39. Diseases of the stifle joint. Diseases of the ligaments in stifle joint- LCC and LCCa and collateral ligaments. Diagnosis and treatment.
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
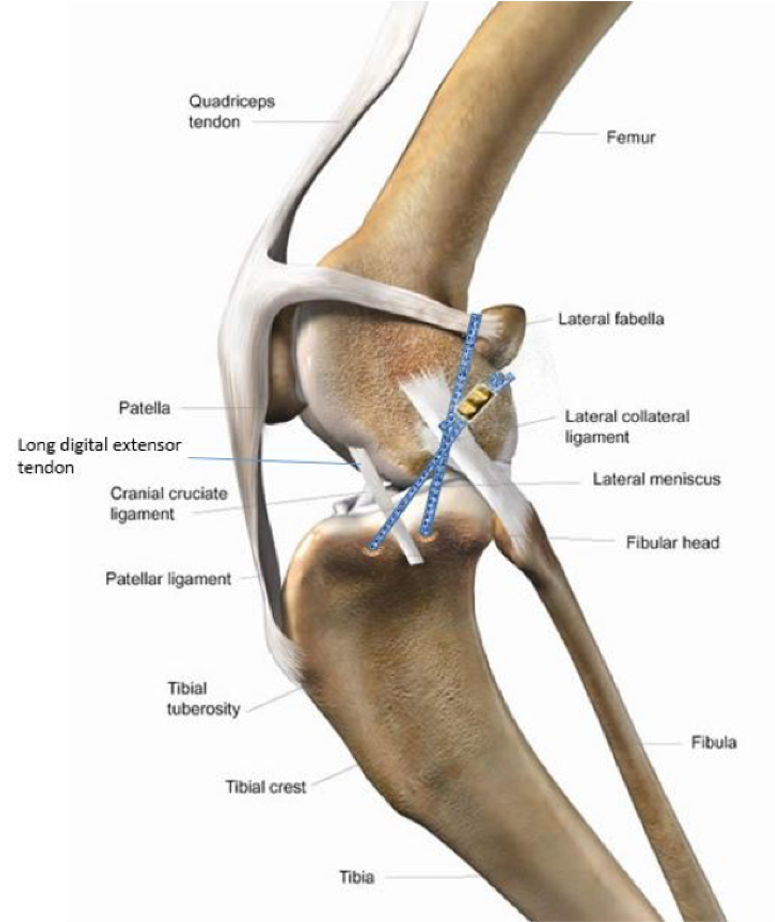
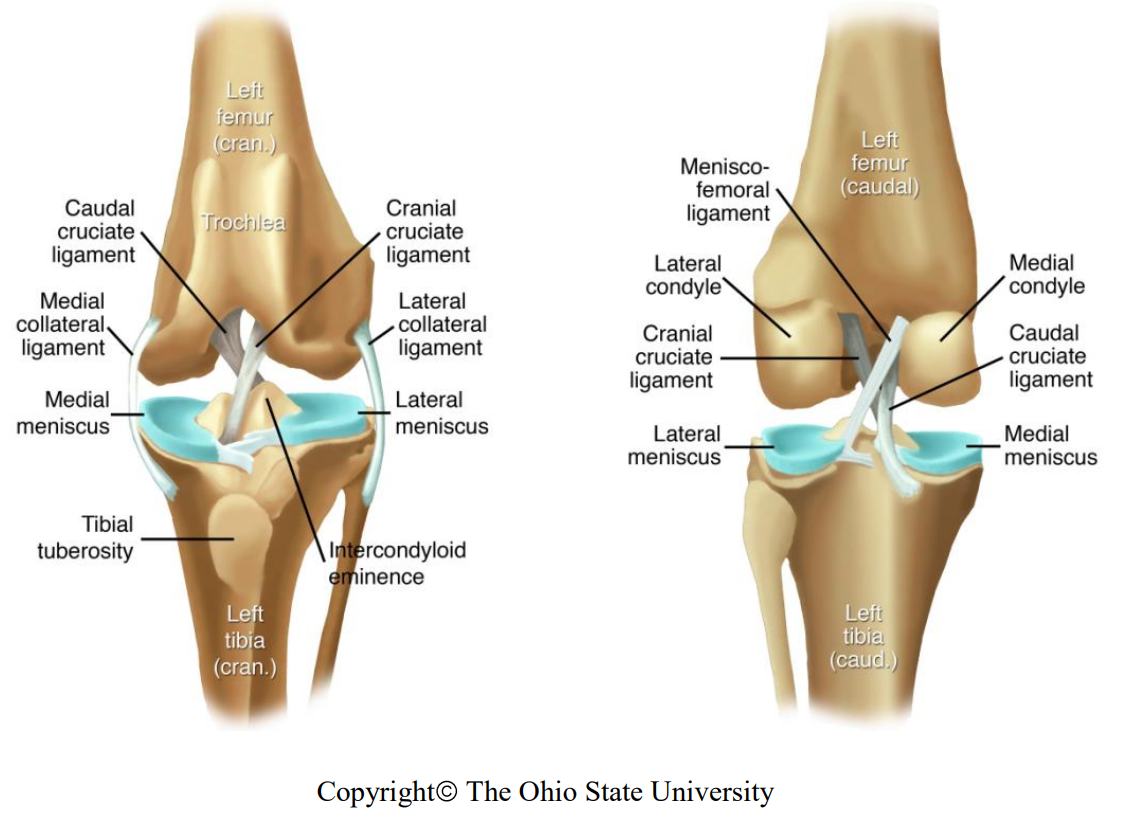
What are the collateral ligaments of the stifle?
lig. collaterale mediale
lig. collaterale laterale
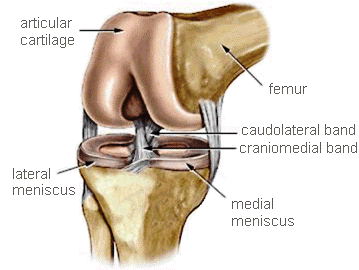
What are the cruciate ligaments?
lig. cruciatum craniale
lig. cruciatum caudale
Degenerative disorders, patella luxation, trauma, overloading, chronic stress, obesity, breed, age, sex, genetics, conformation
Lameness, effusion, osteoarthritis, muscle atrophy, positive sit test, joint instability
How is CrCL rupture diagnosed?
History: Acute: onset of non-weight bearing lameness, or chronic intermittent lameness with sudden lameness.
Positive sit test: sits with affected leg extended. It is painful to put in normal flexed position
Orthopaedic examination: distant observation, gait assessment, standing & laying palpation
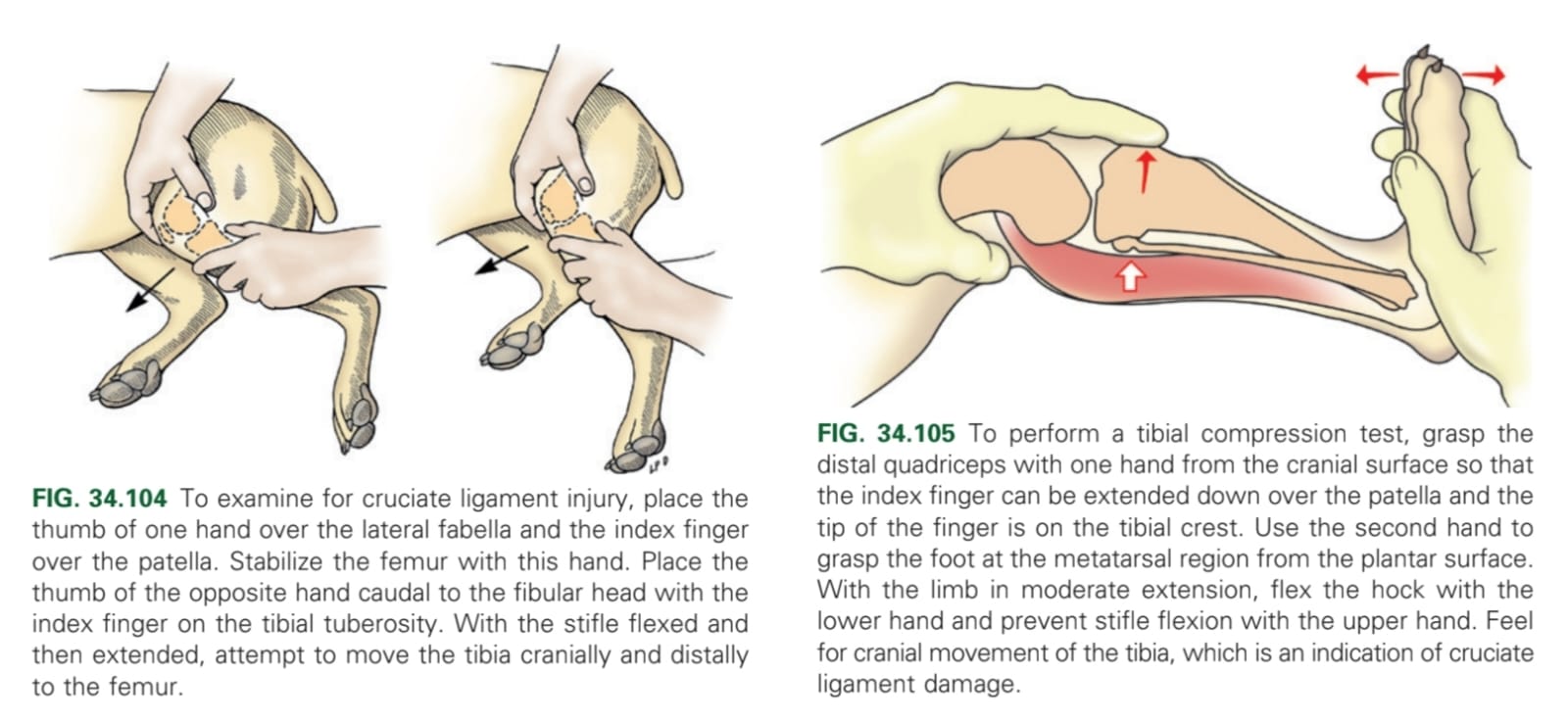
Tibial compression test (tibial tuberosity will move forward when flexing metatarsal)
Cranial drawer test (tibial tuberosity will move forward when moving tibia and femur opposite to each other)
Sit test: positive.
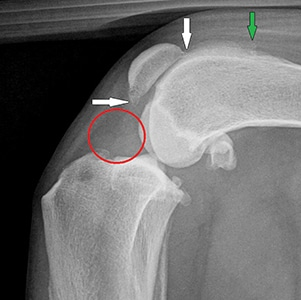
X-ray: joint effusion, decrease in size of cranial fat pad (due to joint effusion; fat pad sign), osteophytes (on apex of patella)
How is partial CrCL rupture diagnosed?
CS, fat pad signs & osteophyte on x-ray, negative cranial drawer test

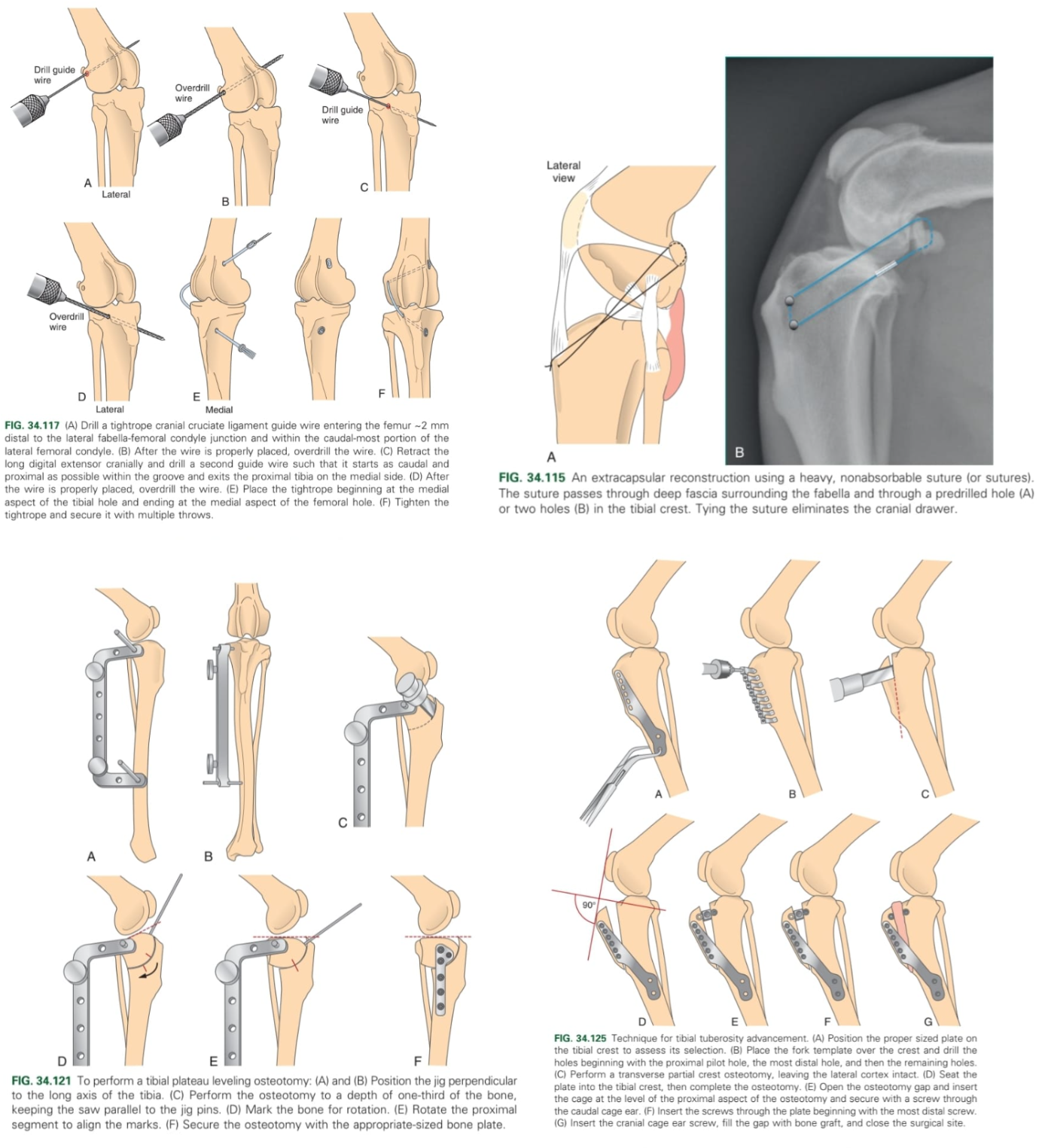
Intraarticular stabilisation – m. fascia lata
Replacing CrCL w/ a flap from m. fascia lata, going through medial side of tibia till the middle of tibial plateau then through the centre of the distal femur till lateral femur
Extraarticular stabilisation - Suture based techniques:
Fabelo-tibial stabilisation: lateral fabellotibial suture - nylon string through tibial tuberosity and around lateral fabella – mimics CCL function.
Osteotomy of tibia – modify the distribution of forces:
Tibial plateau levelling osteotomy (TPLO): corrects the slope of the tibial plateau, preventing the femur from sliding down the plateau and tibial thrust is eliminated.
Tibial tuberosity advancement (TTA): positioning of patellar ligament perpendicular to forces in the joint
What are clinical signs of CaCL rupture?
Acute lameness (though rarely causes problems)
Conservative: Reduced exercise, NSAIDs
Surgery: suture stabilisation, ligament redirection, popliteal tendon tenodesis
Prevent abduction/adduction of the stifle (stabilisation)
What are the clinical signs of collateral ligament rupture?
Variable degree of lameness
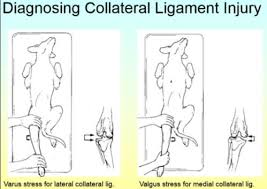
History, physical exam, palpation (stifle joint must be extended during examination)
Valgus stress test: medial collateral ligament rupture
Varus stress test: lateral collateral ligament rupture
Surgical reconstruction with sutures or prosthetic ligament