CO2/Air Flow
1/75
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
76 Terms
is O2 or CO2 the bigger driver of respiration
CO2; very important for the body to get rid of this
___________ is used synonymously w getting rid of CO2
ventilation
what are some factors (5) that can increase the body’s CO2 production
exercise
fever
eating
seizures
hyperthyroidism
what are some factors (4) that can dec the body’s CO2 production
malnutrition
hypotherimia
antipyretic therapy
neuromuscular blockade
what are the three means that CO2 is carried in the blood, rank them by % of total CO2 transport
conversion to bicarbonate 90% > dissolved in blood 6% > bound to Hb (carbamino) 4%
where does the conversion of CO2 to bicarbonate (HCO3-) take place, by what enzyme
mostly in RBC via carbonic anhydrase
what is the Haldane effect
higher % of oxygen binding to Hb dec the ability/affinity of Hb to carry CO2 as carbamino groups
what is the Bohr effect
higher % of CO2 binding to Hb dec the ability/affinity of Hb to carry O2
what is the Haldane-Bohr effect
these effects work together to onload and offload oxygen and carbon dioxide in the the lungs/tissues
describe the Haldane-Bohr effect in the lungs
Haldane: onloading O2 to dec Hb affinity for CO2
Bohr: offload CO2 to inc Hb affinity for O2
describe the Haldane-Bohr effect in the tissues
Haldane: offload O2 to inc Hb affinity for CO2
Bohr: onload CO2 to dec Hb affinity for O2

what is minute ventilation
the volume of gas exhaled per minute

what are the two variables that determine the minute ventilation
the volume of gas exhaled per breath (tidal volume; VT)
the number of breaths per minute (frequency/respiratory rate; f)
what can inc minute ventilation (6)
anxiety
pain
hypoxemia
pregnancy
liver disease
metabolic acidosis
what can dec minute ventilation (4)
opiate pain meds
altered mental status
neuromuscular weakness
metabolic alkalosis
you might expect all the minute ventilation to be devoted to gas exchange in alveoli, but not all of it does! what are the two compartments that add up to minute ventilation
dead space ventilation (VD)
alveolar ventilation (VA)
what is dead space ventilation
areas that are receiving ventilation but there is no perfusion/blood flow in the area→ cannot participate in gas exchange
what are the two types of dead space
anatomic and alveolar dead space
what is anatomic dead space, give an ex
part of the ventilation is left behind in the conducting airways and does not make it to the alveoli to participate in gas exchange; conducting zone
what is alveolar dead space, give an ex
alveoli are ventilated but are not getting an perfusion to the area; pulmonary embolism
the sum of the anatomic and alveolar dead space =
physiologic dead space
what effect will an inc of dead space fraction have on minute ventilation
will also inc in trying to maintain alveolar ventilation
what effect will an inc minute ventilation and constant dead space have on alveolar ventilation
VA will inc
if minute ventilation dec and the dead space fraction is constant what effect will this have on alveolar ventilation
VA will dec
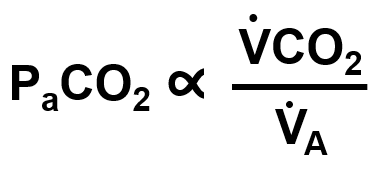
alterations in PaCO2 are due to changes in the balance of…
CO2 production and VA ; VA is affected by VE and VD
in a person who has a respiratory rate of 6 (normal is 12-20) how does this affect their PaCO2
They are taking shallow breaths (low tidal volume) at a low rate → their tidal volume will dec→ this ultimately inc the volume of the anatomic dead space → VA dec and VCO2 is constant →PaCO2 will increase
in a person who is appearing nervous and diaphoretic (sweating) and breathing deeply at a respiratory rate of 20, how does this affect their PaCO2
This patient is taking deep breaths→ meaning the tidal volume is large and the anatomic dead space volume is relatively fixed→ the VA goes up and VCO2 is fixed → PaCO2 will decrease
define hypoventilation
the level of alveolar ventilation is insufficient for your metabolic needs; high PACO2 and PaCO2 (>40 mmHg) but low PAO2
define hyperventilation
the level of alveolar ventilation is too much (in excess) for your metabolic needs; low PACO2 and PaCO2 (>40 mmHg) and high PAO2
the _____________ is the center for respiration and it is driven by ____________ and NOT by ___________
brainstem; driven by PaCO2 and NOT by PaO2
how do we get air to come into the alveoli
negative pressure
how is negative pressure created
happens during inhalation when the diaphragm flattens and pushes against its surrounding structures, stretched everything around it to increase the volume → this decreases pressure that will cause the negative pressure
specifically, what are the two mechanisms that the diaphragm uses to cause the volume of the thorax to inc
inc intra-abdominal pressure → pushes against the lower rib cage in the “zone of apposition”
lifts the rib margins up and outward
how are the lungs connected to the chest wall
the pleural space
what muscles are needed for inhalation, put asterisks (*) by the ones that are the most essential
diaphragm*, external intercostals*, scalene, sternocleidomastoid
what accessory muscles are used for forced inhalation
SCM, pectoralis major and minor, serratus anterior, latissimus dorsi
exhalation during quite breathing is entirely a ____________ (passive/active) process, therefore, there is _________ (no active/active) contraction of muscles
passive; no active
what muscles are used for tidal exhalation
none
what muscles are used for forced exhalation
internal intercostals, rectus abdominus, internal/external obliques, transverse thoracis/abdominis
what are the factors that most affect resistance (3), put an asterisk by the factor that affects resistance most
caliber*, length, and viscosity
what is caliber in Poiseulle’s Law
radius of the airway
what are the three main factors that can affect caliber
bronchoconstriction, edema (inflammation), airway secretions (mucous)
what are two other factors (aside from constriction, secretions, inflammation) that can affect caliber, explain
lung volume: more tethering inc the radius
pattern of flow: turbulent flow requires higher driving pressure→ dec radius
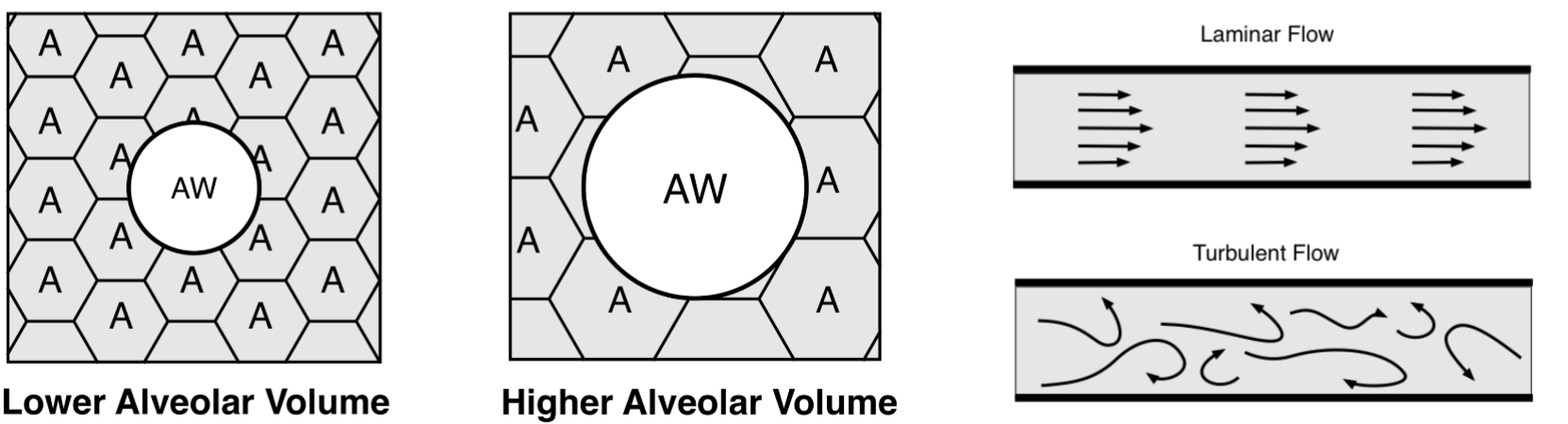
why does the volume of the lung impact the resistance in the airways
as lung volume inc, airway resistance decreases due to radial traction (tethering) from surrounding alveoli; the alveoli pull on the small airways making them wider thus reducing resistance (and you can think about it vise versa if there is dec lung volume → less alveolar tethering → inc airway resistance)
what is functional residual capacity
the resting volume of the respiratory system
FRC is determined by…
the balance of inward recoil of the lung and the outward recoil of the chest wall
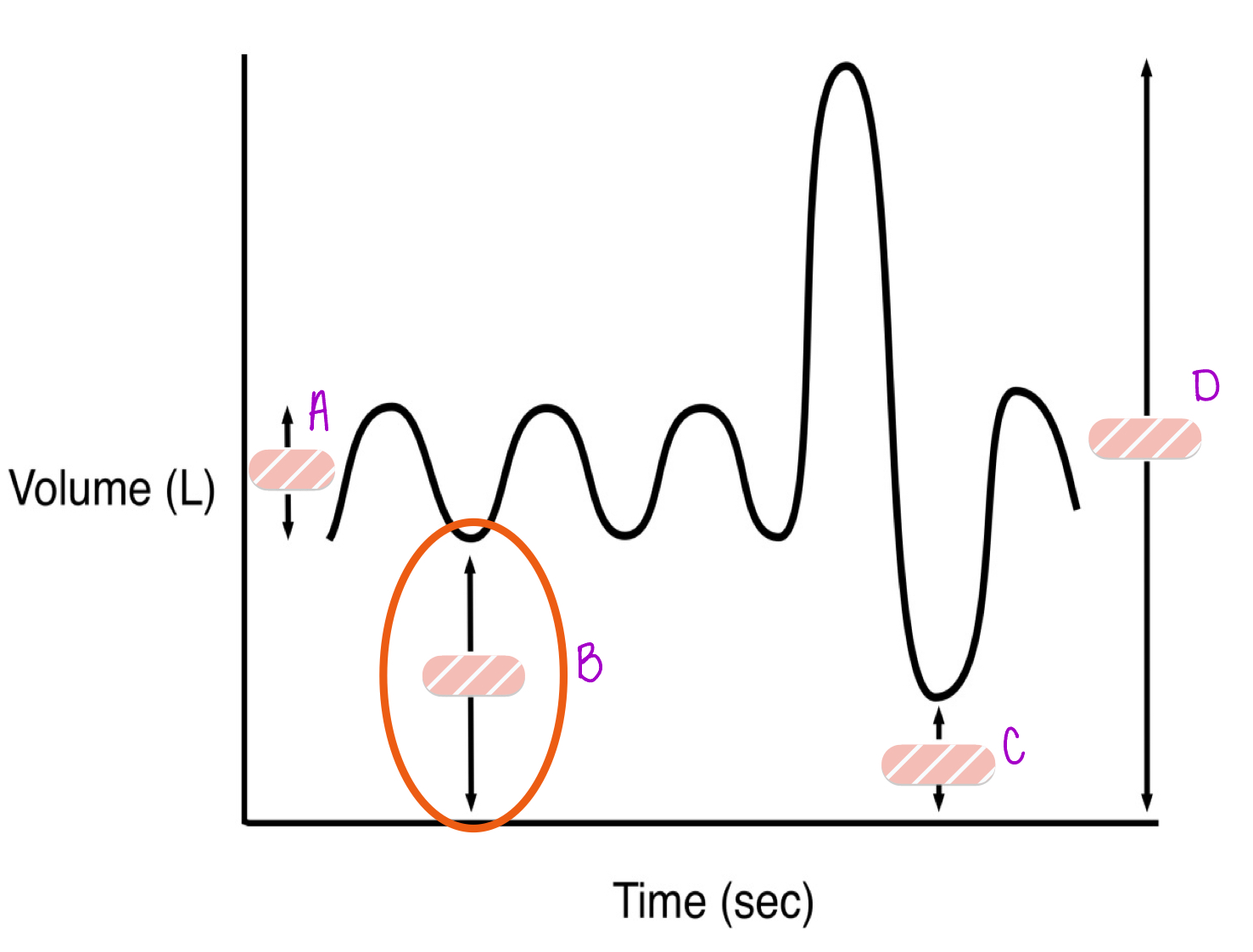
A
TV- tidal volume
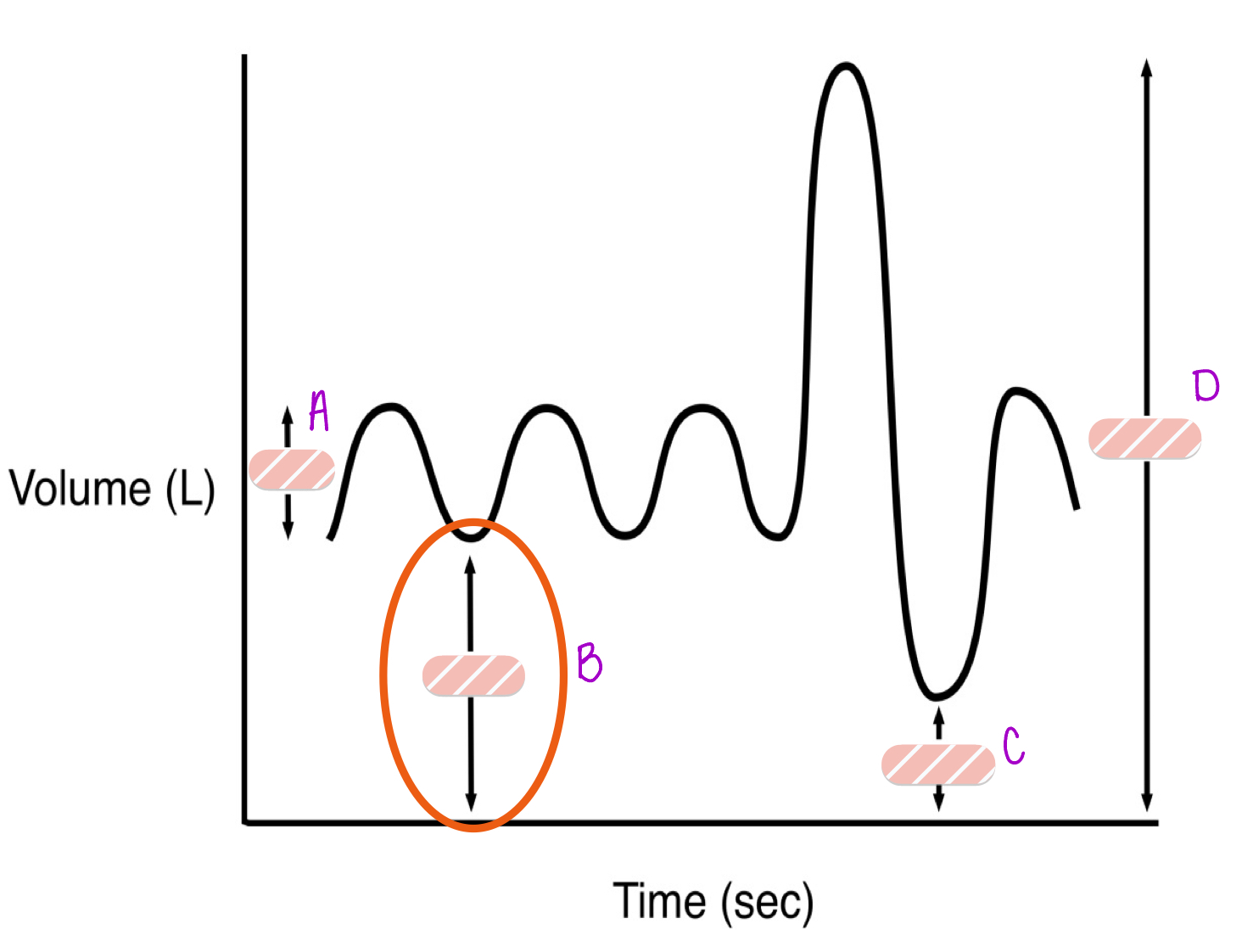
B
FRC- functional residual capacity
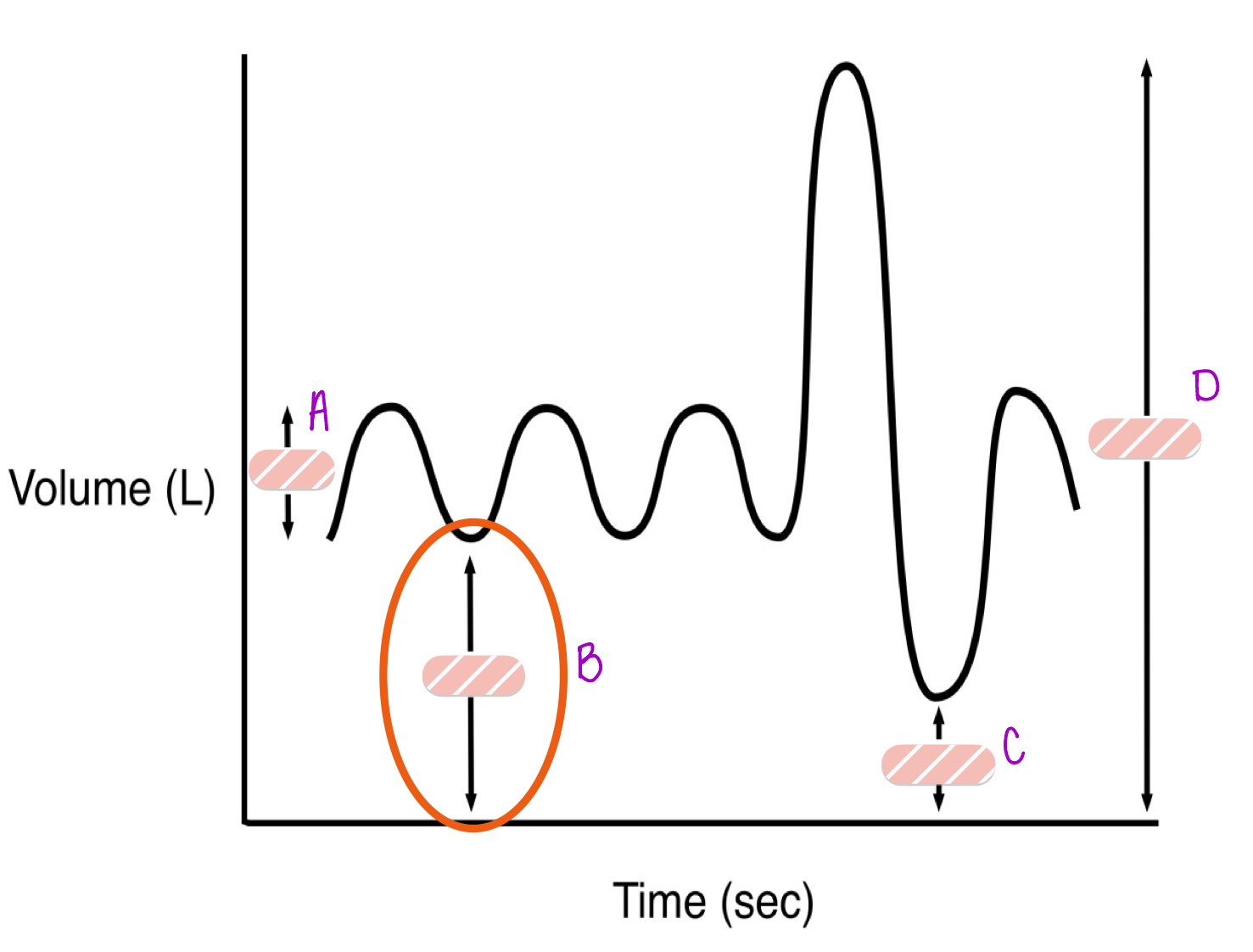
C
RV- residual volume
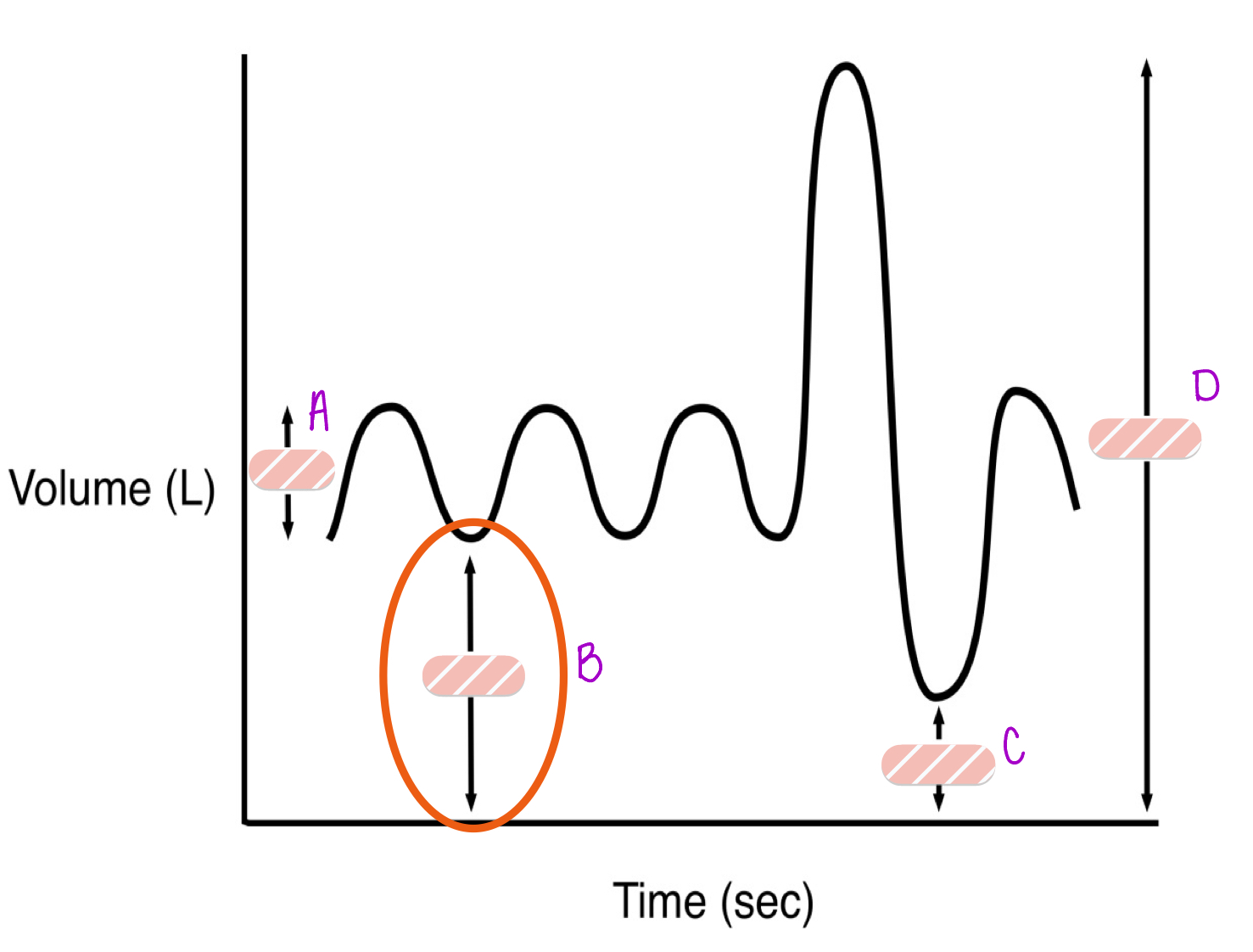
D
TLC- total lung capacity
what two factors contribute to the work of breathing
resistance and compliance
what is compliance
refers to how easily the lungs/chest respond to pressure
what are the three factors of compliance
lung parenchyma, pleural space, chest wall/abdomen
if there is a loss of lung tissue (general ex: emphysema), how does this affect FRC and compliance
there would be less elastic recoil meaning the lungs wouldn’t “snap back” as much leading to air trapping and a higher resting lung volume → inc FRC and compliance
if there is excess lung tissue (fibrosis), how does this affect FRC
there would be inc elastic recoil causing the lungs to collapse more therefore reducing the amount of air left after exhalation → dec FRC and compliance
what is transmural pressure
refers to the pressure difference across any hollow structure’s wall (inside pressure - outside pressure)
what is transpulmonary pressure
is a specific type of transmural pressure but applied to the lungs
the greater the distension away from resting volume (the more you blow the balloon up) the ________ (higher/lower) the transmural pressure
higher
FRC is determined by the balance of…
the inward recoil of the lung and the outward recoil of the chest wall
what is surfactant and how does this help alveoli
it dec surface tension in alveoli → dec tendency for alveoli to collapse → this overall inc compliance
what cells produce surfactant
type II pneumocytes
a patient w a fast respiratory rate is referred to as…
tachypneic
ventilation describes the ____ status, NOT the ___________
PCO2; respiratory rate
is pt presents w shortness of breath, fever, chills, and hypoxemia and it not responding well to supplemental oxygen, what is the likely cause
pneumonia; most common is viral but also can be bacterial Strep
what is the purpose of a ventilator
allows us to control many aspects of breathing that a fatigued and ill person cannot control by changing the TV, RR, and FIO2 concentration
in a pt w pneumonia, this acts as a dead space, why
because the sick alveoli cannot participate in gas exchange
normal PCO2 is ______ mmHg
40
we know in a pt w pneumonia, we can manipulate their PCO2 through a ventilator, how do we manipulate (inc) their PaO2
we will inc the PiO2 specifically by inc the FiO2 by bumping the standard 21% to 100% O2
in a person w pneumonia, how do we convert the alveoli that are not ventilating (dead space alveoli) to alveoli that can participate in gas exchange
killing off the offending agent w antibiotics to antivirals
in a pt w asthma, what is the primary problem
there is inc airway resistance due to bronchial smooth muscle contraction and hypertrophy, airway mucosal edema- overall narrowing the airway which will greatly impact exhalation
in a pt w asthma, why can accessory muscles be recruited for passive exhalation
pt is trying to maintain airflow normally on exhalation but due to the inc in resistance, the body needs to compensate by inc pressure gradient (driving pressure) between the alveolar space and atmosphere, this can be done by contracting abdominal muscles

is there anything wrong w this pts diaphragm
no, this is healthy!

is there anything wrong w this pts diaphragm
this is hyperinflated
what does hyperinflated mean when referring to the diaphragm
diaphragm is flat due to and inc in lung volume → air trapping
hyperinflation is a response mechanism to…
deal w inc resistance caused but can also be problematic in causing flattening of the diaphragm → dec diaphragms contractile efficiency → makes it more difficult for the pt to initiate breathing
what can cause air trapping in reference to hyperinflation
during an asthma episode, pt cannot completely exhale air with each breath so pt continues to retain air in his lungs, thus inc his lung volume