Asthma – pathophysiology, diagnosis, prognosis and treatment
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
Describe asthma incidence
- 8 in 100 people have asthma
- UK has the highest asthma disease mortality rates in EU
- 4 people day a die in the UK from asthma - 2/3 deaths are preventable
There is an 11% higher prevalence in the most deprived communities
For controlled asthma, how many flare ups should they be a year?
0 flare ups a years for controlled asthma
What is asthma?
A chronic disease
Inflammation of the airways
Triggers make them hyperresponsive
What are the symptoms of asthma?
Cough
Wheeze
Chest tightness
Shortness of breath
Symptoms vary over time and varying intensity. Patients can have periods of no symptoms - this can give the impression that asthma is well controlled.
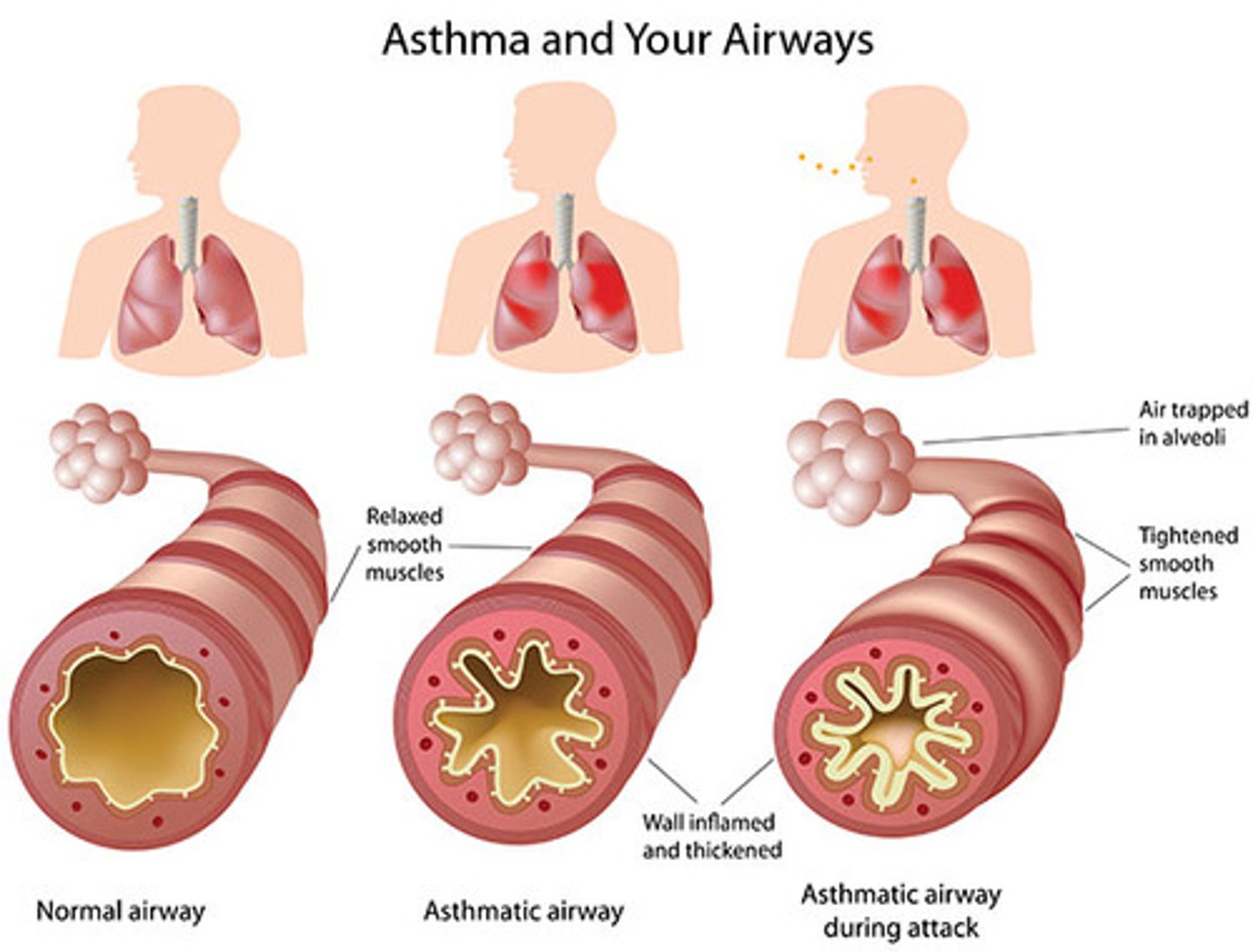
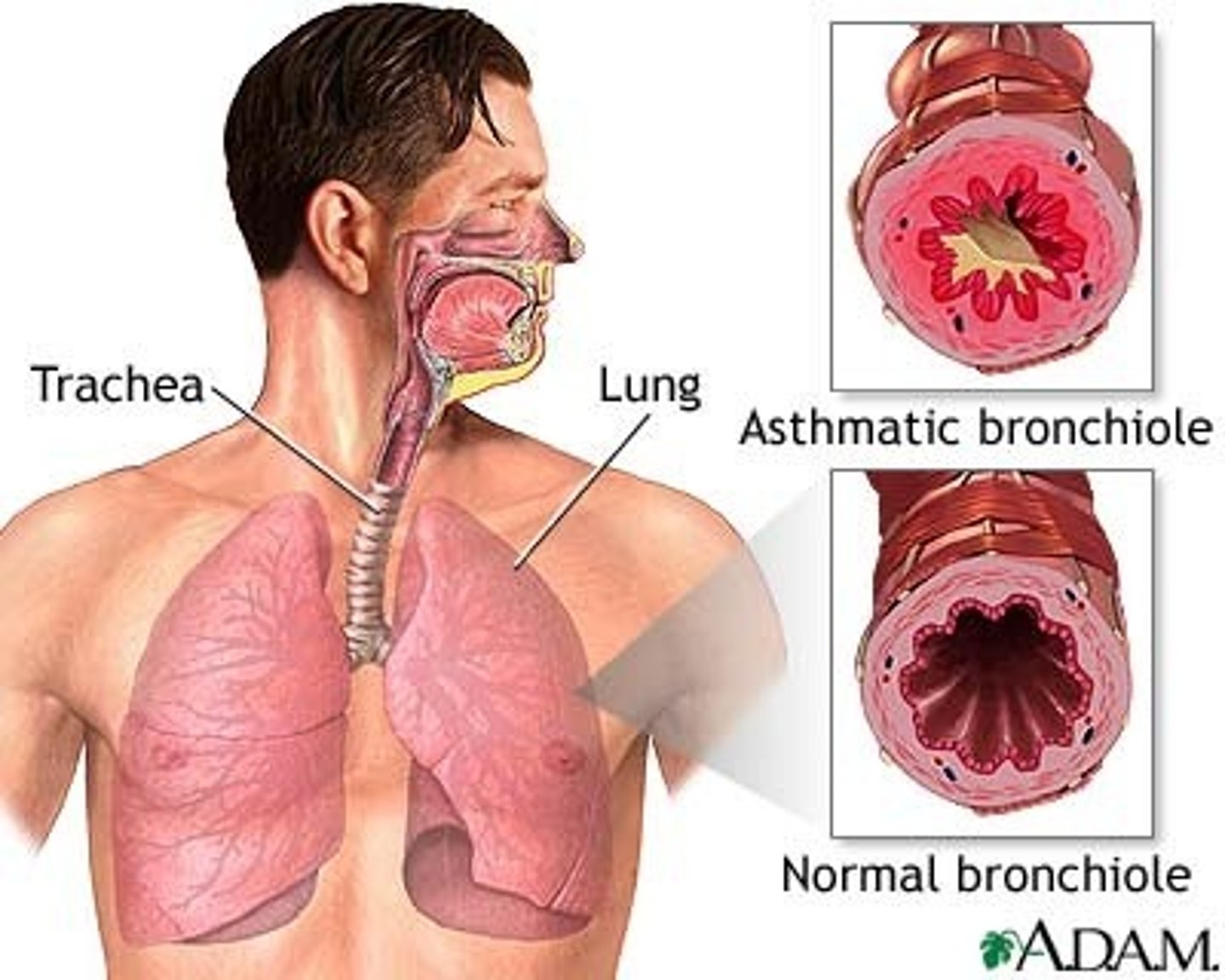
Describe asthmatic lungs compared to healthy patient lungs
Smooth muscle dysfunction: In an asthmatic lung, the muscles become tight (constricted) which reduces the lumen. The lining becomes swollen so the lumen of the airway becomes even tighter. Inflammatory mediator release.
Epithelial dysfunction: There is excess mucous production.
- Airway remodelling
- Cellular proliferation
- Epithelial activation
There is smooth muscle dysfunction AND airway inflammation which cause asthma symptoms.
Why is asthma so prevalent in the UK?
1. Poor awareness of treatment advances
2. Misdiagnosis (over & under), lack of asthma reviews, delayed specialist referrals
3. Undertreatment and mismanagement
4. Poor adherence with treatment
5. Symptoms normalisation by patients
6. Unaddressed environmental factors: smoking, air pollution, cold and damp housing
What are the different types of asthma?
- Allergic
- Non-allergic
- Cough-variant
- Late-onset
- Obesity-driven
- Persistent airflow limitation
Define asthma exacerbation/ flare up
An 'acute' or subacute worsening in symptoms and lung function from usual status.
This can present for the first time.
Define controlled asthma
When symptoms affect person's lifestyle or restrict their usual activities (including flare-ups needing OCS, and/or frequent regular symptoms).
Define severe asthma
Asthma which is uncontrolled despite optimised treatment with high-dose ICS/LABA or OCS (oral corticosteroids), or that requires a high-dose ICS (inhaled corticosteroid)/LABA or OCS to prevent it from becoming uncontrolled
What are asthma risk factors?
Genetic: any atopic disease (from yourself or family)
Environmental: air pollution, allergens, cold/ damp housing, exposure to tobacco smoke and workplace exposure
- if lots of respiratory infections as a child, increases risk of asthma.
Health and lifestyle: obesity, respiratory infections in infancy, premature breath and associated low birthweight
Give examples of asthma trigger
1. Allergens (pollen, mould, dust mites)
2. Irritants (tobacco smoke, air pollution)
3. Respiratory infections (common cold, influenza)
4. Exercise (intense, cold weather exercise)
5. Stress and emotions (anxiety, fear)
6. Medications (NSAIDs, beta blockers, ACEi)
7. Thunderstorms
8. Occupational exposures: chemicals, dust, fumes
9. Allergic reactions: food allergies, insect stings, latex
10. GORD (acid-reflux)
11. Hormonal changes: pregnancy, menstruation
What are current guidelines for asthma?
BTS/SIGN/NICE joint Guideline for Diagnosis, Monitoring and Management of Chronic Asthma - published in November 2024
Describe how asthma is diagnosed
1. Patient history and symptoms
- What triggers a patients asthma?
- Symptoms
- Where does the tightness originate from? Chest, throat
Family history
2. Physical examination
- Polyphonic wheeze: sounds go up and down like a wave
The airways are getting higher and higher. The higher the pitch, the narrower the airways. Then the sound disappeared. This is a life threatening situation
3. We need an objective test before confirming asthma
Objective tests have changed and the order of them have changed recently
Code as "suspected asthma" before confirmed
What are the different objective tests?
These are for children agent 5 and over.
1. Blood eosinophils or FeNO
2. Bronchodilator reversibility with spirometry
3. Peak expiratory flow variability
4. Bronchial challenge test
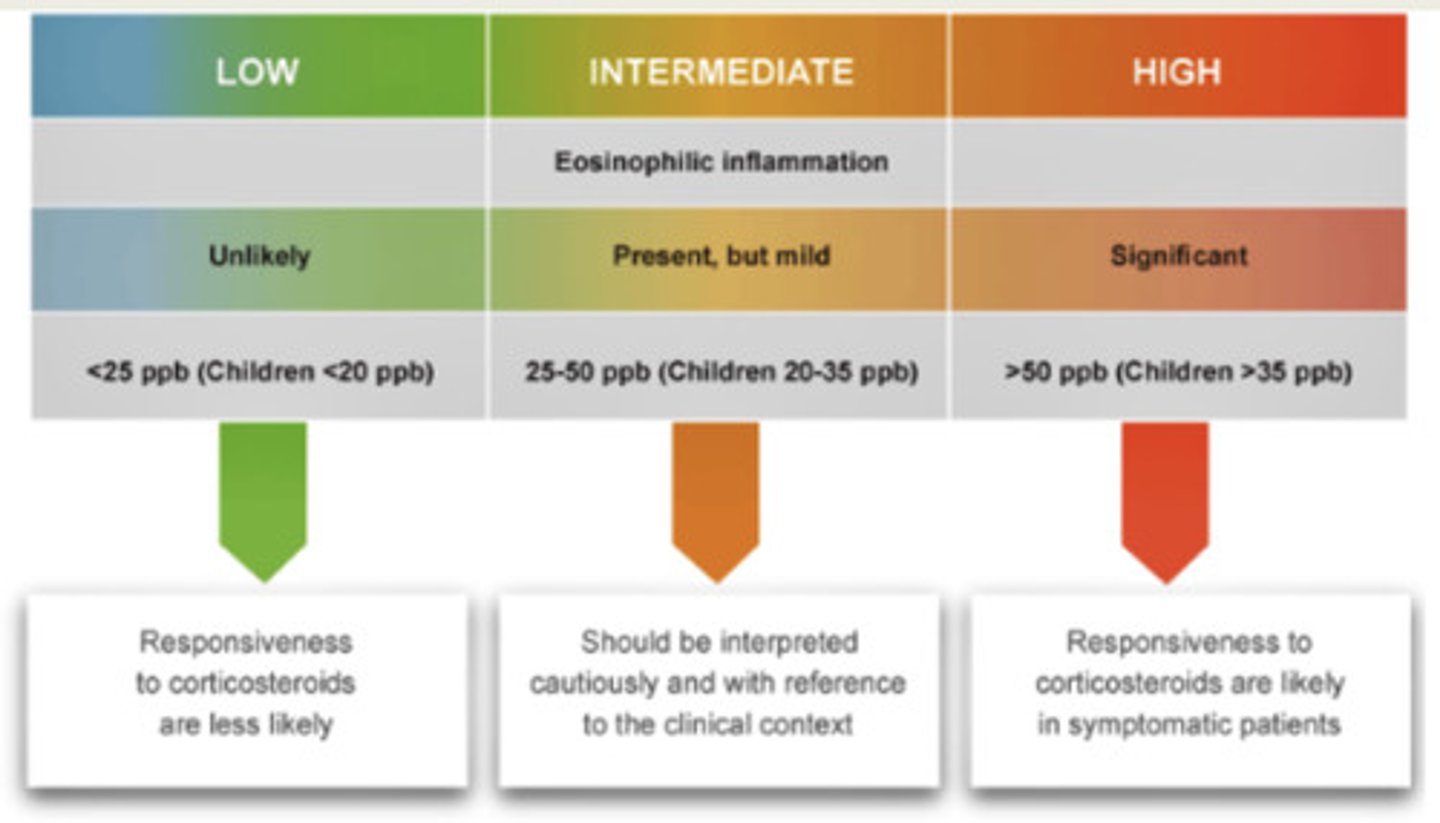
Describe FeNO testing
FeNO is gentle breathing - calm exhalation. This is the eosinophilic inflammation as NO is produced by eosinophils.
It is only recently that FeNO has been used in primary care now.
It is non-invasive simple, non-aerosol generating
It is type 2 inflammation which drives eosinophilic asthma.
Cut-off for asthma diagnosis is elevated in children.
If low FeNO, asthma is unlikely.
If FeNO is high, (FeNO level 50 ppb for adults) asthma is highly likely
What are limitations of FeNO testing?
1. Smoking massively reduces FeNO. This is a limit of FeNO testing.
If high FeNO despite smoking, then there is a lot of inflammation.
2. Some patients breath through nose OR some people can't breathe out for a long enough time.
3. If patient has oral steroids, then it reduced eosinophilic inflammation and masks the results. Therefore we must take a good history.
4. Allergic rhinitis/ rhinovirus infections decreases eosinophil level
5. FeNO testing is mainly reliable when result is high rather than when result is low
What was the effect of COVID-19 on FeNO testing?
Spirometry put on hold after COVID-19.
Breathing out forcefully caused cough which would spread COVID, so it was swapped for FeNO testing.
How should a patient prepare for FeNO testing?
- Avoid smoking for minimum 1 hour - but smoking reduced FeNO levels even from 10 years ago.
- Do not eat nitrate-rich food (green leafy vegetable, beetroot)
- Avoid hot drinks, caffeine and alcohol minimum for 1 hour
Describe spirometry testing
Spirometry measures
- How much air flows
- What is the total lung volume?
Can show:
1. Obstructive asthma e.g. asthma and COPD - obstruction in airways
2. Restrictive asthma e.g. pulmonary fibrosis, pulmonary oedema, lobectomy (remove one lobe of lung) - anything which reduces effective volume in the airways. Can't expand the lungs.
Both have reduced FEV1, FVC and FEV1/ FVC ratio
What is FEV1?
Forced expiratory volume in 1 second
What is FVC?
Forced vital capacity
Total air expired in a forced breath
What is FEV1/ FVC?
This is the ratio of the total air expired which is expired in the first second breath (during forced expiration). In healthy patients the FEV1/FVC is usually around 70%.
Describe peak flow testing
PEF variability is a measure of the extent to which max speed of expiration varies over time.
Peak flow is given to the patient to breathe out regularly for a number of days and monitor resultsYou breathe in, pause and breathe out as forcefully as you can (same as spirometry but not in a clinic)
We want to monitor how it changes overtime. We then calculate the different between the top and bottom of the wave (max and min speed of expiration). Shows asthma variability.
What is the problem with peak flow testing?
1. Patients often do not do this daily and fill out gaps with what they think is good.
2. Requires trust in patients to use it so that patients can monitor whether their asthma is getting better or worse. However, patients tend to only use their peak expiratory flow when they are getting worse, then we do not know their personal best.
Describe bronchial challenge testing
It measures airway responsiveness - an airway offender such as histamine is introduced in the lungs and then we measure FEV1. We detect how the airways react to it.
This is not done often in primary care
This is performed until FEV1 falls by a predetermined amount (usually 20% from baseline) or the highest dose is reached
What is 1st line treatment of asthma in adults and children 12+?
Low dose inhaled corticosteroid/ formoterol inhaler as required (PRN)
AIR therapy
What is 2nd line treatments for asthma in adults and children 12+?
If symptoms persist, use low-dose inhaled corticosteroid (ICS)/formoterol inhaler regularly AND as needed
MART = Maintenance And Reliever Therapy (ICS)
What is 3rd line treatments for asthma in adults and children 12+?
If asthma remain uncontrolled, increase to moderate-dose MART
MART = Maintenance And Reliever Therapy (ICS)
Why is formoterol used in asthma treatment?
Formoterol is the QUICKEST bronchodilator (LABA remains the same for all asthma treatment).
LABA = long acting beta-agonist
Why aren't SABA used for asthma treatment?
The use of SABA increases exacerbations if not taken with ICS - inhaled corticosteroids.
SABA shouldn't be prescribed without a concomitant ICS.
If treatment with SABA alone:
- Higher risk of asthma-related death
- Higher risk of urgent asthma-related healthcare
- Worse long-term outcomes
- Lower lung function than patients treated with low dose ICS from the time of diagnosis
What does ICS target in asthma treatment?
Airway inflammation
- Inflammatory cell infiltration/ activation
- Mucosal oedema
- Cellular proliferation
- Epithelial activation Airway remodelling
What does LABA/ LAMA target in asthma treatment?
Smooth muscle dysfunction:
- Bronchoconstriction
- Bronchial hyper reactivity
- Hyperplasia
- Inflammatory mediator release
What are the advantages of MART?
1. Improved preventer adherence
2. Reduced exacerbations
3. Single inhaler
4. Reduced confusion
5. Easy to step up/down
6. Reduced cost for patients
When should MART not be used?
- Children unable to use inhalers without spacers
- Mainly exercise-induced
- High risk of CS side effects
- With non-formoterol LAB
Give examples of MART inhalers
Fostair 100/6 only (extra fine particles)
Luforbec 100/6 only (extra fine particles)
Symbicort 100/6 or 200/6
How often should we review asthma treatment?
Review every 2-3 months and step up/down treatment according to response.
Annual reviews for long-term stable asthma
How do we escalate treatment if asthma remains uncontrolled?
If asthma remains uncontrolled despite good adherence and inhaler technique, escalate treatment:
1. Add LTRA (e.g., montelukast - NICE guidance on neuropsychiatric reactions)
2. Increase ICS dose or use ICS + LABA
- If still uncontrolled: trial LAMA - Specialist referral if high-dose ICS therapy ineffective
What are potential reasons for uncontrolled asthma?
1. Alternative diagnoses or comorbidities
2. Poor adherence
3. Poor inhaler technique
4. Smoking (active and passive) e.g. tobacco smoking and vaping using e-cigarettes
5. Occupational exposures
6. Psychological factors (e.g., anxiety and depression)
7. Change of seasons
8. Environmental factors (e.g., air pollution, indoor mould exposure)
What does the choice of inhaler depend on?
Choice based on:
- assessment of correct inhaler technique
- preference of the person receiving the treatment
- lowest environmental impact among suitable devices
- presence of an integral dose counter
How should inhalers be disposed?
All inhalers should be disposed of in a pharmacy
Why do we prefer DPIs over pMDIs?
1. Fewer critical errors
2. Natural inspiration technique can be used
3. No pressing
4. No spacer needed (convenience & being realistic)
5. Easier to teach the technique
6. Can be used by most (e.g. COPD)
7. Dose counter prevents:
- Using when empty
- Disposing when full
- Environmental impact
What are the treatment goals for asthma?
1. Symptom control
- fewer asthma symptoms
- no sleep disturbances
- no exercise limitation
2. Risk reduction
- maintain normal lung function
- prevent exacerbations
- prevent asthma deaths
- minimised side-effects from medication (oral corticosteroids)
3. Minimise environmental impact of medications
What is the ACT?
Asthma control test
It is a questionnaire posed to patients.
25 = asthma under control
20-24 = asthma on target
<20 = off target
ACT only asks patient how they have been OK for the past month (4 weeks).
What is the ACQ?
ACQ-5 or ACQ-7
Asthma control questionnaire
only shows how patient has been feeling for a week.
Score calculated as the mean of 7(5) Qs
0 - totally controlled asthma
>1.25(1.5) - poorly controlled asthma
0.5 - minimal clinically important difference
Give examples or side effects caused by oral corticosteroids
Opportunistic infections Activation of infections (e.g., TB)
Cushing's syndrome Hypokalaemia
Increased gluconeogenesis Osteoporosis
Fluid retention, oedema hypertension
Skin atrophy
Bruising
Muscular atrophy
Impaired wound healing Irritability, restlessness, anxiety
Psychotic disorder
Sleep disturbances
Depressed and labile mood Cataract
Gastrointestinal discomfort, nausea, peptic ulcer Headache
Hirsutism
Menstrual cycle irregularities Weight gain
What should we check before we give patients a course of steroids?
Check inflammatory markers (elevated blood eosinophils and/or FeNO)
If had previously, check the time to respond to OCS
Risks vs benefits
Is it time to refer to an asthma specialist?
NO patient should be on maintenance steroids
Give lifestyle advice for asthma
Stop smoking
Good Inhaler technique
Monitoring
Pharmacotherapy
Lifestyle
Education
What is a PAAP?
A personalised asthma action plan. This should be information on
- how to see if asthma is worsening
- what to do if asthma is worsening
- how to monitor response to treatment
- contact details for asthma nurse
Check if reliever correct & understood by the patient
How to treat "difficult to treat severe asthma"?
We give these patients asthma biologics - given in tertiary sectors.
There are only around 16 tertiary sectors in the country for asthma.
Patients must fit a certain criteria: ICS therapy, 3+ OCS (in practice, refer patients on 2 OCS)
- For most biologics, elevated blood eosinophils required (0.3 or 0.4)
- First administration is often supervised
OCS = oral corticosteroids
When do we refer uncontrolled asthma to tertiary care?
If patient is on maintenance oral corticosteroids
If patient has been admitted previously to intensive care for asthma
What are characteristics of uncontrolled asthma?
1. Needing oral corticosteroid course more than 2 times in a year
2. At least 1 serious hospital visit due to asthma
3. Poor symptom control e.g. waking up at night, wheezing
4. 6 or more SABAs in 12 months