ANA 2 - MOD 7 - RESPIRATORY SYSTEM
1/108
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
109 Terms
Respiration
exchange of O2 and CO2 between atmosphere, blood, and cells
External Respiration
gas exchange between the air in the lungs and the blood
Internal Respiration
gas exchange between the blood and the tissues
VENTILATION
the movement of air into and out of the lungs
Upper Respiratory Tract
external nose, nasal cavity,
pharynx, larynx
Lower Respiratory Tract
trachea, the bronchi and smaller
bronchioles, and the lungs
Conducting zone
exclusively for air movement and
extends from the nose to the bronchioles
Respiratory zone
within the lungs and is where gas
exchange between air and blood takes place
Nose
consists of the external nose and nasal cavity
External Nose
hyaline cartilage plates, nasal bones, extensions of frontal and maxillary bone
Nasal Cavity
passageway of air
External Nares (nostrils)
external openings
Internal Nares/Choanae
openings into the pharynx
Vestibule
anterior part of nasal cavity, lined with
stratified squamous with coarse hairs called vibrissae
Hard Palate
formed by maxilla and palatine bone
separates the nasal cavity from the oral cavity
Nasal septum
partition dividing the nasal cavity into right and left parts
Cartilage
Anterior to nasal septum?
Vomer and ethmoid bone
Posterior to Nasal Septum
Conchae
three bony ridges that modify the lateral walls of nasal cavity
Paranasal Sinuses
contribute to the humidifying of the inspired air. They also reduce the weight of the skull.
Pharynx
Common opening of both the digestive and the
respiratory systems
Nasopharynx
located posterior to the choanae and superior to the soft palate; opens into two auditory tubes
Soft Palate
an incomplete muscle and connective tissue partition separating the nasopharynx from the oropharynx
prevents swallowed materials from entering the nasopharynx and nasal cavity
Uvula
posterior extension of soft palate
Pharyngeal tonsils
helps defend the body against infection
Oropharynx
extends from the soft palate to the epiglottis
Laryngopharynx
extends from the tip of the epiglottis to the esophagus and passes posterior to the larynx
Larynx
“Voice box”
Located between C4-C6.
It is a passageway for air between the pharynx and the
trachea
Consists of an outer casing of nine cartilages connected
to one another by muscles and ligaments
Arytenoid Cartilage
Corniculate Cartilage
Cuneiform Cartilage
What are the 3 Paired Cartilages?
Thyroid Cartilage (adam’s apple; largest)
Epiglottis Cartilage
Cricoid Cartilage
What are the 3 unpaired cartilage?
Vestibular folds
false vocal cords
Vocal folds
true vocal cords
Glottis
opening between the vocal folds
Trachea
“Windpipe”
It consists of dense regular connective tissue and
smooth muscle reinforced with 15–20 C-shaped pieces
of hyaline cartilage.
The posterior wall of the trachea is devoid of cartilage
Esophagus lies immediately posterior to the cartilage free posterior wall
Diameter of 12 mm and a length of 10–12 cm, descending from the larynx (C6)to the level of the level of carina (T4-T5)
Trachealis Muscle
contraction of this smooth muscle narrows the diameter of trachea
Goblet Cells
Lined by pseudostratified ciliated columnar epithelium with numerous _____?
Main or primary Bronchi
The trachea divides to form two smaller tubes called _______ or _______?
Carina
most inferior tracheal cartilage. Bifurcates the openings into the bronchi
o Sensitive to mechanical stimulation
o Can stimulate a powerful cough reflex
TRACHEOBRONCHIAL TREE
Trachea divided into (R) main bronchus and (L) main bronchus
Difference between two?
• Approximately 16 generations of branching occur from the trachea to the terminal bronchioles
• Main bronchi (primary bronchi) - lobar bronchi (secondary bronchi) - segmental bronchi (tertiary bronchi) - subsegmental bronchi - bronchioles - terminal bronchioles
Lungs
The principal organs of respiration small, air-filled
chambers where gas exchange between the air and blood takes place
Conical in shape, with its base resting on the diaphragm and its apex extending to a point approximately 2.5 cm superior to the clavicle
The lungs are attached to the mediastinum by the roots of the lungs – arrangement: pulmonary artery, superior and inferior pulmonary veins, main bronchus
Hilum
is a region on the medial surface of the lung
main bronchus, blood vessels, nerves, and lymphatic vessels, enter or exit the lung
Right Lung
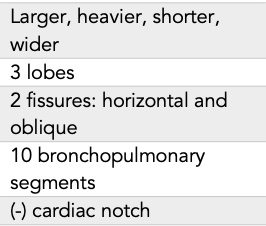
Left Lung
Alveoli
The terminal bronchioles divide to form respiratory
bronchioles, which give rise to alveolar ducts, and end as two or three alveolar sacs which are chambers connected to two or more alveoli
Small, air-filled chambers where gas exchange between the air and blood takes place
Approximately 300 million alveoli are in the two lungs
Contains elastic fibers – allow alveoli to expand during
inspiration and recoil during expiration
Lungs retain some air even not inflated, which gives
them a spongy quality
the epithelium of the alveoli and respiratory bronchioles
is not ciliated - debris from the air removed by
macrophages
Type I PNEUMOCYTES
Type II PNEUMOCYTES
Two types of cells from the alveolar wall?
Type I pneumocytes
are thin squamous epithelial cells that form 90% of the alveolar surface; where most of the gas exchange between alveolar air and the blood takes place
Type II pneumocytes
produce surfactant, which makes it easier for the alveoli to expand during inspiration
RESPIRATORY MEMBRANE
It is where gas exchange between the air and blood takes place
It is formed mainly by the alveolar walls and surrounding pulmonary capillaries
The respiratory membrane is very thin to facilitate diffusion of gases. It consists of several layers:
A thin layer of fluid lining the alveolus
The alveolar epithelium composed of simple squamous
epithelium
The basement membrane of the alveolar epithelium
A thin interstitial space
The basement membrane of the capillary endothelium
The capillary endothelium, composed of simple
squamous epithelium
Thickness of the membrane – increases as a result of
edema in the interstitial space in the alveoli
Surface area of the membrane – usually decreases in
emphysema
Diffusion coefficient of the gas – depends on gas
solubility membrane
Partial pressure difference of gas between two sides of the membrane
Factors affecting rate of gas diffusion
Diaphragm
The ______ is dome-shaped, and the base of the
dome attaches to the inner circumference of the inferior thoracic cage
Central Tendon
Located at the top of the dome is a flat sheet of
connective tissue called the ___________
Diaphragm
Contraction of the ______ results in inferior movement of the central tendon resulting to a normal quiet inspiration
Inferior
Contraction of the diaphragm results in _____ movement of the central tendon resulting to a normal quiet inspiration
Two-Thirds
Responsible for approximately _______ of the increase in thoracic volume during inspiration
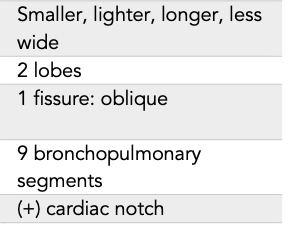
INSPIRATION
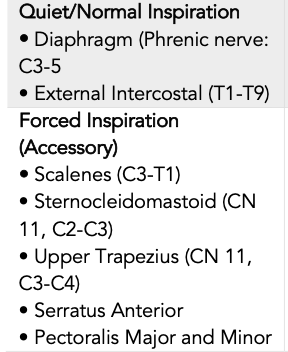
EXPIRATION
Lung Pleura
each lung is surrounded by a separate pleural cavity formed by the pleural serous membranes
Parietal Pleura
covers the inner thoracic wall, the superior surface of the diaphragm, and the mediastinum
Visceral Pleura
covers the surface of the lung. At the hilum, the parietal pleura is continuous with the visceral pleura
Pleural Fluid
acts as lubricant, holds the parietal and visceral membranes together
Pleural Pressure
Is the pressure in the pleural cavity, the thin space
between the lung pleura and the chest wall pleura
When pleural pressure is less than intra-alveolar pressure,
the alveoli tend to expand.
In a normal individual, the alveoli are always expanded. This is because there is a negative pleural pressure that is lower than intra-alveolar pressure
Pleural Pressure
amount of suction required to hold the lungs open is -5 cm H2O
Inspiration
pressure of -7.5 cm H2O expansion of chest cage
Expiration
Reversed
Goes back to -5 cm H2O
Alveolar Pressure
Pressure of air inside the lung alveoli when no air flows in and out of the lungs
Pressure is equal to the atmospheric pressure of 0 cm H2O
Inspiration
alveolar pressure falls below atmospheric pressure (-1 cm H2O) enough to pull 0.5l of air in the lungs
Expiration
alveolar pressure rises to +1 cm H2O forces inspired air to expel
Recoil Pressure
the difference between intra-alveolar pressure and
pleural pressure
measure of elastic forces of the lungs at each instant of respiration, called the _________
Compliance of Lungs
extent to which lungs will expand for each unit increase
in transpulmonary pressure
Total compliance: 200 mm of air/cm of transpulmonary
pressure (every 1 cm of H2O increase in transpulmonary
pressure, lung volume increases)
Determined by:
elastic forces of lung tissue (elastin and collagen)
elastic forces cause by surface tension of fluid lining inside the alveolar walls
Surfactant
surface active agent in water – greatly reduces surface tension of water
secreted type II alveolar epithelial cells
complex mixture of phospholipids, proteins, and ion
Produced as early as 6 to 7 months of gestation
Most important components:
o Dipalmitoyl phosphatidylcholine o surface apoproteins
o calcium ions
• The smaller the alveolus, the greater the alveolar pressure caused by the surface tension
Pump-Handle Motion
Forward and upward movement of the sternum and upper ribs (Ribs 1-6)
Increase in AP dimension
Bucket Handle Motion
elevation and outward turning of the lateral (midshaft) portions of the ribs (Ribs 7-10)
Increase in lateral dimension
Caliper Motion
lower ribs (8-12) flare and open outward
Increase in subcostal angle
Piston Action
central tendon of the diaphragm descends as the muscle contracts
Increase in vertical dimension
Automatic Breathing
by medullary respiratory center in the
brainstem, which is responsible for the rhythmicity of breathing
Voluntary Respiration
by cerebral cortex, which sends
impulses directly to the motor neurons of respiratory muscles.
Respiratory Center
Reticular formation
Sets and controls the rate and rhythm of breathing
If the pons act alone, breathing is stronger and more effective
Pneumotaxic Center (Pontine respiratory group)
Located dorsally in the upper pons
Inhibits inspiration; “switches off” the inspiratory ramp signal to control the filling phase
Controls rate and depth of breathing
Controlled by nucleus parabrachialis/nucleus proprius
Apneustic Center
Located in the lower pons
Prolongs inspiration: reverts switching off of the inspiratory ramp
Major Respiratory Control
Automatic respiratory center – Sets the inherent rhythmicity of breathing
If the medulla acts alone, breathing is weak and irregular
Dorsal Respiratory Group
Located dorsally in the medulla
“Rhythm generator”Plays a fundamental role in causing inspiration Controlled by nucleus of tractus solitarius (solitary tract)
Ventral Respiratory Group
Located in the ventrolateral part of the medulla
Controls expiration > inspiration
Controlled by nucleus ambiguus
Central Chemoreceptors
sensitive changes either in Carbon Dioxide or Hydrogen ion levels or arterial blood
Peripheral Chemoreceptors
Sensitive to partial pressure of oxygen in the arterial blood
Effects of Carbon Dioxide
Small increase in CO2 triggers large increase in rate and depth of ventilation
Chemoreceptors activity: medulla>carotid and aortic
bodies
Effects of Oxygen
Measured as PaO2 (partial pressure of oxygen)
Chemoreceptors in carotid and aortic bodies
small changes in Po2 do not cause changes in
respiratory rate.
Hering-Breuer Reflex
limits the degree to which inspiration proceeds and
prevents over inflation of the lungs
It depends on stretch receptors in the walls of the
bronchi and bronchioles of the lungs
The action potentials have an inhibitory influence on the respiratory center and result in expiration
In adults, the reflex is important only when the tidal
volume is large, such as during exercise.
Dead Space
The part of the respiratory system where gas exchange does not take place
Anatomical Dead Space
150ml
Formed by the nasal cavity, pharynx, larynx,
trachea, bronchi, bronchioles, and terminal
bronchioles.
Physiological dead space
anatomical dead space plus the volume of any alveoli in which gas exchange is less than normal (under perfused or malfunctioning)
Ventilation/Perfusion Ratio
Equal amounts of air (ventilation) and blood (perfusion) needs to be in the same place at the same time for gas exchange to occur
0.8 mL
Normal Value of Ventilation/Perfusion Ratio?
Dead Space
well ventilated, decreased perfusion (high V/Q)
Shunt
well perfusion, decreased ventilation (low)
No ventilation, but blood flow continues.
Sneeze and Cough Reflex
Both reflexes dislodge foreign matter or irritating material from the respiratory passages
SNEEZE REFLEX
occurs in the nasal passages
the soft palate is depressed, so that air is directed primarily through the nasal passages, although a considerable amount passes through the oral cavity. The rapidly flowing air dislodges particulate matter from the nasal passages and can propel it a considerable distance from the nose.
Photic sneeze reflex
17-25% of population
stimulated by exposure to bright light, such as the
sun.
COUGH REFLEX
Approximately 2.5 L of air are inspired
The vestibular and vocal folds close tightly to trap the inspired air in the lungsàthe abdominal muscles contract to force the abdominal contents up against the diaphragm and the muscles of expiration contract forcefully.àthe pressure in the lungs increases to 100 mm Hg or moreàthe vestibular and vocal folds open suddenly, the soft palate is elevatedàair rushes from the lungs and out the oral cavity at a high velocity, carrying foreign particles with it
o A forced expiration against a closed glottis
Minute Ventilation
is the total amount of air moved into and out of the respiratory system each minute
It is equal to the tidal volume times the respiratory
rate (RR X TV)
minute ventilation averages approximately 6 L/min