MIC 205 Exam #4: Bacterial Diseases of the Skin
1/112
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
113 Terms
Skin Microbiota normally are harmless microbes able to survive on the skin, what are they
1.) Bacteria:
Gram-positive aerobic cocci belonging to Staphylococcus and micrococcus genera
Gram-positive anaerobic bacilli, including variousdiphtheroids related to Corynebacterium diphtheriae
Yeast: Malassezia
Microbes cannot be removed completely through regular cleaning
Skin microbes may become opportunistic pathogens
Bacteria that infect the skin can cause
a wide range of diseases with mild to life-threatening consequences
Examples of Bacterial Diseases of the Skin
1.) Folliculitis
2.) Staphylococcal Scalded Skin Syndrome
3.) MRSA Infection
4.) Necrotizing Fasciitis
5.) Cat Scratching Fever
6.) Acne
7.) Pseudomonas Infections
8.) Gas Gangrene
Many viral diseases are systemic in nature, but
their signs and symptom are often expressed on the skin
Diseases caused by S. Aureeus
Follicultis
Styes
Carbuncles
Scalded Skin Syndrome
Impetigo
Toxic Shock Syndrome
Bacteremia
food poisoning
Pneumonia
3 Virulence Factors of Staphylococcal
1.) Enzymes
2.) Phagocytic Factors
3.) Toxins
Virulence Factors of Staphylococcal: Enzymes
Coagulase - forms fibrin clots
Lipase - breaks down lipids
B-Lactamase - breaks down B-lactams
Virulence Factors of Staphylococcal: Phagocytic Factors
Slime Layer- Promotes attachment
Protein A - Masks antibodies
Virulence Factors of Staphylococcal: Toxins
Cytolytic Toxins - disrupts cell membranes
Leukocidin - Disrupts leukocytes
TSS toxin - triggers fever, rash etc
Folliculitis
red, swollen bump on the skin ( pimple)
can occur at base of the eyelid (Sty)
spread of the infection can produce furuncles and carbuncles
Folliculitis is caused by
Staphylococcus Sp.
Characteristics of Staphylococcus Sp.
1.) Facultatively Anaerobic - can tolerate sealed environment of “buried” hair follicel
2.) Salt tolerant - tolerate salty human skin
3.) Desiccation Tolerant - can survive on infectious surfaces ( fomites) and skin
4.) Transmission - Direct contact between individuals or individuals
Staphylococcal Scalded Skin syndrome
skin peeling
Signs and symptoms of Staphylococcal Scalded Skin Syndrome
Cells of the outer epidermis separate from one another, and underlying tissue
Outer skin layer peels off in sheets
Pathogen of Staphylococcal Scalded Skin Syndrome
Staphylococcus Aureus
Staphylococcal Scalded Skin Syndrome is caused by
Exfoliative Toxins
Exfoliative Toxins in Staphylococcal Scalded Skin Syndrome
The toxin will cause the dissolution of the cellular bridge protein that holds adjoining cells together of the epidermis
Blood will carry the toxin throughout the body
Septicemia
Toxins in the blood stream
Pathogenesis of Staphylococcal Scalded Skin Syndrome
No scarring since the dermis is unaffected
Death is rare, but may occur due to secondary infections, such as yeast
Epidemiology of Staphylococcal Scalded Skin Syndrome
Diseases occurs primarily in infants or immune-suppressed individuals
Transmitted by person-to-person ( usually direct contact) spread of bacteria
Diagnosis, Treatment, and Prevention of Staphylococcal Scalded Skin Syndrome
Diagnosed by characteristic sloughing of the skin
Treated by the administration of antimicrobial drugs
Prevention is difficult due to the widespread occurrence of Staphylococcus aureus on the skin
Secondary Infections of Staphylococcal Scalded Skin Syndrome are
deadly
Methicillin-Resistant S. Aureus (MRSA): symptoms
May start as small red bumps ( folliculi) that develop into deep, painful abscesses
Serious infections can penetrate tissue, migrating into the bone and other vital
Pathogens and Virulence Factors of Methicillin-Resistant S. Aureus (MRSA):
Strains of Staphylococcus Aureus that exhibit resistance to methicillin; most are resistant to other antibiotics, too
Epidemiology of Methicillin-Resistant S. Aureus (MRSA):
Usually acquired by elderly and immunosuppressed patients in hospitals and long-term healthcare facilities ( HA-MRSA)
Can occur in otherwise healthy people in the form of serious skin, soft tissue, and/or pneumonia-like infections ( CA-MRSA; community-associated MRSA)
Treatment and Prevention of Methicillin-Resistant S. Aureus (MRSA):
- Typically, treated by draining and debriding abscesses, plus vancomycin and/or cocktails of other antibacterial drugs
Vancomycin-resistant MRSA, or Super-MRSA, now becoming particularly problematic.
Necrotizing Fasciitis: Signs and symptoms
Intense pain and swelling due to digestion of muscle fascia by the bacterium, easily misdiagnosed
EXTREME PAIN! PAIN OFF THE CHARTS
Pathogen Factors of Necrotizing Fasciitis
Caused by Streptococcus pyogenes
Gram positive coccus, arranged in chains ( pealrs)
Virulence Factors of Necrotizing Fasciitis
Enzymes: hyaluronidase breaks down tissue, streptokinase dissolves blood clots
Phagocytic Factors: M. Protein interferes with phagocytosis
Toxins:
1.) Exotoxin A causes toxemia and an overreactive immune response
2.) Streptolysin S kills cells, other pyrogens, stimulate fever, rash, and shock
Pathogenesis and Epidemiology of Necrotizing Fasciitis
S. pyogenes enter and breaks in the skin and will secrete enzymes and toxins
Will destroy tissues at a rate of centimeters per hours
Group A streptococci usually spread from person-to-person
about 15% of people with this infection will die
Diagnosis, Treatment, and Prevention Necrotizing Fasciitis
Difficult to diagnose in the early stages because the symptoms are nonspecific and flu-like
Treatment: clindamycin and penicillin often after very aggressive removal of infected tissues
Early treatment is vital
Acne: Pathogen and Virulence Factors
Caused by Propionibacterium Acnes in 85% of cases
Propionibacterium acnes: Gram-positive, rod-shaped diphtheroid that grow within sebaceous glands and lives on secreted sebum
Epidemiology of Acne:
Propionibacterium are normal microbiota
Begins in adolescence, can occur later
Acne: Diagnosis, Treatment, and Prevention
Diagnosed by visual detection of the skin
Treat with antimicrobial drugs, drugs that cause exfoliation, retinoic acid for sebum inhibition ( Accutane), or blue light exposure to destroy P. Acnes
Cat Scratch Fever: Signs and SYmptoms
Fever malaise, localized swelling at the site of infection and red papule
Atypical cases involve organ symptoms.
Optic nerves, Encephalopathy, and meningitis
Cat Scratch Fever: Pathogen and Virulence Factors
Bartonella henselae: gram-negative bacteria that possess the endotoxin “lipid a”
barontella can grow inside RBC and within the lining of blood vessel walls
Cat Scratch Fever: Pathogenesis and Epidemiology
Red papule, 1-2 weeks after contact
Cat scratches, bites, or by blood-sucking arthropods such as a flea
22,000 children are infected yearly
Cat Scratch Fever: Diagnosis, Treatment, and Prevention
Positive Fluorescent Antibody Test
Antimicrobial Macrolide azithromycin
Stay away from Cats and clean cat wounds
Some virulence factors of S. aureus are
resistant to some beta-lactam antibotics
Nosocomial Infection
Hospital Acquired Infections
MRSA is more common today in these areas?
Dormitories
Prisons
Contact-to-contact sports like wrestling
Pseudomonas Infection: Sign and Symptoms
Fever, chills, shock, and sometimes a green color due to the pigment pyocyanin
Pseudomonas Infection: Pathogen and Virulence
Pseudomonas Aeruginosa bacterium:
Diversity of metabolism
Found in soil, decaying matter, and the other moist environments
Pseudomonas Infection: Virulence factors
Various adhesions, toxins, and polysaccharide capsule
Elastase: can degrade components of the IM System
Produce toxic forms of oxygen that destroy the cell
Pseudomonas Infection: Pathogenis
Infection can occur in burn victims when bacteria grow under the surface.
The bacteria kills cells ,destroys tissues, and triggers shock
Pseudomonas Infection: Epidemiology
P. Aeruginosa is rarely part of the microbiota; it can cause infection throughout the body once inside
Most burn victims and C.F patients are infected.
Opportunistic pathogen and is found in most cases of immunocompromised patients
Pseudomonas Infection: Diagnosis, Treatment, and Prevention
-Diagnosis Difficult: pyocyanin discoloration ( green) = massive infection
- Treatment is complex due to the resistance of P. aeruginosa to multiple drugs and disinfectants
Been found live in disinfectants
Biofilms
Is P. Aeruginosa widespread?
Yes, it is widespread, and thus infections are not easily prevented; they typically don’t occur
Can Pseudomonas survive in bleach?
Yes, it can survive in bleach
Gas Gangrene: Causative Agent
Clostridium so.: anaerobic Gram-positive bacillus that formed endospore
Gas Gangrene: Portal of Entry
Introduction into dead (necrotic) tissue via traumatic event
Gas Gangrene: Signs and Symptoms
Pain and swelling at the injury site, fever, crackling sounds and bubbles at the site of infection, foul-smelling drainage, tachycardia
Gas Gangrene: Incubation
1 to 3 Days
Gas Gangrene: Susceptibility
The presence of deep, lacerating wounds
Gas Gangrene: Treatment
Surgical removal of dead tissue and antibiotics treatment
Gas Gangrene: Prevention
Proper cleansing of wounds
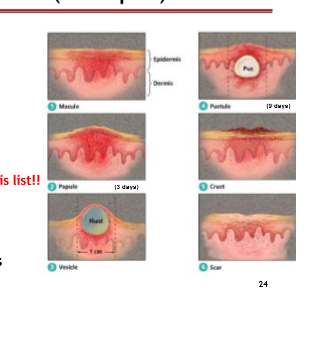
Smallpox
2-3 days severe illness before rash
Lesions first appear in mouth face, and most concentrated on face, hands, and feet
Lesions develop at once and look alike on any part of the body
Lesions change slowly, scabbing over after 9-15 days
lesions firm, dome-shaped, and deep in skin
Rash common on palms and Soles
Chickenpox
0-2 days mild illness before rash
Lesions first appear on face, trunk, and often “ patchy” and most concentrated on torso
Lesions develop in successive crops with some new, some crusting
Lesions changed rapidly, crusting over within 24 hours
Lesions are superficial pustules like water droplet on flower
Smallpox: Cause
Orthopoxvirus ( Variola virus)
Smallpox: Portal of Entry
Inhalation of viral particles
Smallpox: Signs and Symptoms
Rash that develops into papules, vesicles, and then pustules
Smallpox: Incubation
12-14 days
Smallpox: Treatment
Immediate Vaccination
Smallpox: Prevention
Vaccination discontinued in U.S in 1972
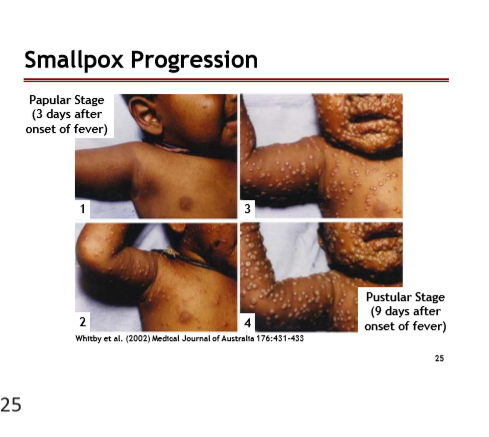
Poxvirus Diseases ( Smallpox)
Smallpox is the first human disease eradicated
Diseases progresses in stages
Poxviruses that can cause human diseases
Smallpox
Cowpox ( infects humans rarely)
Monkeypox
Stages of Poxvirus
Smallpox Progression:
Papular Stage: 3 days after onset of fever
Pustular Stage: 9 days after onset of fever
Chickenpox and Shingles: Cause
Varicellovirus ( varicella-zoster virus, VZV); part of the Herpes family
Chickenpox and Shingles: Portal of Entry
Respiratory Tract —> Blood ( liver/ spleen) —> nerve ganglia (latent). Shingles may develop in ¼ of cases
Chickenpox and Shingles: Signs/ Symptoms
Characteristic rash (CP), Location of the body & AB test (Shingles)
Chickenpox and Shingles: Incubation
2- 3 weeks
Chickenpox and Shingles: Susceptibility
Unvaccinated individuals and those who never had it
Chickenpox and Shingles: Treatment
Relief of Symptoms
Loose fitting cloths and Acyclovir “ rash pain”
Chickenpox and Shingles: Prevention
Attenuated Vaccine
Do not give aspirin to children
Reye’s Syndrome can occur after Chickenpox infection, what does it affect
The liver and brain
Herpes Infections: Signs and Symptoms
Malaise, fever, muscle pain and blister
Characteristic slowly spreading skin lesions.
Infection also occurs at various other body sites
2/3 herpes infections result in the recurrence of lesions of latent virus
Herpes Infections: Portal of Entry
Break in the skin or mucous membrane.
Virus will enter sensory nerve cells ( latent)
Upon stress, the virus will travel down the nerve to form a recurrent lesion
Herpes Simplex-1 (HSV-1): Epidemiology
Occurs via casual contact/ by age 2 & 80% of children are asymptomatic
Herpes Simplex Virus-2 ( HSV-2): Epidemiology
Most infections: Sexual contact, 15-29 years old
Diagnosis, Treatment, Prevention of HSV-1 and HSV-2
Diagnosis made by the presence of characteristic lesions
Immunoassay reveals presence of viral antigens
Chemotherapeutic drugs can help control the disease, but they DO NOT CURE IT
Warts: Cause
Caused by various papillomaviruses that are transmitted via direct contact and fomites
How many types of Human papillomavirus?
60 known types
Warts are typically seen as:
benign growths of epithelial layers of the skin
Some strains of Human papillomavirus contain what?
Oncogenes
How is Warts (HPV) diagnosed?
Direct observation
Various techniques to remove warts are available, though new warts can develop due to latent viruses.
Cryosurgery, Laser, Salicylic Acid, Duct Tape
Warts are formed on many body surfaces, what are these surfaces?
Hands and feet ( cool body reigions)
External Genitalia ( Genital warts)
Cervix
HPV ( Warts) enters through a break in the skin and infects what?
Epithelial layers and Mucous cells
Latent HPV may lead to cervical cancer in women
Not all cervical cancers are caused by HPV, and not all HPV’s cause cervical cancer.
Gardasil vaccine ( Merck) provides immunity to what?
Four HPV’s that cause 70% of cervical cancers and 90% of genital warts worldwide
7 Types of Coronaviruses:
1.) 229E ( alpha coronavirus)
2.) NL63 ( alpha coronavirus)
3.) OC43 ( beta coronavirus)
4.) HKMU1 (beta conversion)
5.) SARs-CoV-1
6.) MERs
7.) SARS-CoV-2
Coronoavirus will cause symptoms of the common cold of the upper respiratory system, but when were they first identified?
In the mid 1960s
Three Viruses of Coronavirus that can cause serious and fatal infections
1.) Sars-CoV-1
2.) MERS
3.) SAR-CoV-2
SARs-CoV-1
Originated in China in 2002
Likely originating in bat population
8098 infected/ 774 deaths ( 9.6% mortality rate)
MERS
originated in Saudi Arabia in 2012
2566 infected/ 882 deaths ( 35% mortality rate)
SARS-CoV-2
Originated in Wuhan China in 2002
32.6 million infected/580K deaths in the U.S ( 1.8% morality rate) as of 12/21
The CDC has identified the Delta and Omicron strains as variants of concern
As of January 2022, the omicron variant has caused more than 96% of COVID-19 cases in the United States
Pathogenesis of COVID-19
Attachment occurs between the virus spike protein and the ACE-2 receptor on the host cells.
Angiotensin-converting enzyme 2 (ACE-2)
primary located in the lungs, colon, and heart tissues
This enzyme is involved in regulation of blood pressure
Secondary locations are in the nose, mouth, and oral mucosa
How does COVID-19 look like at the cellular level?
Virus gains entry to lungs —> Viral replication would occur at the alveolar Type II cells —> Damage of the alveolar cells lead to an inflammation response
Severe damage is known to induce a cytokine storm
What is a cytokine storm?
Causes acute respiratory distress syndrome, blood clotting events such as strokes, myocardial infarction, kidney, liver, and other organ disfunction