Comprehensive Guide to Folate, B12, and Iron in Nutrition
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
47 Terms
What is the primary function of folate (Vitamin B9)?
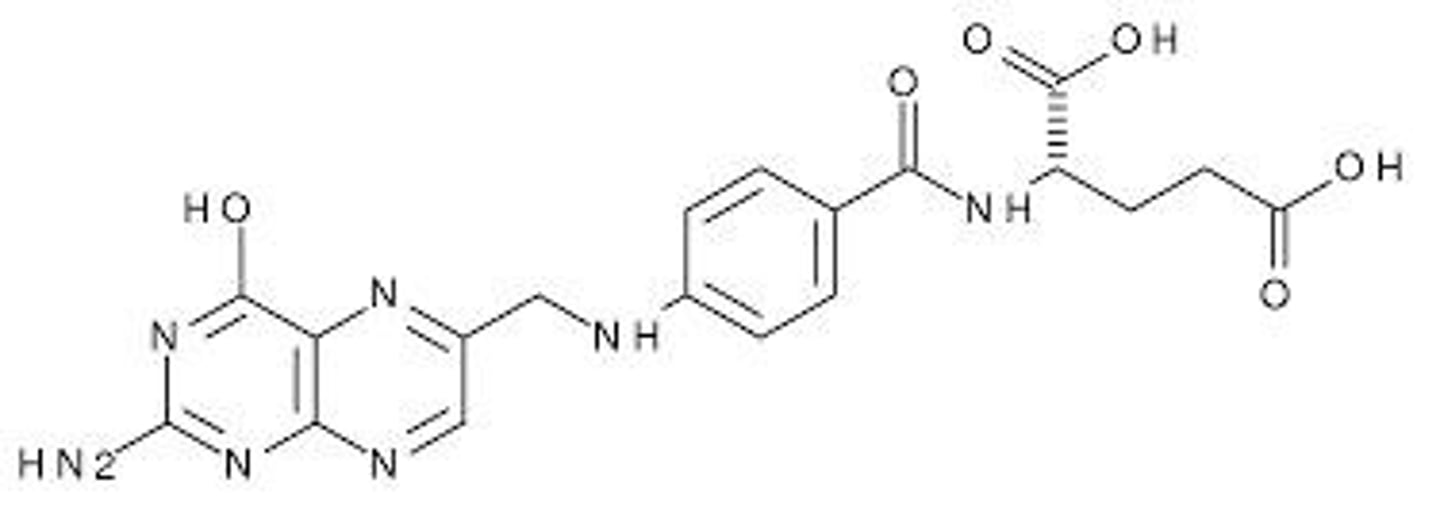
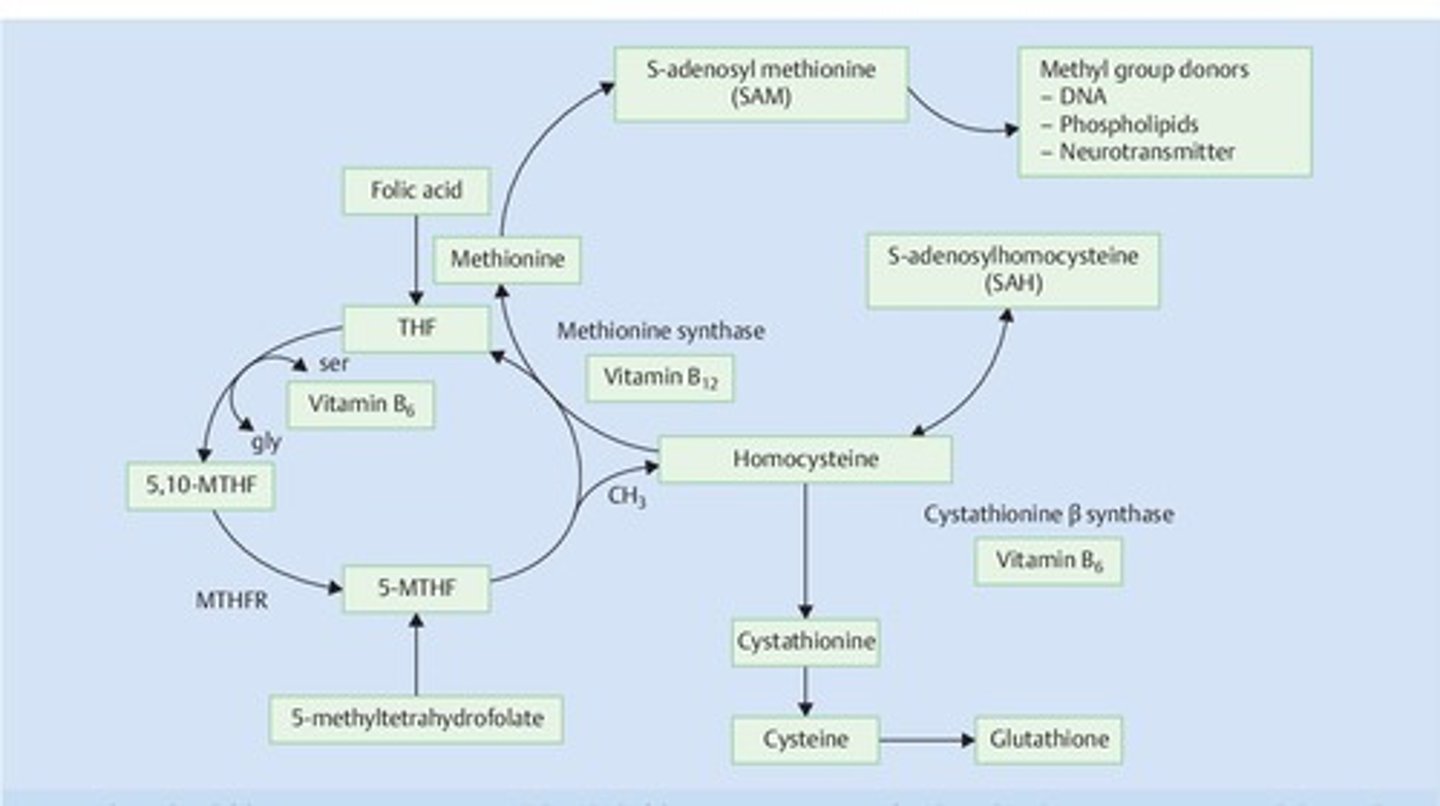
Folate acts as a coenzyme that transports single carbon groups for amino acid metabolism and nucleic acid synthesis, vital for cell replication.
What are some common food sources rich in B vitamins?
Enriched whole grains, brewer's yeast, lean pork, legumes, salmon, clams, almonds, milk, yogurt, eggs, beef, chicken, avocado, spinach, and broccoli.
What is the recommended daily intake of folate for adults?
400 micrograms (mcg) DFE daily.
What is the recommended daily intake of folate for pregnant women?
600 micrograms (mcg) DFE daily.
What health risks are associated with insufficient intake of folate?
Risks include spina bifida, neural tube defects, macrocytic anemia, elevated blood homocysteine, and increased risk of stroke.
What is macrocytic anemia and how is it related to folate?
Macrocytic anemia is characterized by large, under-developed red blood cells, often resulting from folate or vitamin B12 deficiency.
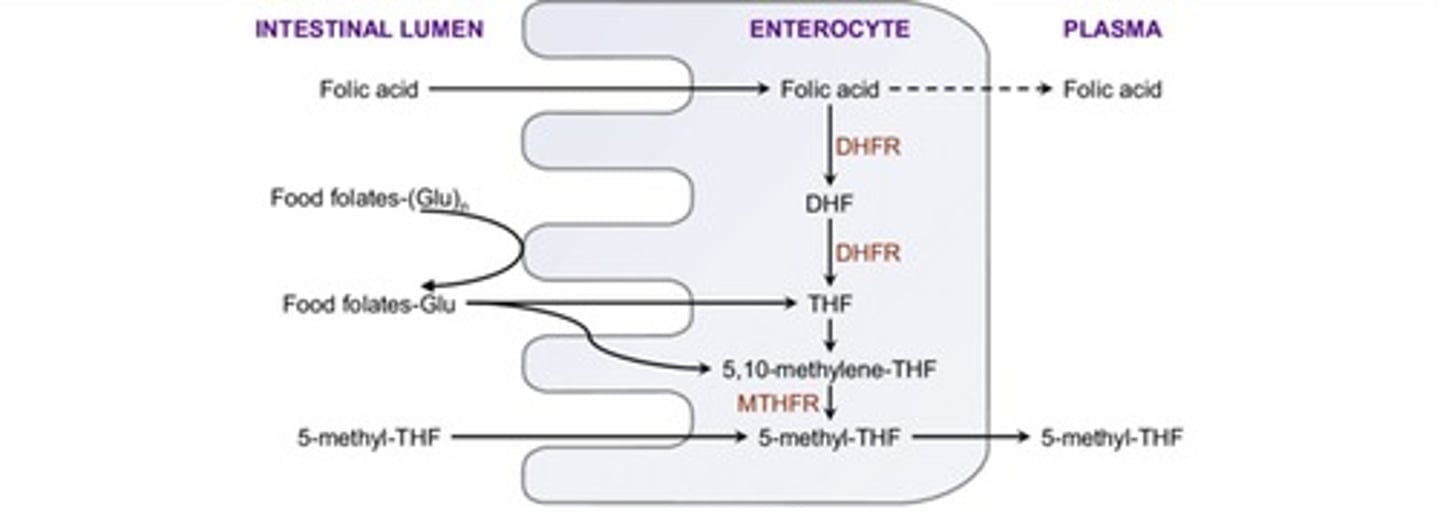
What factors can reduce folate absorption?
Aging, alcohol consumption, intestinal inflammation, insufficient stomach acid, certain medications, and overcooking foods.
What is the impact of excessive synthetic folic acid intake?
It may worsen anemia and cognitive deterioration associated with vitamin B12 deficiency and increase the risk of certain cancers.
What are neural tube defects (NTDs) and when do they occur?
NTDs are birth defects of the brain and spinal cord that occur between day 16 and 28 post-conception.
What is the role of vitamin B12 in relation to folate?
Vitamin B12 is needed to activate 5-methyl-tetrahydrofolate by removing its methyl group, which is crucial for DNA synthesis and nerve function.
What are the active forms of cobalamin (Vitamin B12)?
Methylcobalamin and 5-deoxyadenosylcobalamin.
What is the dietary recommendation for vitamin B12 intake?
The recommended dietary allowance (RDA) is 2.4 mcg/day.
What are some food sources of vitamin B12?
Clams, beef liver, bluefin tuna, and fortified brewer's yeast.
How is vitamin B12 absorbed in the body?
B12 detaches from protein in the stomach, binds to haptocorrins, and then to intrinsic factor for absorption in the distal ileum.
What are the symptoms of folate deficiency?
Symptoms include fatigue, weakness, headache, glossitis, loss of appetite, diarrhea, weight loss, and elevated blood homocysteine.
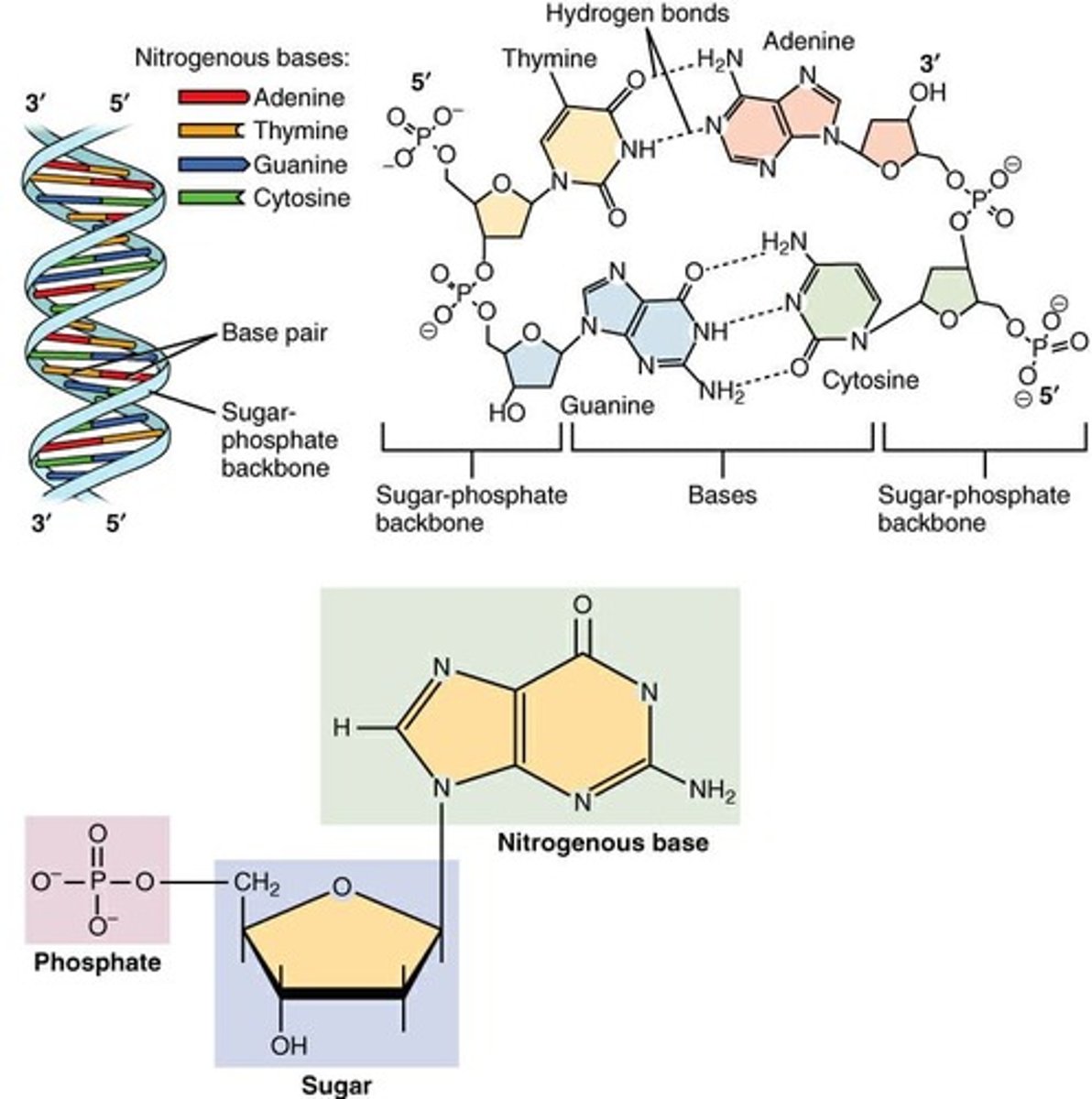
What is the folate cycle's role in DNA synthesis?
It provides dTMP for DNA synthesis and purines for DNA, RNA, and ATP.
What is the effect of folic acid fortification of refined grains?
It has led to a 35% reduction in neural tube defects since its implementation in 1998.
What are the potential consequences of low folate status?
Low folate status can lead to an increased risk of stroke and other cardiovascular events.
What is the significance of the folate-dependent reaction involving homocysteine?
It converts homocysteine to methionine and is essential for the production of S-adenosyl-methionine, a key methyl donor.
What are some conditions linked to inadequate folate intake?
Conditions include cancers, cardiovascular disease, depression, and congenital health defects.
What are the signs of macrocytic megaloblastic anemia?
Signs include large, under-developed red blood cells and low hemoglobin levels.
What is the relationship between folate and spina bifida?
Insufficient folate intake during pregnancy increases the risk of spina bifida and other neural tube defects.
What is the role of folate in epigenetic regulation?
Folate is involved in DNA synthesis and modification, influencing gene expression through epigenetic mechanisms.
Who is at risk for Vitamin B12 deficiency?
Aging adults, those with atrophic gastritis, individuals with pernicious anemia, users of acid-suppressing medications, heavy alcohol drinkers, frequent nitrous oxide users, and vegans.
What is the treatment for individuals without intrinsic factor?
They require periodic intramuscular injections of B12 or daily oral doses of 1,000 to 2,000 mcg of B12.
What is a common sign of Vitamin B12 deficiency?
Macrocytic megaloblastic anemia, glossitis, muscle weakness, fatigue, tachycardia, and nerve damage.
What are the diagnostic criteria for Vitamin B12 deficiency?
Holo TC II < 40 pg/ml, Serum B12 < 200 or <250 pg/mL, MCV >100 fL, elevated serum MMA ≥0.271 micromol/L, and elevated serum homocysteine >12 micromol/L.
What role does iron play in the body?
Iron is part of hemoglobin in red blood cells, myoglobin in muscles, and is a cofactor for enzymes involved in various biochemical reactions.
What is the recommended dietary allowance (RDA) of iron for adult females aged 19-50?
18 milligrams/day.
What is the recommended dietary allowance (RDA) of iron for adult males aged 19-50?
8 milligrams/day.
How is heme iron absorbed in the body?
Heme iron is absorbed into enterocytes with the help of HCP1 and is stored as ferritin or transported into circulation via ferroportin.
What factors affect the absorption of non-heme iron?
Stomach acid, vitamin C, sugars, sulfur-containing amino acids, and the presence of MFP factor enhance absorption, while high calcium intake can reduce it.
What are common causes of low iron in infants and toddlers?
Low-iron formula, lack of supplemental iron, excessive dairy consumption, and insufficient iron-rich foods.
What are symptoms of iron deficiency?
Weakness, shortness of breath, rapid heartbeat, headache, dizziness, pale skin, and microcytic hypochromic anemia.
What are the stages of iron deficiency?
Stage 1: Depleted iron stores, Stage 2: Iron deficiency without anemia, Stage 3: Iron-deficiency anemia.
What is the biochemical test result indicating iron deficiency?
Serum ferritin < 30 mcg/L, transferrin saturation < 15%, serum iron < 60 mcg/dL.
What is the difference between macrocytic anemia and microcytic anemia?
Macrocytic anemia is due to folate and/or Vitamin B12 deficiency, while microcytic anemia is due to iron deficiency.
What is the effect of excessive supplemental folic acid or iron?
It can be harmful to the body and should not be taken before a proper blood evaluation and diagnosis.
What is the role of iron in hemoglobin production?
Iron binds to oxygen within heme groups in hemoglobin, facilitating oxygen transport in the blood.
What dietary sources are rich in iron?
Meat, poultry, fish, beans, nuts, grains, leafy greens, and fortified cereals.
What is the absorption rate of heme iron compared to non-heme iron?
Roughly 15% to 35% of heme iron is absorbed, while less than 10% of non-heme iron is absorbed.
What is the function of transferrin in iron metabolism?
Transferrin transports iron in circulation to tissues after it has been absorbed.
What is a common treatment for iron deficiency?
Iron supplementation and dietary adjustments to increase iron intake.
What is the relationship between obesity and iron deficiency?
Obesity may lead to chronic low-grade inflammation, contributing to iron deficiency.
What is the Lucky Iron Fish or Leaf?
A tool that releases iron into cooking liquids to help increase dietary iron intake.
What is the significance of elevated serum methylmalonic acid (MMA)?
It is an indicator of Vitamin B12 deficiency.
What are the cognitive symptoms associated with Vitamin B12 deficiency?
Memory loss, confusion, depression, and irritability.