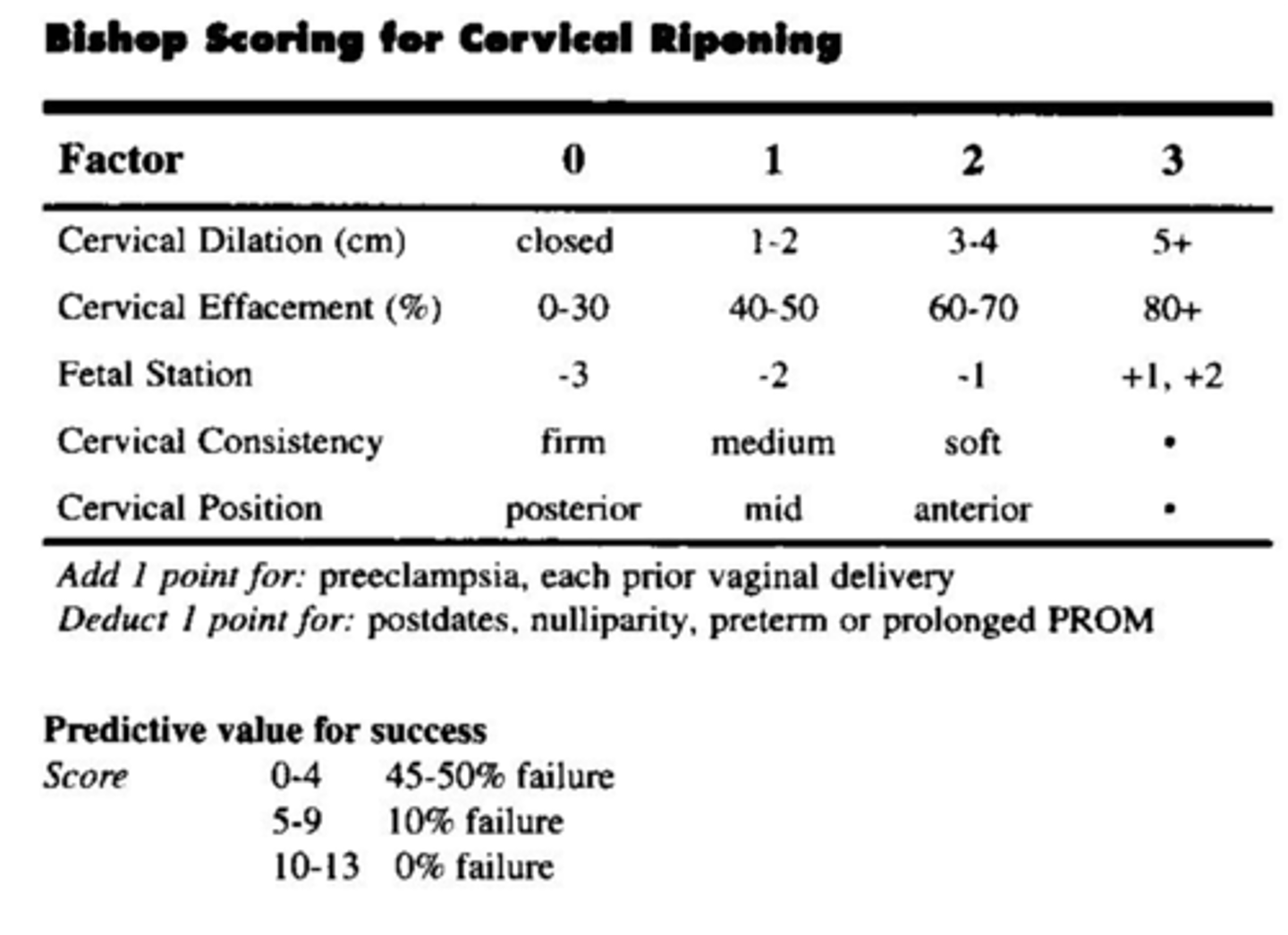
______ of labor is the attempt to begin labor in a nonlaboring patient, whereas ______ of labor is intervening to increase the already present contractions
induction vs augmentation
what are the indications for induction of labor? how do you induce?
indications: postterm pregnancy, preeclampsia, LGA, nonreassuring fetal testing, intrauterine growth restriction, chorioamnionitis, IUFD, etc.
labor is induced with prostaglandins (to "ripen" cervix; misoprostol or PGE2), oxytocic agents (oxytocin aka Pitocin), mechanical dilation of the cervix, and/or artificial ROM (amniotomy)
an external tocometer is placed on the pt's abdomen near the fundus and is used to measure
contractions by sensing pressure when abdomen gets firmer- best for measuring frequency of contractions and to monitor fetal heart rate accels/decels
what degree of fetal heart rate variability is reassuring?
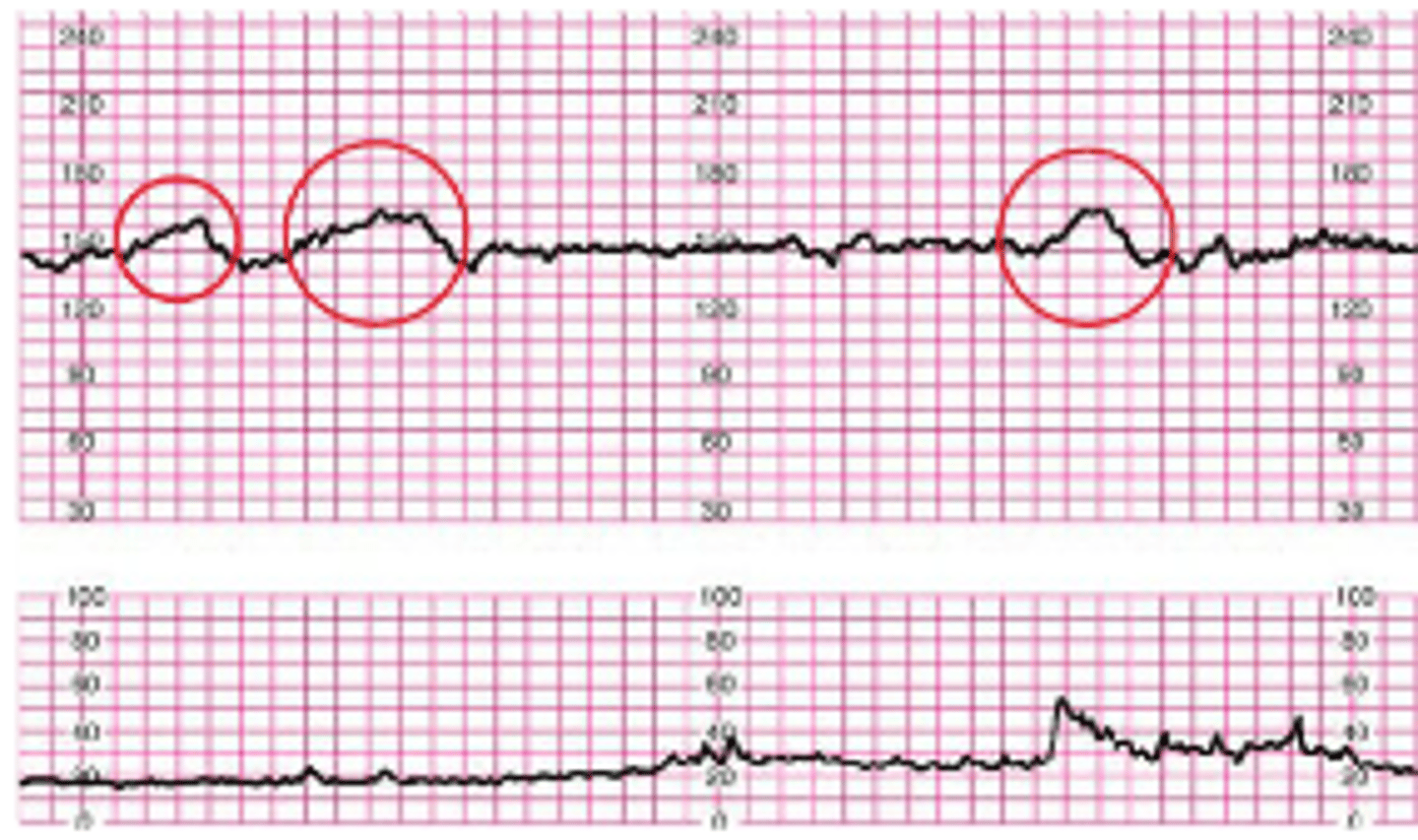
moderate (little variability may mean fetus is asleep or inactive and absent variability may mean fetal death) aka lines will appear squiggly instead of flat like top line
a reactive fetal heart tracing is defined as ___ accelerations of at least ___ beats per minute over the baseline that last for at least ___ seconds within 20 minutes
2 accelerations, at least 15 bpm above baseline, for at least 15 seconds in 20 minutes
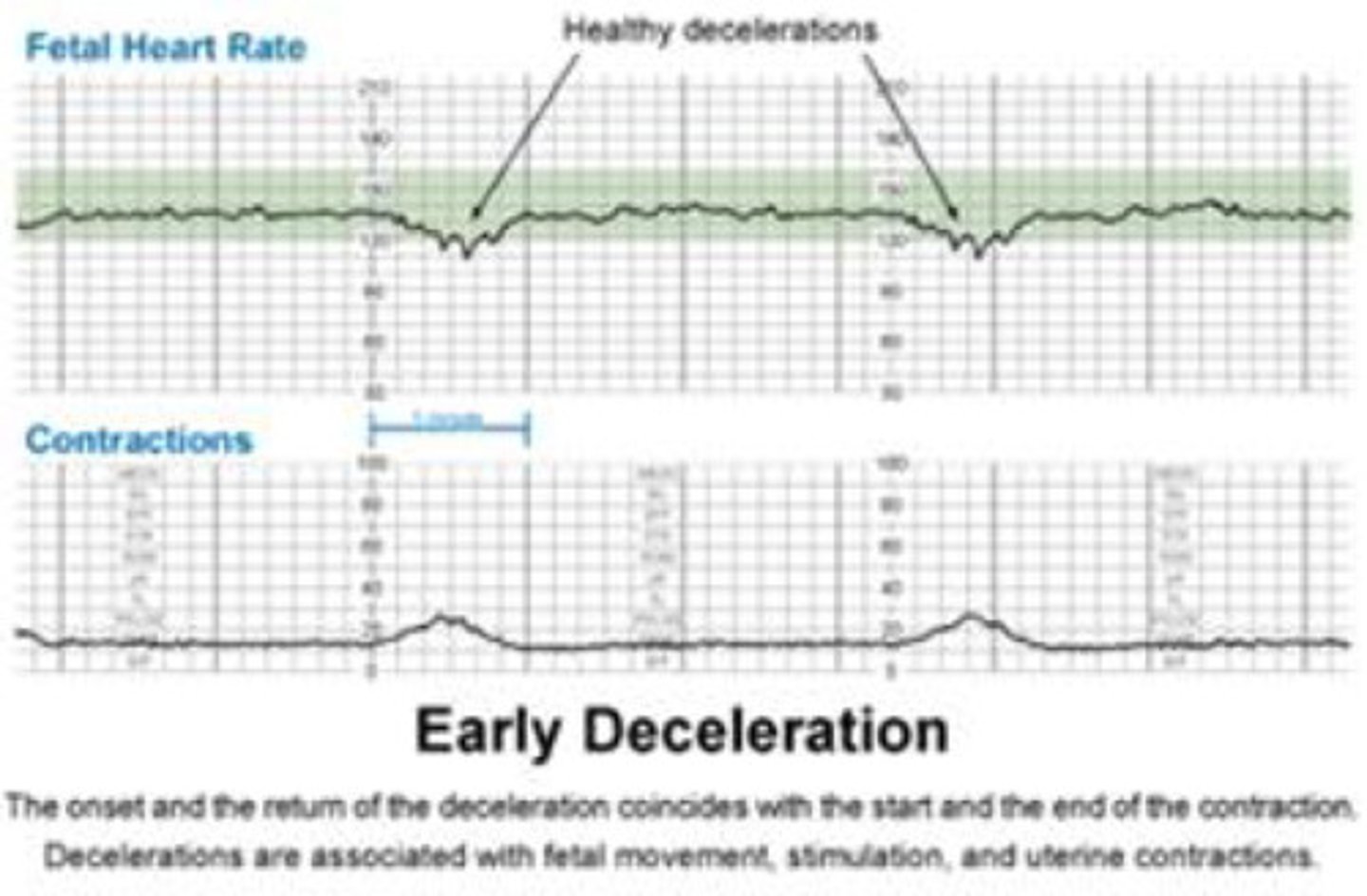
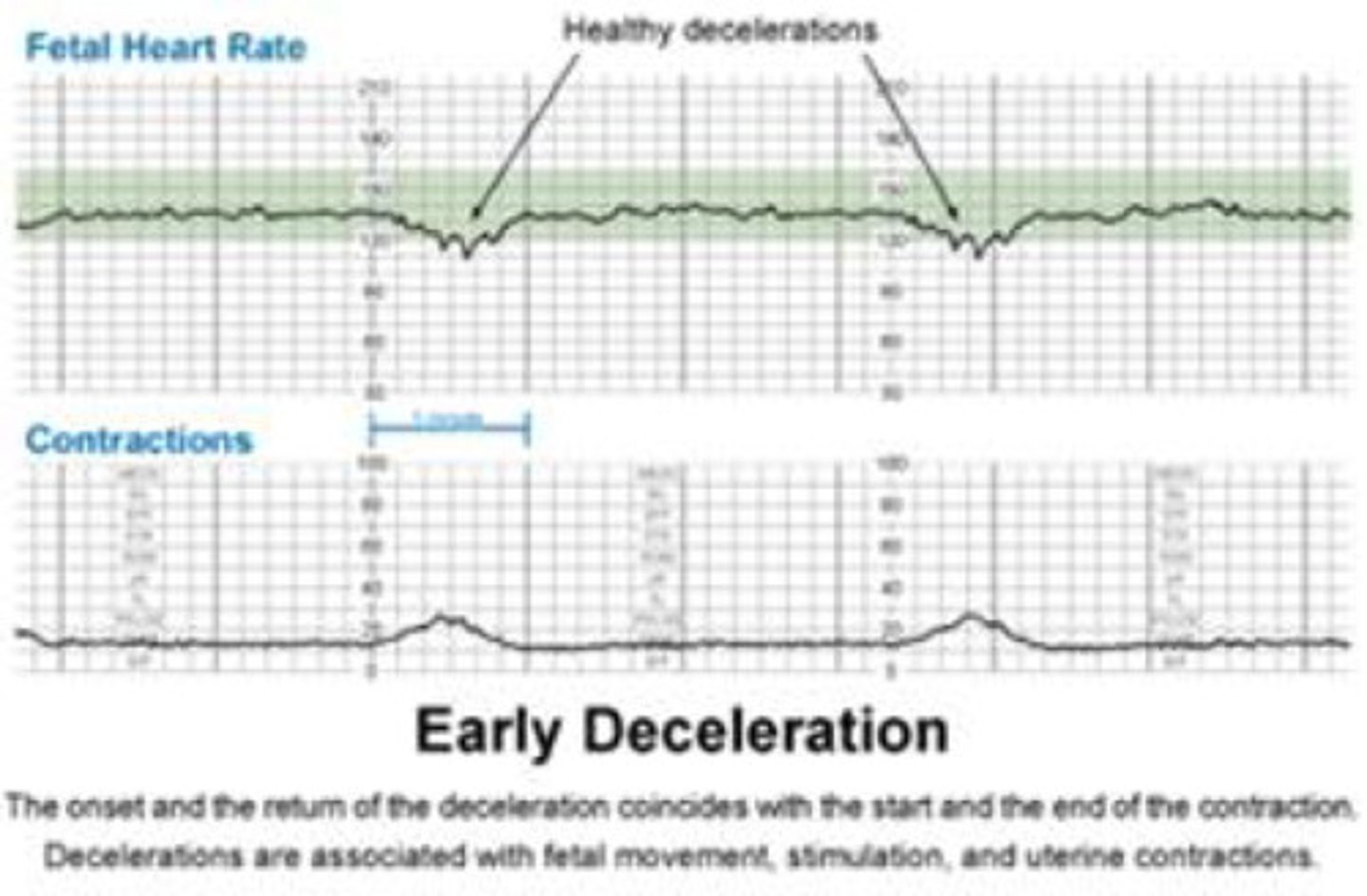
what kind of fetal heart deceleration is a result of fetal head compression during a contraction?
early decel (begins and ends with contraction)
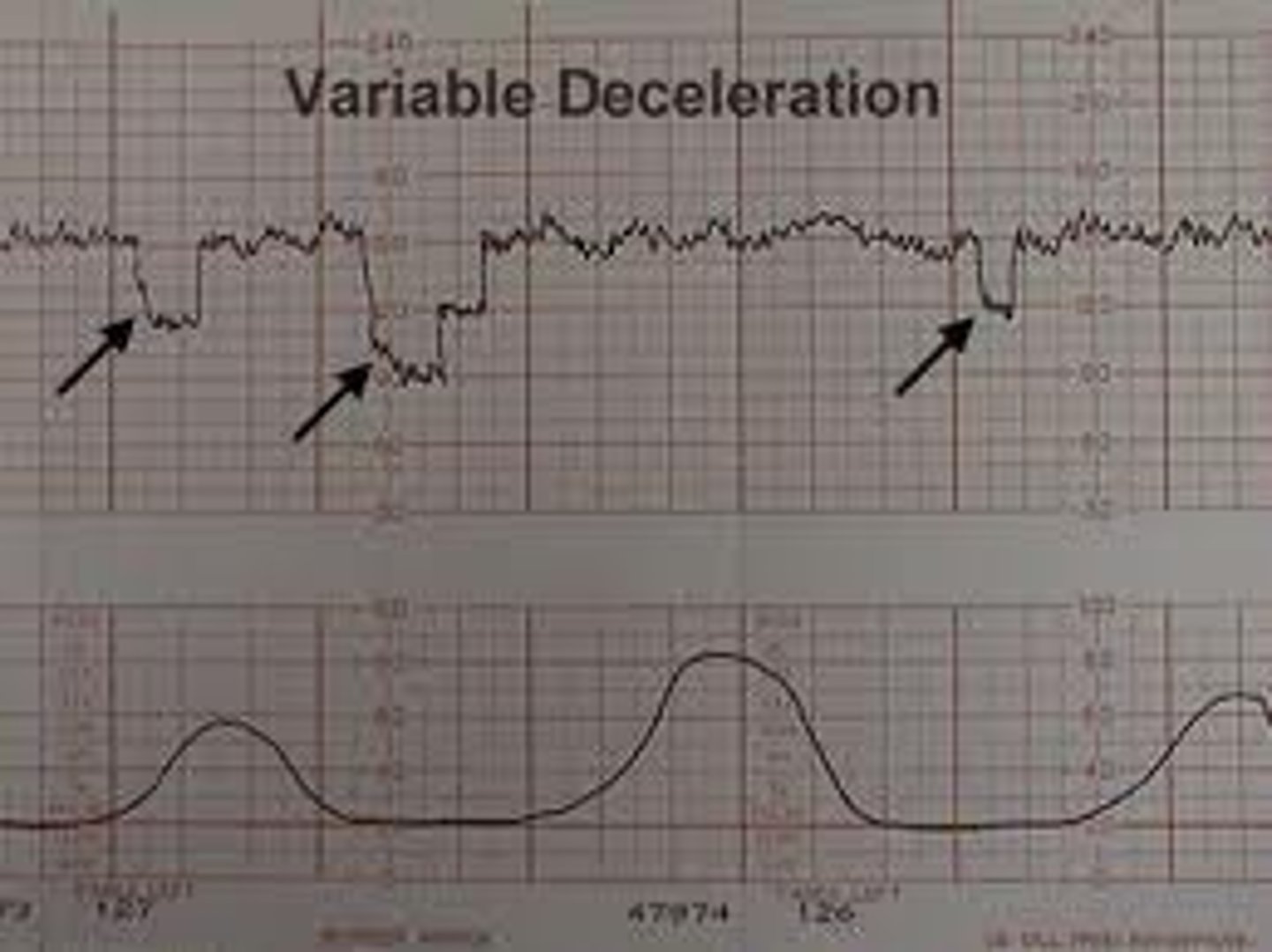
what kind of fetal heart deceleration is a result of umbilical cord compression?
variable decel (can occur at any time and drops more precipitously than early or late decels)
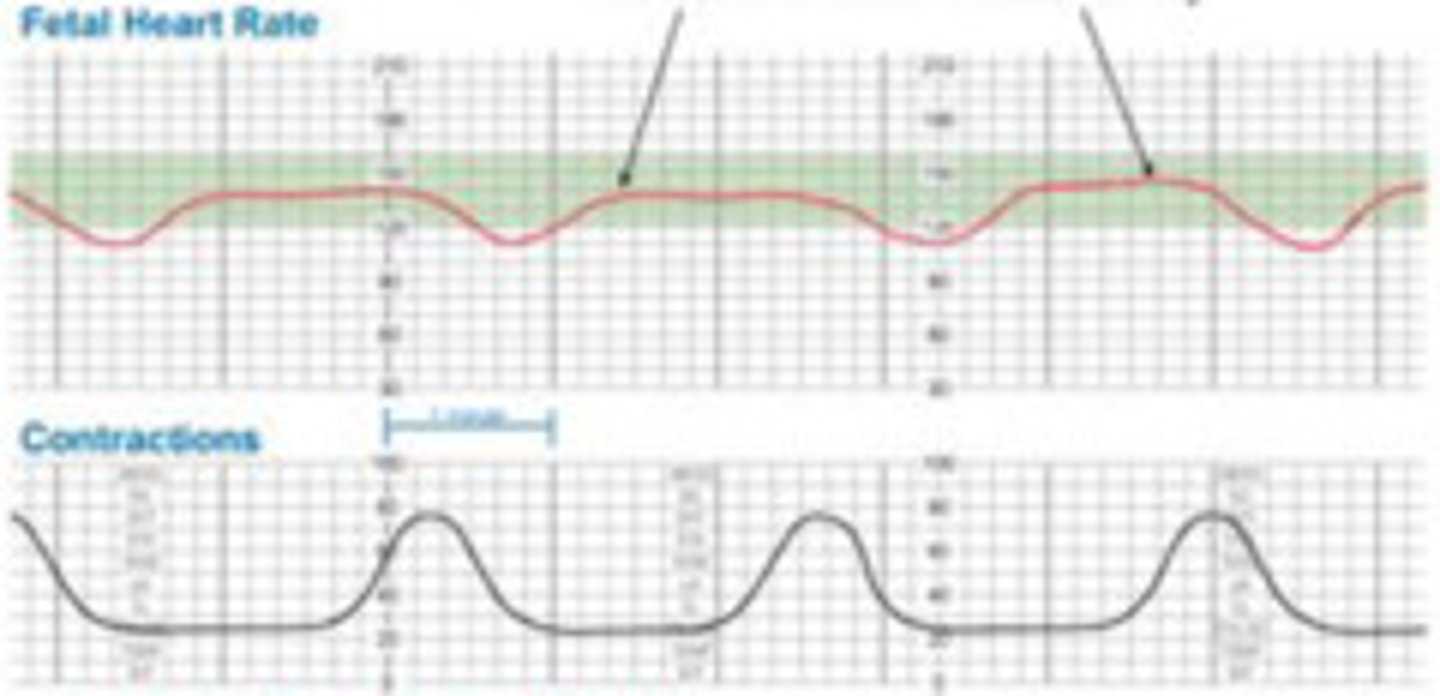
what type of fetal heart deceleration is a result of uteroplacental insufficiency and are the most worrisome type?
late decel (begin at peak of contraction and slowly return back to baseline after contraction has finished) they may degrade into bradycardias as labor progresses
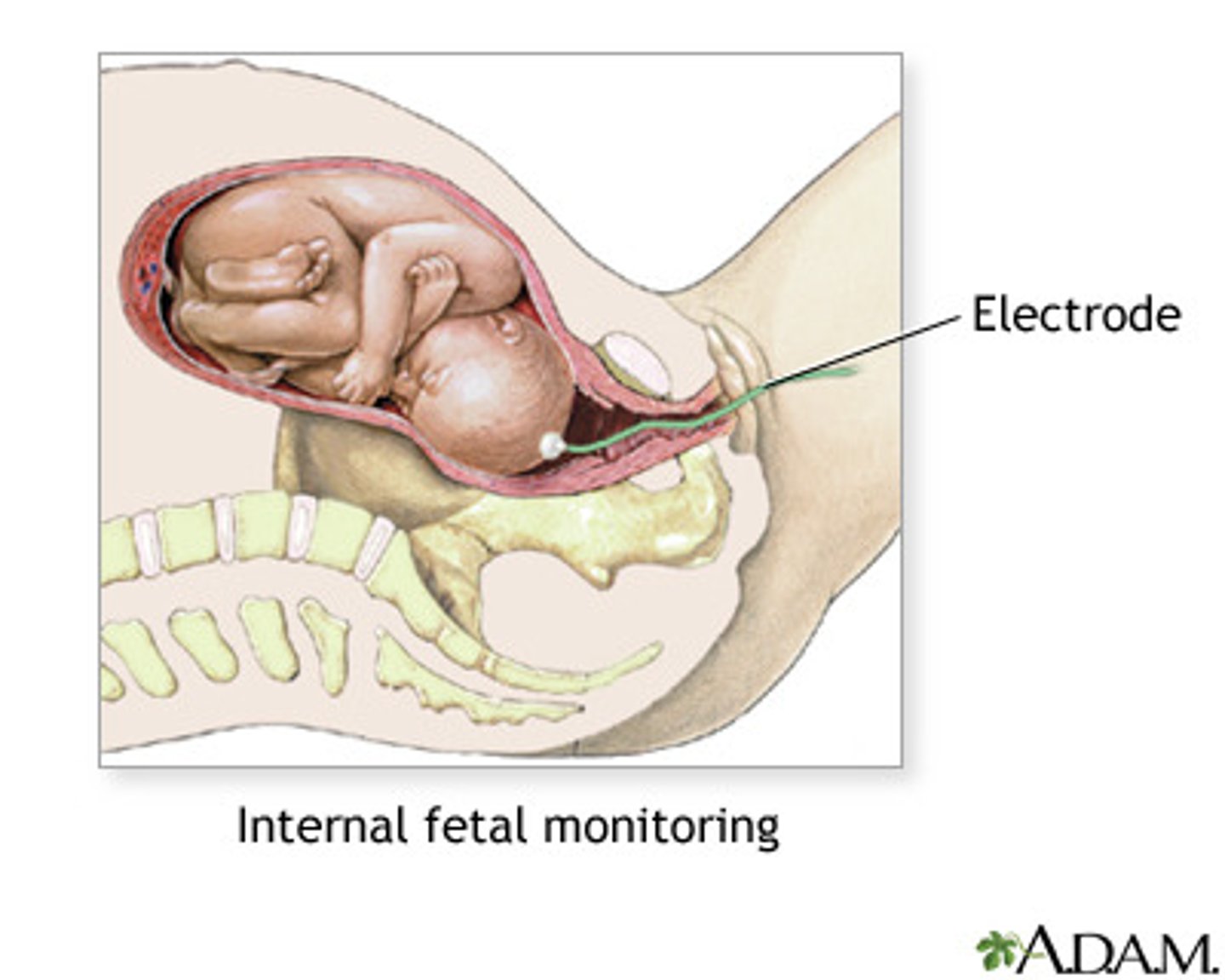
when is a fetal scalp electrode indicated (FSE) to monitor fetal heart tracings?
a fetus with late decels bc the FSE is more sensitive by tracking the potential difference created by depolarization of the fetal heart; it also is better because the tracings do not get lost during contractions or fetal position changes like they do with the Doppler
describe what category I-III fetal heart rate tracings are?
-cat I: nml FHR w/ nml baseline, moderate variability, & no variable/late decels
-cat II: indeterminate FH tracing (variable/late decels, brady/tachycardia, or minimal/marked variability)
-cat III: abnml FH tracing (absent variability, recurrent late/variable decels, or bradycardia; sinusoidal pattern consistent w/ fetal anemia)
in obese patients or those where the external tocometer is not adequately assessing the frequency or strength of contractions, what else can be placed?
IUPC (intrauterine pressure catheter)
-baseline pressures b/t 10-15 mmHg
-early contractions inc by 20-30 mmHg
-late contractions inc by 40-60 mmHg
what are 2 ways to assess hypoxemia in a fetus during labor?
1. fetal scalp pH (nick scalp for blood sample and assess acidemia- not really used in US anymore)
2. oximeter (placed against their cheek- not really used either)
during the second stage of labor, what types of decels are normal as long as they resolve quickly after each contraction and there is no loss of variability
early and variable decels are common
-nonreassuring fetal status during 2nd stage: repetitive late decels, bradycardias, or loss of variability
in nonreassuring fetal status during 2nd stage of labor (repetitive late decels, bradycardias, or loss of variability) what actions should be taken?
-O2 face mask
-turned to left side to dec IVC compression and inc uterine perfusion
-oxytocin (if being used) should be d/c'd
what are the highest risks of operative vaginal deliveries (forceps and vacuum extraction)?
-forceps (facial nerve palsies)
-vacuum (cephalohematomas and shoulder dystocias)
*these can be performed during a prolonged 2nd stage, maternal exhaustion or need to hasten a delivery
what is given during stage 3 of labor to strengthen uterine contractions to decrease placental delivery time and blood loss?
oxytocin (pitocin)
retained placenta is defined as placental delivery/stage 3 lasting >___ minutes; it is common in preterm deliveries but can also be a sign of _________; how is it removed?
>30 minutes
-sign of placenta accreta (placenta invaded into or byond endometrial stroma)
-manual extraction (hand placed in intrauterine cavity and fingers used to shear placenta off surface of uterus)
what are the indications for cesarean section?
-2-4 hrs w/o cervical change in setting of adequate uterine contractions in active phase of labor
-breech presentation
-transverse lie
-shoulder presentation
-placenta previa
-placental abruption
-fetal intolerance of labor
-nonreassuring fetal status
-cord prolapse
-failed operative vaginal delivery
-active herpes lesions
-at least 2-3 previous c/s (risk of uterine rupture)
VBAC (vaginal birth after cesarean)/ TOLAC (trial of labor after cesarean) are common but have a slight risk ~1% of _________
uterine rupture
*1% after 1 c/s, 2% after 2 c/s, but after 3 risk goes way up so do a c/s
how long should stage 1 of labor last?
nulliparous: ~10-12 hrs (~ half a day)
multiparous: ~6-8 hrs (~ a 3rd of a day)
-but not really considered prolonged unless >20 hrs in nulli, >12 hrs in multi
how long should stage 2 of labor last?
nulliparous: 2 hrs or less
multiparous: 1 hrs or less
-add an extra hour if they have had a epidural
-considered prolonged if above these limits
spontaneous abortion is classified as before ___ weeks of pregnancy
<20 weeks (& it is MC during 1st 7 weeks)
Dx/Tx? a pregnant woman comes in at 8 wks GA c/o foul, brownish d/c, F/C, spotting that lead to heavy bleeding; on PE she has cervical motion tenderness; US shows no fetal heart beat
-septic spontaneous abortion (retained POC becomes infected and can spread to uterus/organs)
-D&E (dilation & evacuation) to remove POC (products of conception)
-broad spectrum abx
in a missed spontaneous abortion, the fetal demise occurred but the POC (products of conception) are retained in the uterus- usually found by lack of uterine growth, serially falling hCG, and US; what is the Tx?
-D&C if in 1st trimester (D&E if not)
-misoprostol (stimulate uterine contractions to expel POC)
what is the difference between a complete and missed spontaneous abortion?
-complete is when all POC (products of conception) are expelled; usually occurs w/ pain, cramps, and bleeding
-if mother Rh- need to give RhoGAM in complete abortions
what is the difference between incomplete and inevitable spontaneous abortions? tx?
-while they both involve cervical dilation, bleeding, & cramping, incomplete expels some of the POC (products of conception) while inevitable does not expel any POC.
-incomplete tx: RhoGAM (if indicated), pitocin, D&C in 1st tri, D&E in 2nd tri
-inevitable tx: RhoGAM (if indicated), suction curettage aka D&C in 1st tri, D&E in 2nd tri
what is the only type of spontaneous abortion where the pregnancy may still be viable?
threatened- pregnancy may progress or abortion may follow- just a wait and see issue so you send them home to rest
it is the MC cause of 1st trimester bleeding
in a threatened spontaneous abortion s/sx are bloody vaginal d/c, spotting to profuse bleeding, +/- contractions, uterus size compatible w/ dates, closed cervical os; are there POC (products of conception) expelled? what can you check to see if pregnancy still progressing?
-no POC expelled
-serial B-hCG to see if doubling
-remember to give RhoGAM if indicated
what is the MC cause of spontaneous abortion?
-fetal chromosomal abnormalities (50%)
-others include: maternal infxn, uterine defects, endocrine abnormalities, malnutrition, immunologic, physical trauma, smoking, drug use, etc.
what types of medical txs for elective/induced abortion are available?
1. (safe up to 9 weeks pregnant) mifepristone (an anti-progestin) + misoprostol 2-3 days later (prostaglandin that causes uterine contractions)
2. (safe up to 7 weeks pregnant) methotrexate (antimetabolite) + misoprostol 3-7 days later
surgical elective/induced abortions can be performed up until ____ weeks pregnant by what procedures?
until 24 weeks pregnant
-D&C (dilation & curettage w/ or w/o suction) @ 4-12 weeks gestation (1st trimester)
-D&E (dilation & evacuation) >12 weeks gestation (2nd trimester)
Dx/Tx? painful dark red vaginal bleeding in the 3rd trimester, contractions, fetal bradycardia, possible shock symptoms, tender/rigid uterus
-dx: placental abruption (premature separation of placenta from uterine wall)
-tx: hospitalization for hemodynamic stabilization, immediate delivery usually bc c/s
*DIC (disseminated intravascular coagulation) occurs in 10% of pts
what is the MC cause of placental abruption (premature separation of placenta from uterine wall)?
-HTN
-others include: smoking, ETOH, cocaine, folate deficiency, high parity, AMA (advanced maternal age), trauma, chorioamnionitis
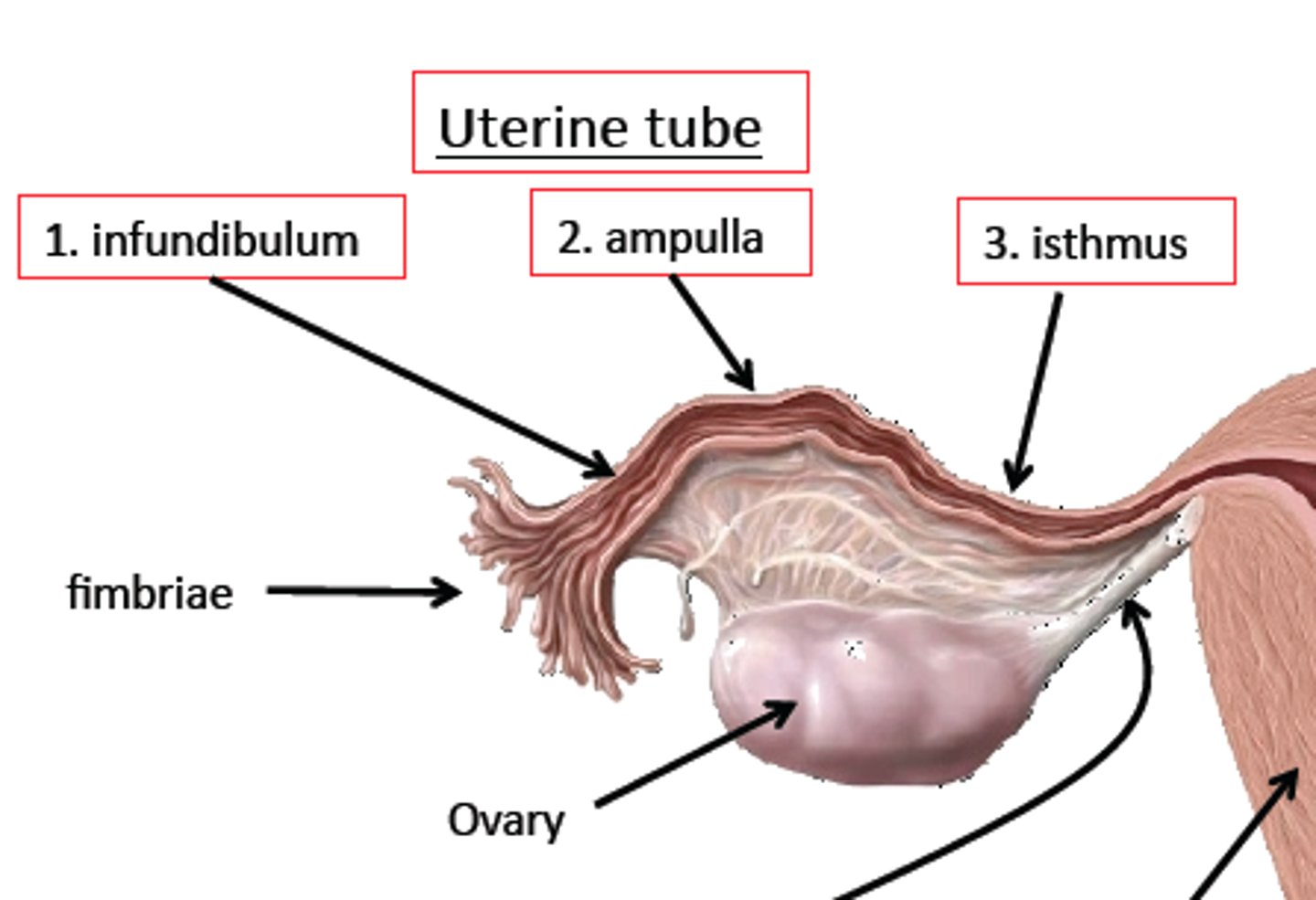
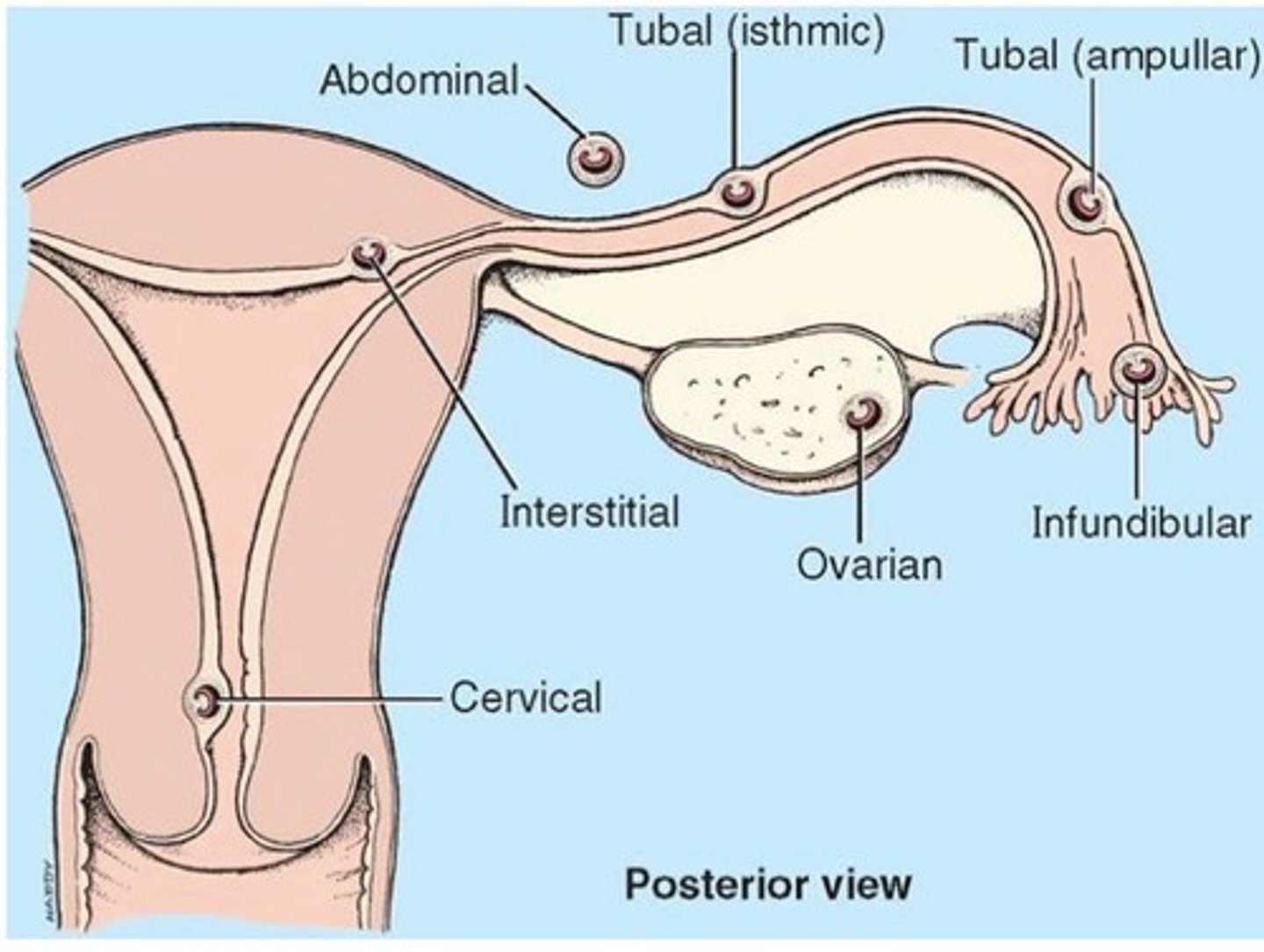
where is the MC site of ectopic pregnancies?
-98.3% in fallopian tubes (especially ampulla)
-1.4% in abdomen
-0.15% in ovary
-0.15% on cervix
what are some risk factors for ectopic pregnancy?
-previous abdominal surgery (adhesions)
-PID
-previous ectopic
-tubal ligation
-endometriosis
-IUD use
-assisted reproduction
what is the classic triad of sx's with ectopic pregnancy?
1. unilateral pelvic/abdominal pain
2. vaginal bleeding
3. + pregnancy (noticed by test or by amenorrhea)
how is a ectopic pregnancy (that has not ruptured) diagnosed and treated?
-Dx by serial quant B-hCG that do not double q 1-2 days & TVUS
-Tx: methotrexate (disrupts cell multiplication) w/ B-hCG monitoring for ≥15% drop OR laproscopic salpingotomy or salpingectomy + RhoGAM if Rh-
MTX can be given in single/double or multiple doses (4) w/ Leucovorin (med to help protect against harmful s/e of MTX)
-single/double dosing: monitor B-hCG on days 0, 4, 7 for a ≥15% drop
-multiple dosing (4 doses): monitor B-hCG on days 0, 1, 3, 5, 7 until ≥15% drop on 2 successive draws
what are the indications/contraindications for giving MTX to tx an ectopic pregnancy?
-indications: hemodynamically stable, early gestation <4 cm, B-hCG <5,000, no FHT (fetal heart tones)
-contraindications: ruptured ectopic, h/o TB, B-hCG >5,000, +FHT, noncompliant pt
Dx/Tx? severe unilateral abdominal pain, dizziness, N/V, signs of shock (syncope, tachycardia, hypotension), vaginal bleeding, cervical motion tenderness, adnexal mass, US showing absence of gestational sac, hCG that isn't doubling q1-2 days
-ruptured ectopic pregnancy
-Dx by serial quant B-hCG (check for doubling) and TVUS
-Tx: laparoscopic salpingostomy to remove ectopic gestation- may need salingectomy; RhoGAM if Rh-
an incompetent cervix/cervical insufficiency is painless dilation and effacement of the cervix usually occurring in the ____ trimester and puts the fetus at risk for...
-2nd trimester
-infection (fetal membranes exposed to vaginal flora)
-trauma/rupture of membranes
cervical incompetence causes ~15% of all 2nd tri losses
what are the RF for cervical incompentence/cervical insufficiency?
-MC is prev surgery or cervical trauma
-previous D&C
-LEEP (loop electrocautery excisional procedure)
-cervical conization
-congenital abnormality of cervix (from diethylstilbestrol/DES exposure in utero)
how is incompetent cervix/cervical insufficiency differentiated from preterm labor?
Dx by pelvic exam or US but preterm labor has contractions while cervical insufficiency has only mild cramping caused by cervical dilation
how is cervical incompetence treated?
-in previable pregnancies (<24 wks GA) elective termination an option
-betamethasone to inc fetal lung maturity
-strict bed rest
-cerclage (suture cervix shut)
Dx/Tx? sudden onset painless bright red vaginal bleeding in the 3rd trimester with nml fetal heart tracing; on PE soft, non-tender uterus
-dx: placenta previa (diagnose by pelvic US- DO NOT do pelvic exam)
-tx: hospitalization for stabilization, bed rest, tocolytics (magnesium sulfate) to inhibit uterine contraction, amniocentesis (to assess fetal lung maturity and give betamethasone if needed), delivery when stable (if L:S >2 aka lungs matured, >36 wks gestation, blood loss >500mL) vaginal if partial or marginal placenta, c/s if complete
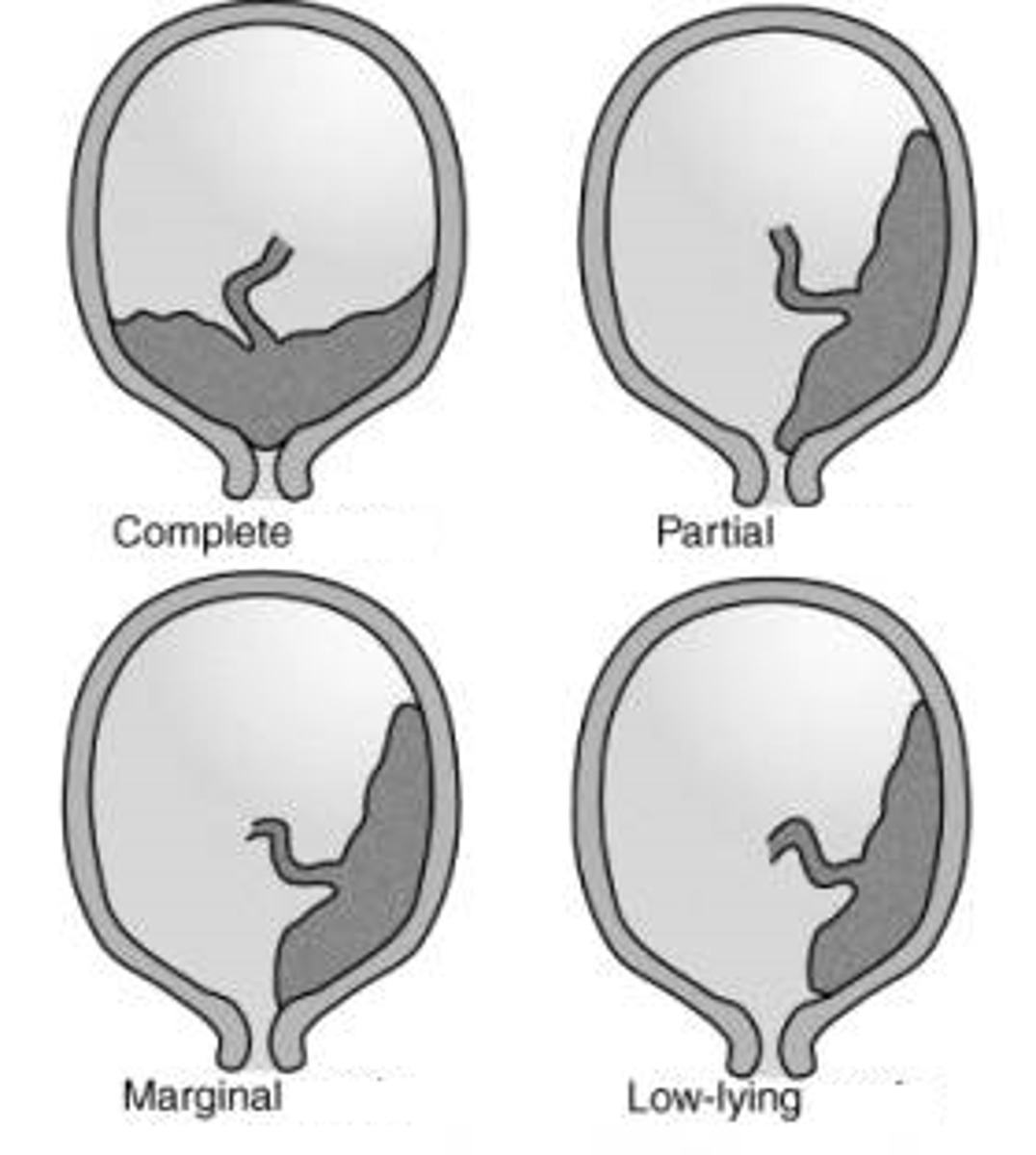
what are the differences b/t marginal, partial and complete placenta previa?
-marginal- 2-3 cm of cervical os
-partial: covering cervix partially ahead of fetal presenting part
-complete: total coverage of cervical os
*can deliver vaginally w/ marginal or partial if fetus is matured but c/s indicated for complete placenta previa
what is the pathophysiologic cause of gestational diabetes?
-placental release of growth hormone, corticotropin releasing hormone & human placental lactogen (HPL)
-these antagonize insulin (works similar to growth hormone as a counterregulatory hormone increasing glucose availability for the growing fetus)