INTRODUCTION TO RADIOLOGY
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
67 Terms
what characteristic of the body allows radiographs to be taken
diagnostic imaging uses radiations
the human body is partially transparent to those radiations
this partial transparency allows an image of the body to be formed
what are the major sub-disciplines in imaging
radiography
radiology
define radiography
radiography: the acquisition of the image
define radiology
radiology: the interpretation of the image and requires understanding of normal anatomy and disease processes
in which year were X-rays discovered
1895
who is considered the ‘Father of X-rays’
Wilhelm Röntgen
how are X-rays produced
when a bombarding electron interacts with either the nucleus or an inner electron shell of a metal atom such as tungsten
image of a dental X-ray tube

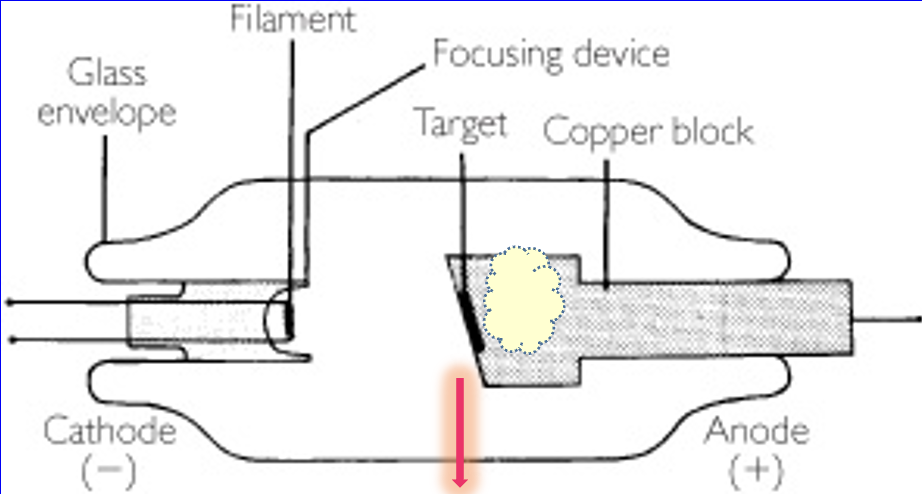
X-ray production process
X-ray tube is enclosed in a glass tube, in which is a vacuum
on the opposite end, a tungsten target is embedded in a copper block (ANODE)
the filament is a thick piece of tungsten wire
electrical current passed through the filament causes it to heat up to 2220°C and glow white hot (CATHODE)
electrons are emitted spontaneously from the white hot filament
this forms a cloud around the cathode
high voltage between the cathode and anode provides electrons an acceleration force
this emits them towards the tungsten anode at half the speed of light causing collision with the electrons around the anode
this leads to the emission of X-rays/ X-ray photons from the anode through the glass vacuum of the X-ray tube
name the processes that produce X-rays in the tungsten atoms of the anode
braking radiation
characteristic radiation
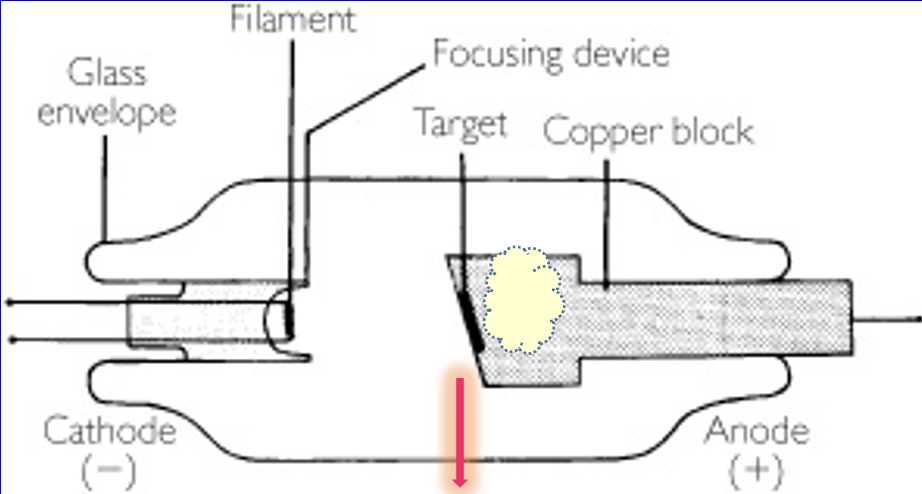
describe the process of braking radiation
incoming electron from the cathode threads its way between the different electron shells of the tungsten atom
it gets close to the nucleus of the tungsten atom
electrostatic interaction between -ve electron and +ve proton causes the electron to bend and change its path
this also causes the electron to slow down
consequently, the electron gives off some of its energy as an X-ray photon
this is emitted from the X-ray tube
—
OCCURS NEAR NUCLEUS
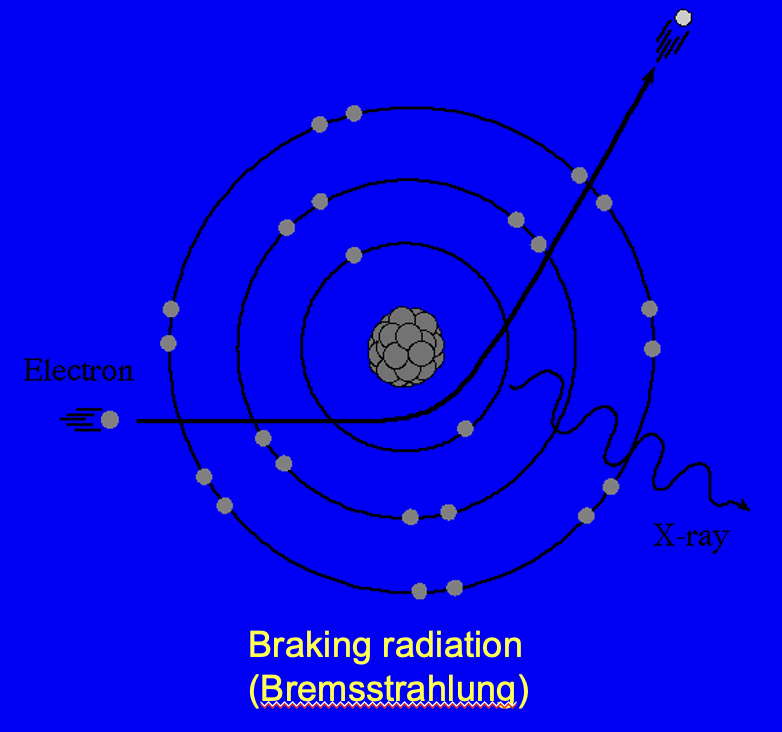
describe the process of characteristic radiation
one incoming electron collides with an inner shell electron of a tungsten atom
the incoming electron ejects the electron from the tungsten atom which leaves a space where that electron once was
another electron drops down from a higher shell
when this happens it gives off characteristic radiation
this produces X-ray photons which are emitted from the X-ray tube
the energy of characteristic radiation depends on what metal the target is made from
—
OCCURS AT INNER SHELL OF ELECTRON AROUND NUCLEUS
is it possible to alter the intensity of the X-ray beam?
yes
what factors need to change to alter the intensity of the X-ray beam? (3)
kV = kilovolt
the potential difference between the anode and the cathode
controls the penetrating power of the X-ray beam
mA = milliampere/ milliamp
how much current flows through the cathode/ the number of electrons emitted from cathode
exposure time = the duration the cathode is heated for
how does changing kV alter the intensity of X-ray beams
kV = the potential difference between the anode and the cathode
electrons flowing from cathode have more energy so when they collide with the tungsten anode they give off more energy
therefore they release more X-ray photons
X-ray film is blacker
how does changing mA alter the intensity of X-ray beams
mA = how much current flows through the cathode/ the number of electrons emitted from cathode
more current = hotter = more electrons emitted from cathode
more X-ray photons at anode
film is blacker
how does changing the exposure time alter the intensity of X-ray beams
exposure time = the duration the cathode is heated for (usually milliseconds)
increased ET emits more electrons
more X-ray photons at anode
film is blacker
IN PRACTICE which factor is the only one that can be changed
exposure time
what about kV and mA?
kV and mA are fixed in practice for dental X-ray sets
only the exposure time can be changed
what can happen when X-rays enter the human body? (3)
once X-rays pass into matter they can either be
completely absorbed - give all of its energy into matter
pass through unchanged i.e. transmitted - has the same energy exiting as it had when entering
scattered to a new direction with or without loss of energy
how is the radiographic image formed
the attenuated beam that emerges from the matter (patient) forms the radiographic image
attenuated: some photons completely absorbed, some lose energy, some scattered to a new direction
how else can X-rays be used to produce an image
in some applications X-rays can cause certain materials to fluoresce i.e. emit light
what methods can be used to capture the radiographic image
film
digital sensor
capturing the radiographic image: what is the process of film
X-ray photons that fall onto the emulsion (coating on top of film) ionise the silver bromide contained within it (X-ray sensitive)
this produces free electrons which attract mobile silver atoms to them to form a grain of metallic silver
the developing process allows this latent image to be made visible - it gets rid of the silver bromide and leaves behind metallic silver
the image formed on film is an atomic silver map of how dense the body is to X-rays passing through it
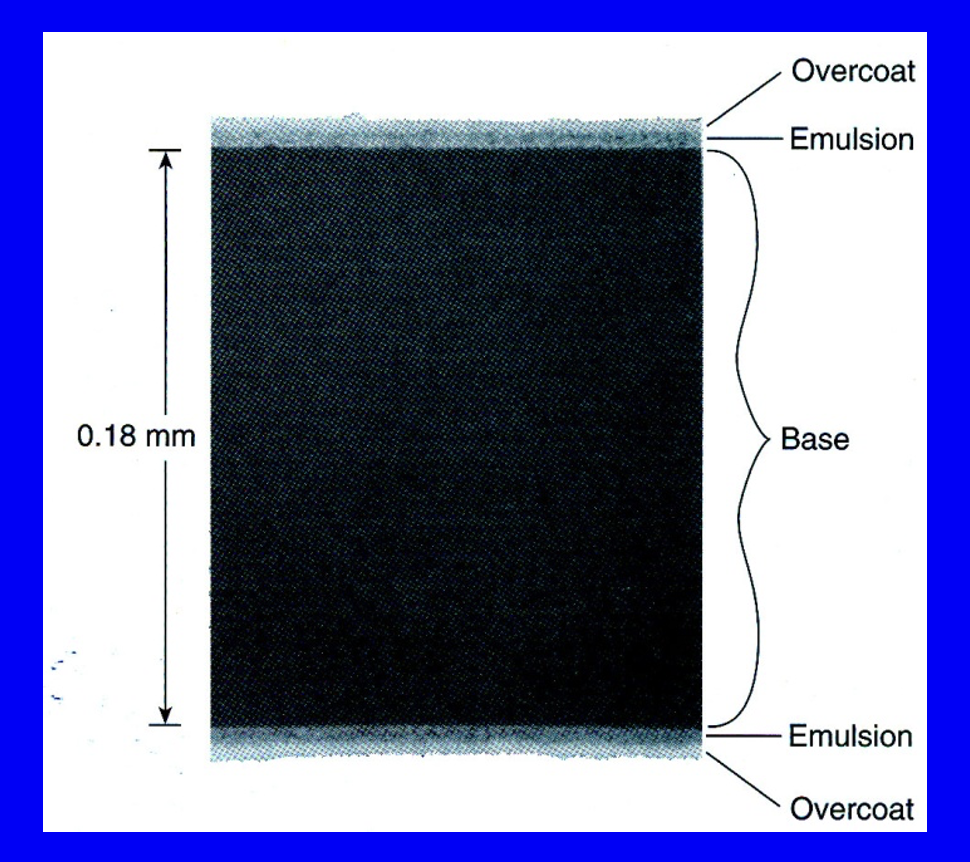
image of film
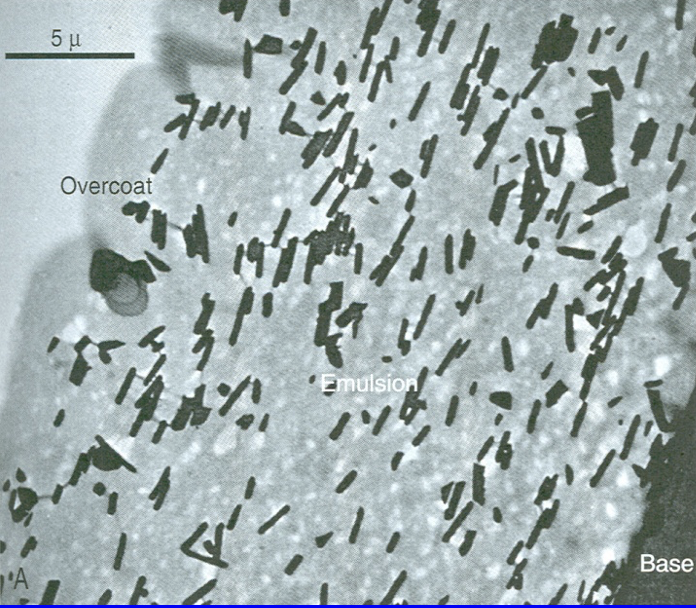
what does this electron micrograph show
silver bromide crystals = little black rods
capturing the radiographic image: how do digital sensors work
digital sensors exploit the capacity of certain materials to store X-ray energy within them, then give this out as light
some have a chemical that trap energy which is revealed in a scanning method
some uses a technology similar to a phone camera
is the use of film or digital sensors a faster way of producing a radiographic image
image produced from digital sensor is much faster than film
—
digital sensor = 5-25 secs
film ≈ 15 mins
images of digital sensors

what is a collective name for film and digital sensors
image receptor - because they detect X-rays and produces an image
where should the object/ person of interest be in relation to the image receptor when taking an X-ray
the image receptor and object/ person of interest should be parallel
the object/ person also has to be as close to the receptor as possible to prevent magnification
at what angle should the X-ray beam hit the image receptor
the X-ray beam should hit the image receptor at 90°
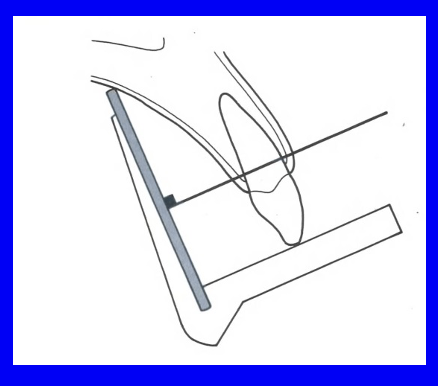
what does this diagram show
X-ray film is parallel to the long axis of the tooth
the X-ray beam passes through the tooth and film receptor at 90°
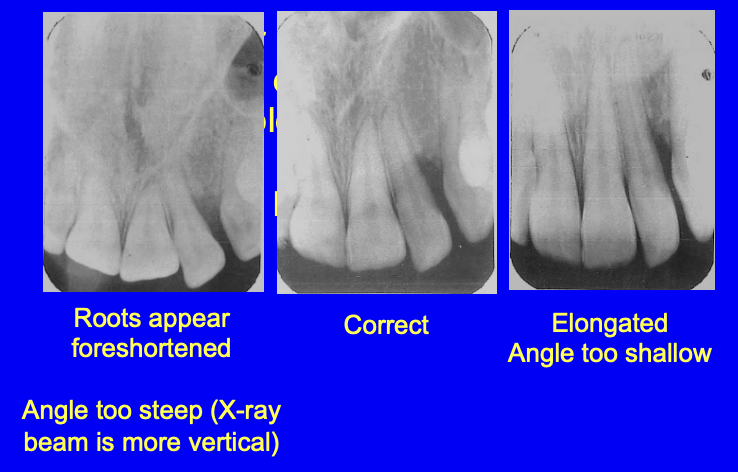
images of X-rays taken wrongly
clinically, what is used to enable the tooth + film to be parallel and the X-ray beam to hit the film at 90°?
a film holder
Hawe Super-Bite usually used

what negative effects can ionising radiation cause
skin blistering
hair loss
sunburn
why are X-rays harmful?
when ionising radiation e.g. X-rays interact with living tissues, some of it is absorbed by the tissue
chemical changes then occur almost instantly in the tissue
this can lead to molecular damage in seconds to minutes
after this, over hours e.g. sunburn to decades, biological damage can occur
what is the primary reason radiation damages tissue
radiation damages tissue primarily because it causes chemical changes in tissue by ionisation
define ionisation
ionisation: the process whereby atoms or molecules gain or lose electrons to acquire a negative or positive charge
what molecules are thought to be ionised
cellular enzymes e.g. those that control cell division and DNA (cannot be observed directly)
what is a direct effect of radiation
direct effect of radiation
breaking of bonds between atoms
what is an indirect effect of radiation
indirect effect of radiation
damage by the production of free radicals
these are powerful oxidisers that can rearrange organic molecules
—
H2O + radiation = H2O+ + e-
H2O+ » H+ + OH.
the positive water ion does not exist for very long
it immediately disintegrates into H+ and the hydroxyl free radical
how does damage to DNA and enzymes affect cells
inhibits cell division
causing direct cell death » tissue damage
causing a cell to transform i.e. uncontrolled cell division
what can cell transformation/ uncontrolled cell division lead to
development of a radiation-induced cancer
what is the term for the effects that lead to
cell damage » cell death » tissue damage
deterministic effects
what is the term for the effects that lead to cell transformation
stochastic effects
what is the pattern of the occurrence of stochastic effects
stochastic events are random
they occur by chance
what is the chief stochastic effect from X-rays
development of a radiation-induced cancer
do stochastic effects have a threshold?
no - there is no safe dose of radiation where your chances of developing a stochastic effect is 0%
what is the correlation between radiation dose and chances of developing a stochastic effect
positive correlation
as radiation dose increases the chances of developing a stochastic effect increases
the severity of the effect i.e. tumour does NOT change
list the harmful tissue effects of radiation
skin reddening/ skin burning
hair loss
cataracts - if eye is irradiated
foetal developmental abnormalities
all harmful tissue effects have a _________
threshold
explain what the threshold dose is
less radiation than the threshold dose to cause a harmful effect means the effect will not occur
if the threshold is exceeded then an increasing number of people will show the effect
what is the major risk to patients from dental X-rays
the stochastic (random) triggering of a radiation-induced cancer
what type of cancers are usually radiation-induced
blood cancers
leukaemia: takes 5-10 yrs to develop
connective tissue cancers
sarcoma: takes 20-40 yrs to develop
how many cases of radiation-induced cancers occur in the UK annually
≈ 1000 cases
how many of those 1000 cases come from dental X-rays
≈ 10/1000 come from dental X-rays (impossible to tell which patients they are)
explain the term ‘effective dose’
effective dose
a measure used to estimate the risk of developing a radiation-induced cancer from an imaging technique using ionisation radiation
unit of measurement = Sievert (Sv)
milli- and micro- Sv are used in the context of radiation dosage from imaging tests - because one Sv is a huge amount of radiation
can a radiation-induced cancer be differentiated from a non radiation induced cancer i.e. normal disease?
no, radiation-induced cancers look just like normal disease clinically and histologically
_ in _ will die naturally from cancer in the UK
1 in 4 will die naturally from cancer in the UK
what is the current annual exposure of the average UK resident to radiation
2.7mSv per yr - depends where you live
at least 50% comes from radon gas

list the radiation protection principles developed by the International Commission on Radiological Protection (ICRP)
justification
optimisation
dose limitation
radiation protection principals: explain the ‘justification’ principal
JUSTIFICATION
ionising radiation should only be used if the benefits of having the test done exceed the risks to the patient being exposed
easier to justify smaller doses compared to larger doses (risk is proportional to dose)
radiation protection principals: explain the ‘optimisation’ principal
OPTIMISATION
if exposing the patient to ionisation radiation is justified, then the dose should be as low as reasonable practicable (ALARP principal)
radiation protection principals: explain the ‘dose limitation’ principal
DOSE LIMITATION
there should be a system of dose limits
doses greater than the limits cannot be justified - no matter the benefits