EMED EXAM 2 - Toxicology
1/91
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
92 Terms
Toxicology
Lecture 6: Toxicology
What is was
When they took it
How much
Why
Intent !
What is important to find out when someone comes in with a suspected OD?
1. ABCD’s, vitals, temp (rectal), other diseases, complications
2. Get BGL--> Hypoglycemia
On PE what should be done to asses a suspected OD patient?
1. GAG reflex
2. Aspiration PNA
We must do a specific evaluation of a _______ and if any question as to the integrity use active airway management to prevent _________ PNA
vent support
If respirations are <10 s/p intoxication what do we do?
1. RECTAL temp
2. Hyper= Ecstasy
3. Hypo= ETOH
Temperature
1. Always get a _______ temp
2. Hyperthermia=
3. Hypothermia=
AMS
Respiratory complications are common in patients with _______. So beware of aspiration, ARDS and bronchospasm!
Rhythm disturbances (tachyarrhythmias)
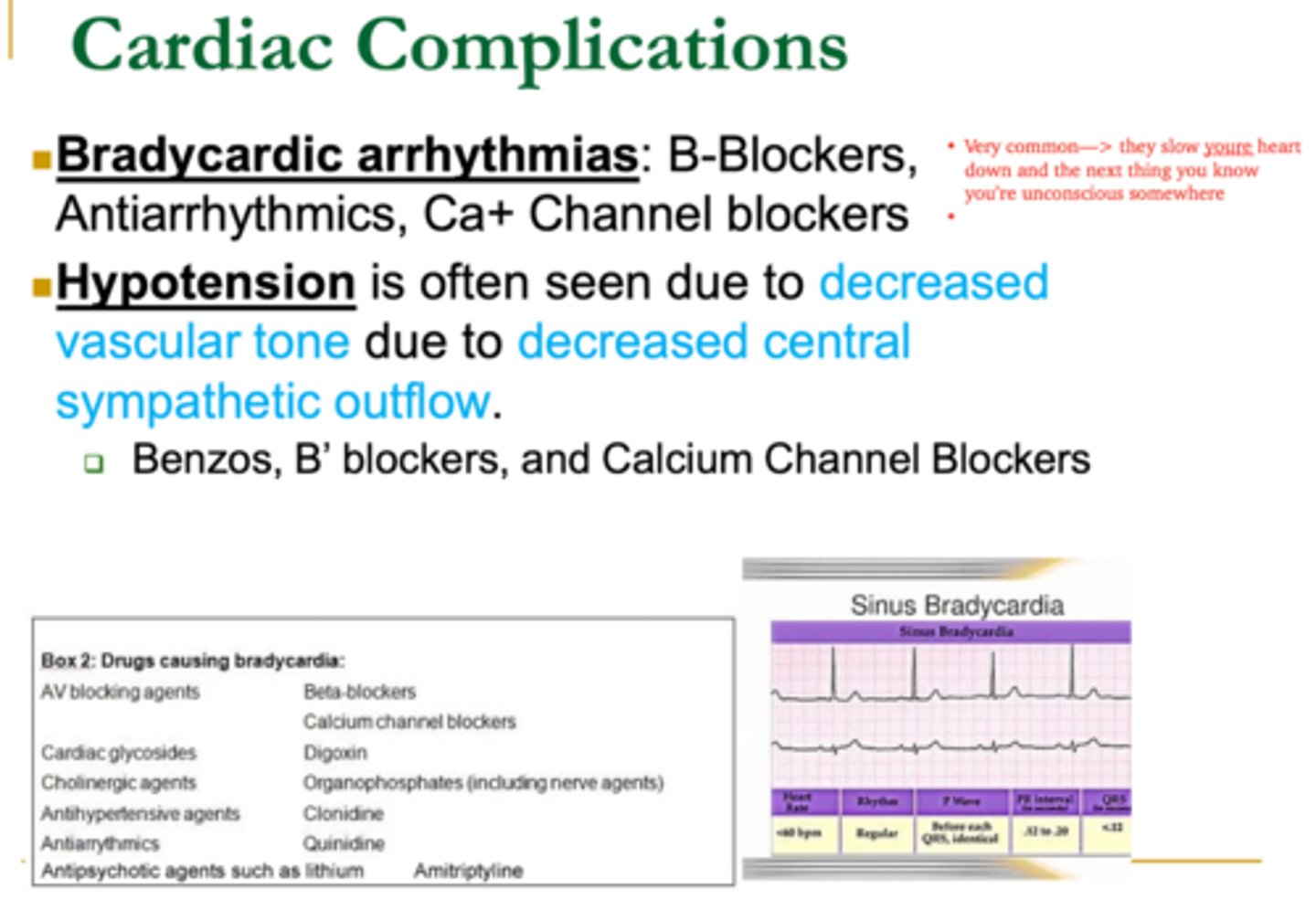
The main causes of cardiovascular complications 2/2 OD is ________ which are a common SE and usually not a cause of perfusion problem (unless very tachycardic)
1. BB
2. Anti-arrhythmic
3. CCB
What medications can cause bradycardic arrhythmias?
1. Benzo's (-pams/lams)
2. BB (-olol)
3. CCB
Hypotension is often seen due to decreased vascular tone due to decrease sympathetic outflow. What medications can cause hypotension to happen 2/2 to overdose?
1. AMS
2. Seizures
3. Behavioral
Neurologic Complications 2/2 Overdose
1. Commonly seen with _______, drowsiness, agitation, hallucinations, coma
2. This is the MOST serious complication seen!
3. Cocaine, MDMA, Amphetamine, Stimulants,PCP, Marijuana can all cause _______ abnormalities
Decontamination gastrointestinal track either by removal, prevent absorption or antidote
What is the GOAL management for an overdose patient in the ER?
1. Remove
2. Prevent absorption
3. Antidote
What is the 3 step process to Decontamination of GI tract 2/2 to overdose?
1. Gastric lavage
2. Cathartics
3. Whole Bowel Irrigation
4. Activated charcoal
What are the ways we can decontaminate the GI tract?
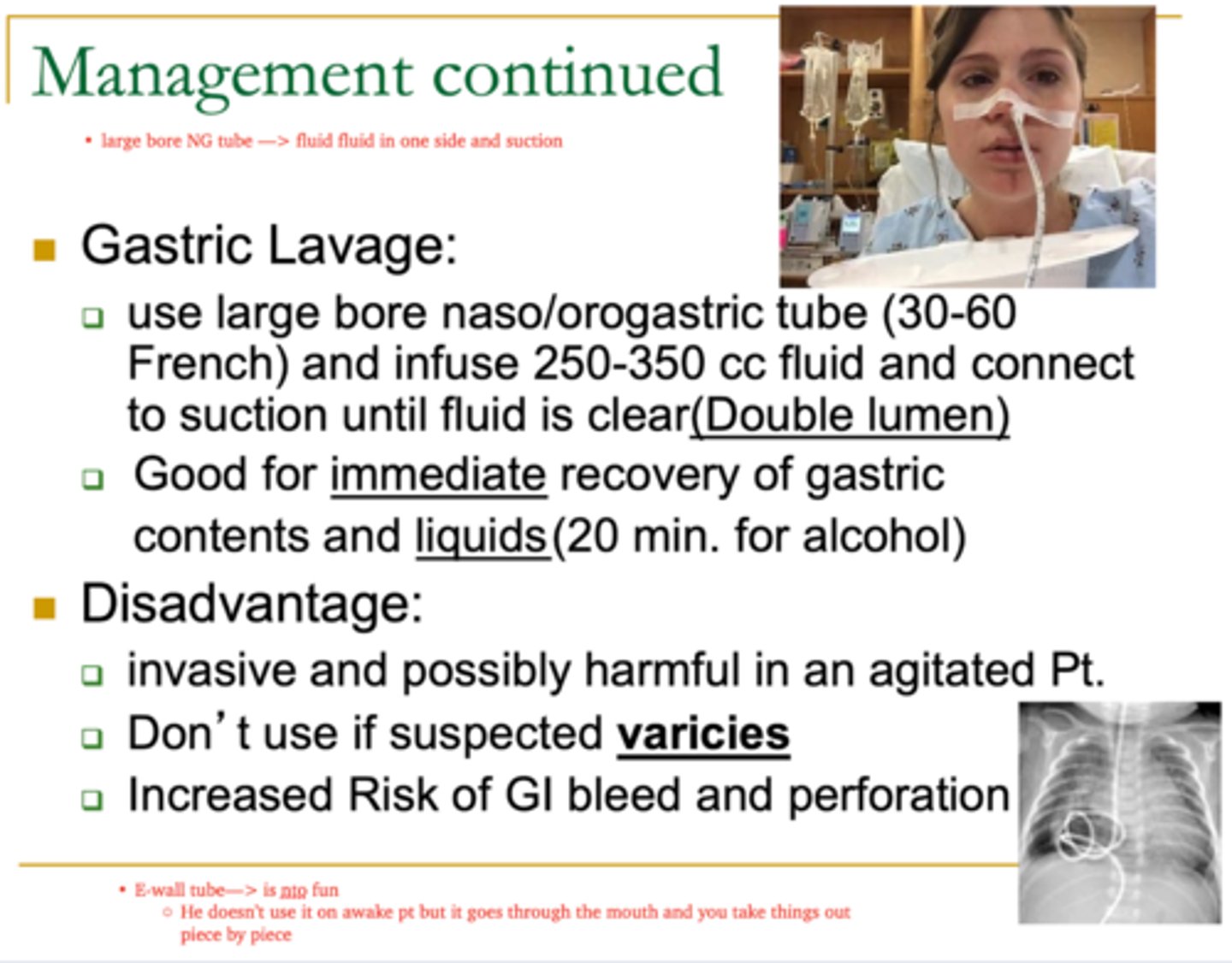
2. Immediate recovery; liquids (ETOH in 20min)
4. Varices ***
5. GI Bleed/perforation
Gastric Lavage
1. Use a Large bore NGT/orogastric tube (30-60 French) & infuse 250-350cc fluid. Connect to suction until fluid is clear (double lumen)
2. These are good for ______ recovery of gastric contents and ______
Disadvantages
3. Invasive & possible harmful in agitated pt
4. Do NOT use if you suspect _______
5. Increase risk of ____ bleed & perforation
1. Sorbitol & Mg2+ citrate
2. Inc. Motility; dec. absorption
3. Frequent liquid stools
4. Electrolyte imbalance (Mg2+, K+)
(He said he doesn't like to use it)
Cathartics
1. What are the two used?
2. It causes increase GI ________ therefore decrease GI _________
Disadvantages
3. Frequent _______ stools
4. Dehydration & __________ imbalance (_____, ______)
5. Most absorption already took place
1. Dec. absorption
2. Enteric coated meds, sustained release/poorly absorbed
3. illicit drugs
4. NGT with GO-Litely
Whole Bowel Irrigation
1. Rapidly wash GI tract to decrease _______
2. Works well in ________ meds, _______ or _______ by activated charcoal
3. Good for large amounts of______
4. Procedure uses a _____ with _____ at a rate of 1-2 L/hour until objects recovered
Disadvantages
1. Handling, collecting and discarding waste
Activated Charcoal
EXAM Q: What is the decontamination treatment of choice ?
1. Prevents absorption**
2. Within 1 hours of toxic ingestion ***
3. Dec. LOC
4. low affinity meds (IRON, Lithium)
5. GI bleed/perforation
(KNOW)
Activated Charcoal
1. This prevents _________, thats why its the TX of choice !
2. When do we need to give it?
Contraindications to using
3. Decrease _______
4. Ingestion of _______ medications (____,___)
5. Any patient with increased risk of _________
Whole bowel irrigation
What do we use if activated charcoal is CI?
*Immediate IV access: IV Thiamine + Dextrose + Naloxone
1. Thiamine: avoid wernicke syndrome in coma pt
2. Dextrose: finger stick
3. Naloxone: reverse coma, hypotension & resp. depression from OPIOIDS (need larger dose for Fentanyl)
What is the AMS cocktail?
Flumazenil (Romazicon)
This is an important adjunct to the diagnosis and treatment of benzodiazepine toxicity
1. Benzo OD
Contraindications
2. Seizures
3. Benzo's
4. TCA or Coke
Flumazenil
1. This is used for the TX of _______ overdoses
- Give small amounts to avoid AE
Contraindications
2. Hx of _______
3. Chronic use of ______
4. Co-ingestions that may induce seizures like _____ or _____
1. Anorexia
2. Elevated LFTs
3. Jaundice
4. lethargy
5. liver failure
6. N/V
(KNOW)
What are the SXS of Acetaminophen overdose?
1. AMS: Amnesia & confusion
2. Ataxia
3. Coma
4. Drowsiness/ lethargy/ sedation
What are the SXS of Benzo overdose?
1. Bradycardia & Hypotension
2. Bronchospasm & Resp depression
3. Coma
4. hyper/hypoglycemia
5. hyperK+
6. Seizure
What are the sxs of beta blocker overdose?
1. Bradycardia & Hypotension
2. Lethargy & seizures
3. Coma & dizziness
What are the sxs of CCB overdose?
1. Apnea
2. Bradycardia & hypotension
3. hypothermia & AMS
4. Pinpoint pupils
What are the sxs of clonidine overdose?
1. Hypotension, Coma, Lethargy
2. Miosis: small pupils
3. Pulmonary edema & stupor
4. Pruritis & flushing
5. N/V & seizures
What are the sxs of Opioid overdose?
1. Acidosis / Alkalosis
2. hyperventilation
3. Renal failure
4. N/V
5. Tinnitus
6. Hyper/hypoglycemia
7. Electrolyte abnormalities
8. Coma/ Diaphoresis/ disorientation
What are the sxs of Salicylates overdose?
1. Coma & Seizures
2. decreased appetite & hypoglycemia
3. Dizziness, lethargy, weakness
What are the sxs of Sulfonylurea overdose?
1. Coma, Confusion, tachycardia
2. Delirium & dilated pupils
3. Dry mouth & urinary incontinence
4. Hypotension & Seizure
What are the sxs of TCA overdose?
1. Agitation & psychosis
2. Diaphoresis
3. HTN
4. Hyperthermia
5. Mydriasis
6. Seizures & tachycardias
What are the sxs of Sympathomimetics OD? (amphetamines, caffeine, theophylline, cocaine)
Belladonna & Benadryl: “blind as a bat, mad as a hatter, red as a beet, hot as a hare and dry as a bone”
1. Delirium
2. Hyperthermia
3. Mydriasis
4. Tachycardia
5. Urinary retention
6. Warm and dry skin
What are the sxs of Anticholinergics overdose?
Physostigmine, pilocarpin
1. Bradycardia
2. Miosis
3. Bronchorrhea & wheezing
4. *Sludgem: Salivation, lacrimation, urination, defecation, Gi cramps, Emesis, Miosis
What are the sxs of Cholinergic Muscarinic overdose (organophospate or nerve gas)?
1. ABD pain
2. Fasciculations
3. HTN
4. Paresis & Tachycardia
What are the sxs of Cholinergic Nicotinic overdose?
1. Atropine (2-5mg q 3-5 minutes) PRN
2. Activated charcoal
3. benzo if seizure
What is the TX for Cholinergic OD?
1. Anticholinergics (Benadryl), sympathomimetics, Belladonna (Atropine)
2. Cholinergics, ***Opiates, clonidine
3. Phenytoin, ETOH, PCP (Phencyclidine)
What drugs change pupillary size or movement
1. Mydriasis (large Pupils)
2. Miosis (small pupils)
3. Nystagmus
MUDPILES
Methanol
Uremia
DKA
Paraldehyde
INH/Isopropyl
Lactic acidosis
Ethylene glycol
Salicylates
Normal gap= 9-16
Screen for anion-gap acidosis present in co-ingestions or lactic acidosis resulting from impaired perfusion. What are some causes of anion-gap acidosis?
True
True/False
Hypoglycemia may worsen myocardial depression or potentate seizures/arrhythmias
1. Urine Toxicology screening
2. Salicylate
3. Acetaminophen
________ toxicology screening and serum ______ and _____ levels to screen for co-ingestions
1. QT interval prolongation
2. Sinus tachycardia
3. Arrhythmias (Torsades)
4. T morphology (peaked or flattened)
5. ST segment ischemia
Must get an EKG for overdose patients to evaluate for potential life-threatening conditions like?
Head CT
If there is any head trauma associated with the overdose, what test is needed?
ME DIE
Methanol
Ethylene glycol
Diuretics
Isopropyl alcohol
Ethanol
Its important to get the urine osmolar gap plasma because it represents the unmeasured osmoses in solution. Normal level is < 15. What can be some causes for > 25 value?
1. Elevil & Nortriptyline
2. INTENTIONAL
3. Noreen & Serotonin
4. Tachycardia, HTA, Hyperrflexia, Seizures
5. Coma, Convulsions, Cardiac conduction abnormalities (QRS >100)
Tricyclic Antidepressants
1. Name a few..
2. Responsible for more _______ OD related deaths than any other meds (used to be)
3. They BLOCK the RE-UPTAKE of _____ and _____
4. What are sxs of OD?
5. What are the 3 C's for TCA OD?
1. AMS Cocktail: Thiamine/Dextrose/Naloxone
1. BICARB (QRS > 100 or >0.12 sec) & K+ IV
2. Activated charcoal within 2 hours
(GI lavage NOT recommended)
What is the TX for TCA overdoses?
1. In coma?
Need at least 3 or more of:
1. AMS
2. Tremor
3. shivering
4. diarrhea
5. Hyperreflexia
6. Myoclonus/twitching
7. Hyperthemia
8. Ataxia
What are the sxs of serotonin syndrome?
1. Clinical suspicion & Hx (NO Labs)
2. d/c MAOIs and SSRIs
Serotonin syndrome
1. Dx is made based on ______ and _____
2. TX is
1. Neurotransmitters (Dope, Norepi & serotonin)
2. HTN
3. Tachycardia & flushing
4. Tremors
5. seizures
6. Hyperthermia
7. Cardiovascular collapse
MAOIs inhibit the break down of _________ resulting in ____, ______,_____, _____, and _____.
1. Overdose
2. Drug-food interaction (Tyramine)
3. Drug-drug interaction (SSRIs & TCAs)
What are the three subtypes of MAOI OD?
1. IVF & Cardiac monitor
2. Activated charcoal
3. Short acting anti-HTN: Nitro, Labetolol or Amlodipine
4. Benzos: Ativan for seizures
5. Hyperthermia: Decrease temp by wetting body and fan
What is the TX for MAOI OD?
1. dopamine, Alpha 1&2, histamine (Phenothiazine)
2. Dystonic rx ( involuntary muscle spasms) & motor d/o
3. Tardive dyskinesia
- Akathisia: motor restlessness
- Parkinsonism: Dopamine blockage
Neuroleptic OD
1. Antipsychotics & tranquilizers (tx for schizophrenia) → act by blocking _____, ______ and ______ receptors
2. ______ reaction & _______ disorders are common
3. What other sxs can be seen?
1. Benadryl (50 mg IV) or Cogentin (2mg IV)
2. Baclofen: Tardive dyskinesia
What is the TX for neuroleptic OD?
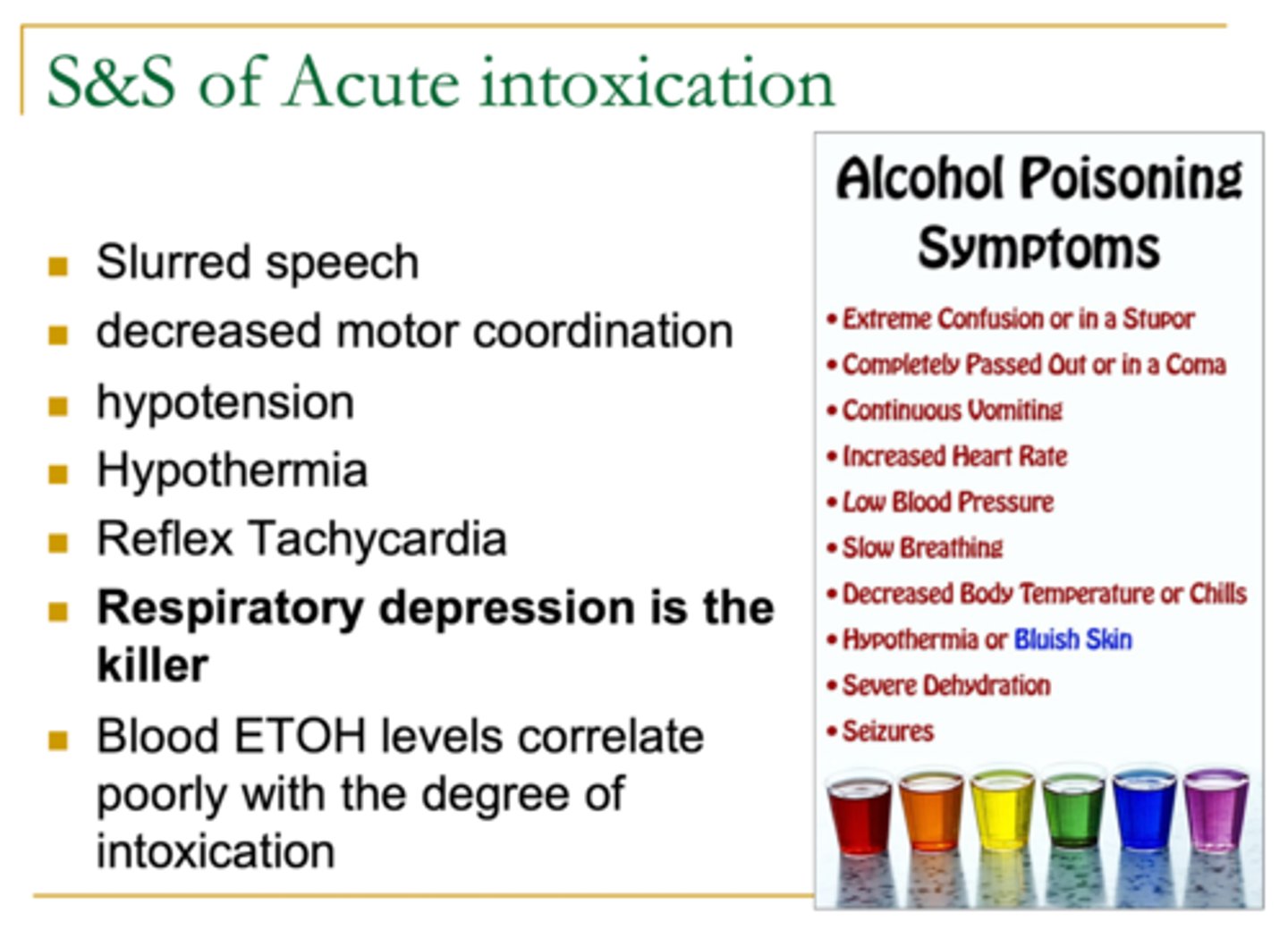
1. ETOH intoxication sxs
2. Resp. Depression: Lethargy, poor coordination, slurred speech, CNS depression, coma
3. Hypotension
4. Cardio Shock
What are the sxs of Barbiturate OD?
1. Can mimic ______ intoxication
2. __________ depression with sxs such as....
3. ______
4. Early death usually due to _______
1. Resp management: intubate
2. CXR (aspiration)
3. ABG
4. Charcoal & Gastric lavage
5. diuresis & Alkalize urine (>7.5)
6. hemodialysis
What is the TX for Barbiturate OD?
Benzodiazepines (Ativan, Xanax, Klonopin)
These are used for anxiety, insomnia, alcohol withdrawal, conscious sedation
1. Alcohol
2. FLUMAZENIL (Romazicon)
3. DO NOT induce vomiting because decreased CNS means decreased gag reflex = risk of aspiration
1. Benzo's are NOT usually lethal alone. If combined with _____ that cause them to OD
2. What is the TX for Benzo OD?
3. What should be avoided ?
ETOH
What is the MC used and abused intoxicant in the US that causes CNS depression?
resp depression
What is the killer in ETOH intoxication?
1. IVF
2. Thiamine (Banana Bag)
3. Head CT
What is the TX for ETOH intoxication?
Rubbing alcohol: Isopropanol
This is common in home. Poisoning is due to ingestion and inhalation. Since it is 2x as potent as ETOH, causes S&S to last 2x as long as ETOH. Commonly used for suicide attempts with Profound CNS depression
1. Profound CNS depression
2. Hypoglycemia 2/2 liver failure
3. Nystagmus
3. Hypotension
What are the sxs of Isopropanol intoxication (Rubbing ETOH)?
1. Smell of rubbing ETOH
2. NO AG acidosis
3. + osmolar gap
How is Isopropanol OD diagnosed?
hemodialyiss
What is the TX of isopropanol if BAC >500?
Ethylene Glycol
This is known as anti-freeze coolant that is toxic to the liver and kidney. The Lethal dose is 1g/kg and it is SWEET tasting. (children & cats like to eat)
1. seen 1-2 hours after
2. slurred speech, hallucinations & seizures
3. Tachycardia, HTN and Tachypnea
4. seen 24-72 hours
5. CVA tenderness, Acute tubular necrosis
- Oliguria, hematuria, flank pain
What are the sxs of Ethylene glycol?
1. CNS depression is seen _____ after ingestion
2. What sxs of CNS depression will you see?
3. What cardiopulmonary symptoms will be seen?
4. Nephrotoxicity is seen ______ after ingestion
5. What sxs of Nephrotoxicity is seen?
1. HX & suspicion
2. + gap acidosis & + osmolar gap
3. ***URINE for OXALATE crystals
How is Ethylene glycol OD diagnosed?
1. Sodium bicarb
2. Ethanol
3. IV crystalloid 250-500 cc/hr
4. Fomepizole**
What is the TX for Ethylene glycol?
Fomepizole
What is an ETOH antagonist that is used for the TX of Ethylene glycol?
Hemodialysis
What is the BEST method of removing toxic alcohol and metabolites?
1. Heroin
2. Pin-point pupils, AMS, Resp. Arrest, hypotension
1. What is the MC illicit narcotic used?
2. Sxs of narcotic OD?
NEAL
1. Narcan
2. Epi
3. Atropine
4. Lido
What medications can be passed down Endotracheal tube?
Cocaine
What is the Most abused stimulant in U.S → M/C/C of ED visit due to drug OD except for ETOH and tobacco**
1. tachycardia (+/- MI)
2. Seizures
3. Hemorrhage, asthma, pneumonitis, edema
4. Necrosis, ischemia, perforation seen with drug mules
5. Abortion, Abrupto placentae, induced delivery
What are the sxs of Cocaine OD?
1. Cardio toxic
2. CNS
3. Pulmonary
4. GI
5. OB
DX: Urine Tox screen
1. IVF
2. Benzo to control HTN and seizure
3. DO NOT USE BB!!!***
What is the TX for cocaine OD?
3. What must be avoided
unopposed alpha blockage
What is the reason why we dont use beta blockers in cocaine OD?
Salicylates: like ASA, Darvon, Percodan, alka seltzer
What is the #1 OD in the Elderly ?
>40 mg/dl usually toxic
What ASA level is considered toxic?
1. GI bleed, vomiting, renal failure
2. Seizures, Paradoxical fever, Resp. arrest
3. Acidosis, hyperthermia, electrolyte abnormality, PVCs, Vtach/Vfib
4. ARDS
5. Tinnitus & hearing loss
What are the sxs of ASA OD (Salicylates)?
1. IVF
2. Charcoal
3. IV N/S with BICARB (1mEq/Kg IV bolus until pH 7.4)
3. Urine alkalinization
What is the TX for ASA overdose?
1. hepatic & necrosis
2. 24-36hrs
3. 150mg/kg or 7g
4. 12 hours
Acetaminophen OD
1. Tylenol (cold and pain meds also) → causes _____ toxicity and _____
2. Hepatic injury may not become apparent until _____ post ingestion
3. Toxic dose is about _____OR _____ in adults
4. Subclinical rise in serum transaminases levels begins at about ___ hours post ingestion
1. 4000 mg
2. 7000 mg (OD dose)
You should NOT take more than _____ of acetaminophen a day (typical dose is 650mg qid). Taking more, especially ______ or more, can lead to a severe overdose if not treated.
1. n/v, anorexia
2. RUQ pain, N/V (death in 2-3 days)
3. renal failure, hepatic encephalopathy, jaundice, death
4. resolution
What are the sxs of each stage of Acetaminophen (Tylenol) OD:
Phase 1 (0-24hr)
Phase 2 (18-72 hr)
Phase 3 (72-96 hr )
Phase 4 (4 days-3 week)
1. N-Acetylcystine (Muco-mist) 21 hr IV
2. Activated charcoal with 1 hour
3. IVF
What is the TX for Acetaminophen (Tylenol) OD?
▪ Levels are high at 4 or more hours after ingestion
▪ Unknown ingestion time and APAP level >10mcg/dl
▪ > 24 hours and lab evidence of liver injury & hx of excessive ingestion
What are the indications for N-Acetylcystine for Acetaminophen OD?
8 hours
If TX with N-Acetylcystine is with ____ hours of Acetaminophen OD is nearly 100% hepatoprotective and there is a very good chance of recovery
> 2
(#2 OD in elderly)
What level of digitalis is consider toxic?
1. AV blocks or SVTs
2. HA
3. HyperK
4. bradycardia
What are the sxs of Digitalis OD?
1. Digibind
2. Activated charcoal + gastric lavage
3. Avoid K+, Ca2+ & Mg2+
What is the TX for digitalis OD?
V-Fib or asystole.
Cardiac pacing is CI in dig toxicity because of the fear of inducing ____ or _____
A. > 5.2 mEq/L with dig > 2
B. > 5.5= Die
C. < 5.0= live
Digibind Indications:
1. K+ ________ with dig level _____
2. K+ ______ → DIE
3. K+ ______ → LIVE
4. Cardiovascular collapse, co-ingestion with other drugs
They have a lot of patients
Why is a Physician Assistant always calm?