096 Module 4 - Coronary Artery Disease
1/40
Earn XP
Description and Tags
Midterm Content
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
41 Terms
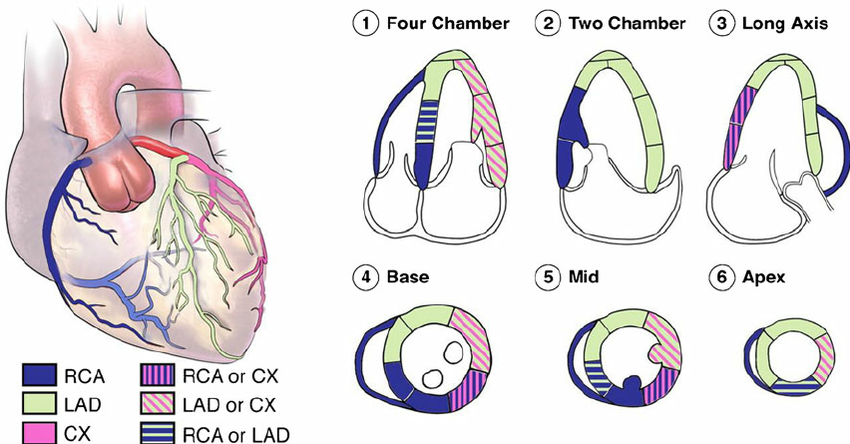
Draw coronary artery perfusion of the LV wall segments.
Name the 3 control mechanisms of the cardiovascular system.
autoregulatory (local control)
neural control
endocrine (hormonal) control
Name the 2 determinants of myocardial O2 supply.
coronary perfusion pressure
coronary vascular resistance
Name the 3 determinants of myocardial O2 demand.
wall stress (Pr x r /2h)
HR
contractility
Flow is ______ (directly/inversely) proportional to Pr gradient and ______ (directly/inversely) proportional to resistance.
directly, inversely
At what stage of the cardiac cycle do coronary arteries perfuse? Why?
Coronary arteries perfuse during diastole.
During systole, flow is going in the direction of the ascending aorta due to kinetic energy. The dicrotic notch during isovolumetric relaxation is when the backflow hits the AoV and blood will enter the coronary arteries.
During systole, there is external compression of the myocardium, thus increasing resistance in the coronary arteries. Blood will not flow in high resistance areas.
Explain the short term autoregulation when there is a coronary occlusion. What is the goal of this mechanism?
coronary occlusion → organ perfusion Pr decreases → vasodilation → perfusion Pr increases vasoconstriction → returned to homeostasis
The goal is to maintain coronary artery perfusion while protecting smaller blood vessels.
List and define the 2 long term autoregulation mechanisms when there is a coronary occlusion.
collateral circulation: enlargement of small blood vessels to maintain perfusion
angiogenesis: new blood vessel growth to supply hypoxic region
Draw a pressure-volume loop comparing increased and decreased inotropy.
Increased inotropy:
decreased ESV from increased SV
Decreased inotropy:
increased ESV from decreased SV
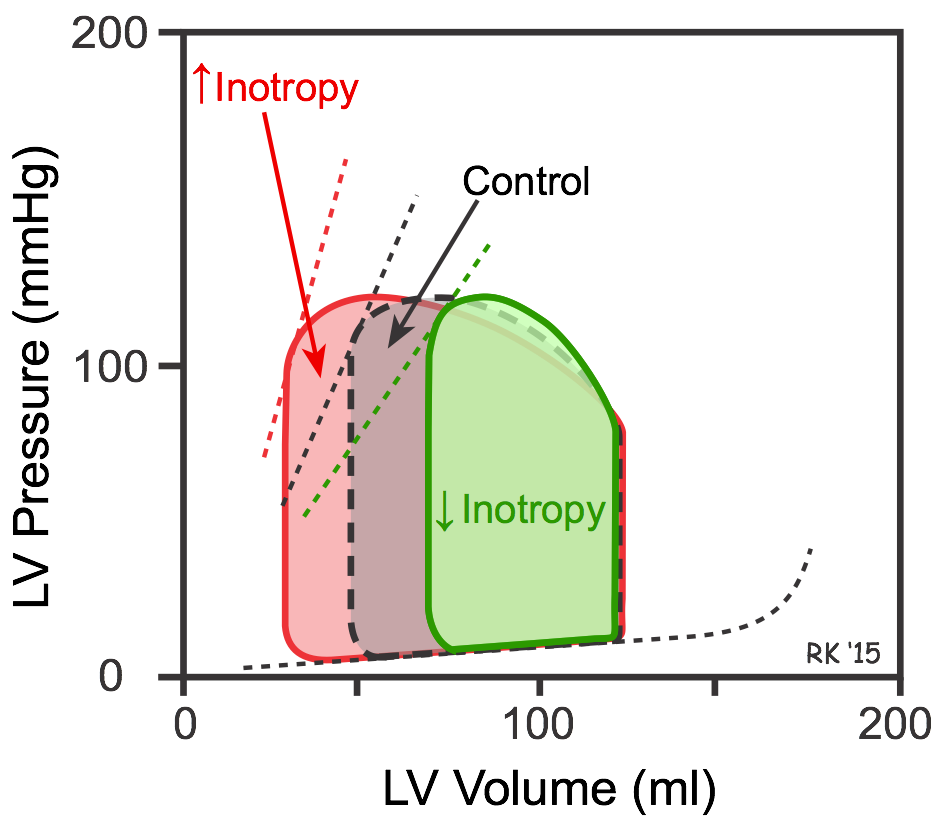
The width of a pressure-volume loop represents…
Stroke volume
The area of a pressure-volume loop represents…
The work the ventricle performs with each beat and is proportional to myocardial oxygen consumption
Myocardial ischemia can be caused by:
atherosclerotic plaques
abnormal vascular inflammation
abnormal vascular tone
drop in blood volumes
Define myocardial infarction.
Heart tissue death, symptomatic as a heart attack
If myocardial ischemia is left untreated, it eventually leads to…
Myocardial infarction
Define acute coronary syndrome.
Sudden, reduced blood flow to the heart.
List the four types of acute coronary syndrome.
stable angina
unstable angina
NSTEMI
STEMI
Describe stable angina.
Increased O2 demand an area with atherosclerotic plaque. The vessel cannot dilate enough to meet O2 demands, causing demand ischemia but no infarct.
Describe unstable angina.
Atherosclerotic plaque ruptures and a thrombus forms, causing partial occlusion of the vessel. Pain occurs at rest and causes supply ischemia, but no infarct.
Describe NSTEMI.
Complete occlusion of coronary blood vessel from atherosclerotic plaque and thrombus. Causes infarct to the subendocardial myocardium with a normal/relatively normal ECG and elevated troponin levels.
Describe STEMI.
Complete coronary blood vessel occlusion, resulting in transmural injury and infarct to the myocardium. Hyperacute T wave or ST elevation in ECG and elevated troponin levels.
Describe how atherosclerotic plaque impacts hemodynamics.
Narrowing and irregular walls causes turbulent flow (↑wall damage), increases the resistance (↓radius), and restricts blood flow.
If an echo requisition form indicates elevated troponin levels, what condition does this indicate? How does elevated troponin result from this condition? What should the sonographer expect to see during the exam and what information can be gathered from this observation?
Elevated troponin → myocardial infarction (heart attack)
Lack of O2 supply → lack of ATP production → accumulation of intracellular Ca2+ → damaged myocyte dies → release of troponin into the bloodstream
The sonographer should be expecting to see ventricular wall abnormalities. The location of the ventricular wall abnormality indicates the coronary artery affected and the degree of wall thickening in systole indicates the severity.
When performing a normal echo on a patient with a suspected heart attack, why can’t the sonographer just look at the coronary arteries?
Echos do not have the resolution to see coronary arteries without contrasting agents.
Name a procedure that allows visualization of coronary arteries.
Coronary angiography.
A patient with a suspected heart attack has normal presentation during their routine echo. What procedure can be done to better analyze heart function under an increased workload?
Stress echo.
Normal LVEF.
Male: 52-72%
Female: 54-74%
Severely abnormal LVEF.
<30%
Mildly abnormal LVEF.
Male: 41-51%
Female: 41-53%
Moderately abnormal LVEF.
30-40%
Define systolic dysfunction.
Inability to pump blood effectively and failure to meet normal cardiac output at every heart beat.
Name 3 causes of systolic dysfunction.
volume overload (high output failure)
pressure overload (outflow obstruction)
myocardial disease (impaired contractility)
Name and define the 3 factors to a wall motion analysis.
Endocardial excursion: endocardium moving inwards during systole
LV cavity reduction: LV cavity decreasing in size during systole
Wall thickening: LV walls thickening in systole
List the standard qualitative wall motion terms per ASE guidelines.
Normal
Hyperkinetic
Hypokinetic
Akinetic
Dyskinetic
Aneurysmal
What is observed in a hyperkinetic wall?
Excessive wall motion and thickening in systole.
What is observed in a hypokinetic wall?
Reduced endocardial excursion and thickening.
What is observed in a akinetic wall
Absent endocardial cushioning and thickening.
What is observed in a dyskinetic wall?
Outward motion / bulging of thin wall during systole.
What is observed in a aneurysmal wall?
Bulging outward during diastole and worse bulging during systole.
A patient is referred for a coronary angioplasty of the RCA. Which wall segments should receive better perfusion after the procedure?
All of RV walls
Basal-mid inferoseptal walls
Basal-mid inferior walls
Basal-mid inferolateral walls
A patients echo reveals hypokinetic walls in:
Basal-mid anteroseptal walls
Basal-apical anterior walls
Apical septal wall
Apical inferior wall
Apical lateral wall
Which coronary artery is likely affected?
LAD
A patient cardiac angiography reveals partial occlusion in the circumflex artery. What wall segments can the cardiac sonographer expect to be affected during wall motion analysis?
Basal-mid anterolateral walls
Basal-mid inferolateral walls
Apical lateral wall