Newborn/ Complications test
1/132
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
133 Terms
what are the 4 methods of heat loss?
A: Convection
B: Radiation
C: Evaporation
D: Conduction
Convection
- the flow of heat from the body surface to cooler ambient air
Radiation
- the loss of heat from the body surface to a cooler solid surface not in direct contact, but in relative proximity
Evaporation
- the loss of heat that occurs when a liquid is converted to vapor. Wet surfaces exposed to air. Dry quickly, place hat on baby at birth, dry diapers
Conduction
- the loss of heat from the body surface to cooler surfaces in direct contact. Loss of heat via direct contact with cold surface. Cover the scales while weighing newborn with a blanket
what is the primary source of energy in a newborn infant?
Glucose
Mild respiratory distress can become severe hypoxia if oxygen must be used for?
heat production
Jaundice
- Pathological vs. physiological
- Breastfed babies usually more prone
- Associated w/ destruction of RBC's that are no longer needed
- Blanch the skin over a boney prominence (chest, nose, forehead) and observe the color before regular color returns
Coomb's Test
pathological jaundice usually occurs when?
within the first 24 hours, something in wrong
physiological jaundice usually occurs when?
happens after 24 hours, normal process
The most common cause of jaundice in breastfed infants is:
Insufficient intake
What causes jaundice in a new baby?
The liver may not be mature enough in the first week of life to prevent jaundice
When caring for a jaundiced baby what do you check for?
A: Absent moro reflex
B: Poor sucking
C: High pitched cry
D: Other signs of lethargy
What characteristics predispose newborns to heat loss?
-Thin skin
-Decreased SQ fat
-Being premature
-Being sick
-Not being flexed
-Head is ¼ of their body and they lose heat through their head
-Blood vessels near surface
-Larger ratio of surface area to body mass
-Heat regulating and circulatory systems not yet matured
Why is a preterm or sick newborn at higher risk for heat loss/ cold stress?
-preterm babies usually have little body fat and may be too immature to regulate their own temperature
-they are smaller and had way less fat to keep them warm
-also less brown fat
-they also may have other issues going on and their energy and glucose is more focused on that than warmth (like breathing)
Newborns will rarely shiver to produce heat. What behavior may be seen in a newborn in an attempt to generate warmth?
use of brown fat, crying, flexed position
How does brown fat help maintain body temperature? Under what circumstance can newborns have inadequate brown fat and why?
in term babies as a reserve to help with survival in the first few months. When they are premature/sick they might have inadequate brown fat because they have used their stores to survive.
what to do if APGAR score is low like a 2?
- set respiratory stuff up
- make sure warmer is ready
- get suction out
- get ready for resuscitation
What glucose level on a screening test requires further follow-up?
<40-45, feed them, may need an IV
What is the primary source of bilirubin? Why is it common in neonates?
-Dead damaged erythrocytes
-Liver cannot process that and cannot metabolize or get rid of them because of that
-All babies are at risk
-Common in neonates because liver is immature
What factors lead the production of excessive amounts of bilirubin?
-Extra RBC
-Cephalhematoma, bleeding, bruising, injury
-Sick, temp, breathing, glucose problems delay mechanism and eating and all the things babies do in the first day of life which delays the passage of extra bilirubin and it builds up in the body
-Immature livers (preterm)
What methods are used to decrease bilirubin levels?
- Phototherapy (lights)
- Bili blankets
- Bili beds
In an infant who is receiving phototherapy, what are 6 specific nursing responsibilities related to this treatment?
A: Lights are proper strength
B: Cover eyes
C: Cover genatalia
D: No lotions or creams
E: Promote bonding with mom and dad
F: Have to be on I&O
G: Check temperature
What is our main concern when a baby is receiving phototherapy?
dehydration
Hyperemesis Gravidarum
-Persistent, uncontrollable vomiting
-Can persist, but typically it is early in 1st trimester
S&S of dehydration (hyperemesis gravidarum)
- Ketones in the urine, decreased I&O, electrolyte imbalances, decreased skin turgor
-The difference between hyperemesis and morning sickness is the dehydration.
- Hyperemesis MUST be treated.
Treatment of Hyperemesis Gravidarum
- IV Fluids
- Daily weight and I&O
- Antiemetics: Phenergan, Benadryl, Zantac, Reglan, and Zofran
- Zofran is the main one used
- 6 small meals/day - the more bulk you put in the stomach, the more it will reject.
- Bland foods and drink fluids between meals
- TPN
- Emotional support
what is preeclampsia also characterized by?
- hypertension
- proteinuria
- edema in hands, face, and above waist
what signs would make you want to call the dr for preeclampsia?
- low urine output
- increased weight gain
What is the Major cause of perinatal death and intrauterine grown restriction?
preeclampsia
Pathophysiology of preeclampsia
- Generalized vasospasm of the body.
- Decreased diameter of blood vessels results in endothelial damage.
- Impeded blood flow, elevated BP
- Circulation is decreased to all organs.
- Major organs affected: kidneys, brain, liver, and placenta.
- Placenta can't get enough blood to baby - IUGR. (intrauterine growth restriction)
How is baby affected by preeclampsia mother?
utero placental insufficiency
what should you do for a pregnant mother with preeclampsia?
- Try to maintain the pregnancy for as long as possible to have the best outcome for the baby.
- Maintain BP, monitor weight, CNS, and baby.
- Once things are too bad, we deliver.
Post partum treatment preeclampsia
- Tx continues for at least 24 hours.
- Meds to prevent seizures are still given
assessments for preeclampsia
- Bedrest, side-lying - promotes blood flow to baby
- High protein diet
- BP, FHT checks
- Daily weights
- I&O/protein dipstick
- DTR/clonus
- HA, visual disturbances, RUQ pain, n/v
- Lung sounds
medications for Preeclampsia
-antihypertensives (hydralazine, nifedipine, labetalol)
-anticonvulsants (magnesium sulfate)
-NO DIURETICS (they will not take fluid off and may be harmful to fetus)
class of magnesium sulfate
anticonvulsant
what is magnesium sulfate used for in the OB setting
treatment and prevention of seizures associated with eclampsia or preeclampsia
what are the 2 categories in the gestational age assessment
neuromuscular and physical
what does magnesium sulfate do for the body
-CNS depressant
-prevents seizures
what to monitor in a patient receiving magnesium sulfate
-BP, pulse, respirations, and ECG
-neurological status and initiate seizure precautions
-newborn for hypotension, hyporeflexia, respiratory depression if mother was given this
-I&O ratios
-magnesium levels and renal function
-LOC
-O2 saturation
-ability to move arms and legs
what level cause magnesium sulfate toxicity
>8
S&S of magnesium sulfate toxicity
-cardiac or respiratory depression
-absent reflexes
-excessive sleepiness
-N/V
-oliguria
Mag sulfate setup
- IV infusion/piggyback.
- Main line in the closest port in case we have to d/c.
Diabetes
- Endocrine disorder with major effects on carbohydrate metabolism.
- Can be present pre-pregnancy or during pregnancy
- Insufficient insulin production
Potential effects: diabetes
- Hydramnios (extra fluid while pregnant)
- Preeclampsia
- Dystocia (baby is big and the shoulder gets stuck)
- Still birth
- Macrosomia (big baby)
pre-pregnancy diabetes
- Insulin needs early 1st trimester decrease because our baby is rapidly growing and utilizing the extra glucose we were treating.
- End of 1st trimester/start of 2nd the insulin needs go back up because the baby isn't growing as fast and using the extra sugar.
- We then see the moms become resistant to insulin and that it breaks down quicker.
- Once the baby is born and we take the placenta away, the insulin needs return to normal.
- The placenta is an endocrine organ.
- They require specific tx; often hospitalized.
Gestational diabetes
- Usually goes unknown until the end of the 2nd or start of the 3rd.
- Is still resistant to insulin and it breaks down quicker; may have to start her on insulin.
- Once baby is born, everything goes back to normal.
Gestational diabetes is diagnosed how?
diagnosed by two glucose tolerance tests above 140, 1 hour and 3 hour
Insulin
- Change in insulin requirements
- 1st trimester: needs are low - r/t of rapidly growing baby.
- Needs increase late 1st trimester
- Cells have increased resistance to insulin
- Increased speed of breakdown
Shoulder Dystocia
where the baby's shoulder gets stuck behind the mother's pubic bone after the head is delivered, preventing the rest of the baby's body from being born
Placenta Previa
where the placenta attaches to the lower part of the uterus, near, or covering the cervix (comes out 1st instead of baby)
Abruptio Placenta
when the placenta prematurely separates from the uterine wall before the baby is delivered
Amniotic Fluid Embolism
where amniotic fluid containing fetal cells, hair, or other debris enters the mother's bloodstream (moms usually don't survive)
S&S of hypoglycemia
- Diaphoresis
- Passing out
- Jittery
- Shaky
tx of diabetes:
- Glucose: 70-120
- Maintain the following
- Glucose monitoring
- Urine testing (glucose and ketones)
- Insulin (NO oral hypoglycemics) (category X)
- Diet control
- Exercise
Effects on mom (diabetes)
- Vascular changes in placenta
- Spontaneous abortions
- Abnormal fetal developments
- Intrauterine death at 36 weeks
- Do biophysical profiles and nonstress tests weekly
- Delayed fetal lung maturity
- Large for gestational age (LGA) infant
- Other problems in the infant (low blood sugar)
what happens to the placenta in a diabetic mom and what are they at high risk for?
- Our placenta in a pregnant mom age faster than moms who isn't diabetic (high risk of full-term stillbirth)
- Often don't let diabetic moms go full term
Physiological Changes newborn
- Profound changes occur (starts breathing)
- Respirations
- Cardiovascular (shunts close)
- Neurological (babies' ability to keep itself warm) (before 34 weeks we have to keep babies in warmer)
Focus of Newborn care is?
- maintaining respirations & thermoregulation
- keep it breathing, keep it warm
Respiratory Adaptation
- Chemical, thermal, mechanical, & sensory factors
- Surfactant
When our babies come out why do they start breathing? chemical
moms' feelings of excitement (epinephrine, norepinephrine) help the babies shunts to close, helps the lungs to absorb the fluid
When our babies come out why do they start breathing? thermal
baby being exposed to the real world, the change of the thermal environment going from warm to cold air
When our babies come out why do they start breathing? mechanical
babies head is out; mom's vagina is squeezing the babies' fluids out of its body (vaginal birth)
When our babies come out why do they start breathing? sensory factors
contact with the baby is stimulating them because they've never experienced physical contact before (being touched and rubbed down helps baby to breathe)
When our babies come out why do they start breathing? surfactant
added benefit of surfactant in the lungs helps the process (L/S ratio)
What behavior do we see in newborns to generate warmth? (effects of baby getting cold)
cry, become lethargic, glucose drops, quit breathing
Brown fat
- helps maintain their warmth, when needed
- Used under normal circumstances when they get cold
- We don't want them to use their brown fat for circumstances that we are controlling
- Absent feedings
Relationship between oxygen, body temp., glucose stores, bilirubin levels
- the relationship is if one is off, they will all be thrown off.
- Interrelated, if one goes bad the rest will too. Make sure breathing, stays warm, glucose stays good. If bilirubin is messed up, they will get jaundice in two days
S&S respiratory distress
- Nasal flares (1st sign), retraction (use of accessory muscles), cyanosis (late sign), Tachypnea, grunting (noise made)
what is a good APGAR score?
between 8-10
APGAR score
A - Appearance
P - Pulse
G - Grimace
A - Activity
R - Respiratory
Done at 1, 5 and sometimes 10 minutes
APGAR Score (test question)
A- Appearance
- Color
- Blue or Pale - 0 points
- Body pink, extremities blue (acrocyanosis) - 1 point
- Completely pink - 2 points (not typical even at 5min)
APGAR score P-Pulse
- Heart Rate
- Absent - 0 points
- <100 - 1 point
- >100 - 2 points
APGAR Score G-Grimace
- Reflex response/irritability
- No response - 0 points
- Grimace - 1 point
- Crying/coughing - 2 points
APGAR score A-Activity
- Muscle tone
- Flaccid/limp - 0 points
- Some flexion when stimulated - 1 point
- Active motion/ well flexed - 2 points
APGAR Score R - Respiratory
- Respiratory Effort
- Absent - 0 points
- Slow irregular, weak cry - 1 point
- Good, crying - 2 points
APGAR
- Scoring
- 0-3- severely depressed- need resuscitation
- 4-6- moderately depressed
- 7-10- doing fine
- 8-10 is normal findings
- 1 min test - how was the baby doing inside?
- 5 min APGAR - how its doing outside, what we've done to help our baby.
· Immediate Responsibilities with the Newborn (TEST QUESTION)
- Note time of birth
- APGAR w/ stabilization
- Take VS q 15 minutes x 4 then hourly
- Assess for anomalies.
- Vitamin K shot
- E-mycin ointment to eyes
what is the priority for the immediate responsibilities of the newborn
- Priority APGAR !!! *** Clue: 1st min (crying, HR, resp, color)
- Temp is not priority
Cardio-respiratory Assessment Airway
- clear the airway, by bulb syringe or suctioning. ABCs
- Respirations, Breath Sounds (normal resp. 30-60)
- New baby breath sounds can sound crackly
Cardio-respiratory Assessment color
pink, acrocyanosis is normal (blue hands and feet)
Cardio-respiratory Assessment Heart sounds
fast HR, looks for background swooshing or murmur (report all murmurs)
Cardio-respiratory Assessment pulses
femoral, & brachial (we don't want bounding pulse, if could indicate heart defect)
Cardio-respiratory Assessment capillary refill
<3 secs. Check it on their chest, nose, or forehead (hands is not the best place to check)
Vital Signs
- Done q 15 minutes x 4 then hourly, then q 4 hours
- Respiratory & heart rate done prior to disturbing the infant for 1 full minute.
- Resp (30-69)
- Heart rate (110-160)
- Temp (97.7-99.5) - axillary (98.0 happy place for temp.)
Vital Signs - Temperature
- Newborn's temp reflects that of the environment: R/T thin skin & limited SQ fat
- Heat regulating and circulatory systems not yet matured (they lose heat through their head)
- Special tissue called brown fat helps increase body heat
- Use pre-warmed blankets &/or incubator to maintain temperature
Highest priority after birth?
- Dry the baby, warm the baby
- Skin to skin to the best way to warm a baby
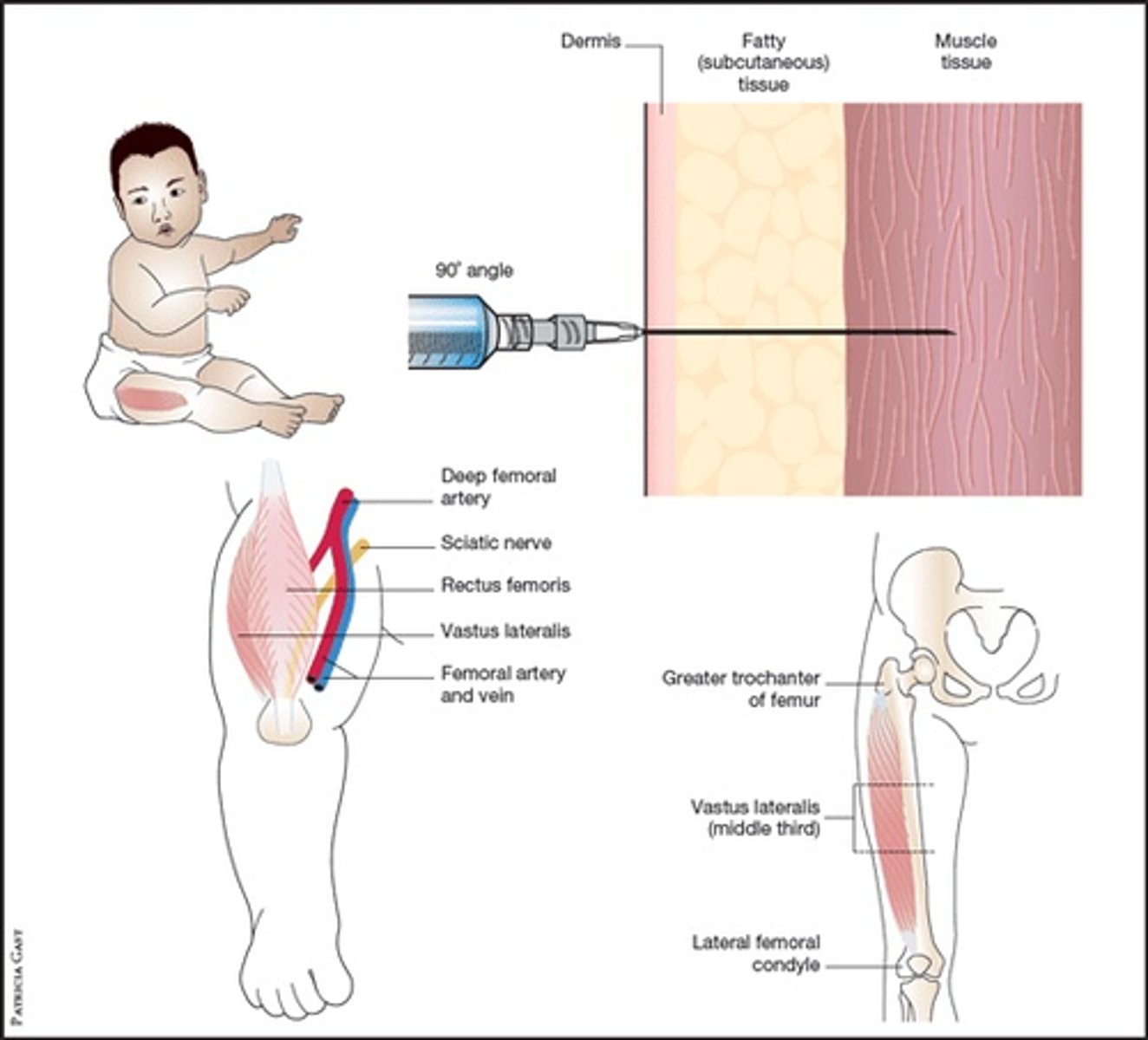
Newborn IM injections
Why do we give Vitamin K?
clotting, decreases risk of bleeding for baby
Respiratory System
- 1st breath helps expand the collapsed lungs at birth
- Cry should be strong & healthy
- Position on back or side
- Dress to maintain warmth
- Suction nose & mouth as needed
- Be aware of APGAR score**
Immediate Assessment
- Head & Neck - tells the baby's story
- Cord - 3 vessels "AVA'
- Extremities
- Vertebral Column
- Measurements
Caput succedaneum
- Edema of the soft tissues of the scalp
- CROSSES THE SUTURE LINES
- Gone usually after 24 hours.
- Results from prolonged pressured on the head during labor
- squishy due to fluid
Cephalhematoma
- trauma, use of vacuum
- Edema on the head
- DO NOT CROSS THE SUTURE LINES
- Clots & becomes hard, will not feel like Jello
- Takes longer to heal. (3-4 months)
- Effusion of blood b/t bone
- Can have an end result of jaundice, utilize Billi lights
- hard due to blood
how long is the neonatal transitioning period?
6 hours
Blood Glucose
- 40-60 (1st day)
- 50-90 (subsequent days)
- < 40-45 (intervention)
- Hypoglycemia
What babies are at risk for hypoglycemia? Preterm/ small
they have less stores, potentially breathing issues, sickness, thinner skin
What babies are at risk for hypoglycemia? Large for gestational age
- mom is diabetic usually and gave them too much sugar when pregnant
- the baby's pancreas secreted extra insulin to compensate for the extra glucose and when the baby was born and the extra glucose was no longer given to them
- the baby's pancreas still secreted extra insulin
What babies are at risk for hypoglycemia? Post-term
the placenta is aged
Priority care for large gestational age baby?
breathing due to lungs not fully developed