Blood Physiology lecture 2 (RBC & WBC)
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
57 Terms
What does erythropoietin (EPO) cytokines do as a factor for affecting RBC production?
stimulates RBC production
What dietary factors are needed for RBC production?
iron needed in Hb, folic acid, and vitamin B12
Why is intrinsic factors important for RBC production?
made by cells in the stomach and needed for absorption of vitamin B12
What stimulates erythropoietin (EPO)?
decreased oxygen delivery to the kidneys
erythropoietin (EPO) acts on:
bone marrow hematopoietic stems cells to increase product of RBC
Decreased tissue oxygenation causes what?
stimulates release of EPO from kidneys → stimulates hematopoietic stem cells in bone marrow → increases production of RBC by bone marrow → increases oxygen-carrying capacity of blood → increase tissue oxygenation
What is low oxygen concentration in the blood called?
Hypoxia
What are the factors contributing to hypoxia?
Reduced ability of blood to carry oxygen (low blood volume, anemia, low hemoglobin), that affects delivery of oxygen to tissues (low blood volume and flow) and affects ability to take in oxygen (pulmonary disease)
Iron is needed for:
Production of RBC
Iron is obtained from:
food and absorbed into blood in intestine
Iron is transported in:
blood bound to transferrin (iron transport protein)
Iron is used to bone marrow to:
Make RBC
50% of body iron reserve is from:
Hb from dying RBC
25% of body iron reserve is:
stored in other iron containing proteins (other than Hb)
The remaining 25% of body iron reserve is:
stored in liver bound to ferritin (a protein)
Old or damaged RBC taken up by
macrophages in spleen by phagocytosis
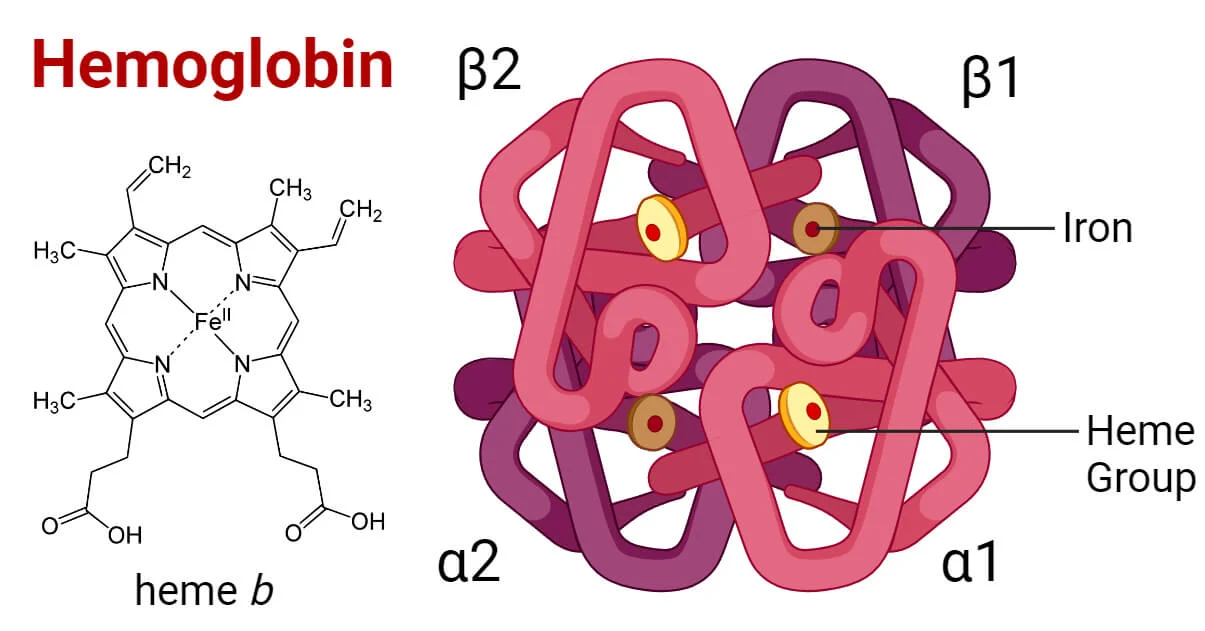
As old or damaged RBC are taken up by macrophages hemoglobin is broken down into:
Heme and globin
The heme part of hemoglobin is broken down into _____ and _____ by macrophages.
iron and biliverdin
Where does iron go after RBC is broken down by macrophage?
absorbed into blood for erythropoiesis or stored in spleen or liver bound to ferritin
What does Biliverdin (from broken down heme) become as macrophage continues to brake down the RBC?
it is converted to bilirubin, secreted into bile and enters small intestine
The globin part of hemoglobin is broken down into what by the macrophage?
amino acids
Vitamin B12 is required for:
normal production of RBC
VItamin B12 is obtained from:
diet (e.g. liver, fish, eggs, dairy)
Absorption of vitamin B12 from the GI tract requires:
intrinsic factor (a protein), secreted by cells in stomach wall
What is Pernicious anemia?
Lack of vitamin B12 or intrinsic factor
The decreased oxygen-carrying capacity of the blood due to a deficiency of RBCs and/or hemoglobin contained in the RBCs is called:
Anemia
What are the factors leading to anemia?
Lack of iron, pernicious anemia, aplastic anemia, chronic kidney disease, hemolytic anemia, haemorrhagic anemia, abnormal hemoglobin structure
damage of bone marrow due to radiation/drugs, resulting in low RBC production is called:
Aplastic anemia
Chronic kidney disease causes:
reduced level of erythropoietin, EPO, reducing RBC production
Increased RBC breakdown due to abnormal shape of RBC or due to immune reactions during transfusion is called:
Hemolytic anemia
Increased blood loss due to injury, bleeding ulcers or chronic menstruation is called:
Hemorrhagic anemia
A normal adult has what components in hemoglobin?
2 alpha and 2 beta protein chains
In sickle cell disease, red blood cells have abnormal Hb called:
HbS
The shape of sickle cell red blood cells are due to:
A single amino acid mutation in the B-chain
The characteristics of sickle cell disease are:
sickle-shaped RBC with hard, nonflexible cell membranes
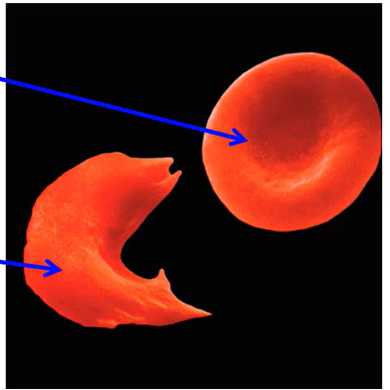
What occurs to RBC in sickle cell disease as they pass thru capillaries?
They are damaged, leading to hemolytic anemia
What type of disease is sickle cell?
autosomal recessive disease (the gene for Hb S has to be inherited from both parents)
Immunity refers to:
The process that help a cell or the interior of our body defend against anything foreign; protects our ‘self’ from our ‘non-self
What is innate/natural immunity?
Immunity we are born with; non-specific defenses in the body such as physico-chemical barriers, or physiological and chemical barriers of the body
What does innate/natural immunity include?
skin, enzymes in body fluids, acid secretion in stomach, WBCs = granulocytes, monocytes/macrophages
What is acquired/adaptive/specific immunity?
Acquired over time and upon exposure to foreign pathogens/cells. Foreign object triggers the immunity to develop
What plays a role in acquired/adaptive/specific immunity?
WBCs that are lymphocytes
WBCs are produced from:
pluripotent stem cells in bone marrow
Pluripotent cells converted to:
Granulocytes (neutrophils/eosinophils/basophils), monocytes or lymphocytes (B cells and T cells)
Lymphocyte production begins in:
The bone marrow
T-Lymphocytes migrate to:
thymus to complete development then return to blood
B-Lymphocytes mature in:
The bone marrow
What cells may migrate to peripheral tissues and are returned to circulation by lymphatic system?
Lymphocytes
Key features of Innate/natural memory are that its:
Non-specific, no memory of foreign body, is fast (sec/mins/hrs)
Key features of acquired/adaptive memory are that its:
Specific, has memory of foreign body, is slow (days/weeks)
Major cells involved in innate/natural immunity are:
Phagocytes (neutrophils and macrophages)
Major cells involved in acquired/adaptive immunity are:
Lymphocytes (B & T-cells)
The major molecules involved in innate/natural immunity are called:
A complement system
The major molecules involved in acquired/adaptive immunity are:
antibodies; cytotoxic molecules
Acquired immunity cannot develop by itself, requiring:
Innate/natural cells to develop
Defense, and removing old/damaged/abnormal cells are what kind of responses of the immune system?
Appropriate
allergies, and autoimmune reactions (attacking self immune) are what kind of responses of the immune system?
Inappropriate