Infection Control + Disease in Acute Care
1/78
Earn XP
Description and Tags
DPT 5025
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
79 Terms
Nosocomial Infection/Hospital Acquired Infections (HAI)
Infections that occur while receiving health care, developed in a hospital or other health care facility that first appear within 48 hours or more after hospital admission, or within 30 days after having received health care.
Incidence of HAI/Nosocomial Infections
Approximately 1.7 million infections each year
98,000 (1 in 17) associated deaths each year
Prevalence of Nosocomial/HAI Infections
Approximately 1 in 31 patients has at least 1 infection in association with their hospital care.
The overall direct cost of HAIs to hospitals ranges from $28 billion to $45 billion. While the range is wide, HAIs are clearly expensive.
Prevention– Nosocomial/HAI Infections
Simple infection-control procedures such as cleaning hands with an alcohol-based hand rub can help prevent HCAIs and save lives, reduce morbidity, and minimize health care costs.
Surgical Asepsis
Process or procedures to make an area free of microorganisms.
Medical Asepsis
Process or procedures to reduce the number and transfer of microorganisms.
In Physical Therapy, do we focus primarily on surgical asepsis or medical asepsis?
Medical Asepsis (clean procedure vs. sterile procedure)
Hand Hygiene
The use of alcohol-based hand rub (ABHR) or handwashing with soap and water is a simple yet effective way to prevent the spread of pathogens and infections in healthcare settings.
For Transmission of Infection to happen, what 3 things do you need?
A source, host, and means of transmission.
Source
Patients, Staff, Visitors, Equipment/Objects
Host
A person who serves as the home for the infectious agent.
What factors make a host susceptible?
Age
Medical status
Medications
Treatment
Open skin
Means of Transmission
This is where CDC recommendation are focused.
There will always be sources and hosts so controlling the transmission is the only way to break the chain.
Contact Transmission
Infection spread through direct contact with an infectious person or with an article or surface that has become contaminated.
Droplet Transmission
Infection spread through exposure to virus-containing respiratory droplets (larger and smaller droplets and particles) exhaled by an infectious person.
Droplet Transmission is most likely to occur when?
When someone is close to the infectious person, generally within about 6 feet.
Airborne Transmission
Infection spread through exposure to those virus-containing respiratory droplets comprised of smaller droplets and particles that can remain suspended in the air over long distances (usually greater than 6 feet) and time (typically hours).
Two Tiers of Isolation
Standard Precautions and Transmission Based Precautions
Standard Precautions
Precautions applied for ALL patients regardless of diagnosis, known or presumed infection status.
Replaces universal precautions
What are Standard Precautions Based on?
The principle that:
All body fluids (blood, secretions, excretions except sweat), non intact skin, and mucous membranes MAY contain transmissible infectious agents.
Standard precautions protect both patient and healthcare provider (HCP)
Standard Precaution Practices
Hand Hygiene (handwashing, antiseptic hand wash, antiseptic hand rub or surgical hand antisepsis)
PPE (depending on anticipated exposure)
Gloves– when in contact with bodily fluids or the risk for contact is great
Gowns– when the skin or clothing is at risk for contact
Mouth, nose, eye protection
Respiratory hygiene/cough etiquette
Safe injection practice
Cleaning of contaminated equipment
Transmission Based Precautions
Used with specific patients who are known to be or are suspected to be infected with pathogens that are highly transmissible and need special precautions BEYOND standard precautions.
What are the 3 types of Transmission Based Precautions?
Contact
Droplet
Airborne
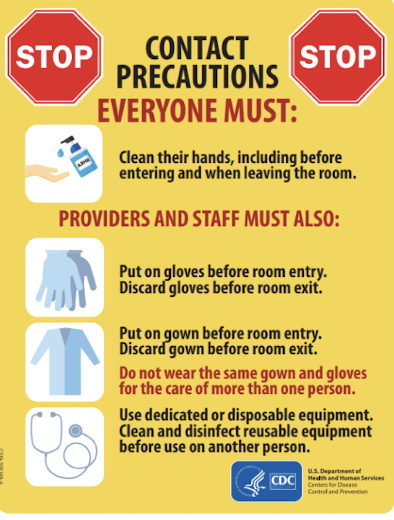
Contact Precautions
Used when patient has an infection that spreads through direct contact with an infectious person or with article/surface that has become contaminated (MRSA, C Diff)
Contact Precaution Practices
Standard Precautions PLUS
PPE (gloves, gown) when touching patient skin or equipment near patient
Limit transport– cover open area if necessary
Clean equipment
Dedicated equipment
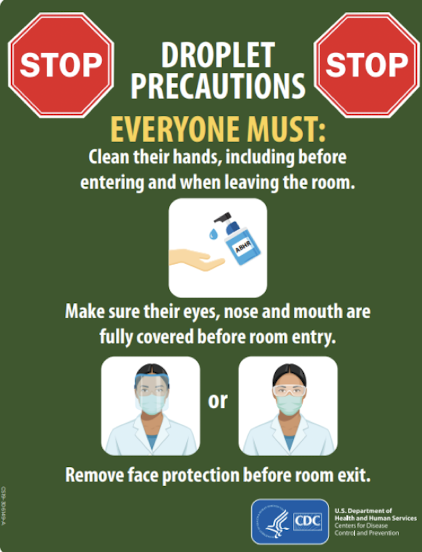
Droplet Precautions
Used when patient has an infection spread through exposure to virus-containing respiratory droplets exhaled by an infectious person.
Transmission is most likely to occur when someone is close to infected person (around 6 feet)
Influenza, cold, pertussis, rubella, mumps
Droplet Precaution Practices
Standard Precautions PLUS
Mask (and eye protection)– before entering room
Limit transport– mask patient; cough hygiene
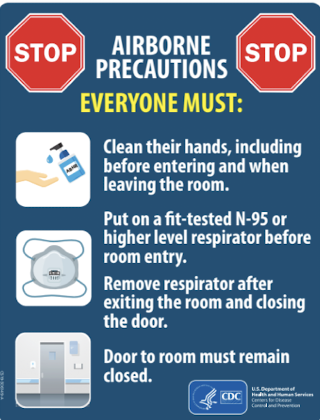
Airborne Precautions
Used when patient has an infection spread through exposure to those virus-containing respiratory droplets comprised of smaller droplets and particles that can remain suspended in the air over long distances (usually greater than 6 feet) and time (typically hours).
Chicken pox, TB, Measles, Shingles (also contact)
Airborne Precaution Practices
Standard Precautions PLUS
Fit-tested mask, N95, respiratory
Patient in negative pressure room– Airborne Infection Isolation Room
Limit transportation; Patient wear mask during transport
What are the 4 most common sources of HAI?
Central Line-Associated Blood Stream Infections (CLABSI)
Catheter–Associated Urinary Tract Infections (CAUTI)
Surgical Site Infections (SSI)
Ventilator-Associated Events/Pneumonia (VAE/VAP)
Clostridium Difficile (C. Diff)
A bacterium that can cause symptoms ranging from diarrhea to life-threatening inflammation of the colon.
Escherichia Coli (E. Coli)
Leading cause of UTIs in hospitals; can cause gastroenteritis, pneumonia or neonatal meningitis.
Hepatitis A
Healthcare personnel infected when handling a patient in whom the infection is not yet recognized and is fecal incontinent or has diarrhea.
Hepatitis B
Can cause acute infections or chronic liver infections; can turn into chronic Hepatitis B, causing lifelong infection, cirrhosis, liver cancer, liver failure and death; spread in healthcare settings through contaminated needles, syringes, or other sharps.
Hepatitis C
Unlike HAV and HBV, there is no vaccine against HCV; mainly transmitted through intravenous drug use in the community, the healthcare setting sees HCV transmission through contaminated syringes, needles or sharps, infected blood transfusions and sometimes organ transplants that have not undergone adequate HCV screening.
Human Immunodeficiency Virus (HIV)
Transmission in hospitals is rare, it is possible to be spread to patients via improper infection control procedures, such as sterilization and disinfection; transferred through bodily fluids. I
Influenza
The influenza virus is common but variant strains often emerge; H1N1 strain, or swine flu, was one of the most recent deadly variants causing annual updated flu vaccines.
Methicillin-resistant Staphylococcus Aureus (MRSA)
A bacteria that is resistant to many antibiotics. Skin infections are most common but can lead to lung infections or sepsis if untreated. Non-intact skin is often the site of a MRSA infection. Usually spread by things that carry the bacteria (infected personal items). Injection of drugs in communities= staph infection.
Norovirus
Common cause of gastroenteritis; healthcare facilities optimal transmission spaces for the highly contagious virus, as the close quarters enable rapid person to person transmission; exhibits strong survival outside of a human host.
Pseudomonas Aeruginosa
One of the most common isolated pathogens in people hospitalized for more than one week; thrives on moist surfaces, heightening the risk of infection for patients with catheters or ventilators.
Staphylococcus Aureus
Normal part of the skin flora, and approximately 30% of people carry the bacteria in their nose asymptomatically; can be fatal when identified as the cause of sepsis, pneumonia, endocarditis, or osteomyelitis.
Myobacterium Tuberculosis
Causes tuberculosis; the disease is not very common in U.S; can be spread through the air.
Control of Transmission Primary Strategy
Standard and Transmission Based Precautions. WASH HANDS!
Chain of Transmission
Reservoir/Host
Pathogen
Portal of Exit
Transmission
Portal of Entry
Susceptible Host
Infectious Agent
The pathogen (germ) that causes diseases
Reservoir
Includes places in the environment where the pathogen lives (this includes people, animals and insects, medical equipment, and soil and water)
Portal of Exit
The way the infectious agent leaves the reservoir (through open wounds, aerosols, and splatter of body fluids including coughing, sneezing, and saliva).
Mode of Transmission
The way the infectious agent can be passed on.
Portal of Entry
The way the infectious agent can enter a new host (through broken skin, the respiratory tract, mucous membranes, and catheters and tubes).
Susceptible Host
Can be ANY person (the most vulnerable of whom are receiving healthcare, are immunocompromised, or have invasive medical devices including lines, devices, and airways).
Sources of Bodily Fluids
Urine (catheter, toileting)
Feces (colostomy, toileting)
Vomit
Naso/gastric fluid (from NG, PEG)
Blood (going in/out)
Mucus/Sputum (nasal, oral, trach)
Bile (T-tube)
Pleural (chest tube)
Sero-sanguinous (suction/drainage/collection systems)
Ventilator droplets (oral or trach)
Wound drainage
CSF
PT gym/multi-use patient area
Clean/dirty signs
Dirty bin/area
Plastic gait belts
Mats/linens
Patient Care Units
Use dedicated gait belts or plastic gait belts.
Clean equipment before leaving room if possible (gait devices, oximeters, w/c, ankle foot orthosis)
PT Role in Patient Care
Know and follow facility infection control policy and procedures.
Identify if patient has transmission precautions, pathogen.
Identify sources of POTENTIAL nosocomial infections in each patient, take appropriate actions to prevent infection.
Observe all patients for signs and symptoms of infection. Notify RN/MD immediately.
Document
Tubes/Drains/Collection Devices
Draining fluids out: keep low to prevent return to body: chest tubes, Foley catheter
Have RN empty if too full to prevent spills (Foley, Jackson Pratt bulbs; JPs, osteomy)
Do not “push” or pull on lines or drains: can “dirty” it and introduce pathogens (CLABSI, CAUTI)
Feeding tubes: usually head of bed (HOB) up 30 degrees
When should you give a patient water, ice chips, or food?
NEVER unless you KNOW the patient can have them
Aspiration precautions
Strict NPO– unsafe swallow, procedure or test planned?
Specific diet (dysphagia- thickened, no straw, sit upright and chin tuck)
Alert enough
Hospital-Acquired Pneumonia (HAP)
Lower respiratory infection that was not incubating at the time of hospital admission and that presents clinically 2 or more days after hospitalization.
Pneumonia that presents sooner should be regarded as community-acquired pneumonia.
Ventilator-associated pneumonia (VAP) is defined as pneumonia that presents more than 48 hours after endotracheal intubation.
The most common cause of HAI deaths.
Hospital-Aqcuired Pneumonia (HAP)– Portal of Entry
Aspiration
Surgery
Endotracheal Intubation/Ventilation
Sick contacts
Hospital-Acquired Pneumonia (HAP) Precautions
Standard– always!
Contact– for multidrug-resistant organisms (MDROs)
Droplet– for some types of infection and/or if evidence
Best Practice– ALL
Seasonal Influenza
Spread from person to person primarily through large particle respiratory droplet transmission (cough or sneeze).
Transmission via large-particle droplets requires close contact between source and recipient persons; droplets travel only short distances (approximately 6 feet).
Indirect contact transmission via hand transfer of influenza virus from virus-contaminated surfaces or objects to mucosal surfaces of the face (nose, mouth) may also occur.
All respiratory secretions and bodily fluids are considered to be potentially infectious; however, the risk may vary by strain.
Seasonal Influenza Precautions
Standard + Droplet
Seasonal Influenza Prevention
Flu vaccine for all medical providers
Medical providers should not interact with patients when ill
Limit visitors to hospitals
Tuberculosis
Nosocomial/HAI transmission in U.S. is rare.
Carried in airborne particles that be generated when person who have pulmonary or laryngeal TB disease cough, sneeze, should, or sing.
Particles can stay airborne for prolonged periods and spread throughout a room or building.
Usually transmitted only through air, not by surface contact.
Tuberculosis Precautions
Standard + Airborne
N95 masks and negative air pressure room
HIV/AIDS
Nosocomial/HAIR transmission in U.S. is rare
Standard precautions
Methicillin-resistant Staphylococcus Aureus Bacteremia (MRSA Bacteremia)
A bacteria that is resistant to many antibiotics.
Skin infections are most common but can lead to lung infections or sepsis if untreated.
Non-intact skin (abrasions or incisions) is often the site of an MRSA infection
MRSA is usually spread in the community by contact with infected people or things that carry the bacteria. This includes through contact with a contaminated wound or by sharing personal items, such as towels or razors, that have touched infected skin.
The opioid epidemic may also be connected to the rise of staph infections in communities. People who inject drugs are 16 times more likely to develop a serious staph infection.
How does MRSA present?
A bump or infected area on the skin that might be
red
swollen
painful
warm to the touch
full of pus or other drainage
accompanied by a fever
often confused as a spider bite
MRSA Precautions
Standard + Contact
Clostridium Defficile Infection (C. Diff)
A bacterium that can cause symptoms ranging from diarrhea to life-threatening inflammation of the colon; up to 7 liters with up to 5 bouts/day!
Most commonly affects older adults in hospitals or in LTC facilities and typically occurs after the use of antibiotic medications.
Annually, about half a million people get sick from C. difficile in the US.
Recurrent C. Difficile infections are on the rise.
It is resistant to many routine cleaning products, including alcohol-based hand cleaners, so it is able to survive in clinical locations for extended periods of time, so use SOAP and WATER.
Precautions for C. Diff
Standard + Contact
Hand washing with soap and water vs. hand sanitizer recommended especially during an outbreak.
Varicella Zoster Virus– Shingles (Herpes Zoster)
The virus that causes shingles, varicella zoster virus (VZV) can spread from a person with active shingles and cause chickenpox in someone who had never had chickenpox or received chickenpox vaccine.
VZV spreads through direct contact with fluid from the rash blisters.
A person who has active shingles can spread the virus when the rash is in the blister phase; not infectious before blisters appear.
One rash crusts, you are no longer infectious.
Precautions for Varicella Zoster Virus– Shingles
Standard + Contact (if rash is present)
Airborne (to prevent spread of chicken pox virus)
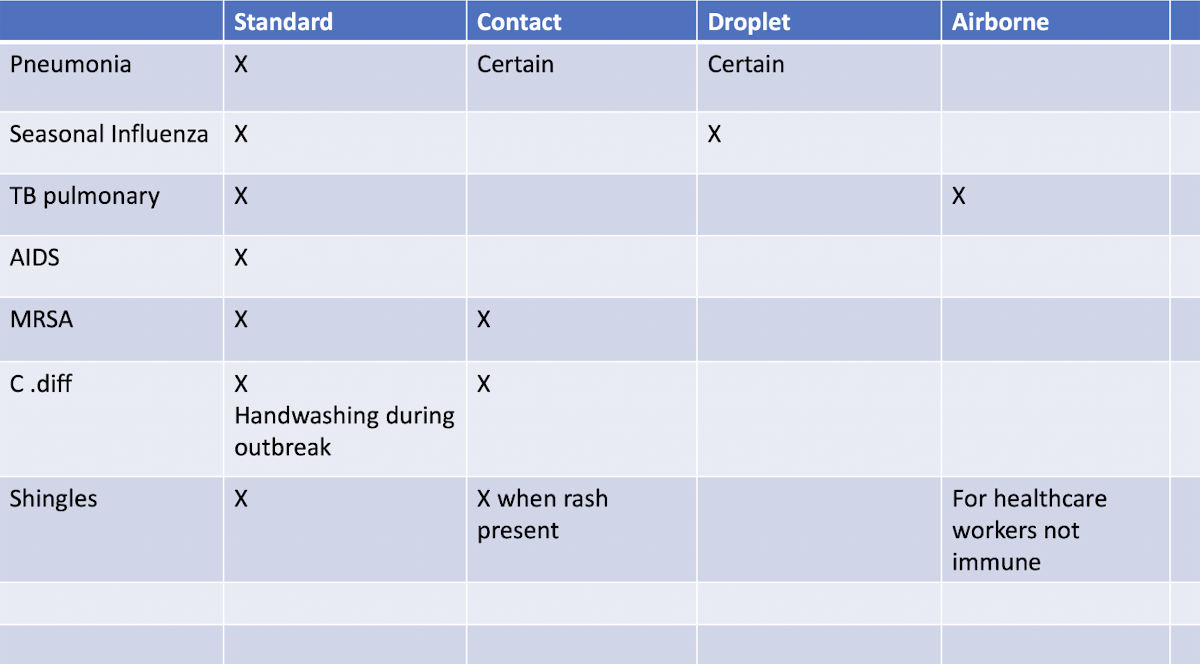
Chart!
What does not ever require Airborne precautions?
C-Diff
Environment where the pathogen lives
Reservoir
MRSA, C-Diff, and Shingles with a rash all require which type of precaution?
Contact
True or False: Shingles and chickenpox are both caused by the Varicella Zoster virus.
TRUE
Chickenpox is spread via Airborne and Shingles is spread via contact.
TRUE
What do droplet precautions include?
Standard precautions plus mask and eye protection.