SOCL 4451: The Sociology of Medicine Exam 1
1/79
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
80 Terms
confirmation bias
What is the tendency to search for, interpret, favor, and recall information in a way that confirms or supports one’s prior beliefs and values
The Enlightenment
What intellectual movement occurred in the 17th and 18th century?
emphases: reason, skepticism, tolerance of free speech, individual freedom
Key figures: John Locke, Isaac Newton
scientific inquiry based on the principles of this movement
Employer, individual purchase
What are the different sectors of the private healthcare insurance system in the U.S.?
employer (56%)
What type of insurance accounts for a majority of the American Healthcare system?
Medicare, Medicaid and CHIP, Veterans Affairs, Tricare, and Indian Health Service
What are the different sectors of the public healthcare insurance in the U.S.?
17%
What percentage of the U.S. population are covered through Medicare?
20%
What percentage of the U.S. population are covered by Medicaid and CHIP?
9%
What percentage of the U.S. population is uninsured?
32-41%
What percentage of people in Louisiana are covered primarily by Medicaid program?
Healthy Louisiana
________ is the primary Medicaid program in Louisiana that has different private health plans that help manage care benefits.
private health plans include
Aetna
Amerihealth Caritas Louisiana
United Healthcare Community Plan
Amerigroup Louisiana
Louisiana Healthcare Connections
economic resources, social and political values, and historical experience
The implementation and policies regarding Medicaid reflects the national….
critical junctures
_____ are situations of uncertainty in which decisions of important actors are casually decisive for the selection of one path of institutional development over other possible paths.
many healthcare systems for different countries were set in stone after WWII
different points in history where lots of decisions are made at once and its really difficult to go back and change your mind.
path dependency
______ is a situation when a system or organization follows one possible path such that others become more difficult to adopt.
economic and military power and political stability
Europe developed their Health Services in the late 19th century (1800s) and expanded them gradually. Many Europeans receive comprehensive health insurance for all citizens of any income. What were their motivations?
80%
Greater than ____ of all health costs in the EU financed from public sources like direct or consumption tax. (does not include UK and Norway)
11% :: 17%
Europe expenditure on healthcare: ______ GDP :: U.S. expenditure on healthcare: ______ GDP
United States Model
What model is a mostly private health care system with public insurance and for-profit private insurance but no universal coverage?
profit → unique part of system
some public insurance: most covered privately
low regulation of prices → lack of changes in prices
no individual mandate to have health insurance
Bismarck model
What model is a mostly private healthcare system with both private and public insurance?
ex. Japan, Germany, Netherlands, Switzerland, Belgium, France, US full-time workers <65
multi-payer system
payers generally private
funding: employer/employee tax, premiums, general tax
mostly non-profit but some for-profit
providers are generally private
doctor’s office → private business
Beveridge model
What model is a mostly public healthcare system with public insurance (and some private) with universal coverage?
payer typically the government
single payer* but also room for private insurance so has government and private payers
funded: taxes
supplemental private insurance (want private room/ faster waiting times)
fee or minimal cost at point of service
providers typically public but some private
regional administration; different administrations per area
non-pure single payer systems
ex. Great Britain, Italy, Spain, Nordic
Pure: Cuba, US Veterans Affairs, and Indian Health Service
tight regulations → strong individual mandate for health insurance
strong (complete) government control of medical procedures and prices
National Health Insurance Model
What system is a mix of the Bismarck and Beveridge model?
payer: public insurance
national or regional
funding: everyone pays into
providers: typically private (main difference from Beveridge model)
ex. Canada, South Korea, Taiwan, Australia*, US Medicare/Medicaid/CHIP/Tricare
Australia → required to have insurance, 60% of hospitals are public, and ½ of population has private insurance to control their healthcare experience
in some places private is allowed to compete with public insurance → private insurance market for certain types of services
mostly private hospitals and doctors, more flexible, public/ quasi public, pay premiums directly to healthcare
What makes the National Health Insurance model different from the Beveridge model?
Beveridge
majority/ almost all public hospitals
doctors paid by government
less flexible
paid out of general taxes → part of national budget
Tommy Douglas
Who is known are the “father of Medicare” in Canada because he created the 1962 law in Saskatchewan?
faced a lot of backlash, had privatized system prior (path dependency)
people who were upset: healthcare insurance agencies, members of public, and doctors
American Medical Association also opposed and did not want pay cut
1971
When was Medicare enacted in all of Canada?
Out of Pocket model
What model has no mass medical care system with some private and public insurance and care with no universal coverage?
urban with economic means/well-connected: private insurance/ pay directly for reliable care
public/charitable care options may exist; significant access and quality issues
may have untrained doctors practicing without proper safeguards
much of the population has little access and insufficient means
ex. Cambodia, India, Central African Republic, uninsured in U.S.
rising costs, aging populations, acute shocks
What are some of the challenges to healthcare systems worldwide/ external issues to the U.S.?
high prices, national spending, medical debt/bankruptcy, and uninsured going without care
What are some of the serious problems in the U.S. internal to the system?
provider services (prices are sky high and unregulated), provider administrative activities, and provider salaries (specialties are paid higher)
What are the top problems/ contributors of U.S. healthcare spending?
sources of U.S. healthcare spending
What are these sources contributing to?
provider services: high prices that are unregulated
provider administrative activities
provider salaries: specialists are paid higher
insurance administrative activities
prescription drug costs
medical technology/equipment: providers adapt newest tech
for-profit element: maximize return to share holder
utilization: we have a high level of people using system
comprehensive benefits, innovation in payment, chronic care coordination, mental health care, innovation in care delivery, and access to innovative drugs
What areas is the U.S. good at compared to other healthcare systems? (there are 6)
social factors
Only about 10% of contribution to premature death comes from health care. What accounts for the largest portion of contribution (60%)?
includes: social circumstances, behavioral patterns, environmental exposure
medical sociologist
_____ study the social factors that shape health. The American public generally recognizes the idea that social factors influence health.
minimized
In behavioral medicine, public health, and epidemiology, social factors are _____ with the exception of stress.
thought of as an indirect, secondary cause of illness
exposure, susceptibility, and disease course/ outcome
How do social factors shape health?
social factors have a direct causal effect on health
social conditions are needed to bind a person to the disease → therefore, causal
smoking
What is associated with more diseases than any health-related lifestyle behavior?
10 years shorter life expectancy
rates have declined
45% 1950s → 20% recent decades
Low SES people are more likely to participate
occupation, education, social network, income, and general wealth
becoming a smoker, continued smoking, regular smoker, addicted smoker, and smoking cessation
What are Hughes 5 stages of smoking?
start to finish of the behavior are social
biomedical model
What model states that every disease has a specific pathogenic origin whose treatment can best be accomplished by removing or controlling its cause using medical procedures (e.g., a drug)?
ex. measles line graph → shows that availability of drug/vaccine declines disease rates
limits for addressing chronic disease
limited access
social conditions and behaviors
epidemiological transition
What theory claims that there is a replacement of infectious disease with chronic diseases as major threats to health?
age of pestilence and famine, age of receding epidemics, and age of degenerative and human-made diseases
What are the three ages of the epidemiological transition theory?
early times to 1800s
At what time did the age of pestilence and famine occur?
infectious and parasitic diseases
1800s to 1960s
At what time did the age of receding epidemics occur?
better living conditions and medical treatment
infectious and parasitic disease are controlled
1960s to present
At what time did the age of degenerative and human-made diseases occur?
availability of resources and treatment now killing us
less exercise required now but that can lead to other issues
chronic disease
social factors become more prominent
possible 4th stage “age of mixed causes”
chronic and emerging infectious disease
experience of illness, social patterning of population health and disease, and causation of health and disease
What do social factors of health impact?
social determinants of health
What is the condition in which people are born, grow, work, live, and age, and the set of forces and systems shaping the conditions of daily life (WHO)?
social factors → causation of health and disease
fundamental cause theory
What theory says that social conditions can be fundamental causes of disease and mortality?
by Link and Phelan
impact multiple diseases, impact through multiple pathways, occurs over time, and affect access to health-protective flexible resources
What are the 4 criteria a cause must meet to be considered a fundamental cause by the FCT?
social conditions
What are factors that involve a person’s relationship with other people?
flexible resources
_______ are broadly useful across times and places.
when a new risk emerges, or a new protective factor is discovered, they shape who benefits and who is harmed
can limit choices (avoid risks)
can expand choices (health promotion)
individual people use resources to get healthy outcomes
resources can provide access to salutary contexts
ex. neighborhoods, occupations, marriages
collective health agency
What is the collective resource pooling when people in such contexts push for good circumstances in the context called?
ex. good schools, safe parks, reduced crime, good medical facilities
socioeconomic status
What has been a particular concern to the fundamental cause theory?
checks all the fundamental cause boxes
we have an education gap in life expectancy
widening gap
widening from Bachelors degree improvement and non-Bachelors degree stagnation
unit of analysis
What is the entity being studied called (ASSR)?
most common is people
families, high schools, corporations, religious congregations, cults, governments, counties, nations, or people
What are some different types of units of analysis (ASSR)?
ecological fallacy
What occurs when a researcher incorrectly concludes that ecological or contextual factors directly influence individual-level experiences, where group-level data are used to make claims about individual-level processes (ASSR)?
using data from one type of unit to draw conclusions about another type of unit
use data/observations from one level to draw conclusions based on that level of analysis only
To avoid the ecological fallacy, researchers should… (ASSR)
the health care system, health behaviors, and the built environment
What are the three explanations as to why the U.S. population health has fallen so far behind its high-income counterparts thought of as proximate determinants of health (HH3)?
social inequality, social policy, and culture
What are the three distal reasons that the US population health has fallen behind its high-income counterparts (HH3)?
health care system and health behaviors
Emphasis on these two proximate determinants of health in research are due to being easier to compare and measure across countries rather than explain the argument that health care and behaviors are more important than structural determinants. What two factors are often focused on in research literature (HH3)?
not providing universal, publicly funded system of health care
Why is the United State unique among high-income countries (HH3)?
Veterans Health Administration
What system in the US is similar to the UK’s National Health service that is government-run, funded through taxes, that provides care to all British citizens (HH3)?
Medicare, Medicaid, and the Children’s Health Insurance Program
What U.S. health system is similar to Canada’s national health insurance program that pays for health care from private providers for all Canadians (HH3)?
socioeconomic status (SES)
What are differences between individuals and groups in the possession of highly valued societal resources, most importantly educational attainment, occupational status, income, and wealth called (HH5)?
social class
What Marxist based idea is based upon an individual’s relationship to the means of production (HH5)?
economic status, social standing, and political power
What are the three important components of social stratification outlined by Weber (HH5)?
health and longevity
Weber developed the idea that individuals actively utilize their class, status, and power to improve their “life chances.” What are two critical components of life chances (HH5)?
educational attainment
What is the most often-utilized measure of socioeconomic stats in the U.S. studies of population health?
because it does typically does not change when individuals experience declines in their physical or mental health
False
Individuals who have a low income or who live in a household with low income simply have far greater monetary resources to protect their health (HH5). T/F
material; psychological
Individuals may experience poorer ______ conditions when living with low income, but also individuals who have low income while living in a wealthy society may also experience poorer ________ conditions of relative deprivation when comparing themselves with their wealthier counterparts (HH5).
wealth
Which is more unequally distributed in American society, wealth or income?
no wealth
15% of U.S. families have ______.
$40,000
40% of American families have less than ________ in wealth.
inequality
Since the 1970s, American social stratification have resulted in the highest-ever levels of income and wealth ______ in American history.
de-unionization, changes in the way corporations are governed, tax policies favor high earners and the wealthy, and federal spending on income transfers has been redistributed away from the poorest people to those with higher incomes
What specific institutional changes and circumstances have led to such widening in the U.S. distribution of income and wealth in recent decades?
True
The United States is experiencing the widest gap in SES disparities in key measures of population health ever documented. T/F
1980s
When did the association between health and education become strong?
the accumulation of socioeconomic resources across the life course
Why do the SES differences in health tend to be small in young adulthood but grow larger in middle adulthood and early old age?
childhood and adult SES
What are important predictors of old age functional health in the United States?
relationship between socioeconomic status and health
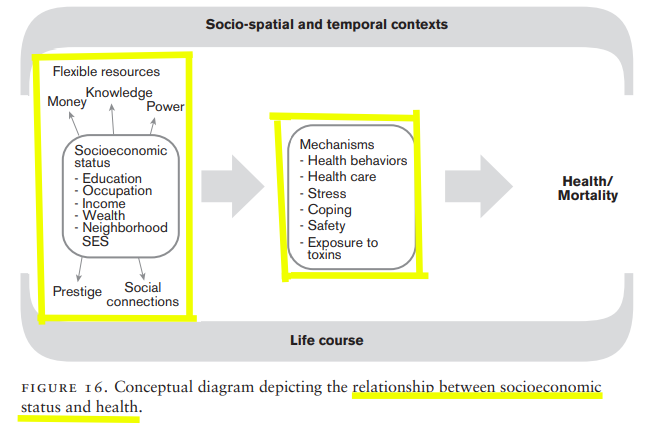
the issue of multiple mechanisms
Why is a policy or programmatic focus on single mechanisms not enough to reduce or eliminate SES disparities in health?
technological advances, rapid availability of health-enhancing information, and advanced medicine giving humans more control over health
Why have social factors like SES become especially more important in modern societies?
it could be genetics, family background, or infant and child health characteristics
What are some critiques of using SES as a fundamental cause of population health or other reasons for the strong-association between SES and health over the life course?
researchers cannot use experimental designs in this area of study
Why is the scientific work on the causal effect of SES on health extremely difficult?