GMED2000
1/82
Earn XP
Description and Tags
exam LOL
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
83 Terms
pharmacology
the study of drugs, including their sources, nature, actions and effects on living systems
Drug
a substance used to modify or explore the physiological system or pathological state for the benefit of the recipient
Potency
is the amount of chemical required to produce an effect
selectivity
is the narrowness of a drug’s range of action on a receptor, cellular processes or tissues
specifcity
refers to the range of action of a drug and the relationship between the chemical structure of the drug and its pharmacological action (e.g.. beta blockers)
drug classifications
Source •Chemical formula or structure •Pharmacokinetic parameters •Activity and drug action •Clinical use •Body system(s) affected by the drug •Drug Schedule •Pregnancy safety •Allowed to be used in sport/ competition
pharmacodynamics
study of the interaction between a drug and its molecular target and of the pharmacological response ‘What the drug does to the body’, its actions and effects > ACTION and REACTION
pharmacokinetics (defintion)
factors that affect the passage of a drug through the body ‘What the body does to the drug’, with respect to absorption, distribution, metabolism and excretion > UTILISATION
four fundamental pharmacokinetic processes
absorption, distribution, metabolism, excretion
pharmacokinetics control
speed, duration and intensity of the drug.
absorption
Unchanged drug is absorbed into body fluid and transported to the site of action – determined by the route of administration
Distribution
Process of reversible transfer of a drug between one location and another in the body
Metabolism
Drug metabolism is the process of chemical modification of a drug and is almost invariably carried out by enzymes
excretion
A drug continues to exert pharmacological effect until it has been eliminated by the body through urine, feaces, or exhalation.
development of obesity
develops when energy intake is greater then expenditure, excess energy stored as adipose tissue
obesity risk factors
Lifestyle factors (Unhealthy diet, Physical inactivity, Stress, Smoking, Socioeconomic factors), genetic factors and metabolic factors.
pathophysiology of obesity
refers to the biological and physiological mechanisms that contribute to the development and persistence of obesity, including hormone regulation, metabolism, and energy balance.
Type 2 diabetes aetiology and risk factors
obesity, sedentary lifestyle, genetics, hypertension, tobacco usage
Type 2 diabetes pathophysiology
starts as insulin resistance, because tissues aren’t absorbing enough glucose, the liver releases more sugar which over time exhausts the beta cells which will make them less effective and therefore release less insulin
Type 2 Diabetes Clinical manifestations
include increased thirst, frequent urination, extreme fatigue, blurred vision, and slow healing of wounds.
Type 2 Diabetes Evidence-based management stratergies
Managing blood pressure and cholesterol, increased physical activity, healthy diet, weight loss blood sugar monitoring, medications which may progress to insulin therapy if necessary.
BGL lowering medication classes
biguanides (e.g. metformin), thiazolidinediones, sulphonylureas, alpha-glucoside inhibitors.
Type 2 diabetes acute complications
hypoglycaemia, hyperglycaemia, diabetic ketoacidosis, hyperglycaemic hyperosmolar state (HONK, poor glucose control leading to severe dehydration)
Pain
unpleasant sensory or emotional potential or actual tissue damage.
Types of pain
Nociceptive, neuropathic and psychogenic
Noicicpetive pain
Most common type of pain, can be internal or external. Occurs when noicicpetive stimuli triggered associated with peripheral tissue damage.
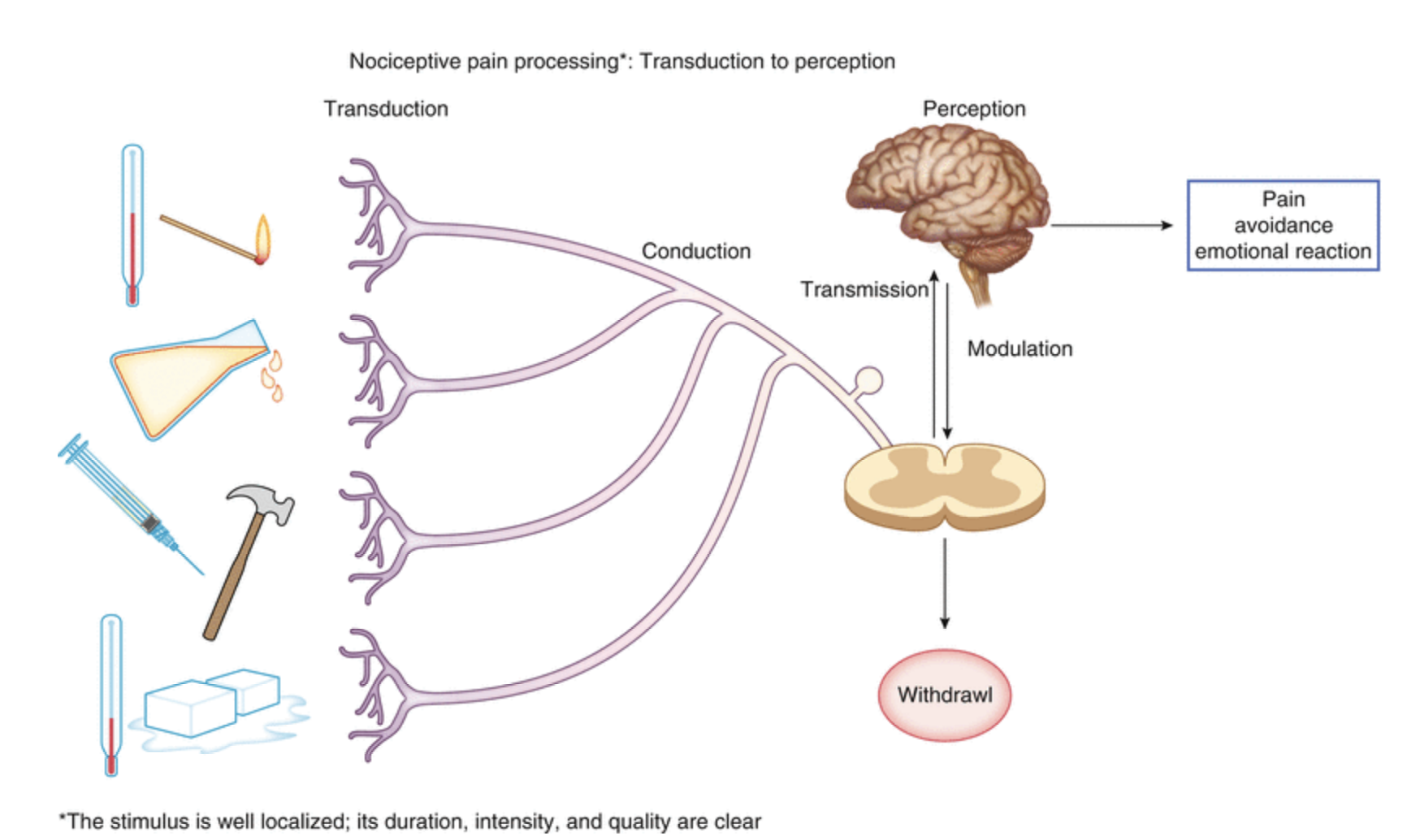
Noiciceptive pain pathway
Transduction
Conduction
Transmission
Perception
Modulation
Neuropathic Pain
Caused by disease or injury to Nervous System, it is complex and can be severe and persistent.
Pyschogenic Pain
Less common and is severe and persistent despite no underlying pathology. It can be debilitating and as a result of psychological disorder.
Characteristics of pain
Acute and chronic
Breakthrough- hyperalgesia and allodynia
Acute Pain
Pain that accompanies tissue injury. It is a sudden onset of sharp and localised pain that intiates fight or flight.
3 types: 1. somatic (nerve receptors), 2. visceral (from organs and is dull pain), 3. referred (felt in areas different from site of stimuli)
Chronic Pain
Ongoing and prolonged pain. It is not always associated with an identifiable cause but often arises from an acute situation such as post trauma, herpes zoster, acute back pain and postoperative surgical pain,Typically it lasts beyond expected healing time, ~3-6months or more.
Chronic pain Pathophysiology
Neurological changes that can occur with persistent pain are changes in perception.
Physical changes that result are loss of muscle mass, deconditioning, postural changes, alterations in appetite and weight, constipation and sleep disturbances.
Persistent pain is complex and is poorly understood. It is suggested that when persistent pain is present it can develop to an individual disease process because of the secondary changes that occur in the body
Breakthrough pain
Pain that occurs between analgesia doses, preventable with a higher analgesia dose.
Hyperalgesia
Increased pain response from a stimulus that is normally painful
Allydonia
Pain that results from a stimulus that does not normally produce pain
Clinical manifestations of pain
Evidence based management stratergies
Treat underlying cause first, use pain questionnaire and utilise pharmacological and non-pharmacological.
Non-pharmacological pain management
Physio, hypnosis, relaxation, distraction, massage and hot and cold packs.
Pharmacological Pain management
Non-opoid, opoid, NSAIDs
Analgesic Ladder
Mild pain: non-opoid and adjuvant
Moderate pain: non-opioid and opioid
Severe pain: Opoid
Paracetamol//simple analegesia
Mild-moderate pain, fever, headaches and migraines. Safe for kids but toxic in non-safe doses.
NSAIDs//ibuprofen, naproxen
analgesic, antipyrexial, antiplatlet, anti-inflammatory. Can cause G.I. irritation, nausea, vomitting
Opoid analgesia
Drugs derived from opium. Produces analgesia by binding to opoid-receptors, inihibits release of substance P from dorsal horn neurons thus mediating pain. Indicated for severe pain.
Chlamydia
Infection caused by some subtypes of chlamydia trachomatis, it grows within endo+epithelium of endocervix, rectum, peritoneal cavity, fallopian tubes, oropharynx and conjcutiva. Transmission: mother-child, mulitple partners, unprotected sex
Chlamydia clinical Presentations/manifestations
~ 60% women and ~25% men are asymptomatic. Urethral discharge, testicular/scrotal tenderness, abnormal bleeding or vaginal discharge, pysuria, proctitis, bleeding between cycles, painful intercourse, internal inflammation.
Chlamydia diagnosis
at GP or sexual health clinic, urine sample, endocervical swab, urethral swab, oral or throat swab required for oral sex.
Chlamydia complications
can lead to infertility in men and women, conjuctivititis, fever and abdominal pain, pelvic inflammatory disease, peri-hepatitis, fallopian tube blockages, pneumonia of new borns.
Chlamydia Treatments
Antibiotics (doxycycline 100mg 12hrly, azithromycin one 1g dose or 10mg/kg orally for kids.) Important for pregnancy so baby doesn’t get it.
Avoid sex until treatment complete, inform sexual partners, proof of cure 4 weeks post-treatment, contact tracing.
In a child- potential sexual assault or mother to child.
Gonorrhoea
Caused by Neisseria gonorrhoeae (GNID) a bacteria. Can occur motherchild, unprotected sex, multiple partners.
Gonorrhoea clinical presentation
~80% women and ~10-15% men present asymptomatic, urethritis and/or dysuria, cervicitis, intramenstral bleeding, anorectal infection, pharyngeal infection, pelvic inflammatory Disease.
Gonorrhoea diagnosis
NAAT testing, swab peri-anal abd vaginal area.
Gonorrhoea complications
Can become serious and turn into sepsis, PID, prostatitis and epididymitis, skin lesions, meningitis or endocarditis, arthritis, disseminated gonococcal infection.
Gonorrhoea Treatment
depends on type
complicated: ceftriaxone
uncompicated: IM 500mg Ceftraxione and Axithomycin 1g orally
Physiology of wound healing
Complex process made up of ~3-4 stages.
heamostasis (fill the wound)
inflammatory phase
Proliferation (seal wound)
regeneration (shrink)
haemostasis
immediate response to bleeding, platlets rush in and form a clot, strengthened by fibrin and vasoconstriction occurs.
Inflammatory stage
Wound can be red, swollen, tender to touch due to white blood cells (e.g. neutrophils and macrophages) moving to the area to fight infection and clear debris.
Proliferation
Fibroblasts come in and start laying down new collagen, new blood vessels form and bring in more oxygen and nutrients and the wound heals through tissue remodelling. Granulation tissue beings to form and replaces the clot with new tissue.
remodelling/maturation
Collagen fibres reorganise and continue to strengthen the wound site, improving tissue integrity and function over time. Scar tissue gradually becomes less noticeable.
short-acting insulin
insulin aspart
Long-acting insulin
insulin glargine
sulfonylureas
stimulate insulin release
dapagliflozin
decreases glucose reabsorption in the kidneys
Somatostatin
inhibits glucagon and insulin
GLP-1 Analogues
delay gastric emptying
Pioglitazone
increase insulin sensitivity
aberrant healing
wound heals outside normal margins e.g. hypergranulation, contractune, keloid, hypertrophic scar
can happen after surgery or traumatic wound, mindful of drugs that can increase collagen production
factors that can inhibit healing
aging, nutritional, allergies, lifestyle factors, immobility and inactivity, smoking, medications, co-morbidities
diabetes and wound healing
heamostasis- increased infection and imparied vascular supply
inflammatory- slow neutrophil recruitment, persistent inflammation
infection- hyperglyceamia= increased bacterial growth, ineffective neutrophil and macrophage activity
proliferation- decreased tensile strength collagen, decreased collagen deposition and decrease fibroblast activity
maturation- decreased tensile collagen strength, risk of ulcer, recurrence as a result of weakened area of scar tissue.
mood disorders
Mood disorders are broadly categorized into unipolar depression, also known as major or clinical depression, and bipolar disorder.
The development of either type is not due to a single cause, but rather a complex interaction of various contributing factors. These include biological elements like genetics and hormonal imbalances, psychological stressors such as grief, loss, or abandonment, and social influences like poverty or domestic violence, all interacting with broader environmental influences to potentially trigger a psychiatric disorder.
depression
When states such as sadness become prominentand interfere with daily life, leading to changes in sleep, appetite, and energy levels. It can affect overall wellbeing and requires treatment to manage symptoms.
Pathophysiology of depression
The development of mood disorders is primarily understood as a complex interplay between an individual's genes and their environment, rather than simply a result of low serotonin. Stressful life events act as a significant trigger, impacting various bodily systems. This leads to disturbances in neurotransmitters and dysregulation of hormonal systems, particularly the hypothalamic-pituitary-adrenal (HPA) axis, resulting in increased cortisol release, and the hypothalamic-pituitary-thyroid (HPT) system. Additionally, altered circadian rhythms contribute to sleep disturbances, and neuroanatomic and functional abnormalities are also observed in the brains of those affected.
treatment of depression
Treatments for depression encompass both pharmacotherapy and non-pharmacological approaches, often used in combination for optimal results. Key pharmaceutical options include older classes like Monoamine Oxidase Inhibitors (MAOIs) and Tricyclic Antidepressants (TCAs), alongside newer generations such as Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Noradrenaline Reuptake Inhibitors (SNRIs), all of which work by increasing monoamine neurotransmitter levels in the brain.
Escitalopram
a widely used SSRI, specifically enhances serotonergic activity by inhibiting the reuptake of serotonin, leading to increased serotonin levels in the synapse and improved mood, and is notably potent and selective, often with fewer side effects compared to other SSRIs.
oxycodone
classification as a potent semi-synthetic opioid analgesic primarily used for moderate to severe pain, acting as an agonist at mu-opioid receptors in the CNS to block pain signals. Critical adverse effects to remember are respiratory depression (life-threatening, especially with co-ingestants like alcohol or benzodiazepines) and significant constipation. Emphasize its high potential for tolerance, physical dependence, and addiction, making it a Schedule II controlled substance that requires careful prescribing, monitoring, and cautious withdrawal to avoid severe symptoms.
Sciatica
unilateral pain radiating down one leg along the sciatic nerve pathway, primarily caused by compression or irritation of the sciatic nerve roots, most commonly due to a herniated lumbar disc. Key exam points include pain worse than back pain, often described as burning or shooting, accompanied by numbness, tingling, or weakness in the affected leg
osteoarthritis
a common, chronic condition characterized by the progressive breakdown of cartilage cushioning the ends of bones within joints, leading to bones rubbing together. This friction causes pain, swelling, and loss of motion, and the condition typically worsens over time. While any joint can be affected, OA most frequently impacts weight-bearing joints such as the knees, hips, and spine, as well as the hands and ankles. For exams, remember that it's a degenerative joint disease (often called "wear and tear" arthritis) rather than an inflammatory one like rheumatoid arthritis, and that its primary symptoms are activity-related pain (worse with movement, better with rest) and morning stiffness lasting less than 30 minutes.
metformin
oral antihyperglycemic agent primarily used to lower blood glucose levels in Type 2 Diabetes. It achieves this mainly by decreasing glucose production by the liver (hepatic gluconeogenesis) and increasing the body's sensitivity to insulin, allowing cells to better utilize glucose. While its exact mechanism is complex, the crucial takeaway is that by controlling Manisha's blood glucose, Metformin helps to mitigate the negative impact of high sugar levels on her overall health and, importantly, on the impaired wound healing process associated with chronic diabetes.