Molecular and cellular disorders
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
45 Terms
Nucleotide (3)
Polynucleotide (4)
DNA replication (4)
DNA compaction (4)
monomer (sugar, phosphate, nitrogenous base)
complementary base pairing joins stands to form DNA (adenine-thymine, guanine-cytosine, hydrogen bond between bases)
Cell cycle synthesis, parental stand as template, new strands synthesised, daughter molecule one old one new stand (semi-conservative replication)
DNA, around histones, folding to chromatin, folds to chromosome
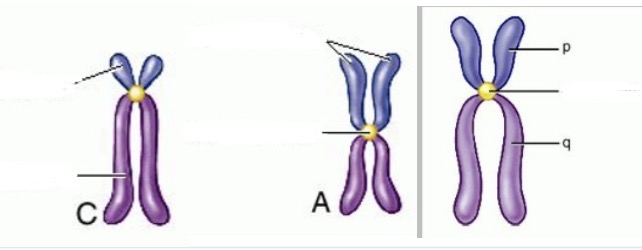
Chromosomes (5)
Dog, Cat, Cow
Compact, protects DNA from damage, organisation and structure, efficient transmission during cell division, each pair has same banding latter and centromere position
Dog 39 pairs (78), Cat 19 pairs (38), Cow 30 pairs (60)
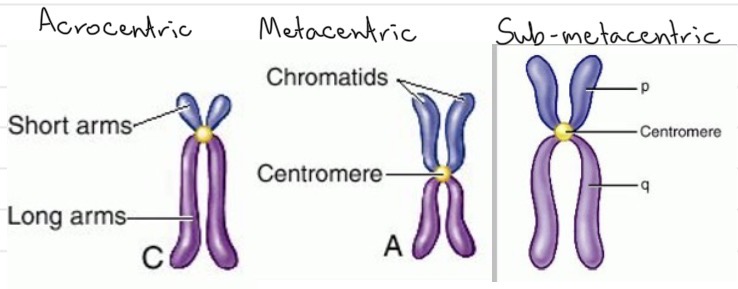
Karyotype
Cytogenetics
Aneuploidy/ Trisomy/ Monosomy
All chromosomes arranged in pairs based on length from longest (consistent comparisons)
Detection and interpretation of chromosomal abnormalities, changes to chromosome number or structure, associates with physical or mental abnormalities
Dif number of one chromosome/ one additional copy of one chromosome/ one copy of one chromosome
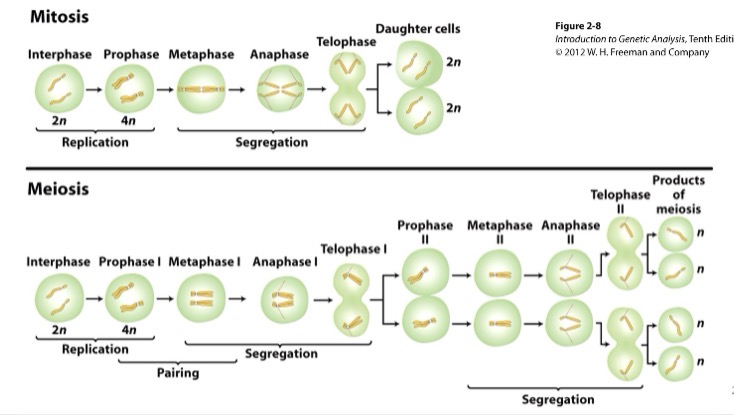
Mitosis
Meiosis
Genome
Genetic mutations
Phenotype
Genotype
Complete set of genetic material found in an organism, includes nuclear and plastid DNA, contains coding and non-coding DNA
Are permanent and heritable changes or disruptions in the base sequence of the genome that alter the expression/structure/function of the coded protein
Clinical manifestation of specific gene
Specific combination of alleles an individual has
Aspects at which faulty genes cause disease (central dogma) (5)
DNA replication
Transcription (exons)
Translation
Additional elements affecting successful expression of gene (prior to gene in DNA)
Multiple transcription factors
Single gene disorders:
Factor VII deficiency (FVIID)
clotting disorder, results in mild breeding episodes and bruising
Lack of proconvertin (clotting factor 7)
Gene mutation (GGA to GAA), glutamic acid (not glycine) in exon 5, polypeptide altered, change in EGF2 domain structure, reduced function (interacts with tissue factors in coagulation cascade)
Mendelian inheritance:
The law of segregation
Law of independent assortment
Genetic linkage
Sex chromosomes
Organisms inherit two alleles for each characteristic from each parent, two alleles for each characteristic segregate at gamete production
Inheritance pattern of one trait will not affect the inertiance pattern of another
Tendency of DNA sequences that are close together on a chromosome to be inherited together during meiosis
Gene located on differential regions of sex chromosome (most on X), pseudoautosomal region (allows correct lining up) and differential regions (not found on other sex chromosome)
Codominance
Incomplete dominance
Epistasis
Lethal alleles
Penetrant
Both dominant genes expressed, equally expressed
Neither allele is dominant, blended expression
Expression of one gene is affected by expression of one or more independently inherited genes
Essential to life, one copy of recessive lethal allele is survival with defects, two recessive or dominant lethal alleles is death
Proportion of individuals with genetic variant/mutation who exhibits signs and symptoms of genetic disorder
Chromosomal mutation (4)
DNA replication mutation (3)
Spontaneous/ Induced mutation
Point mutations (substitution 3, insertion/ deletion)
Deletion, duplication, inversion, translocation
Mistakes in DNA replication base pairing (proofreading and post-replication mismatch repair to increase accuracy)
Occur in natural environment without addition of mutagens at low rate/ created by addition of mutagens
Alters sequence of bases within genes
-One base changed to another
-Missense mutation (mutated codon for incorrect amino acid)
-Nonsense mutation (mutated codon for stop codon)
-Silent mutation (amino acid sequence not affected)
-Adding or removing once base, inappropriate number of bases in a DNA sequence, affects reading frame onwards (frame shift mutation, function affected)
Canine haemophilia B
Bovine leukocytes adhesion deficiency (BLAH)
Hyperkalemic periodic paralysis (HYPP) horses
Porcine stress syndrome/ malignant hyperthermia
X-linked tremors/ shaking puppy syndrome
Sex linked recessive missense mutation, substitution of A for G at nucleotide 1477, reduced coagulation
Autosomal recessive missense congenital disease, substitution of ITGB2 gene on chromosome 1, leukocytes can’t emigrate to sites of injury from circulation
Autosomal dominant congenial disease, substitution in SCN4A gene, episodic electrical inexcitability and paralysis of skeletal muscle as sodium channels effected
Missense mutation in ryanodine receptor gene
Missense mutation in preteolipid protein gene, coarse tremors of the head and body, lack of myelin in CNS
Mutagens:
Physical (3)
Chemical (3)
Biological (3)
Effects (6)
Radiation, UV light, x rays
Base analog (similar to nucleotide), Base altering agents (induce methylation, alkylation or deamination of DNA bases), Intercalating agents (similar to base pair heterocyclic ring)
Transposons and insertion sequences, viruses, bacteria
Direct DNA or nucleotide damage, induce cross-linking (bases which shouldn’t link), break chromosomes, break DNA strand (single or double), base deletion, nucleotide dimers (same bases joined if closed together)
Types of mutations:
Somatic (3)
Germ-line (3)
In non-reproductive cells, may not be manifested, can result in cancer if altered cell division patterns
In gametes or reproductive cells that produce gametes, heritable, transfer to next progeny in all cells
Types of alleles (4)
Homozygous dominant AA
Heterozygous A (carriers)
Homozygous recessive aa
Hemizygous (males for sex linked chromosomal disease as they can only have one X copy)
Modes of inheritance:
Autosomal recessive
Autosomal dominant
X-linked recessive
X-linked dominant
Two copies for presentation, asymptomatic carrier parents, 25%/ 1 in 4 affected offspring probability, can skip generations, Myoclonic epilepsy in Rhodesian ridgebacks (defective DIRAS1 gene, longer AA sequence bc of stop loss)
One copy needed for presentation, often lethal if two copies present, no generation skipping, defective product usually structural protein, Polycystic kidney disease in Persian cats (point mutation in PKD1 gene on chromosome 3)
Consider which parent has abnormal gene, females only express if abnormal from both parents, female carriers if one, males affected if recessive allele present from mother, Haemophilia A and B (coagulation cascade factors 9 and 8)
Consider which parent has abnormal gene, females affected unless homozygous recessive, males affected if dominant allele present
Genetic mosaicism
X inactivation
Pedigree
Mode of inheritance using pedigree
Mutation during embryogenesis, amount and location of mosaicism determined by timing and lineage of affected somatic cells
Random inactivation of X chromosome alleles post division, leaves two different alleles active, Tortoiseshell coat in female cats
Chart of genetic history of related individuals over several generations, used to predict likelihood of disease progeny, determine mode of inheritance and probability of affected offspring for given gross
X linked disorder (mostly males effected), Autosomal disorder (even between males and females), Dominant (one parent must have disorder), Recessive (neither parent has disorder)
Inborn errors of metabolism
Result of single gene disorders
Cellular metabolism has many enzymatic pathways (cascade or inhibition) with many steps, each requires enzyme or protein with specific function
Non-functional proteins stops pathway, results in product accumulation, may have toxic effects
Citrullinemia (single gene disorder):
Clinical signs
Cycle effected
Mutation
Effects
Clinical sings 1-4 days (blindness, depression, convulsions, head pressing)
Urea cycle (liver converts ammonia to urea for excretion vis kidneys), ASS enzyme converts citrulline to argininosuccinate
Substitution of T for C on first position of 86th triplet, nonsense mutation (stop codon) terminated at 85th AA, ASS not functional
Autosomal recessive disease, carriers have 50% ASS activity compared to normal, affected have 0% ASS activity, buildup of toxic ammonia in blood
Ehlers-Danlos syndrome (single gene disorder):
Clinical signs
Structure
Mutation
Born with stretchy or very fragile skin
Collagen fibres form from triple-helix pro-collagen, requires enzymatic modification to form mature functioning collagen, contains a-1 chains and a-2 chains, coded for by separate genes, pro-collagen forms collagen by removal of terminal AA
Mutation can occur in a-1 collagen chain gene, a-2 collagen chain gene, PCP-C-1 endopeptidase gene, PCP-N-1 endopeptidase gene
Genetic heterogeneity:
What (2)
Example
Specific set of clinical signs arises from more than one mutation
More than one mutation in the same gene that causes the same clinical effects
Ehlers-Danilo’s syndrome (dominant if mutation in chain genes, recessive if mutation in endopeptidase genes)
Progressive retinal atrophy PRA: Progressive Rod-Cone Degeneration PRCD(single gene disorder):
Clinical signs
Structural change
Mutation
Diagnosis
Late onset age varied between breeds, night blindness to total blindness
PRA causes retinal cells to degenerate and die, initial loss of rods then cones
Autosomal recessive, mutation in PRCD gene, G to A at chromosome 9
Genetic tests, ophthalmic evaluation after first clinical signs, electroretinography (ERG) very sensitive indicator of PRA
Neoplasia
Carcinogen
Angiogenesis
Metastasis (4 types)
Heterogeneity
Uncontrolled cell growth/ cell cycle leading to neoplasm/tumour, preventative strategies avoided, occurs in any tissue type/ body system in body system
Substance capable of causing cancer or promoting cancer in living tissues, increase risk, causes DNA damage causing mutations leading to cancer
Secretion of growth factor to stimulate blood vessel growth to supply tumour cells, anti-angiogenic signalling overwhelmed by pro-angiogenic signalling
Malignant cells transfer to another part of body, acquisition of invasive phenotype, in circulation (to organs with large blood supply), in lymphatic drainage system (seed in lymph nodes), extension (to neighbouring organ via direct contact), transplantation (exfoliation of tumour cells into a cavity or another site)
Evolution of tumour to form different clonal stem cell lines, additional mutations (resulting in dif genotypes and phenotypes of cancer cells), selection pressure (cancer drug introduction results in resistance due to new genotype)
Control of cell cycle:
Cell response
Checkpoints
Inhibitory proteins
Stimulating proteins
Other protein
Divide/ stop dividing , differentiate, die as response to molecular signals
G1 cell size (rest or divide), S (DNA ok), G2 size and organelles (fully equipped), M (lined up), progression regulated
P53 tumour suppressor/ tumour suppressor gene, stops progression, allows repair time, triggers apoptosis
CDK-cyclins/ protocol-oncogene, activate or inhibit protein via phosphorylation, activate cell cycle stimulating proteins
DNA repair proteins, various genes
Tumour biology:
Mutation
Hyperplasia
Dysplasia
Anaplasia/ Carcinoma in situ
Metastasis/ Invasive carcinoma
Genetically altered
Rapid/ uncontrolled cell division
Abnormal change
Lose function, spread over wide area
Invades normal tissue, enter blood and lymph, metastases form in other sites
Benign tumour/ neoplasms (what, 2 examples)
Malignant tumour/ neoplasms (what, 2 examples of each)
Mast cell tumours
Leukemias
Myelomas
Localised, slow growth/ few mitosis figures, circumscribed/ encapsulated, resemble original tissue, -oma
-Lipoma (adipose cells), Fibroma (fibrous connective tissue)
Invade and metastasis to other sites, rapid growth/many mitosis figures, non encapsulated, don’t resemble original tissue (anaplastic), -carcinoma (epithelial origin) -sarcoma (mesodermal origin)
-Transitional cell carcinoma (urinary tract), Adenocarcinoma (glandular tissue/ mammary glands), Osteosarcoma (osteoblasts), Lymphosarcoma (lymphoid tissues)
Mast cells, usually affects skin, contain histamine so highly reactive when irritated by handling
Hematopoetic cells in peripheral blood or bone marrow, cell lineage identification important step in classification of leukemia
Plasm cells/ terminally differentiated B lymphocytes, results in diffuse disease
Cancer hallmarks:
Original (6)
Emerging (2)
Enabling (2)
Sustained proliferation signalling, evading growth suppressors, enabling replication immortality, activating invasion and metastasis, inducing angiogenesis, resisting cell death
Avoiding immune destruction, deregulating cellular energetics
Tumour-promoting inflammation, genome instability and mutation
Polygenic traits:
What
Behaviour
Coat colour
Phenotype results from joint contribution of multiple independently acting or interacting genes
131 SNPs associated with breed differences in behaviour (genes expressed in brain with neurological function and developmental processes), owner aggression, stranger fear, trainability
Dif allele combinations from dif loci, dif promoter alleles drive dif colour patterns/ have mutations, action of one gene depends on action of another gene (ASIP gene causes pigment change from black/brown to yellow/white)
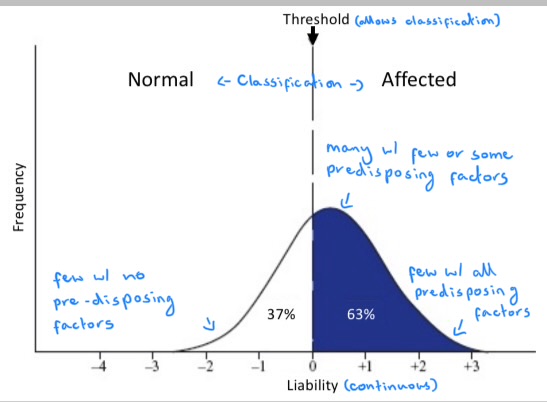
Multifactorial traits/ complex inherited disorders:
What
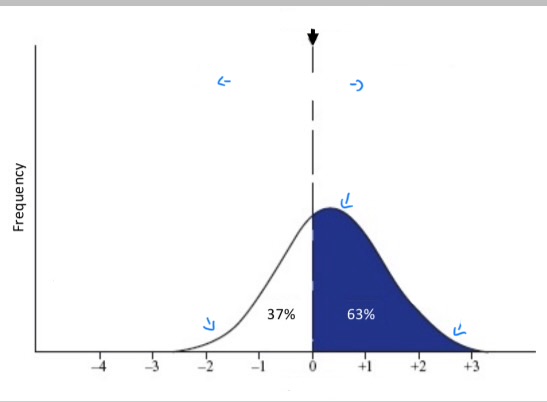
Liability (bell curve)
Hip dysplasia
Equine metabolic syndrome
Caused by multiple genes and influenced by environment, (Cancer)
Combined effect of all factors (environmental and genetic) that render animal more or less likely to develop that disorder
Hip dysplasia gene, food level, dietary electrolytes, exercise level, subjectivity of radiographs
Insulin dysregulation genes (dominant, multiple, reduced penetrance, possible epigenetic influences), obesity, dietary sugar, exercise, concurrent illness
Heritability:
What
Aspects (4)
Examples (3)
Non-genetic alleviation
Proportion of total variation in a trait that can be attributed to variation in genetic factors
Relative importance of genetic and environmental factors, contribution of each, heritability for liability usually greater than 0 (liability based on genes), selection for decreased liability can reduce incidence
Metritis in cows 5, Hip dysplasia in dogs 35, tibial dyschondroplasia in chickens 45
Inherited disorders can be alleviated by non-genetic means even when heritability of liability is high (restricted feeding, exercise during growing phase for hip dysplasia)
Metabolic disorders:
What
Triggers (4)
Effects (3)
Production diseases
Incidence around calving (2)
Disrupt homeostasis/ metabolic processes due to imbalances in key metabolites, acute and sudden onset, requires systemic correction
Sudden dietary changes, high nutrient demands, hormonal and physiological shifts, management practices
Reduced productivity, increased disease risk, reduced profitability
Metabolism can’t handle increased demand/ sudden change, conditions related to imbalances between rates of input of dietary nutrients and output of production
Rapid increase in late periparturient period, peak on parturition day, decline until day 7 of lactation (increased milk production); multiparous cows
Transition period physiology:
When
Prepartum changes (1, 3, 2)
last 3 weeks of gestation and first 3 weeks of lactation
Nutritional/ energy demand increased
Hormonal shifts: HPA
- uncoupling of somatotropic axis (prepartum decreased insulin; postpartum increased T4 and T3, supports lactogenesis)
-low insulin and insulin resistance (spare glucose prepartum and energy source postpartum)
-oestrogen/ progesterone/ cortisol shift
Negative energy balance onset
-lower DMI (oestrogen/ progesterone/ cortisol shift)
-fat mobilisation (lower DMI and lipolytic pathway upregulation)
Mineral deficiencies:
Types (2)
Result from (3)
Lead to (4)
Clinical (severe) and Subclinical (minor)
Low quality feed, impaired absorption, increase demand
Impaired immunity, inhibited growth, reproductive disorders, lower productivity
Calcium:
Functions (5)
Locations (3)
Diet effects
Multiparous effects
Transmission of nervous tissue impulses, excitation and contraction of skeletal and cardiac muscle, cell membrane permeability and cell linkage, cardiac rhythm control, required for milk/colostrum production
Bones (hydroxyapatite crystals), Intracellular, Extracellular fluid/ plasma (in blood bound to proteins, bound to organic components, soluble ionised form)
Ca absorption from gut is reduced by high potassium, high rumen nitrogen/protein, high dietary cation-anion difference DCAD, low phosphorus; high-Ca diet prepartum active transport of Ca from diet and depressed Ca resorption from bone
Decreased capacity to mobilise Ca from bone, fewer 1!25-DHD receptors in small intestine
Calcium homeostasis (3)
Calcium mobilisation sequence during Hypocalcemia (4)
Parathyroid hormone/ PTH (increased blood Ca, increased renal Ca absorption, increased intestinal Ca absorption, if long term increased resorption of bone Ca)
1,25-DHD/ Calcitriol (first hydroxylation in liver for inactive form, second hydrocykation in kidney for active vit D3, increased blood Ca)
Calcitonin (decreases blood Ca, increasing bone Ca storage, increasing Ca excretion in urine)
Immediate release of Ca into blood from bone extracellular fluid; reduced Ca excretion in urine at kidneys; increased Ca absorption at intestines in dietary Ca available (AT of. A from gut regulated by 1,25-DHD, passive transfer if very high Ca conc in digesta, delayed response), bone resorption via bone matrix breakup down by osteoclasts
Hypocalcemia:
What
Types (2)
Consequences (8)
Management/ prevention (4)
Ca loss exceeds Ca intake and resorption
Clinical/ Milk fever (blood Ca below 5 mg/dL, tachycardia, nerve and muscle excitation, lack of muscle control, sternal then lateral recumbency, bloat, test sphincter can’t close, can’t swallow)
Subclinical (low blood Ca 6.6-8.8 mg/dL no obvious clinical signs)
Ketosis, Fatty liver, Displaced abomasum, Decreased milk yield, Increased metritis and retained placenta, Decreased fertility, Increased mastitis, Decreased immune function
Acute treatment (IV calcium borogluconate); dietary prevention (feeding an ionic salts lowers DCAD improving Ca metabolism prepartum); monitoring and supplements (blood Ca and BCS, oral supplements); Staff education (recognise early signs, apply nutritional strategies)
Magnesium:
Location (2)
Function (4)
Grass staggers/ tetany
Hypomagnesaemia (4)
Bone and muscle pools
Prevents excessive nerve and muscle excitation, secretion of PTH for Ca homeostasis, tissue responsiveness to PTH, hydroxyl action process of vit D3 in liver
Minor Mg deficiency (leads to reduced DMI, nervousness, reduced milk yield/ reluctance to be milked, uncoordinated/ muscle spasms and seizures)
Further Mg deficiency; low Mg levels in soil; low fibre pasture (increased passage rate less time for Mg absorption); reduced food intake, high potassium levels (potash fertiliser); high ammonia levels (nitrogenous fertiliser)
Sequencing
Next generation sequencing (NGS)
Why we sequence/ application (2)
Clinical sequencing
Working out exact nucleotide sequence in a genome, using fluorescent coloured tags
High-throughput parallel sequencing technology
To find differences in genes based on comparison between individual genomes (within breed, between breeds, between individuals of same family), clustering algorithm identifies genetically distinct subpopulations (mastiff-type, herding and sight hounds)
Comparing genomes of healthy and sick animals, genetic factors contributing to disease, candidate genes
Genome-wide association studies (GWAS):
What
Use (5)
Application (1)
Compares variants across entire genome in different individuals classified by clinical manifestation (patient and non-patient), identify variant association with disease and risk allele (above threshold of variation)
Drug and diagnostic development, prognostic accuracy, personalised medicine, genetic and complex trait variant identification, cancer cell genome
Norwich terrier upper airway syndrome, not brachycephalic, present upper airway syndrome, graded phenotype, GWAS, region on chromosome 13 identified of candidate gene ADAMTS3
Personalised medicine (What, Outcomes 5)
Pharmacogenetics (What)
Examples (4)
Look at genome to identify which treatment will work for individual
Better disease prediction, target prevention and new strategies, more precise diagnosis, right therapy at right time, participation of owner
How an individuals genes affect response to drugs due to changes in metabolic pathways, prescription on individual basis
MDR1 (non functional p-glycoprotein, alters safety and efficacy of drugs), Cytochrome P450 (2 mutations causing decreased drug metabolism, longer time to wake up from anaesthesia), Cardiomyopathy (multiple genes involved, dif mutations identified, altered pharmacokinetics and pharmacodynamics due to gene polymorphism, beta blockers used but some don’t respond or develop reactions), Cancer (c-kit gene mutation more likely to respond)
Mast cells (what, role, where, action)
Mast cell tumours (MCT) (mutation, clinical presentation)
Diagnosis (2)
Sentinel cells/ tissue resident granulocytes, role in parasitic infection and allergic reactions, found in mucosal surfaces skin and around blood vessels, release inflammatory mediates (histamine) and cross-link surface IgE and binding of C5a
Mutation on c-KIT proto-oncogene, solitary modular reddened soft masses cutaneous or subcutaneous in dogs, visceral in cats
Fine needle aspirate (FNA)- cytology, conscious, cheap quick, can grade not standardised
Biopsy- histopathology, general anaesthetic/ sedation and local, expensive, time for results, grading more accurate, incisional (part) or excision (whole) biopsy, haematoxylin and eosin staining, granules easy to see in well-differentiated neoplasm, harder to see in cats and poorly differentiated
Mast cell tumour MCT:
Grading
Staging
Prognostication (4)
2-tier canine cutaneous MCT grading system; high grade MCT if 7 mitotic figures (structures identified in mitosis) in 10 high-power fields, 3 multinucleated (3 or more nuclei) cells in 10 hpf, 3 bizarre nuclei in 10 hpf, karyomegaly (large nuclei) and anisokaryosis (variation in cell nucleus size); low grade MCT if none of criteria
Metastasis assessment using TNM classification scheme; local tumour size; regional lymph nodes infiltration first, contrast agent used to see spread, classification HN0 0-3 scattered individual mast cells, HN1 more than 3 individual mast cells, HN2 clusters of mast cells, HN3 modules sheets or overt masses of mast cells; distant metastasis, to liver and spleen using imaging
Low grade MCT significantly longer survival time to those with high grade MCT; c-kit mutation significantly shorter survival time; KIT patterns 2 and 3 (nucleus and cytoplasm labelling) decreased survival time and increased incident of local recurrence; cytological evidence of mast cell infiltration in lymph nodes, spleen and liver significantly shorter survival time
Golden retriever muscular dystrophy (GRMD):
Mutation/ molecular pathology (3)
Dystrophin (4, 7)
Clinical signs (8)
Diagnosis (6)
Outlook (5)
X linked recessive disorder, mutation in dystrophin/ DMD gene, mutation in splice site at intron 6 (intron not removed, premature stop codon in intron, exon lost, frame shift, truncated or defective protein)
Long protein, shock absorber, ends interact with cytoskeleton and glycoproteins, connects actin cytoskeleton and extracellular matrix; defective leads to weakened sarcolemma, membrane lesions, reduced membrane integrity,creatine kinase leaks out, calcium influx causes protease activity, muscle abnormalities and necrosis/deterioration, inflammation
Stiff gait, decreased agility, decreased exercise tolerance, muscle atrophy, prominent bones spine ribs skull, megaoesophagus, large tongue, excessive drooling
Elevated creatine kinase in bloodwork, muscle biopsy, histopathological examination, degenerating muscle fibres, change in diaphragm and heart during necropsies, genetic testing
No treatment, stem cell junctions and gene therapy, steroids slow progression, avoid breeding, carrier status via genetic tests
Ageing:
What
Hair pigmentation/loss
Less energetic/ mobile and responsive
Incontinence, chronic renal failure
Odour
Reduced immune function
Osteoarthritis, cardiac failure, diabetes mellitus
Cognitive dysfunction
Progressive loss of physiological integrity leading to impaired function/ rendering more susceptible to disease and death, effects lifespan and health span
Grey hair patches, less melanocytes, less pigment); shedding, atrophied hair follicles
Sarcopenia- muscle loss due to old age, muscle fibre reduction; vision loss- cataracts, iris atrophy, retinal degeneration; hearing loss- nerve cell degeneration; muffled/weak bark- larynx nerve cell degeneration
Weaker anal and urinary sphincters, hormone level changes; nephron destruction
Stinky dry flaky skin, sebaceous gland produce less oil, reduced immune function and recurrent secondary skin infections
Reduced number immune cells, impaired ability to fight infection and target cancer cells
Progressive joint degeneration, inflammatory disorder; dilated cardiomyopathy, valvular diseases, arterial hypertensio; insufficient insulin, more common in overweight
Behaviour change, brain degeneration, canine cognitive dysfunction rating CCDR
Hallmarks of aging:
Primary hallmarks- 4, causes of damage
Antagonistic hallmarks- 3, responses to damage
Integrative hallmarks- 2, culprits of phenotypes
Genomic instability (longer an organism lives greater change DNA damage/mutation/alteration can lead to disease)
Telomere attrition
Epigenetic alterations
Loss of proteostasis (impaired protein homeostasis- stabilisation of correct and degradation of incorrect or unneeded proteins)
Deregulated nutrient-sensing
Mitochondrial dysfunction
Cellular senescence (stable arrest of cell cycle/ no replication, phenotypic change/ altered secretions, accumulation affects function and causes inflammation)
Stem cell exhaustion (decline in regenerative potential of tissues, decreased repair)
Altered intercellular communication (between cells and tissues, inflammaging/ pro-inflammatory status, impacts many organs)
Osteoarthritis:
Synovial joint change (7)
Chondrocytes (3)
Cellular senescence (3)
Pathology (5)
Symptoms/ risk factors (3,5)
Treatment (4)
Degeneration of articular cartilage, build-up of fluid, bone exposure and rubbing, osteophytes and bone cysts formation, joint space lost, inflammation, abnormal joint function
Synthesis and maintenance of cartilage extracellular matrix ECM, limited replication, respond to mechanical and biochemical stimuli
Replication senescence/ loss of cell division ability, decreased ECM synthesis, senescence-associated secretory phenotype SASP (secrete different things/ amounts)
Arrest of cell cycle, chondrocyte necrosis, degradative enzyme release, ECM breakdown, pro-inflammatory cytokines release
Stiff gait, joint pain, sensitive legs; genetics (P53 tumour suppressor gene expression increased with age), joint alignment, injury, activity level, obesity
Lifestyle advice, pain relief, surgery, but non-curable progressive degenerative condition