TTU A&P 1 Boros Exam 4
1/159
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
160 Terms
The Urinary System
Kidney-produces urine
Ureter-transports urine toward the urinary bladder
Urinary bladder-temporarily stores urine prior to elimination
Urethra- conducts urine to exterior
Functions of the Kidneys (1)
Excretion:
-removal of waste from body fluids in urine
Regulation of blood:
-ions
control blood NA^+, K^+, and CL^-
-pH
control blood H^+, and HCO3^- levels
-pressure and volume
control blood fluid volume and thus blood pressure
Functions of the Kidneys (2)
Kidneys accomplish this by three processes:
-Filtration of water, ions, nutrients, and waste products from the blood
-Reabsorption of most of the water, ions, and nutrients back into the blood
-Excretion of metabolic wastes into the urine
The kidneys are our heros
"Insensible" water loss is occurring as I speak and your breathe
-we lost water constantly through:
skin, lungs, and digestive system
The kidneys can regulate water volume in our bodies because they can
-concentrate or dilute the urine
The kidneys are responsible for our ability to survive on land without dehydration
The position of the kidneys
The kidneys are
-located on either side of the vertebral column
-partly protected by rib cage
The divisions of the kidney
Renal cortex
outer portion of the kidney
Renal medulla
inner portion of the kidney
-separated into renal pyramids by renal columns
Blood supply to the kidneys
Each kidney receives blood from a renal artery
It branches into many smaller and smaller arteries which
-travel between renal pyramids within the renal columns and
-ultimately deliver blood via arterioles to a capillary network called "glomerulus"
Facts about the blood supply to kidneys
Kidneys receive 20%-25% of total cardiac output
1.2 L of blood flows through kidneys each minute
The entire blood volume is filtered by the kidney 60 time/day
If the blood is filtered by the kidney were entirely excreted, your entire blood volume would be excreted in 25 minutes
(99% of the filtered blood is actually returned to the cardiovascular system)
Kidney histology
The kidney is composed of:
-nephorns
-collecting duct
The kidney contains about 1.25 million "nephrons" (85 miles in combined length)
The nephron
The nephron is the functional unit of the kidney
Urine production begins in the nephron
-blood is filtered into the nephron
-composition changes during the process
Composed of
-renal corpuscle
-renal tubule
Renal corpuscle (1)
Spherical structure is composed of:
-glomerulus
-Bowman's capsule
-urinary space
Renal corpuscle (2)
-Glomerulus
intertwining network of capillaries
receives blood from the afferent arteriole
blood leaves through the efferent arteriole
Renal corpuscle (3)
Bowman's capsule
-composed of squamous epithelial cells
-sac-like structure surrounds the glomerulus
Urinary space
-Space b/w the inner layer lining of the glomerulus and the outer layer of the capsule
Filtration of fluid from blood into the nephron
Occurs in the renal corpuscle
Blood pressure
-forces water and dissolved substances out of the glomerulus into the urinary space
-produces a protein-free solution called filtrate which is similar to blood
Three layers of filtration
The glomerulus (capillary): endothelial cell layer
Middle connective tissue
Inner lining of the Bowman's capsule: epithelial cell layer
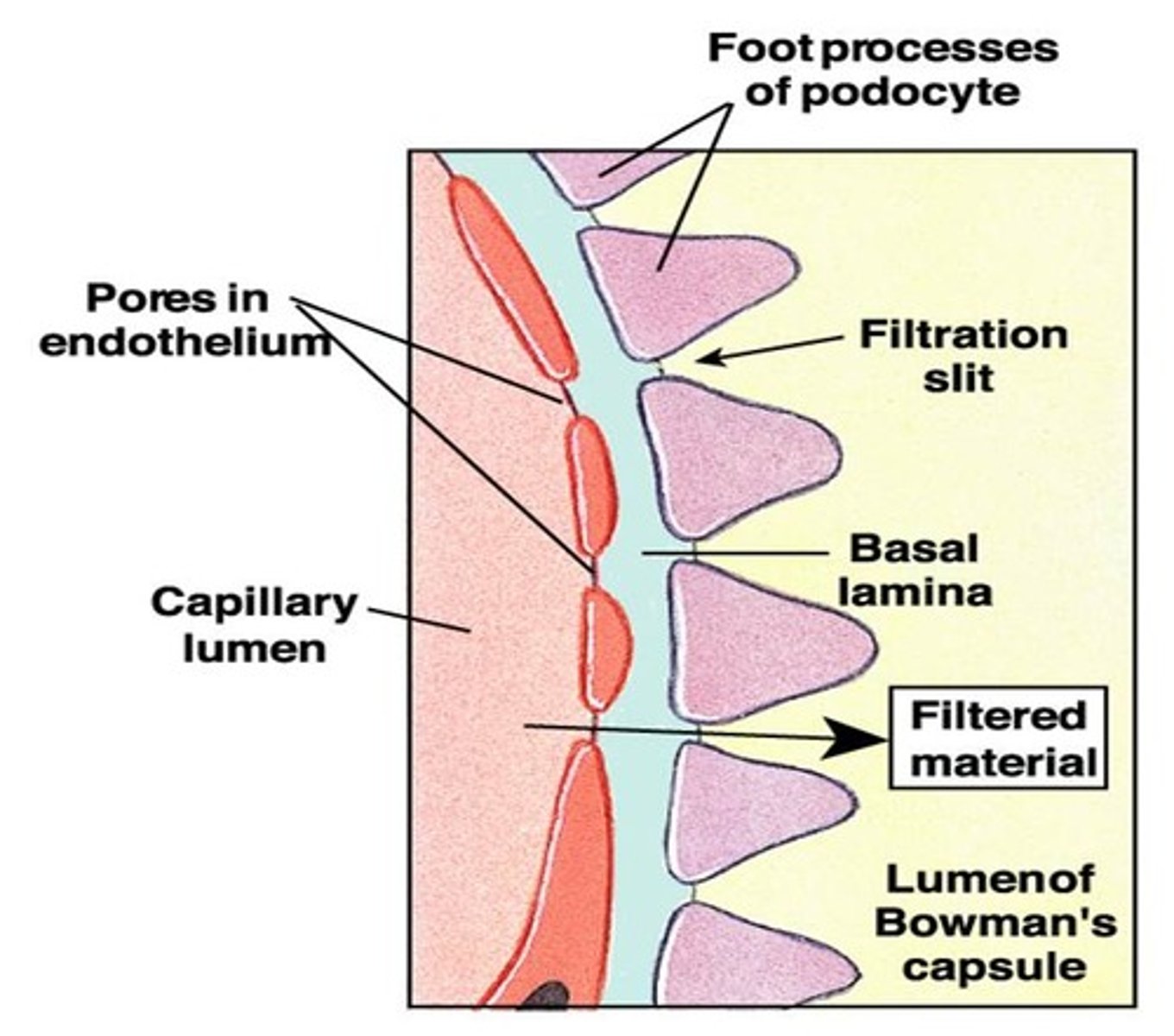
The role of the glomerular endothelial layer
Specifically, there are pores in the endothelial cells lining the glomerular capillaries
-They are small enough that they prevent passage of blood cells into the filtrate
-But they do allow some proteins to get through
Filtration slits retain proteins
The role of the podocyte later of the inner lining of Bowman's capsule (1)
However, the glomerular capillaries are surrounded by epithelial cells "foot cells" called podocytes of the inner lining of Bowman's capsule
-composed of many foot processes called pedicels
The role of the podocyte later of the inner lining of Bowman's capsule (2)
Filtration slits (narrow gaps) between adjacent pedicels of podocyte
-smaller than the pores of the endothelial cells
-They only allow water and dissolved solutes from the blood into the urinary space
Blockade of the middle connective tissue layer induces kidney diseases
The connective tissue layer between the pores and slits can become clogged with "debris"
This leads to kidney disease and to kidney failure
Renal Tubule (1)
A long u-shaped tube extending from the cortex into the medulla and back to the cortex
Renal Tubule (2)
It begins at renal corpuscle
It is composed of the:
-Proximal covuluted tubule (PCT)
-Loop of Henle
-Distal convoluted tubule (DCT)
-It ends at the collecting duct
Composition of the wall of the tubule
The wall of the renal tubule is composed of epithelial cells
-from squamous
-to columnar
-depending on the degree of activity of that portion of the tubule
Return of Filtrate from the nephron back into the blood (1)
Functions of the renal tubule cells:
-reabsorb nutrients from the filtrate
-return them to the blood
Return of Filtrate from the nephron back into the blood (2)
Functions of the renal tubule cells cont.d:
-reabsorb water (90%) from filtrate
-return it to the blood
-what is left in the tubule is excreted in the urine
-filtrate travelling along the tubule composition changes
Peritubular Capillaries and Vasa Recta
The reabsorbed water and solutes returns from teh filtrate in the tubule to the blood via
-peritubular capillaries
-vasa recta
both are branches of the efferent arteriole
they drain blood into the venous system and back to the heart
PCT (Proximal Covoluted Tubule)
The first segment of renal tubule
bulk reabsorption of filtrate occurs here
-60% to 70% of the filtrate is reabsorbed here
epithelial cells have microvilli to increase surface for reabsorption
The loop of henle
Middle segment of the renal tubule
Composed of:
descending limb
-fluid flows "down" into the medulla
ascending limb
-fluid flows "back up" into the cortex
How the loop of henle concentrates urine
-Na^+ and Cl^- are actively pumped out of the ascending limb ( and back into the bloodstream)
-Water follows out of the descending limb ( and back into the bloodstream)
-tubular fluid becomes very concentrated
urea ( most abundant organic waste from amino acid breakdown) is now the main solute left in the tubular fluid, hence "urine"
The DCT (Distal Convoluted Tubule) (1)
Last segment of the renal tubule
Note that the epithelial cells lining the DCT
-are smaller than those of the PCT and do NOT have microvilli
-these cells are less active than the cells of the PCT
-but these cells are more highly specialized than the cells of the PCT
The DCT (Distal Convoluted Tubule) (2)
Further adjustments to the filtrate are made in the DCT
-very selective reabsorption occurs here
in response to hormones
-to regulate blood pressure and volume and blood pH
The juxtaglomerular apparatus
This is the endocrine structure composed of:
-macula densa
specialized epithelial cells in the DCt
-juxtaglomerular (JG) cells
specialized smooth muscle cells of the afferent arteriole
How the DCT regulates blood pressure and volume (1)
If decreased blood pressure is sensed by the JG cells
the JG cells release renin (a hormone)
renin activates angiotensin (another hormone)
How the DCT regulates blood pressure and volume (2)
Angiotensin
-causes vasoconstriction and secretion of aldosterone (mineralocorticoid hormone) by the adrenal cortex
How the DCT regulates blood pressure and volume (3)
Aldosterone causes DCT cells:
-inc. Na^+ reabsorption (water always follows Na^+)
-Both are returned to the blood
-This inc. blood pressure and volume
How the DCT regulates blood pressure and volume (4)
If increased blood pressure or volume is sensed by stretch receptors of the heart walls, the atria of the heart releases Atrial Natriurietic Peptide (ANP hormone) causes dec. in Na^+ and water reabsorption at the DCT so inc. in Na^+ and water excretion into the urine
Results in decrease blood pressure and volume
Summary:
Dec. in blood pressure leads to
-Renin -> Angiotensin-> Aldosterone->
Inc. Na+ and water reabsorption at DCT
Inc. blood volume and therefore pressure
Less water in the urine
Urine becomes more concentrated
Inc. in blood pressure leads to
-ANP->
Dec. Na^+ and water reabsorption at DCT
Dec. blood volume therefore pressure
More water in urine
Urine becomes more dilute
How the DCT regulates blood pH
The DCT controls blood pH by both
-H^+ excretion into the forming urine
-HCO3^- (bicarbonate) production and reabsorption into the blood and also buffers the blood
The collecting duct
Determine the final urine
-composition
-volume
Hypothalamic neurons are stimulated by dec blood pressure or inc blood Na^+/Cl^- concentrations:
-they release ADH (antidiurectic hormone):
causes inc. water reabsorption at the collecting duct
Overview of the functions of the components of the nephron and collecting duct
Renal corpuscle- filtration
PCT- bulk reabsorption
Loop of Henle- concentration
DCT-fine tuning with hormones
Collecting duct-fine tuning with hormones
The collecting system of the kidney
The filtrate continues to pass through the collecting duct where its
-final composition is determined
Collecting ducts converge to empty into a minor calyx, which ends at the renal papilla of each renal pyramid
The renal calyces and pelvis
Minor calyx:
-cup-like structure surrounding each renal pyramid
-collects urine from each renal pyramid
-several join to form a major calyx
Major calyx:
-collects urine from several minor calyx
-joins to form the renal pelvis
Renal pelvis:
-acts as a funnel to drain urine from the kidney to the ureter
Urine, transport, storage, and elimination
Takes place in the urinary tract:
Ureter-transports urine toward the urinary bladder
Urinary bladder- temporarily stores urine prior to elimination
Urethra- conducts urine to exterior
The ureters
muscular tubes (smooth muscle)
-collects urine from renal pelvis
-empties urine into the urinary bladder
pass through bladder wall at an angle
-prevents backflow of urine
flatten
-as the bladder is filled with urine
-and when bladder contracts to void the urine
The urinary bladder
hollow, muscular organ (smooth muscle)
temporary reservoir for urine storage
a full bladder can contain 1 L of urine
Urothelium
AKA transitional epithelium (a type of stratified epithelium)
lines the urinary bladder and ureters
composed of cells that
-are impremeable to water
-can rearrange themselves an spread out as the bladder fills with urine
Male urethra
The male urethra is 7 to 8 inches long
Begins at the inferior pole of the bladder
-passes through the prostate gland and penis
Female urethra
The female urethra is much shorter
-1 to 2 inches long
Therefore, a female is prone to more frequent infections of urinary bladder than is the male
The external urethral sphincter
in both sexes:
-skeletal muscle surrounds the urethra
relaxation permits micturition (urination)
Components of the female reproductive system
Ovaries
Uterine tubes
Uterus
Vagina
External genitalia
-Labia
minora
majora
The ovaries (1)
the ovaries are small, almond-shaped organs
composed of:
-an outer cortex
contains follicles
-an inner medulla
contains blood vessels
Composition of follicle
-a female germ cell
"oocyte", which is surrounded by
-an epithelium layer
the epithelium type and function depends on the development
Ovary Oocyte Production Oogenesis (1)
Begins from oocyte stem cells called "oogonia"
Oogonia undergo mitosis to produce oocytes before birth
-(in spermatogonia, mitosis occurs throughout adult life)
Oogonia "sleep" until puberty
Female has all her oocytes by birth
Primordial follicle
From birth until puberty the ovary contains only primordial follicles
Composition:
-a simple squamous epithelium surrounding
-an oocyte
Primary follicle
At puberty and each month in response to FSH, about 12 primordial follicles mature into primary follicles
Epithelial cells of a primary follicle (now called "granulosa cells")
-enlarge
-divide to form a stratified epithelium
-begin to produce estrogen
Secondary follicle
Primary follicles mature into bigger secondary follicles
Epithelial cells of the secondary follicle
-continue to produce estrogen and
-begin to secrete fluid which accumulates in many small cavities between epithelial cells
Tertiary follicle
Each month, only 1 of the 12 maturing follicles develops into a bigger tertiary follicle
-the rest atrophy and degenerate
small cavities b/w epithelial cells fuse into a single large cavity of fluid called the antrum (can become an inch in diameter)
The oocyte
-bulges into the antrum
-separates from the follicle
-then floats free in atrum
Epithelial cells of a tertiary follicle produce a lot of estrogen, leading to an estrogen surge
Ovulation
The estrogen surge leads to a LH surge
The LH surge leads to:
-Ovulation: the release of oocyte from the follicle
The empty tertiary follicle (only epithelial cells left) is transformed into the corpus luteum
The Corpus Luteum (1)
Corpus luteum (yellow body)
-its epithelial cells start to produce progestrone which prepares uterine lining for pregnancy
Corpus albicans
If fertilization does not occur
-the corpus luteum:
degenerates about 12 days after ovulation
fills with scar tissue
thus becomes the corpus albicans (white body)
Hormonal Regulation of the Ovary
view image
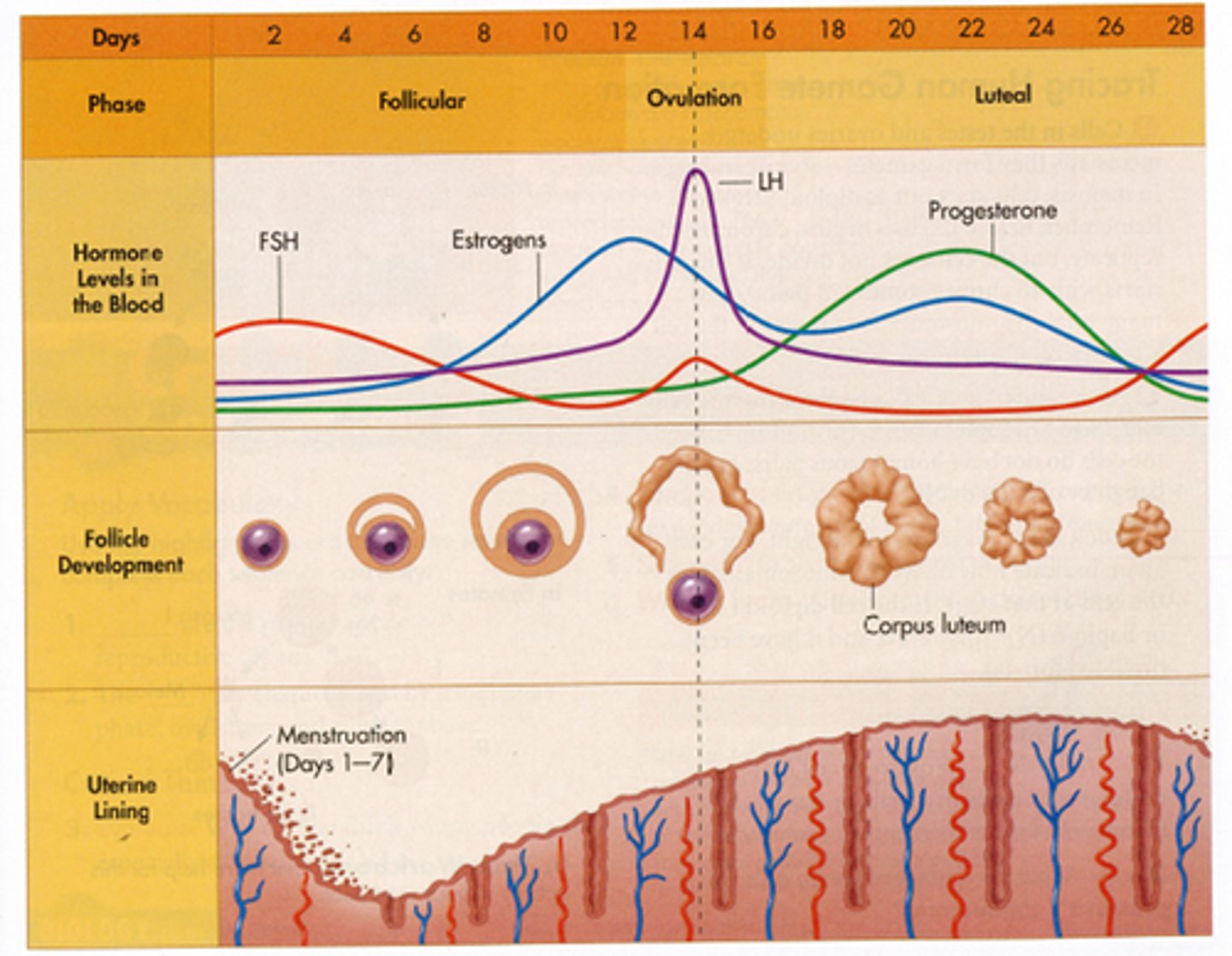
Summary of the hormones stimulating ovarian development
FSH causes:
-follicle maturation
LH causes:
-ovulation
-corpus luteum formation
Summary of the phases of the ovarian cycle
The follicular phase
-Primordial through tertiary follicles
-stimulated by FSH
-Estrogen is the primary sex hormone produced by ovaries during this phase
The luteal phase
-corpus luteum and albicans formation
-associated with LH
-progestrone is the primary sex hormone produced by ovaries during this phase
Summary of the functions of the ovaries
Produce female gametes: oocytes
Secrete female sex hormones
-estrogen
-progestrone
Fun Facts
Several million oogonia are orginally produced
Most die in the fetus
At birth:
-the ovaries contain about 2 million primordial follicles
this is all they will every produce
each containing an oocyte
By puberty:
-the number of follicles drop to about 40,000
By menopause:
-the number has dropped to 500
Probably only about 6-10 oocytes are fertilized and only 1/2 of those results in a new born
This means the safety factor for your existence is in the range of 1,000,000
The uterine tubes (1)
AKA fallopian tubes or oviducts
Hollow, muscular tubes
Transport oocyte from ovary to uterus
-oocyte transport takes 3-4 days
Tubes aren't directly connected to the ovaries
The uterine tubes (2)
Fertilization occurs in the uterine tubes near its entrance into the uterus
Unfertilized oocytes degenerate
Tubal pregnancy
Components and Functions of the uterus
Body
-largest portion of uterus
Cervix ("neck")
-distal end projecting into the vagina
The uterus provides
-protection
-nutrition
-waste removal
for a developing fetus
Three layers of the uterine wall (1)
Perimetrium
-outer layer
epithelium and connective tissue
-continuation of the broad ligament
Myometrium
-middle very thick, smooth muscle layer
-provides the force to move the fetus out of the uterus into the vagina
Three layers of the uterine wall (2)
Endometrium
inner glandular and vascular layer
-support the growing fetus
(becomes mother's portion of the placenta)
-estrogen and progesterone produced from ovary cause the glands and blood vessels of the endometrium to develop and grow each month
-if the oocyte is not fertilized, part of it is sloughed
The uterine cycle
Also called menstrual cycle "Period"
A repeating series of changes in the endometrium
Lasts from 21 to 35 days:
-average 28 days
Responds to hormones of the ovarian cycle
Consists of 3 phases
Menses (1)
the destruction of the superficial layer of the endometrium
results in
-release of blood and tissues
stimulated by decrease in progestrone
Menses (2)
Endometrial sloughing lasts 1-7 days
Sheds 35-50 mL of blood
The deeper portion of the endometrium remains to regrow the superficial portion of the next cycle
The proliferative phase
follows menses
results in
-repair and regulation of the endometrium
stimulated by
-estrogen secreted by the ovarian follicles
The secretory phase (1)
begins at ovulation
results in
-secretion by the glands
-rapid growth of the arteries
stimulated by
-progesterone secreted by the ovarian corpus luteum, persisting as long as corpus luteum does
-prepare for embryo
The secretory phase (2)
In preparation for implantation of the fertilized embryo
-the secretions will provide it nourishment
-the vessels will provide the blood ( and oxygen)
Generally lasts about 12 days if fertilization does not occur
Then the cycle is repeated and menses occurs
Summary of the relationship b/w the uterine cycle and the ovarian cycle
3 phases of uterine cycle
-menstrual phase (menses)
-proliferative phase
both occur during follicular phase of the ovarian cycle
-secretory phase
occurs during luteal phase of the ovarian cycle
The vagina
An elastic, muscular tube
Extends from the cervix to the vestibule
Between the
-urethra
-rectum and anus
Funcitions:
-
for mentrual fluids
for spermatozoa
birth canal
The clitoris
Erectile tissue (a plexus of veins)
The female external genitalia (1)
Labia majora
-contains adipose tissue
-protects inner structures
-covered with pubic hair
Labia minora
- medial to the labia major
-not covered with pubic hair
The female external genitalia (2)
Vestibule
-space between the 2 labia minora
-contains the openings for the:
urethra
vagina
The mammary glands (1)
Lie in pectoral fat pads deep to skin of chest
Composed of lobes
-each containing several secretory lobules
which drain their secretory product (milk) into lactiferous duct
most breast cancer is assoc. with the ducts
The mammary glands (2)
Nipple
-contains the openings of the lactiferous ducts
Areola
-reddish brown skin around each nipple
Secrete milk to nourish an infant (lactation)
-controlled by oxytocin
Female Sexual Response
Parasympathetic activation leads to:
-engorgement of erectile tissue of the clitoris
-increased secretion of mucus glads in the cervix and vestibule
The female orgasm is accompanied by:
-peristaltic contractions of smooth muscle in the uterus and vagina due to sympathetic activation
-rhythmic contractions of skeletal muscles surrounding the clitoris due to somatomotor activiation
Components of the male reproductive system
Testes
produce sperm portion of the semen
Duct system
transport the semen
Glands
produce fluid portion of the semen
External genitalia
penis: release the semen
scrotum
Testes
Testes (male gonads)
-egg shaped structures
-suspended in the scrotum
-contains seminiferous tubules
(1/2 mile of these tightly coiled tubules/each side) where sperm are produced in the walls of the tubules
A section through a sminiferoiu tubule: cytology
Contents of sminiferous tubules:
Spermatogonia
sperm stem cells
Sperm at different stages
Sertoli cells
Leydig cells (interstitial cells)
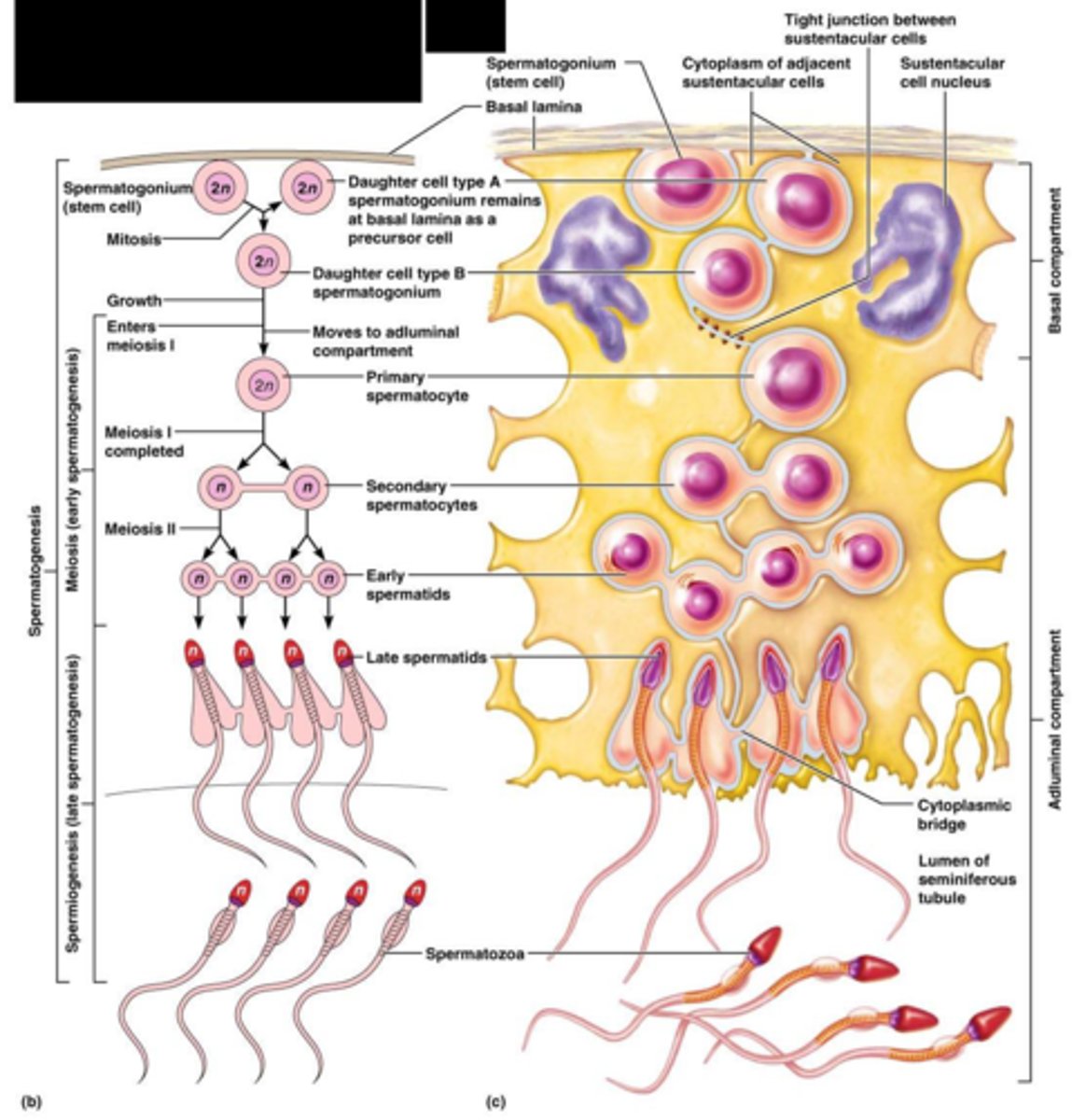
Spermatogensis: Sperm development
the continuous process of sperm production
-begins at puberty
-continues into old age (past 70)
begins at the outermost cell layer in seminiferous tubules
proceeds towards lumen
sperm are released into the lumen
Steps in spermatogensis
Spermatogonia
-sperm stem cells
-undergo mitosis and become into
Spermatocytes
-undergo meiosis and become into
Spermatids
-undergo physical maturation and become into
Spermatozoa (AKA sperm):
-lose contact with wall of the seminiferous tubule
-enter the lumen (about 9 weeks after it was generated by a spermatogonium)
Physical maturation of a sperm
view image
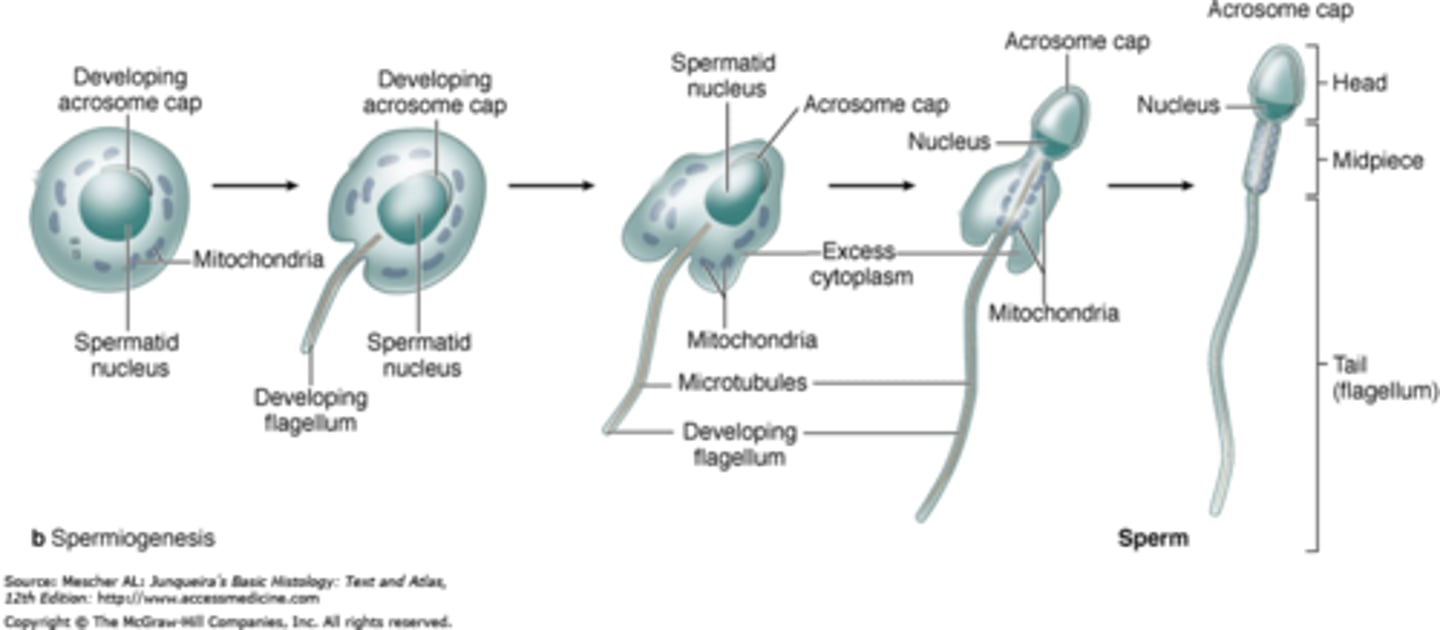
A mature sperm
Head:
-contains nucleus which carries chromosomes
all other organelles are lost, no energy reserves
must absorb nutrients from the surrounding fluid
-the tip of the head is covered by an acrosomal cap essential for fertilization
Middle piece:
-contains mitochondria to provide energy ATP to move the tail
Tail:
-is the only flagellum in the human body, a whip-like organelle to move the cell
Sertoli cells
-extended from the outer capsule to the lumen
-are supporting cells
Support spermatogensis nurture the developing sperm:
provide nutrients and chemical stimuli for development
phagocytize cytoplasm shed by developing sperm
-stimulated by hormones:
FSH and testosterone
Maintain blood-testis barrier
-formed by tight junctions between sertoli cells
-isolated developing sperm cells from blood and immune system since sperm develop after the immune system
Leydig Cells: Not inside the tubules
in the connective tissue surrounding the seminiferous tubules
stimulated by LH to produce testosterone
-the male sex hormone
Male sex hormone: testosterone
is the most important androgen
has many functions:
-stimulates spermatogenesis (maturation of spermatozoa) but not until puberty
-promotes libido (sexual drive) and related behaviors
-establishes male secondary sex characteristics
distribution of facial hair
increased muscle mass and body size
-maintains the glands and organs of male reproductive tract
Summary
Function of Testes
produce male gametes: sperm
produce male sex hormone: testosterone
Semen
Semen= Sperm + fluids
Semen is delivered by the duct system
Along the duct system taken by sperms, fluids are secreted by several exocrine glands
Pathway taken by spermatozoa the duct system: deliver semen to penis
Epididymis
Ductus deferens
Ejaculatory duct
Urethra
prostate gland portion
penis portion
The epididymis
The first part of the duct system next to the testis
a coiled tube almost 7 m long
the primary storage of sperms
-protects sperm
-recycles damaged spermatozoa
sperms leaving the epididymis are still immobile
The ductus deferens
The second part of the duct system begins at the tail of the epididymis about 18 in long
can store sperm for several months:
-in state of suspended animation (low metabolic rates)
contains smooth muscles in its wall, muscular contraction propels semen (sperm and fluid)
travels through the inguinal canal as part of spermatic cord
The spermatic cord
is the name of all of these components that follow the testes, including
-ductus deferens
-nerves
-blood vessels
-and the surrounding layers of the anterior body wall including muscles (e.g cremaster) and connective tissues
The inguinal ligament canal
The inguinal ligament forms inguinal canal
a passageway out the anterior abdominal wall through which the spermatic cord must pass
a weak point in the anterior abdominal wall