3. basics of neoplasia
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
neoplasia
neo= new
plasia= growth
aka tumor
the process
neoplasm
the product of neoplasia
An abnormal mass of tissue, the growth of which exceeds and is
uncoordinated with that of normal tissue and persists in the same
excessive manner after cessation of the stimuli which evoke the
change
can be benign or malignant
Monoclonal proliferation
All the cells in a cancer are the direct descendants of one single cell gone bad
cancer
malignant neoplasm
#2 cause of death
oncology
study of cancer
some prefixes used to naem cancers
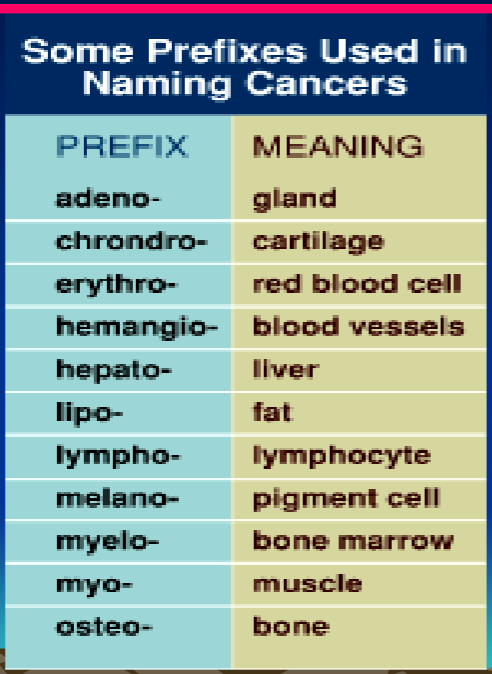
naming tumors: epithelial tumors
-Oma = Benign
Carcinoma = Malignant
naming tumors: Connective Tissue Tumors
Oma = Benign
Sarcoma = Malignant
lymphoma + melanoma = malignant (exceptions)
Benign vs Malignant neoplasms: symptoms
Benign: Usually none
malignant: pain, paraesthesia (numbness), systemic symptoms (malaise, wasting etc.)
Benign vs Malignant neoplasms: differentiation
benign: Resembles cell of origin
malignant: Less differentiated, especially with highly malignant tumors
Benign vs Malignant neoplasms: mitotic rate
benign: Few mitoses, all normal Slow growth rate usually
malignant: Many mitoses, some abnormal, May have rapid growth
Benign vs Malignant neoplasms: nuclear features
benign: Relatively normal
malignant: intensely staining (hyperchromatic) nucleus
Relatively large nucleus in relation to cytoplasm (high nuclear/ cytoplasmic ratio)
Benign vs Malignant neoplasms: cellular uniformity
benign: Cells uniform
malignant: Cells and nuclei vary in shape and size (pleomorphism)
Benign vs Malignant neoplasms: prognosis
benign: Usually very good
malignant: Major cause of death
Benign vs Malignant neoplasms: behavior
benign: Grows locally, compressing adjacent tissue usually
malignant: Invades adjacent tissue
Benign vs Malignant neoplasms: suface changes
benign: Stretches overlying tissues
malignant: Overlying epithelium may be ulcerated
Benign vs Malignant neoplasms: margin
benign: Encapsulated often (prevents them from moving to distant tissues) Therefore freely moveable
malignant: regular invasive margins Therefore fixed to adjacent tissues (indurated)
Benign vs Malignant neoplasms: spread
benign: Expands in one area only
malignant:May metastasize through bloodstream or lymphatics
May spread along nerve trunks
Benign vs Malignant Tumor: cause
Both are caused by increased cellular proliferation
i.e. Increased cell cycling
Genotype VS Phenotype of cancer
The genetics of cancer may start long before changes are visible
clinically + microscopically
Dysplastic/ dysplasia
Some mutations
pre cancerous stage
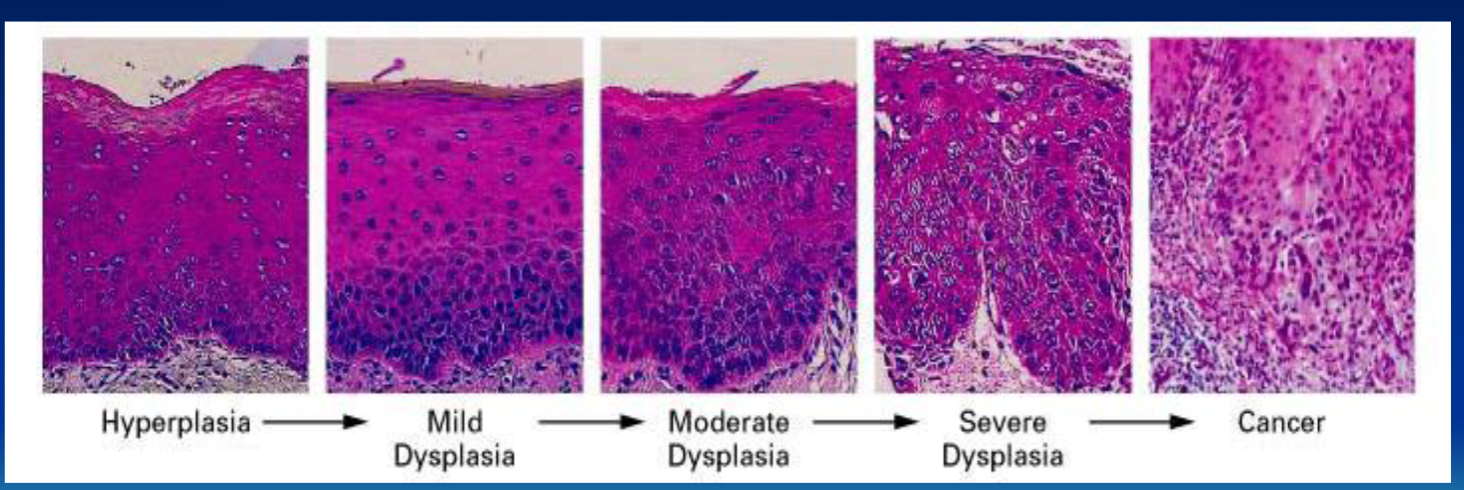
Mild dysplasia
Limited to basal layer
Moderate dysplasia
Basal layer to mid portion of spinous layer
Severe dysplasia
Basal layer to level above midpoint of spinous layer
Ca-in-situ dysplasia
Basal layer to surface ("top-to-bottom")
No invasion
followed by cancer
In situ
Almost able to invade
Malignant
Invades and can metastasize
actual cancer stage
Induration
a hardening or thickening of tissue
does not ONLY mean malignancy
could also indicate scarring or deep inflammation
cancer spreads by penetrating:
basement membrane
extracellular matrix
blood vessels
cancer spread steps: penetration of BM
Tumor cells detach from each other (down regulation of
cadherins)Laminin - Glue binding the BM constituents to each other & to epithelial cells via receptors
increased laminin receptors on cancer cells
Penetration of basement membrane
Tumor secretes Type IV collagenase & other proteases to break down BM proteins
Cleavage products have growth-promoting, angiogenic
and chemotactic properties
cancer spread steps: penetration of ECM
Overexpression of fibronectin helps cancer to spread
Tumor secretes collagenase and actively moves through the tissues (AMF - autocrine motility factor)
cancer spread steps: penetration of blood vessels
Much like penetrating basement membrane
Tumor cells may clump with platelets forming tumor cell emboli
where can cancer spread?
Local invasion
Lymphatic
Blood-borne (vascular)
Seeding body cavities
Cancer Families
Cancer is much more likely than in general population
– earlier age
– multiple tumors
– worse prognosis
Rarely, because damaged DNA cannot be repaired
Fanconi’s Anemia, Xeroderma Pigmentosum, Bloom’s syndrome
Gorlin-Goltz Syndrome or Nevoid Basal cell Carcinoma Syndrome
Mutation in tumor suppressor gene patched (PTCH) on chromosome 9
Basal cell carcinoma starting in childhood
Multiple darkly pigmented nevi (mole)
Palmar and plantar pits (palms & soles)
Gorlin - Goltz Syndrome manifestations
Multiple Odontogenic Keratocysts
May be aggressive
Bifid ribs, Scoliosis, Frontal bossing
Hypertelorism, Marfanoid habitus (long + slim face)
Calcified falx cerebri
Sometimes cleft palate
Gardner Syndrome
Hereditary syndrome - Linked to band 5q21, the adenomatous
polyposis coli locus
Dental team may be first to suspect patient has this disease
Hundreds of colon adenomas that eventually turn into colon cancer
Multiple unerupted and extra teeth
Osteomas
Aggessive fibromatosis (benign desmoid tumors in abdomen)
Cancer & Chromosomes
Cancer may also result from changes in the chromosomes, not just the genes
Numerical + Structural
Structural – Translocation- Examples
Philadelphia Chromosome
Burkitt Lymphoma: Translocation between 8 & 14, Less
commonly 8 & 2 or 8 & 22
Structural - Deletions - Genetic material lost Examples:
Retinoblastoma + Wilms' Tumor
Gene Amplification
Increased expression of oncogene
Example : Neuroblastoma -- N-myc
cancer prevention
Protecting from UV radiation
Avoid Cancer Viruses
Avoid chemical carcinogens
diet
avoid tobacco smoke
Immune Surveillance
Higher rates of cancer in profoundly immunosuppressed patients
Natural selection eliminates clones with lots of antigen
Some may cause immunosuppression, others may result
from it
ex: Organ transplant + HIV / AIDS
cancer detection + diagnosis
biopsy
pap test
Epidemiology of Cancer
Increases with age
Cancer incidence is different for men and women
Prevalence depends on complex interplay of biology and culture
Example- South-East Asia tobacco chewing is common
Oral cancer is a major health risk
In cultures where women do not smoke, lung cancer is much less common in women
Oral Cancer
In North America, about #6
80-90% of oral cancer is squamous cell carcinoma
Risk factors for oral SCC
Tobacco
– Cigarettes, Pipe, cigar, chewing
– Reverse smoking
Alcohol
In association with smoking, not by itself
HPV 16, 18, 31, 33
Clinical / Radiographic features of oral SCC: Endophytic
Pebbly, hard
Clinical / Radiographic features of oral SCC: Exophytic
Rolled border
Clinical / Radiographic features of oral SCC: Leukoplakia
White patch
Clinical / Radiographic features of oral SCC: Erythroplakia
Red patch
Clinical / Radiographic features of oral SCC: Perineural invasion
Pain, paresthesia
Clinical / Radiographic features of oral SCC: Moth-eaten radiolucency
if spread into bone