A&P2 Exam 2
1/173
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
174 Terms
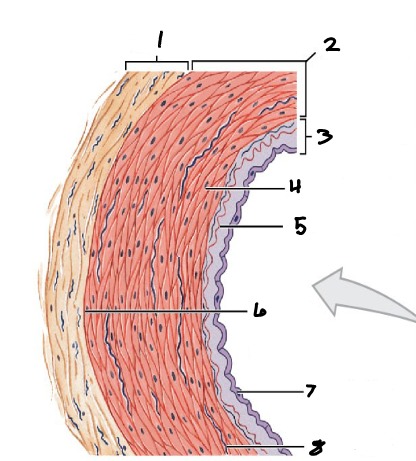
1
Tunica Externa
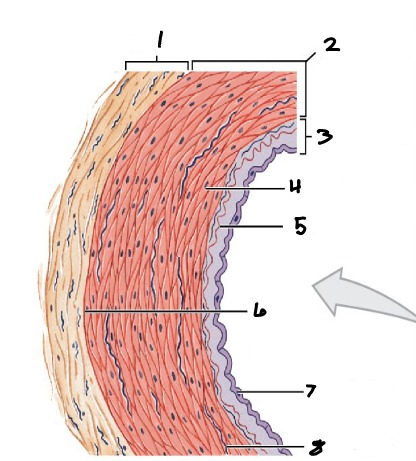
2
Tunica Media
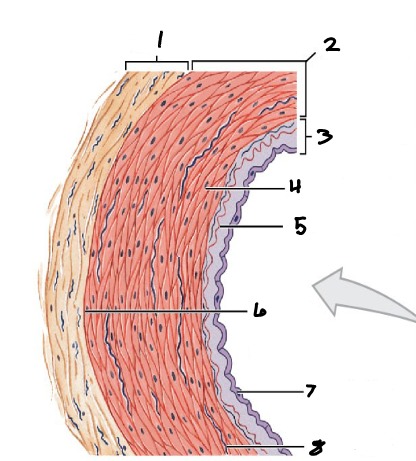
3
Tunica Intima
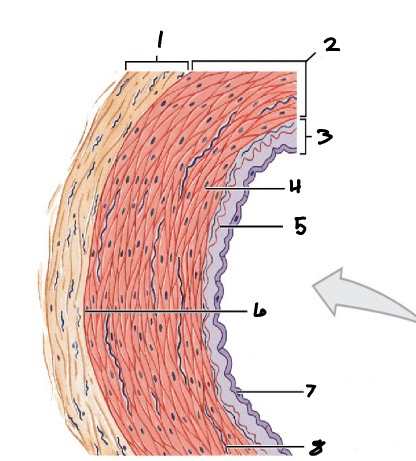
4
Smooth Muscle
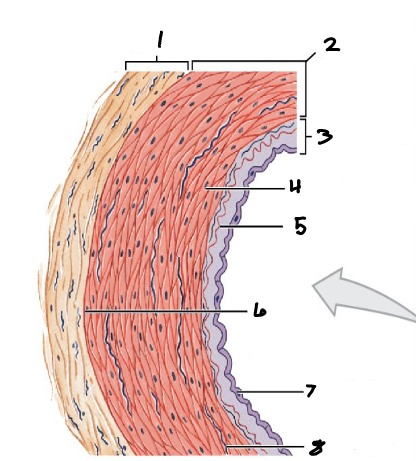
5
Internal Elastic Membrane
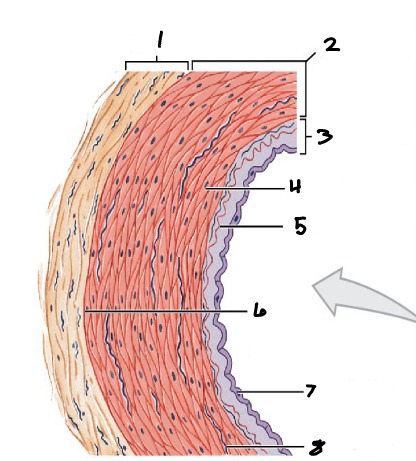
6
External Elastic Membrane
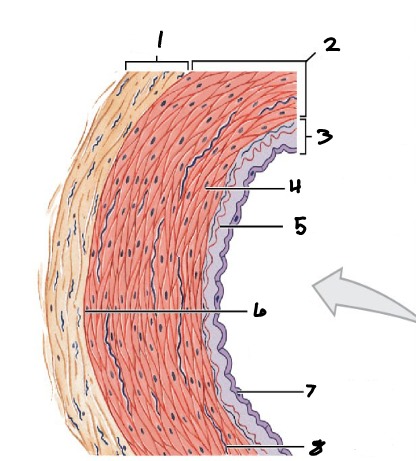
7
Endothelium
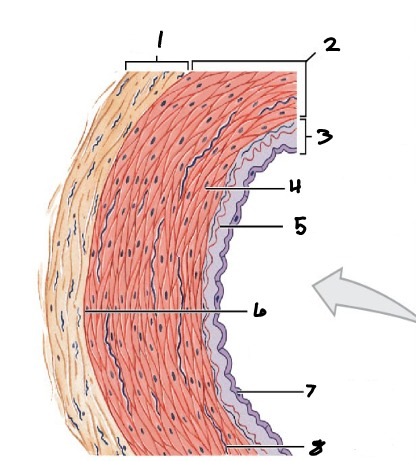
8
Elastic Fiber
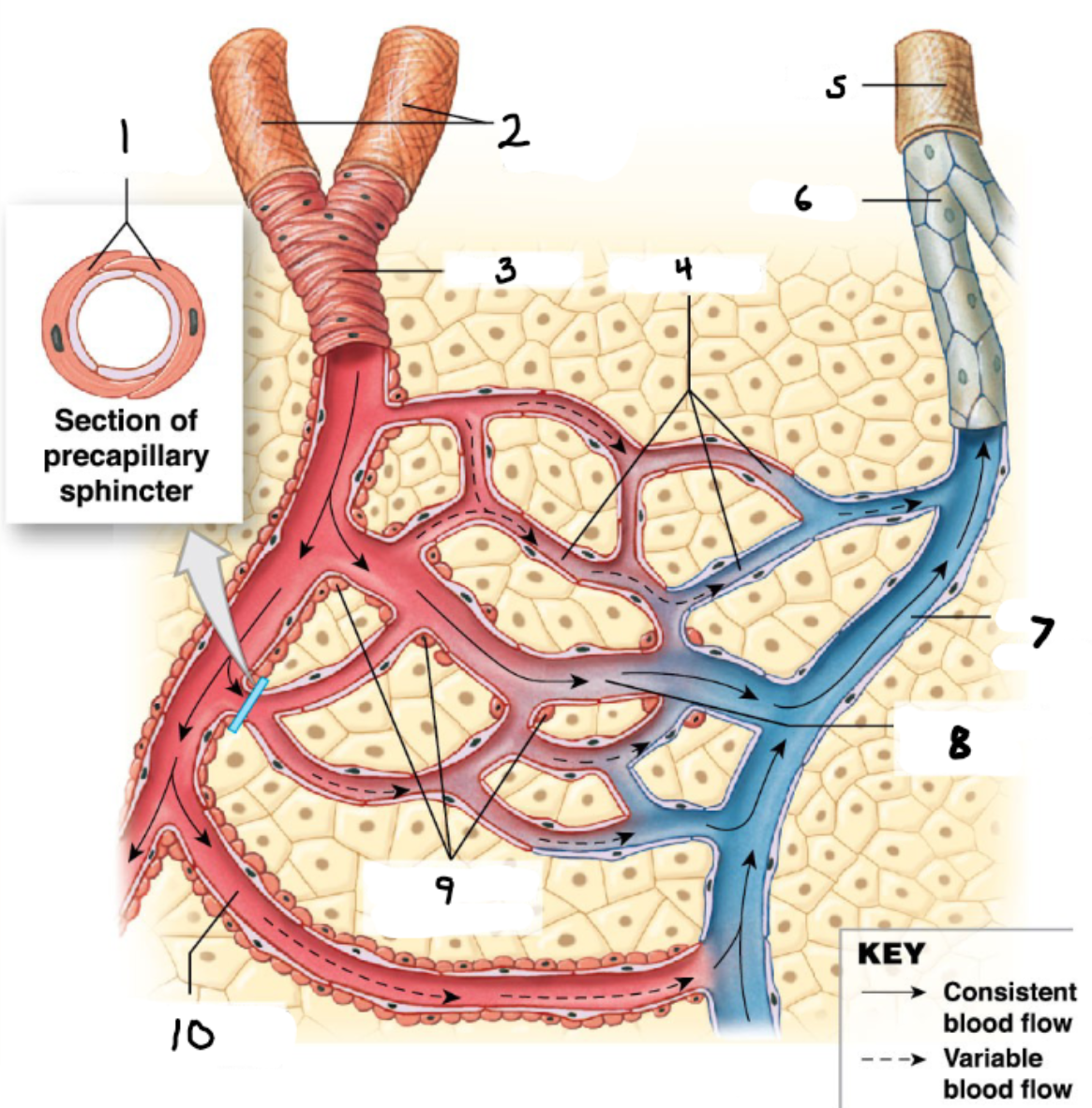
1
Smooth Muscle Cells
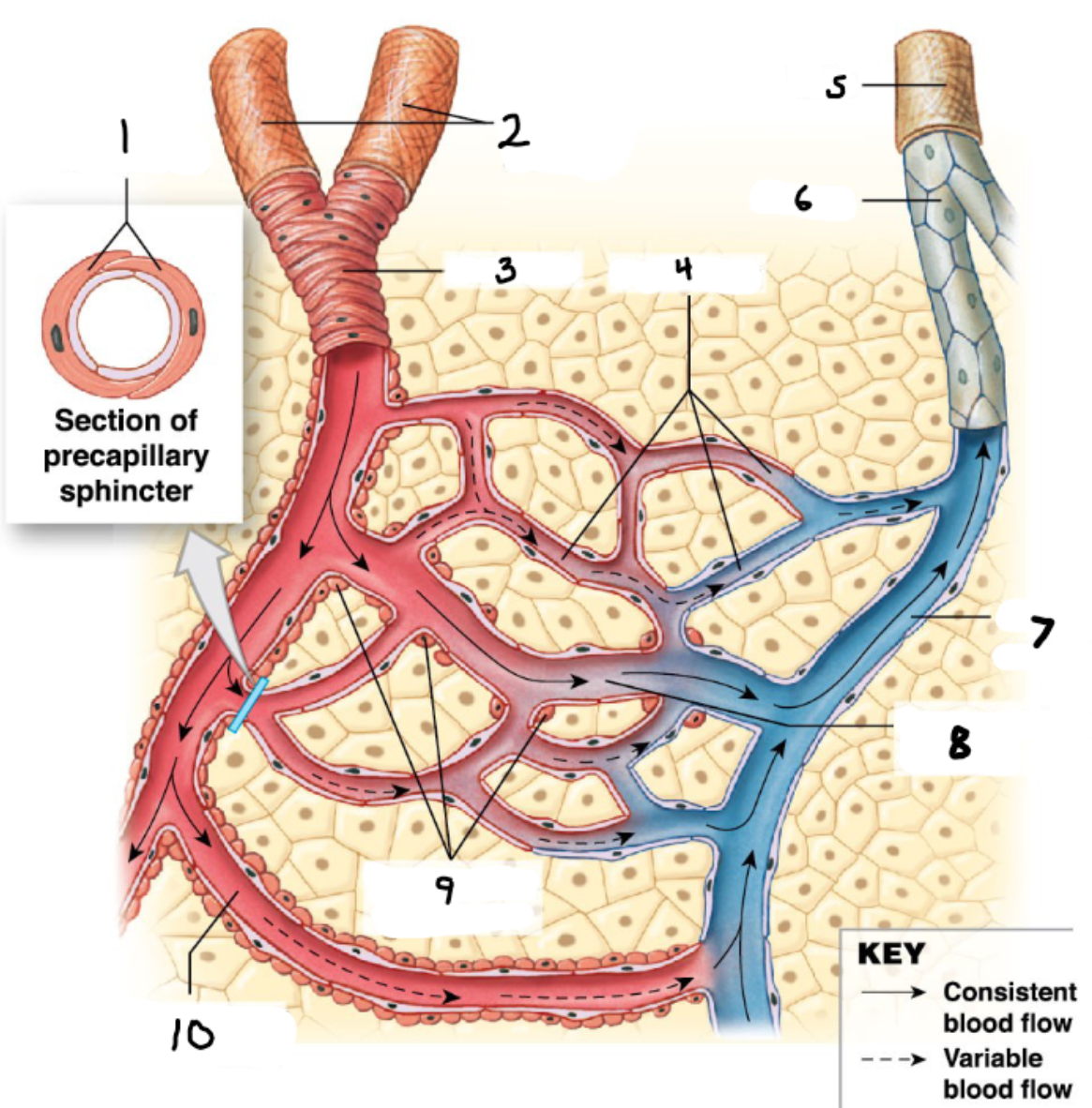
2
Collateral Arteries
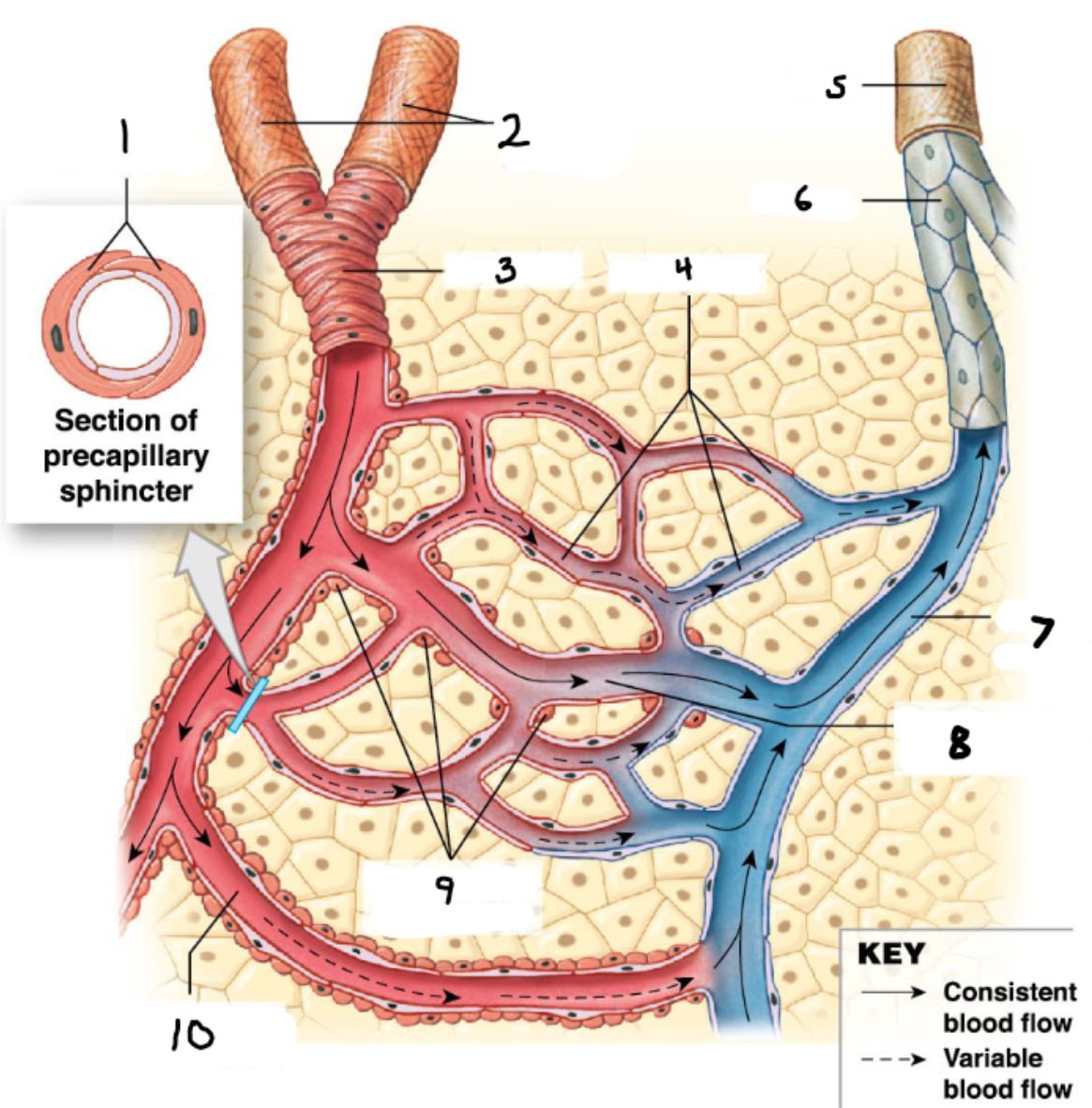
3
Arteriole
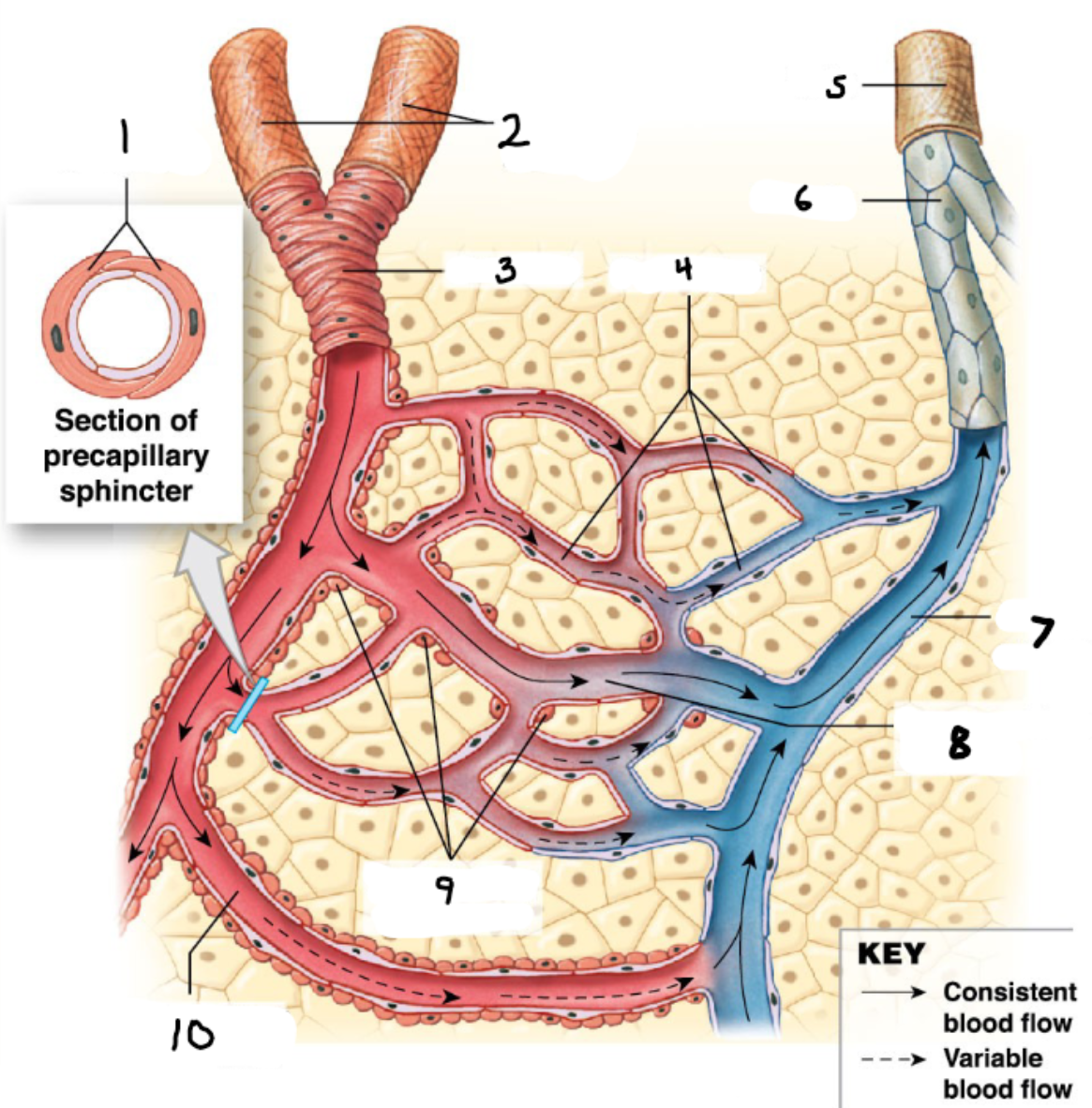
4
Capillaries
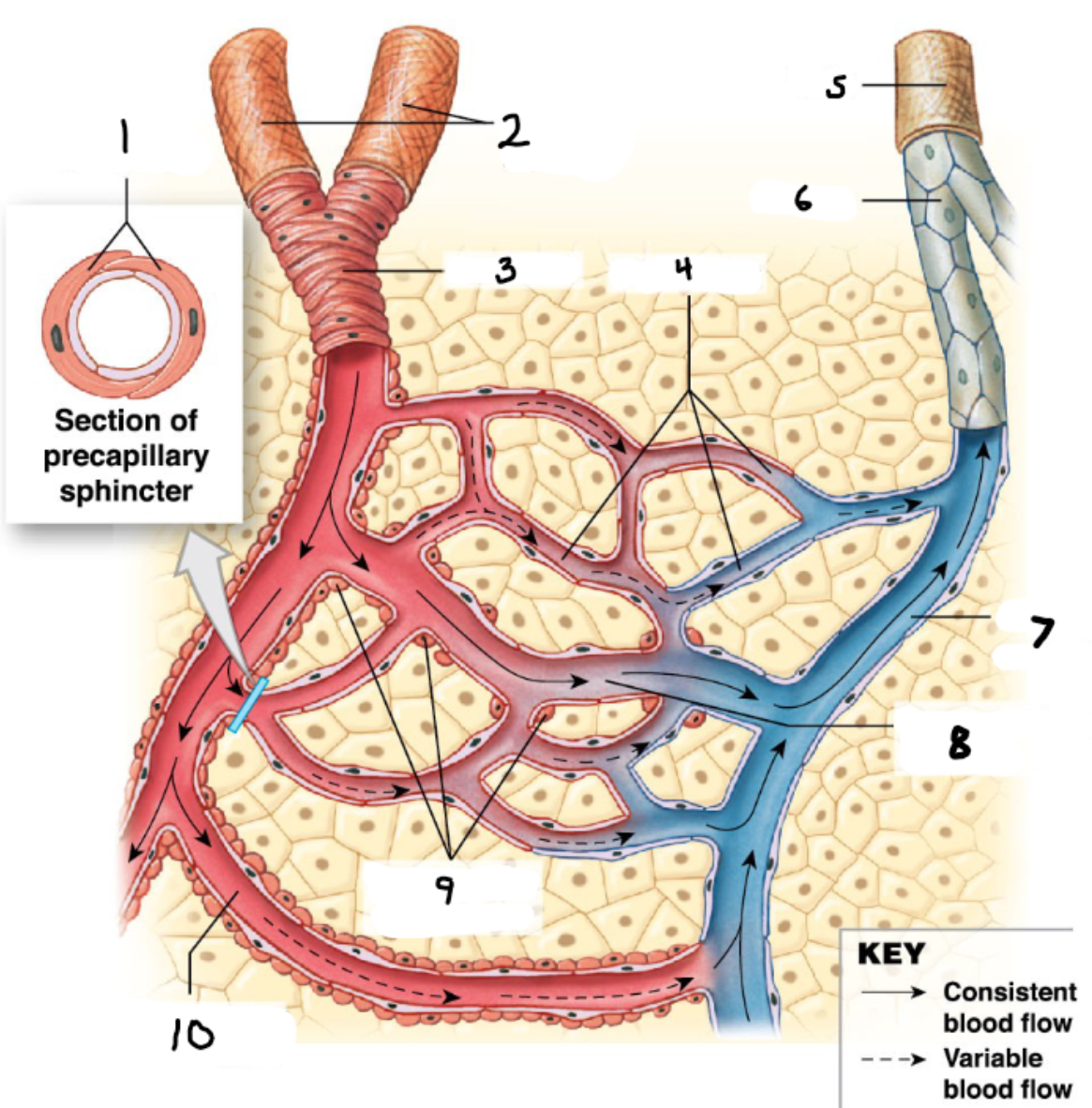
5
Vein
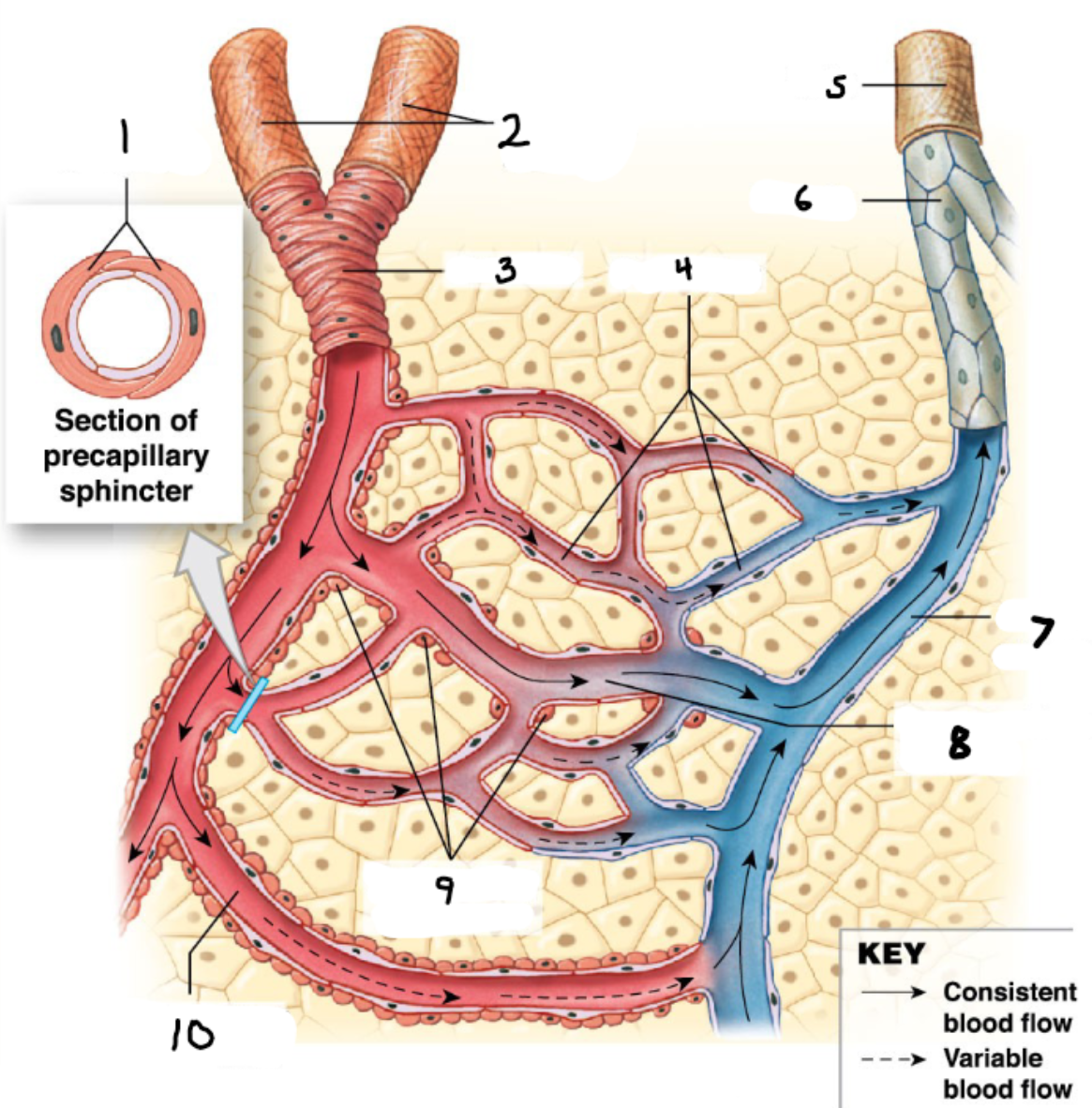
6
Venule
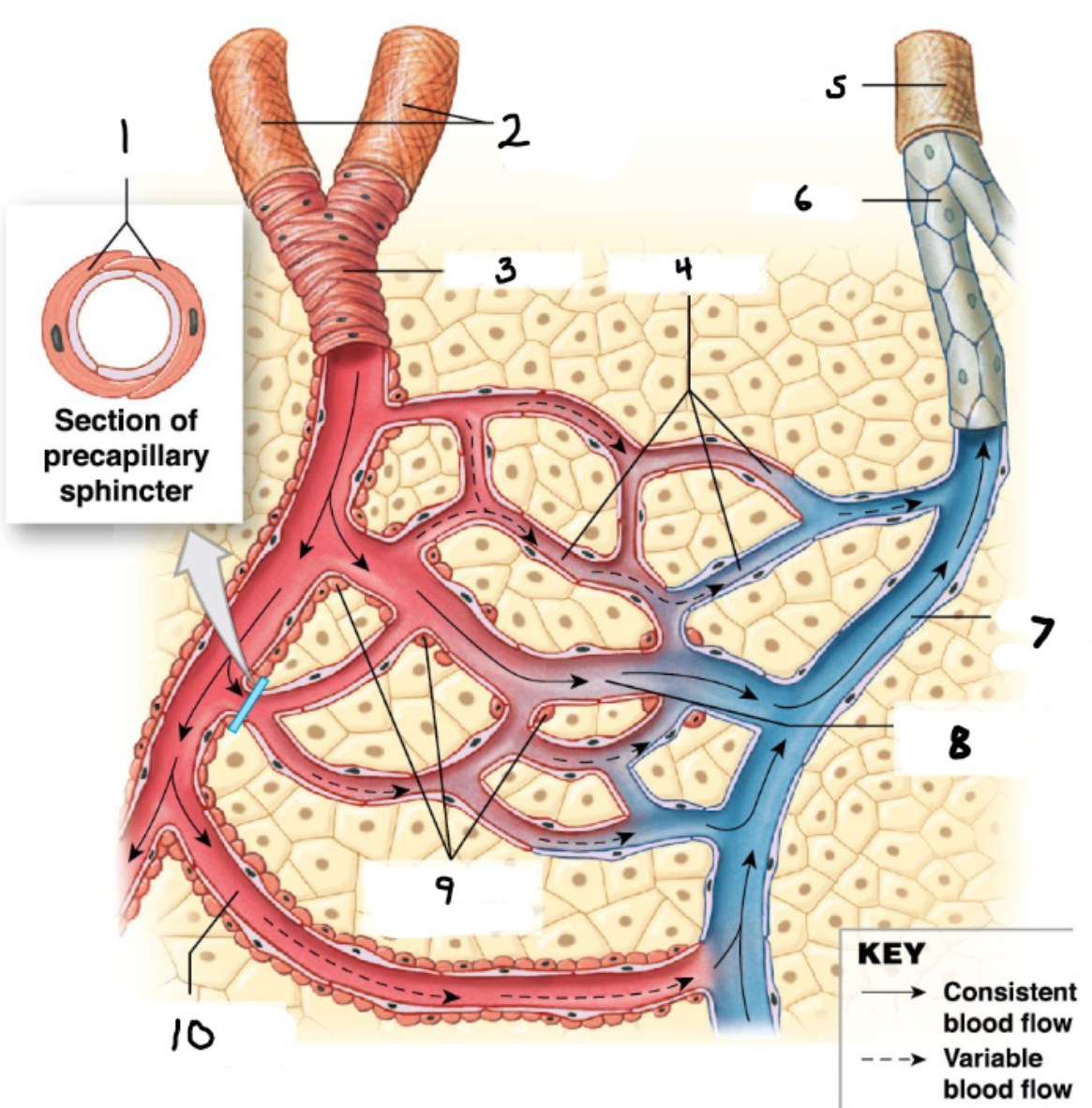
7
Small Venule
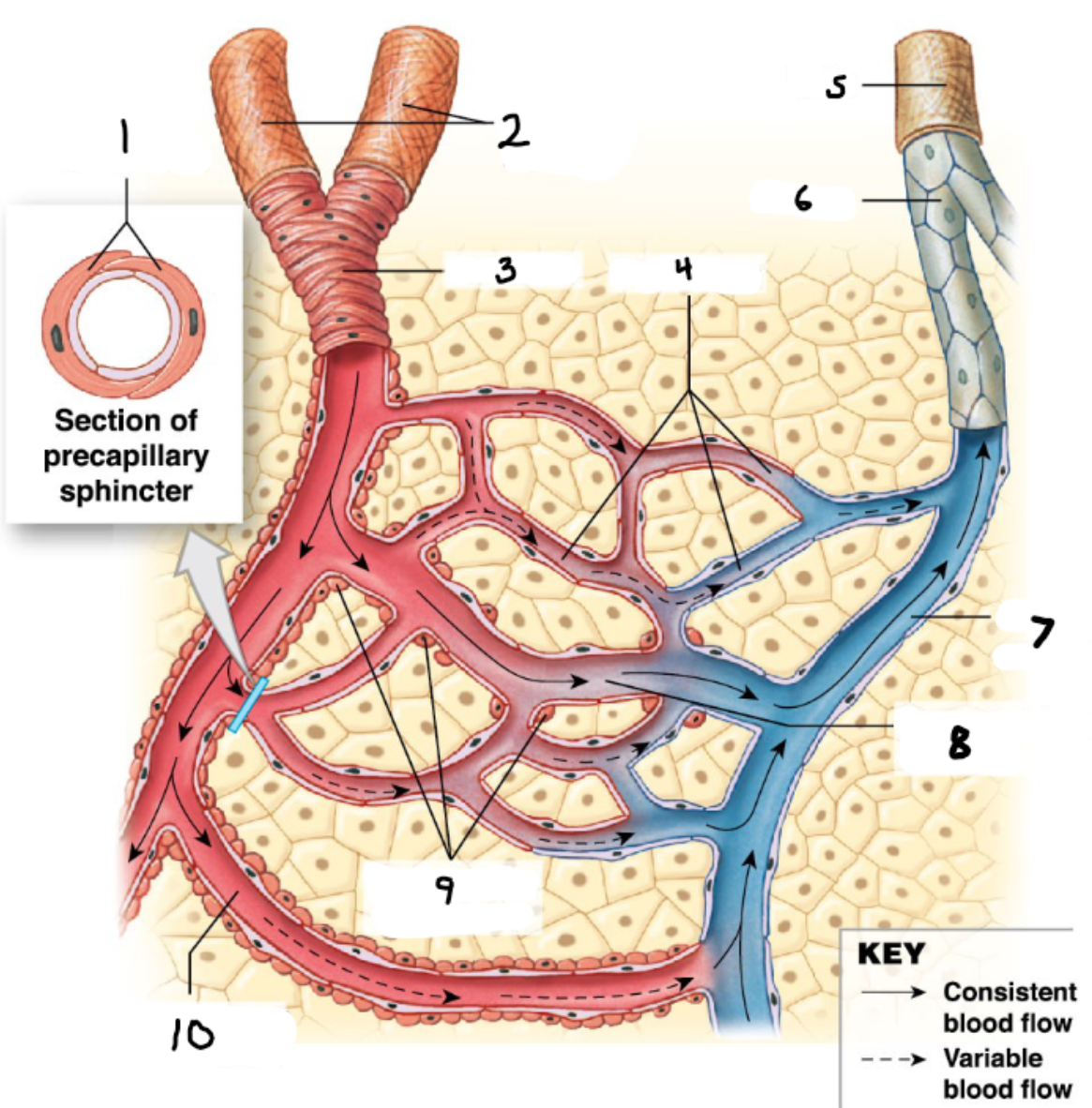
8
Thoroughfare Channel
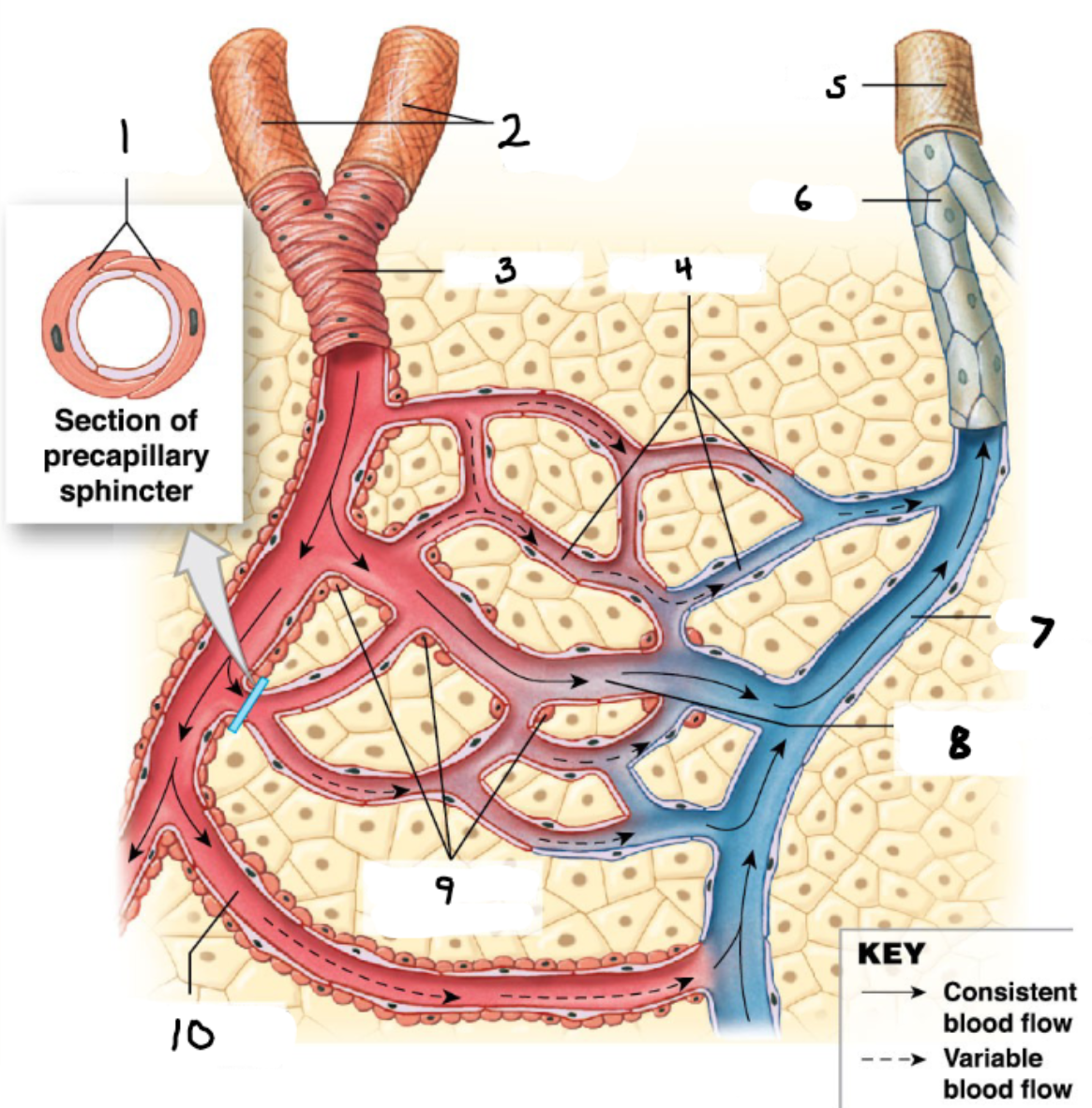
9
Precapillary Sphincters
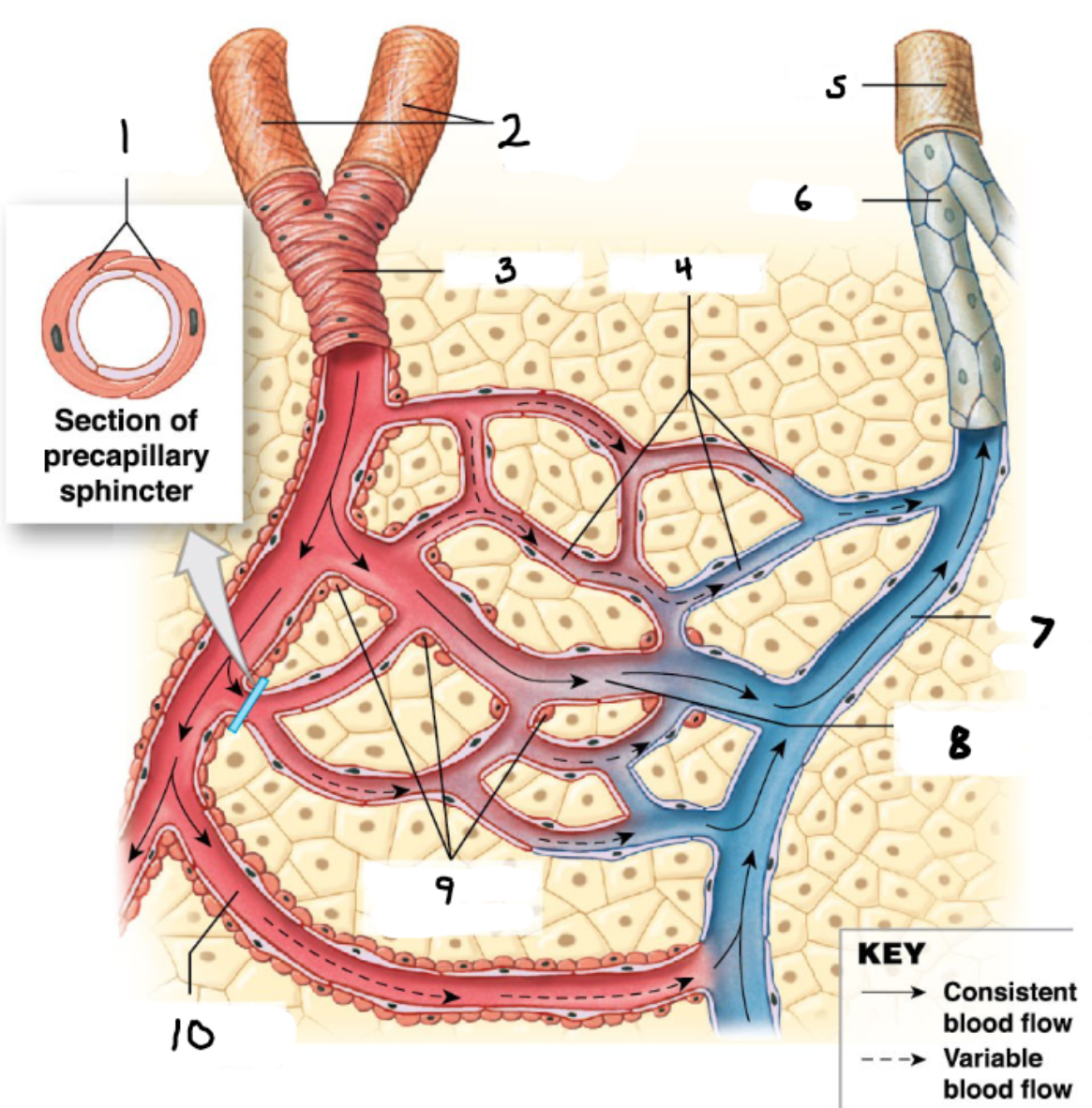
10
Arteriovenous Anastomosis
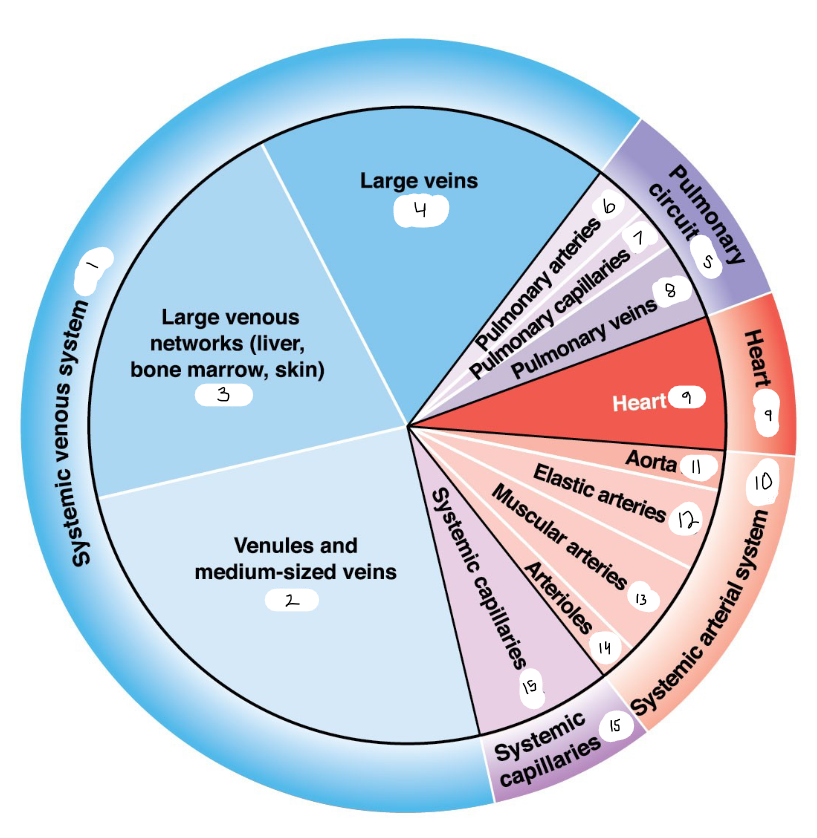
1
64
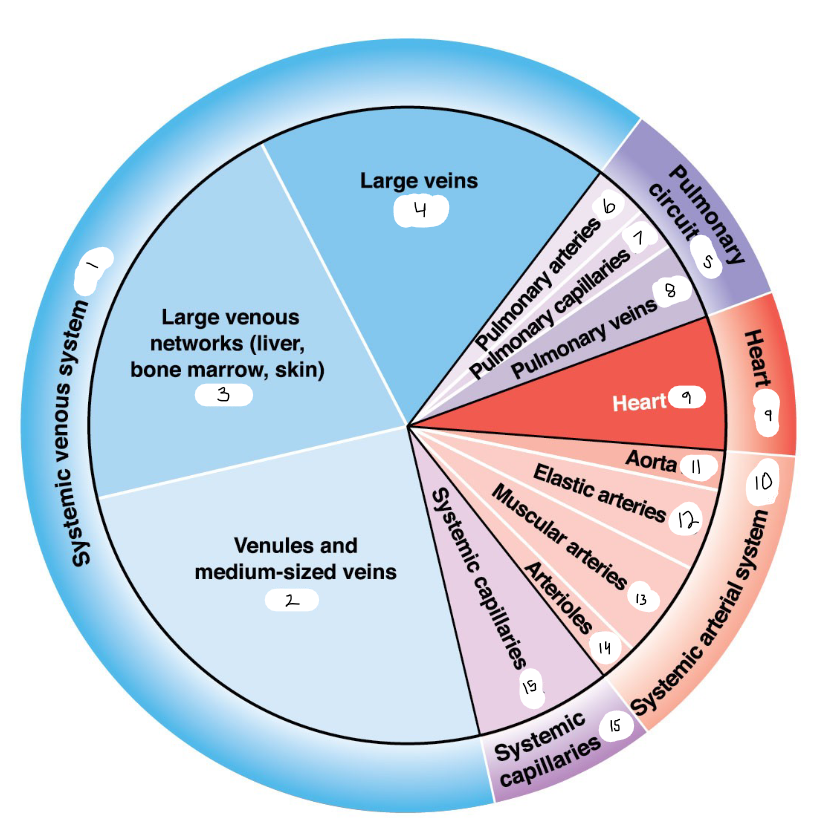
2
25
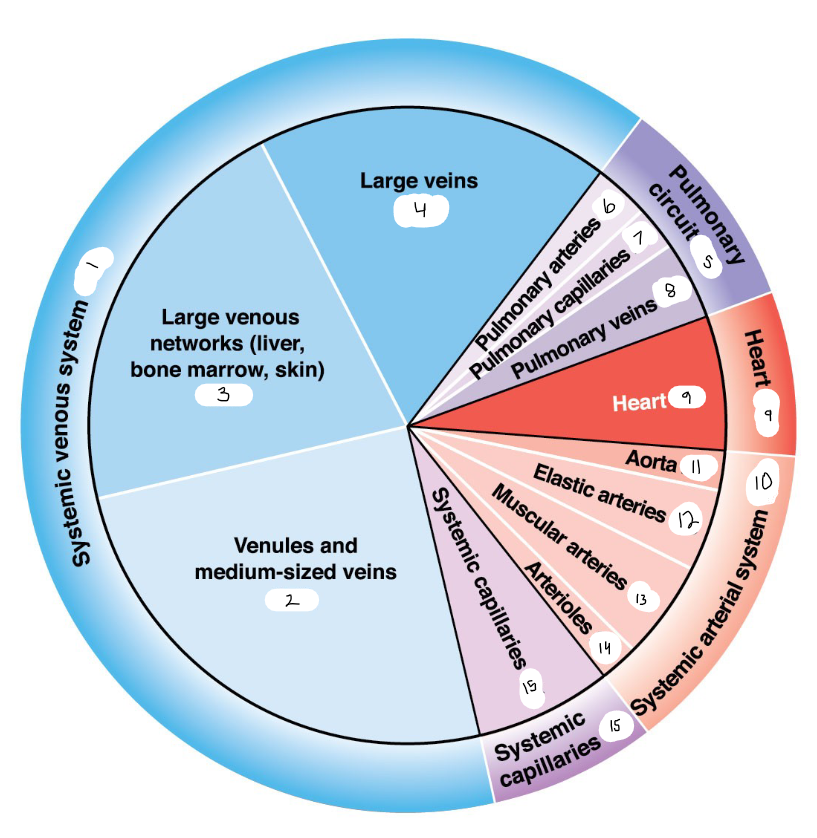
3
21
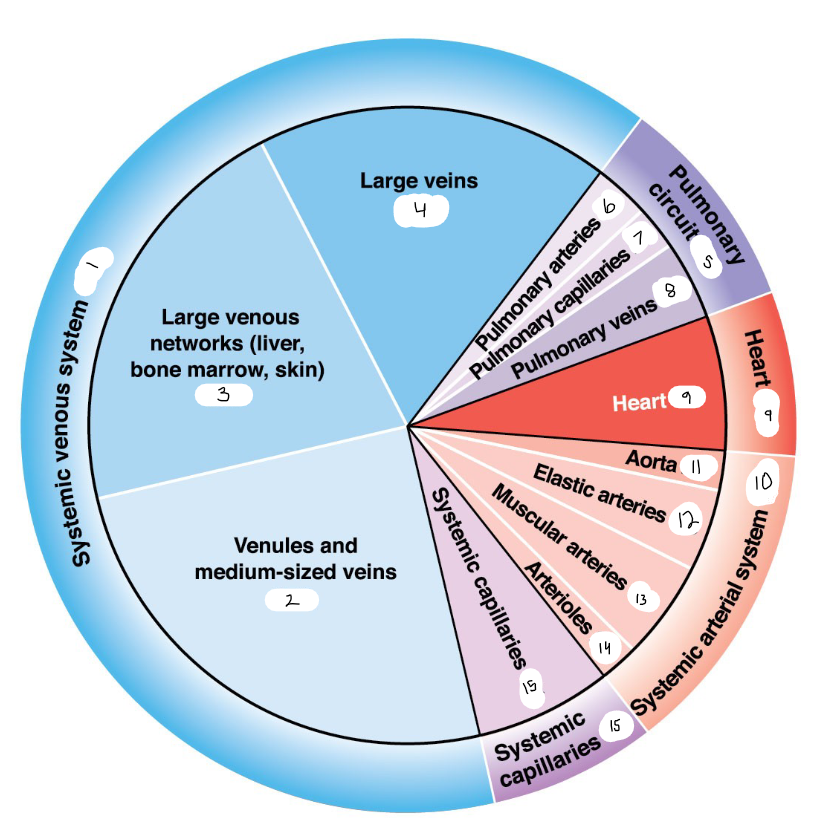
4
18
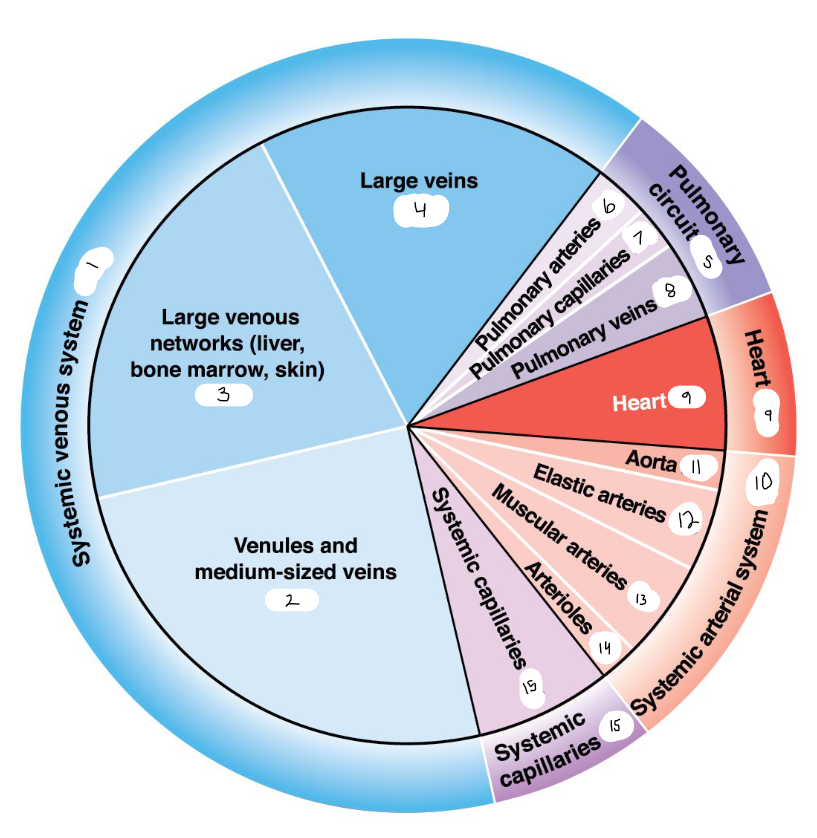
5
9
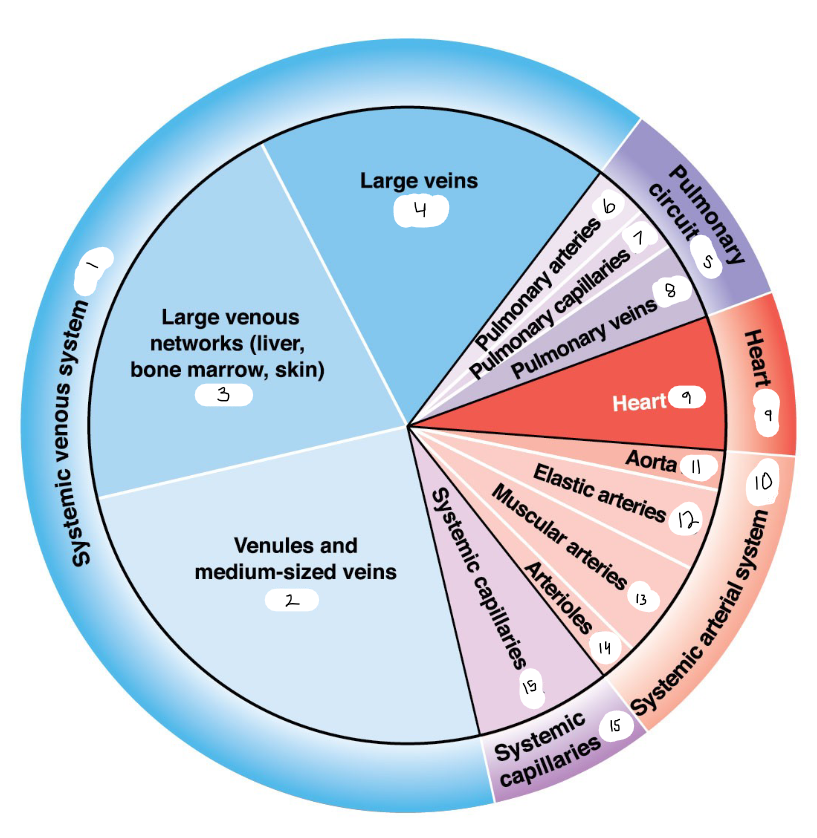
6
3
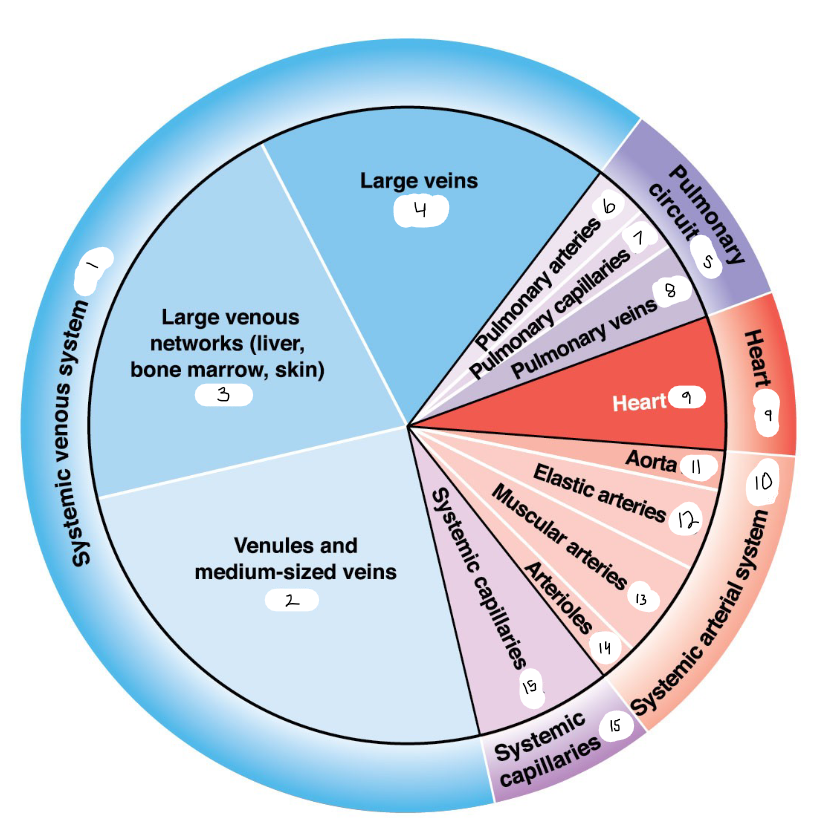
7
2
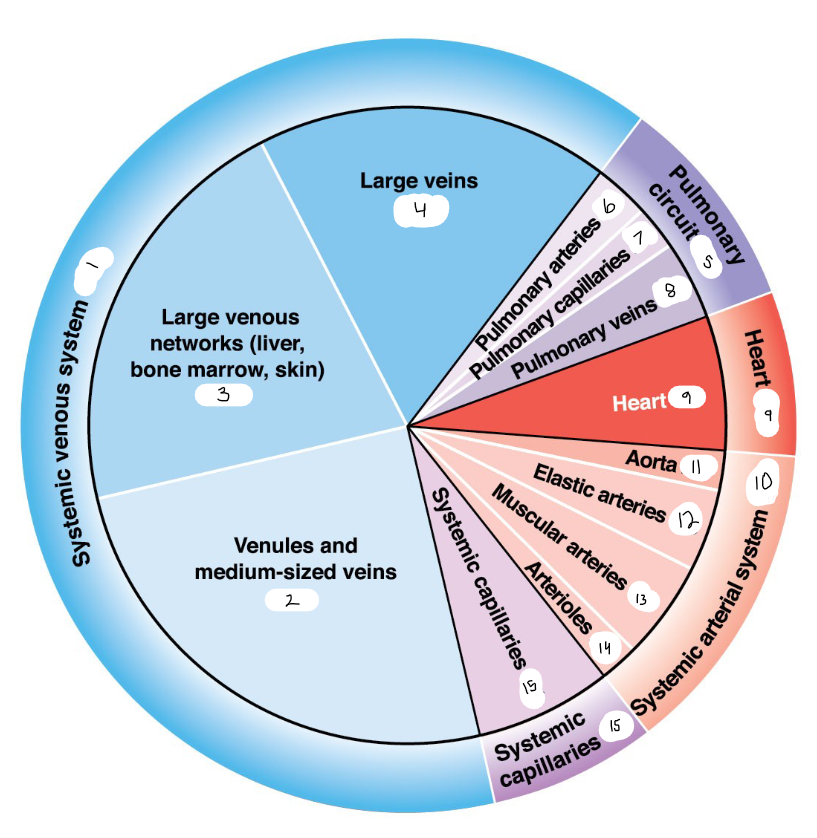
8
4
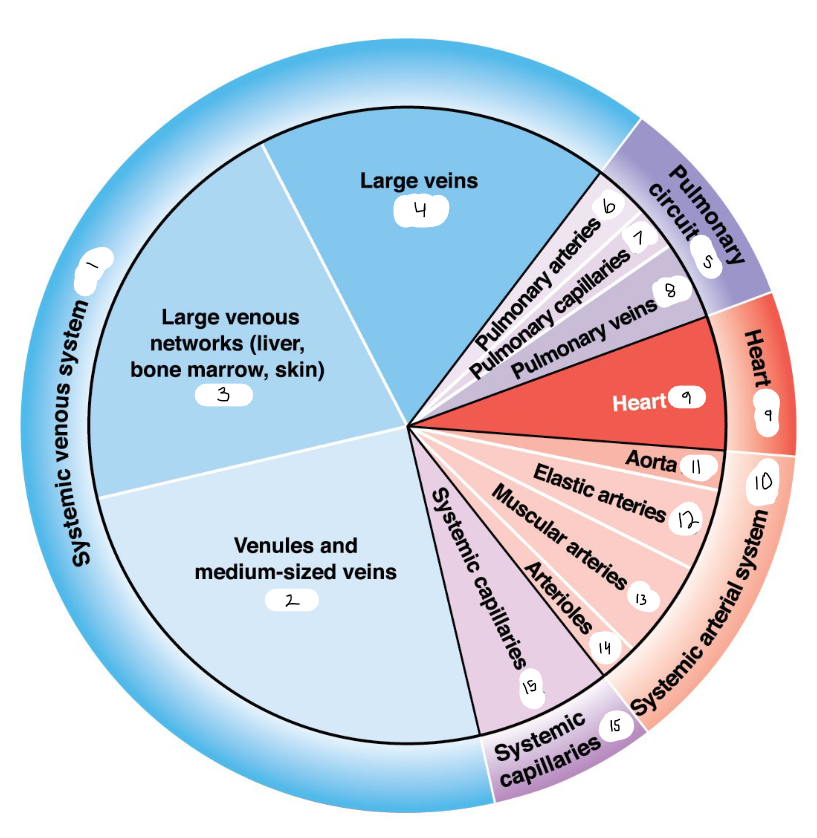
9
7
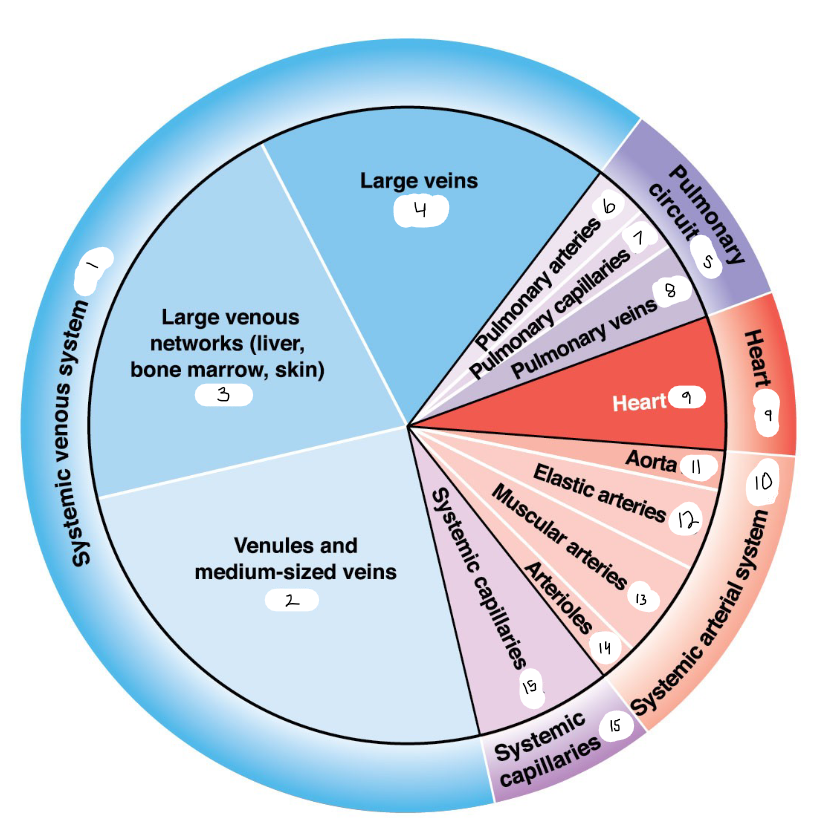
10
13
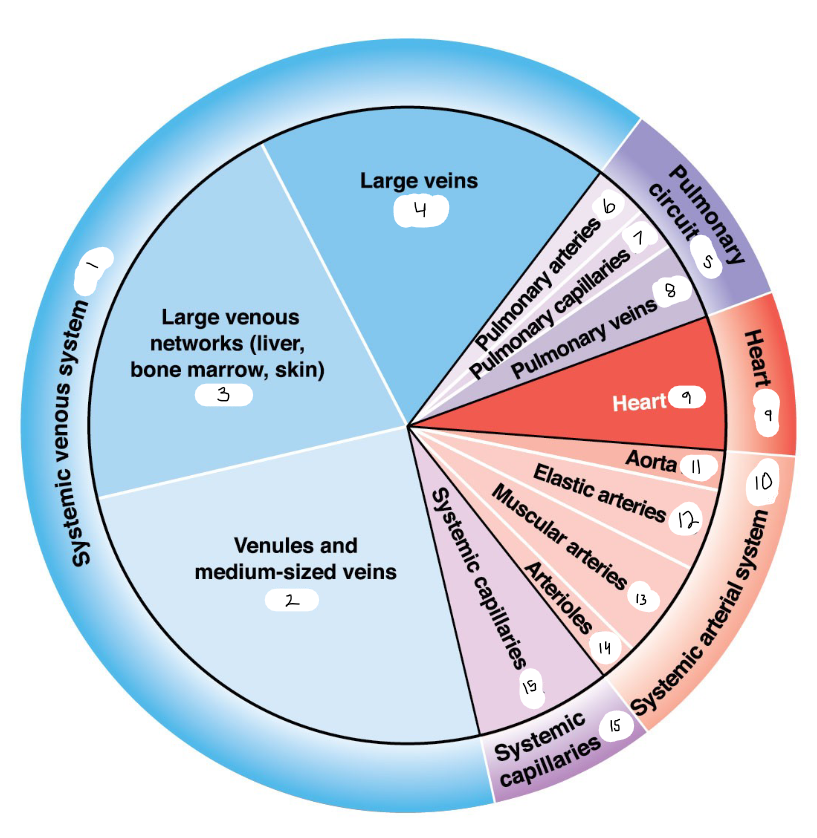
11
2
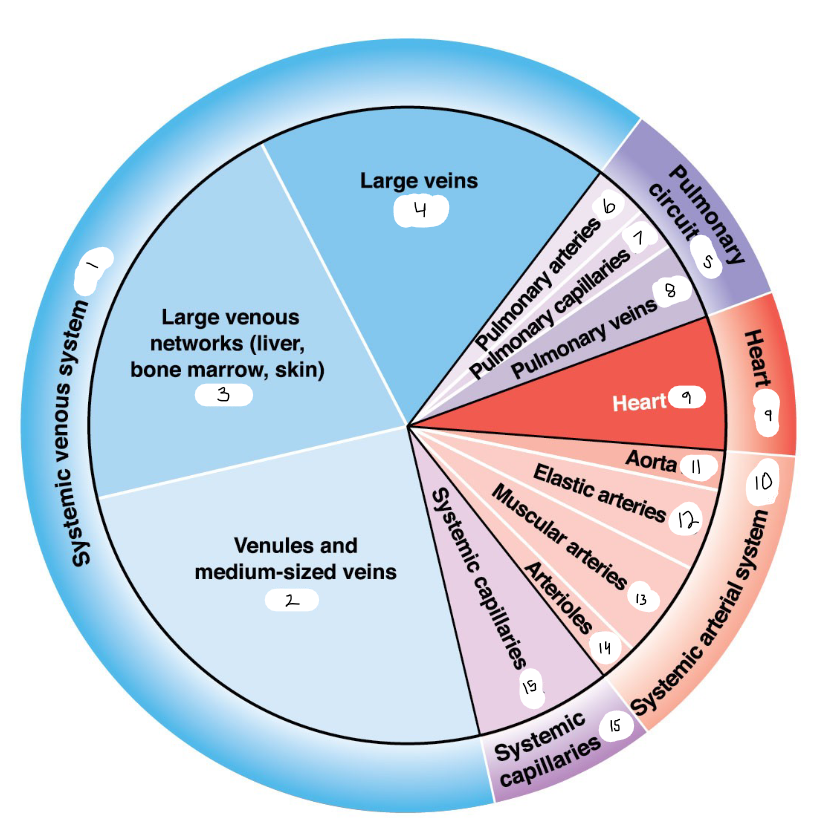
12
4
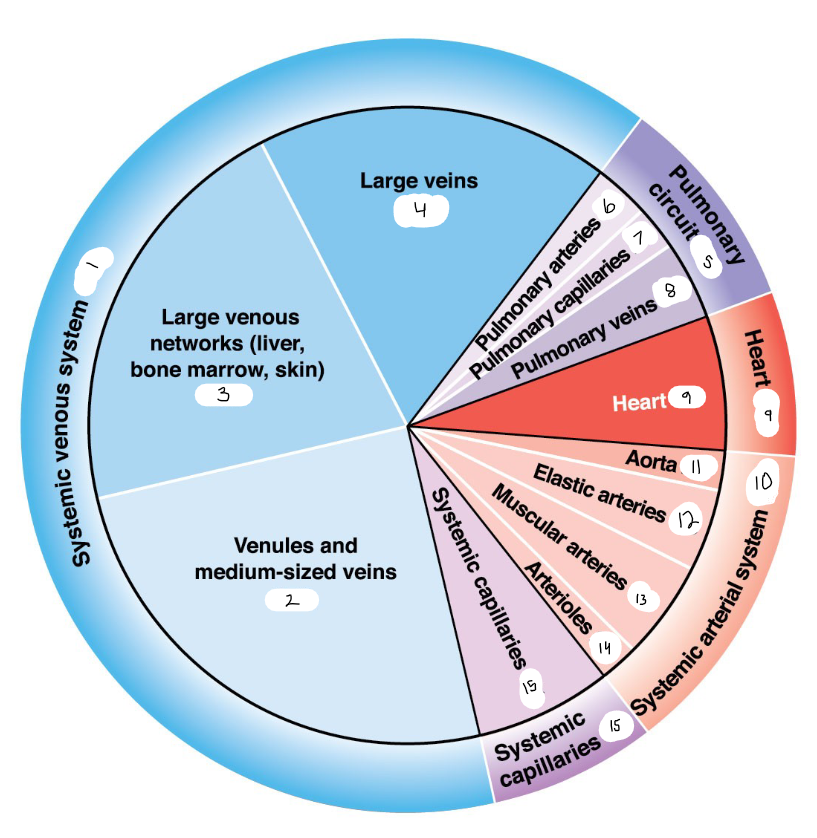
13
5
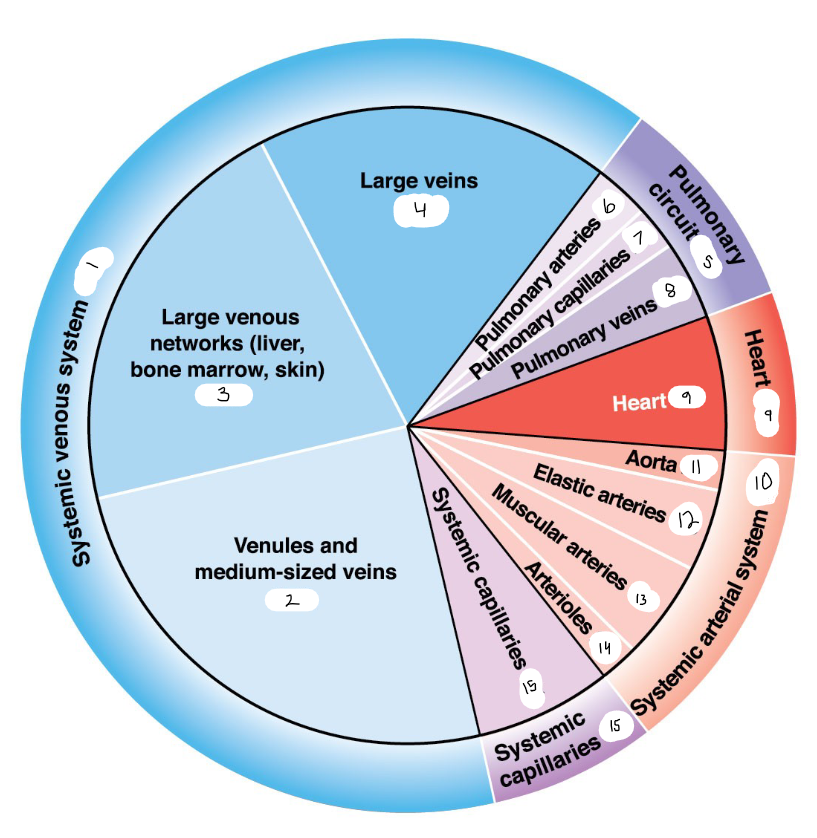
14
2
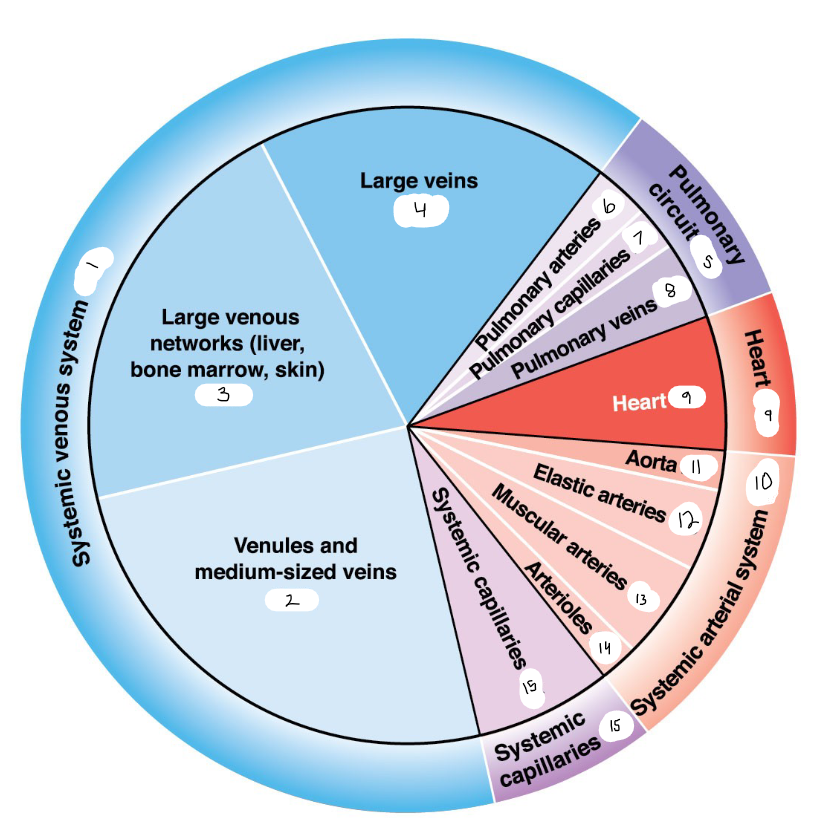
15
7
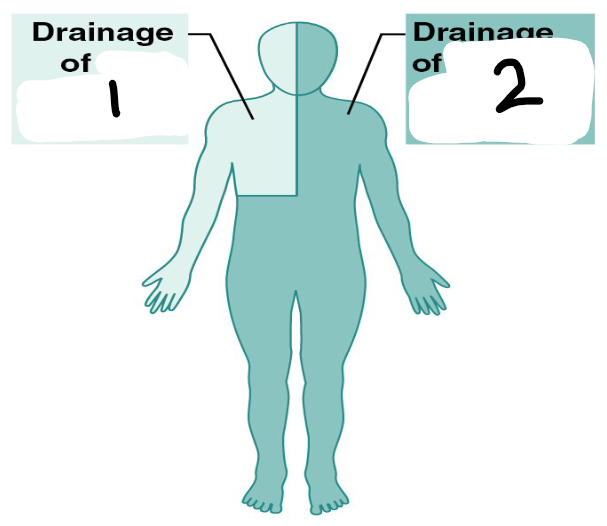
1
right lymphatic duct
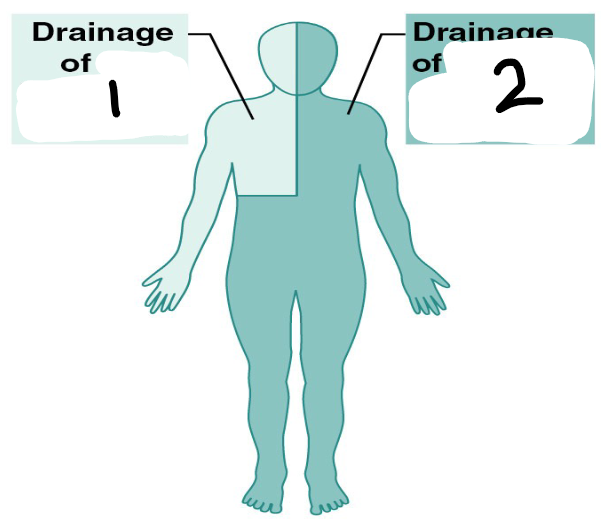
2
thoracic duct
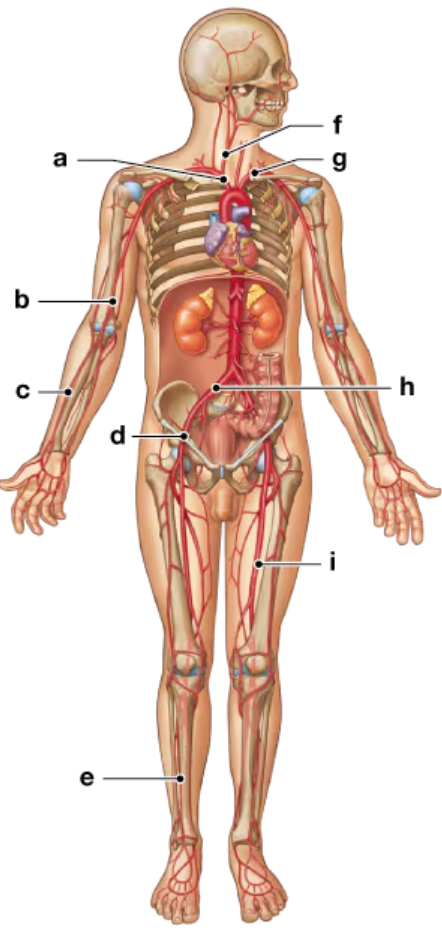
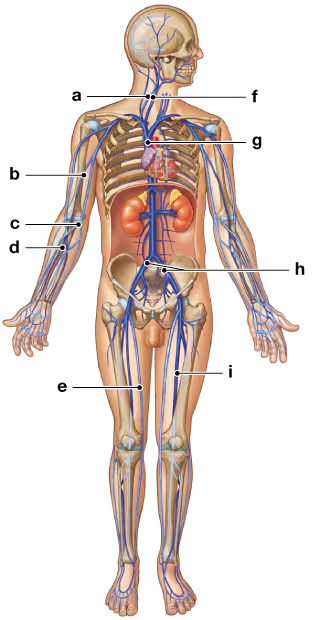
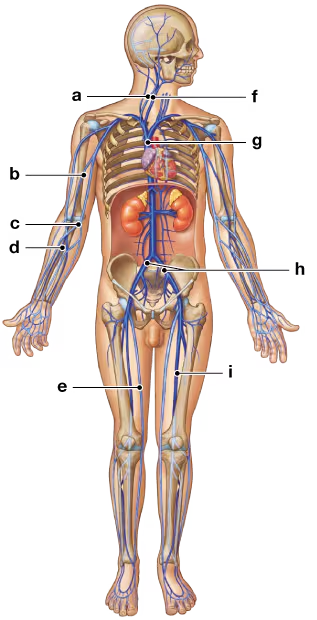
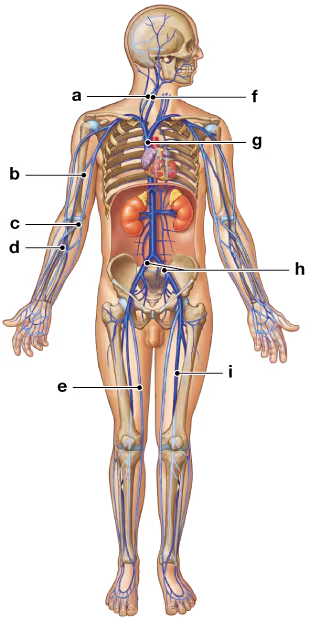
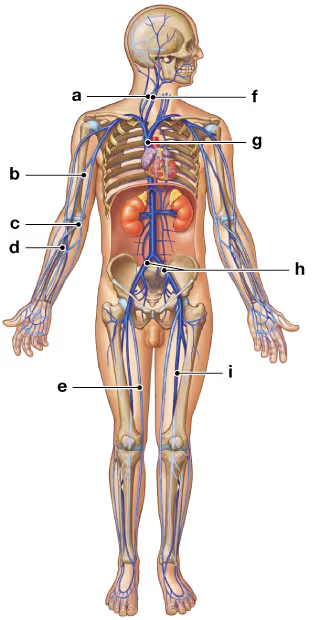
a
brachiocephalic trunk
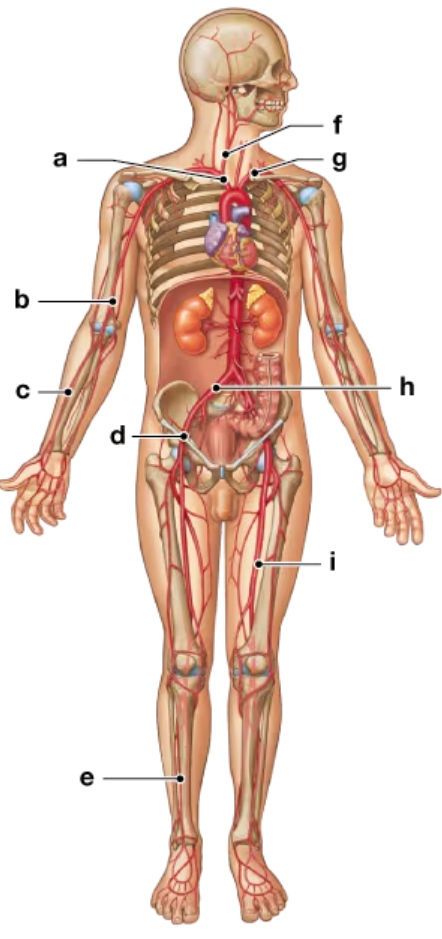
b
brachial
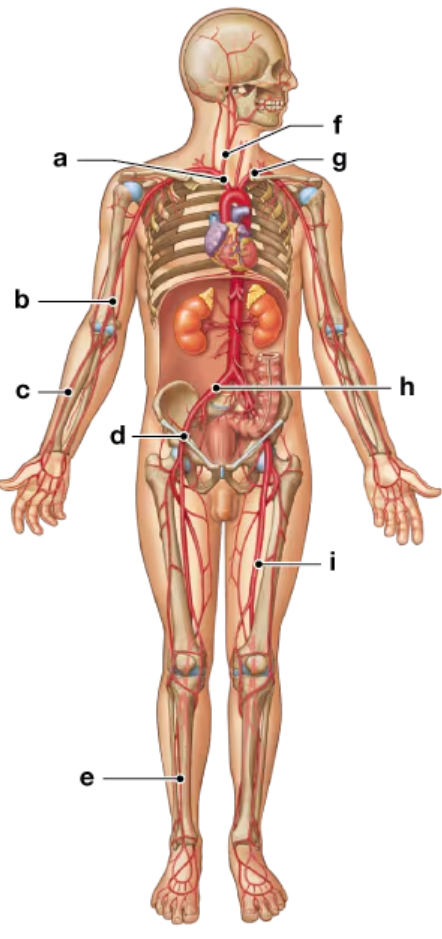
c
radial
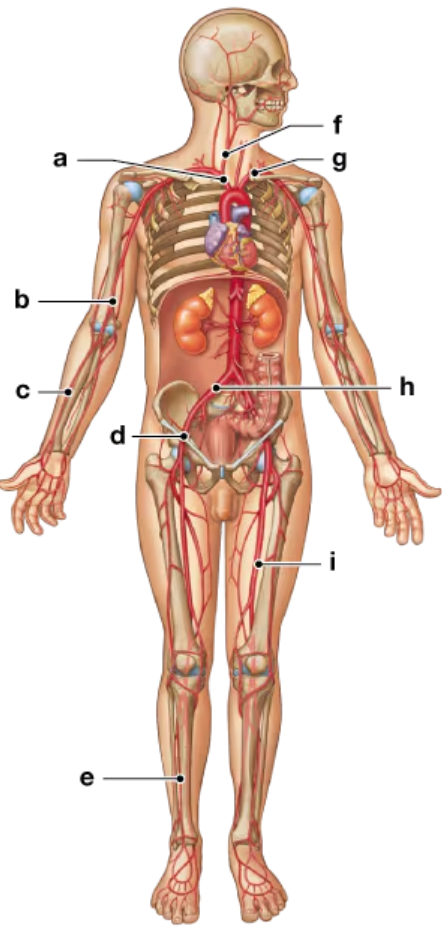
d
external iliac
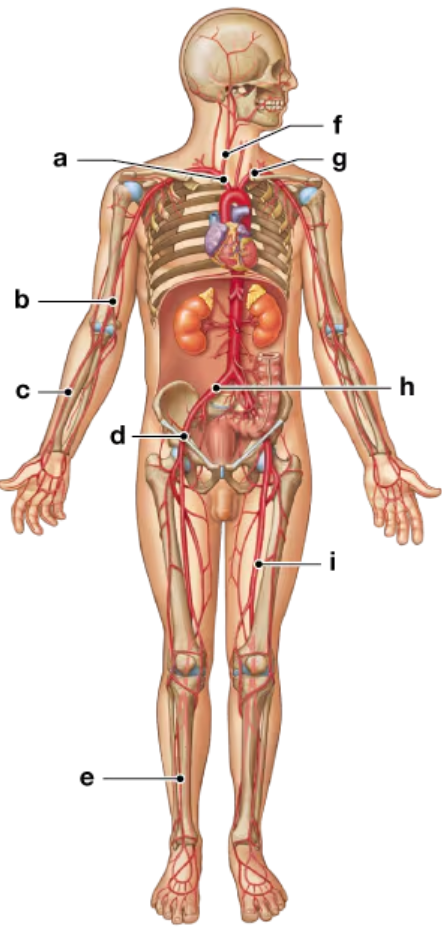
e
anterior tibial
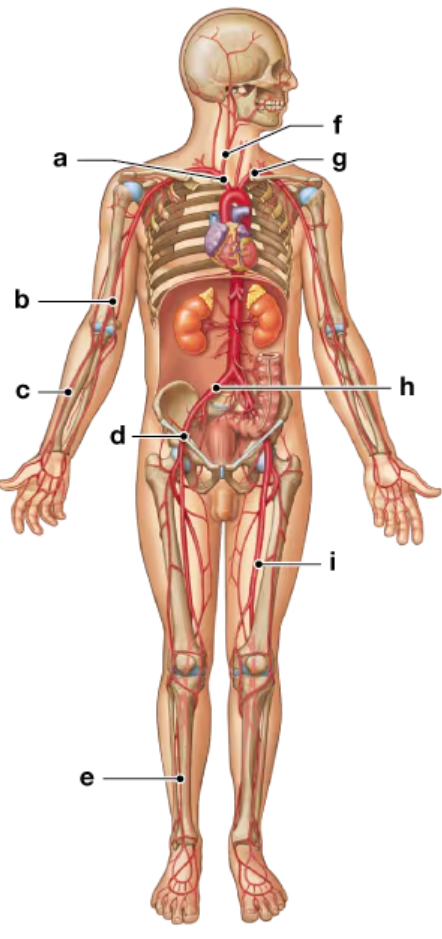
f
right common cartoid
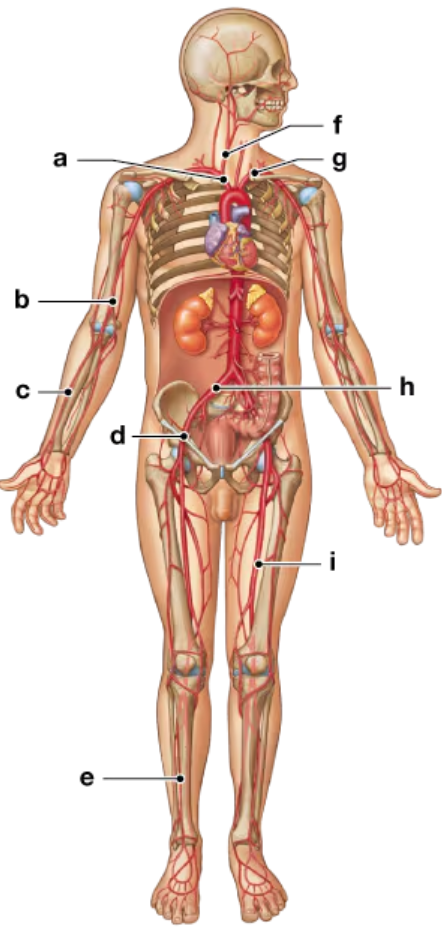
g
left subclavian
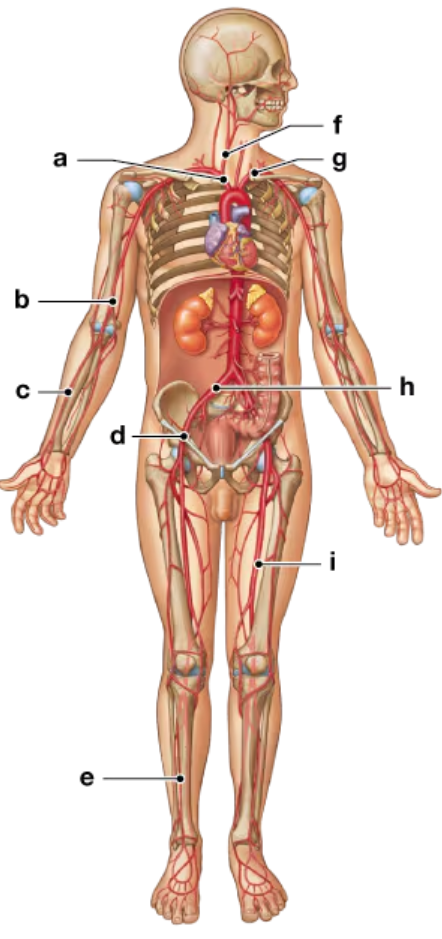
h
common iliac
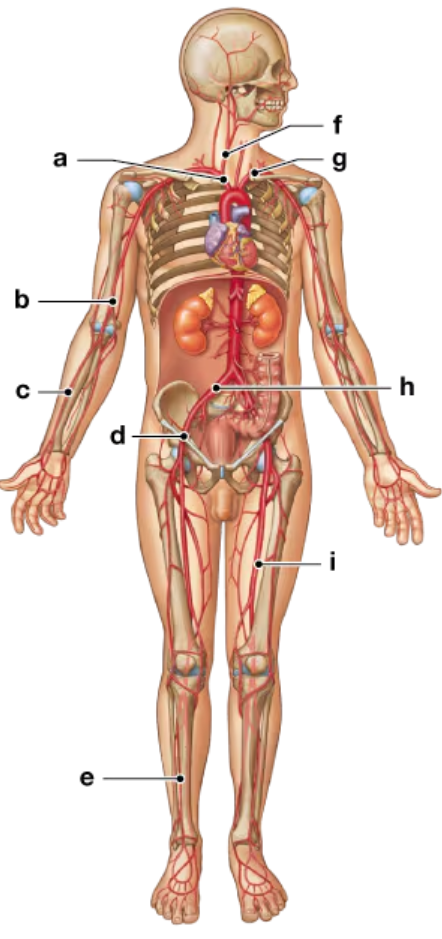
i
femoral
The blood vessels that play the most important role in regulating blood pressure and blood flow to a tissue are the
arterioles
Cardiovascular function is regulated by all of the following except (a) local factors, (b) neural factors, (c) endocrine factors, (d) venous return, (e) conscious control.
e
4Baroreceptors that function in the regulation of blood pressure are located in the
Carotid Sinus
5 The two-way exchange of substances between blood and body cells occurs only through
capillaries
6 Large molecules such as peptides and proteins move into and out of the bloodstream by way of
fenestrated capillaries
7 The local control of blood flow due to the action of precapillary sphincters is
autoregulation
8 Blood is transported through the venous system by means of (a) skeletal muscle contractions, (b) decreasing blood pressure, (c) the respiratory pump, (d) a and c.
d
a
external jugular
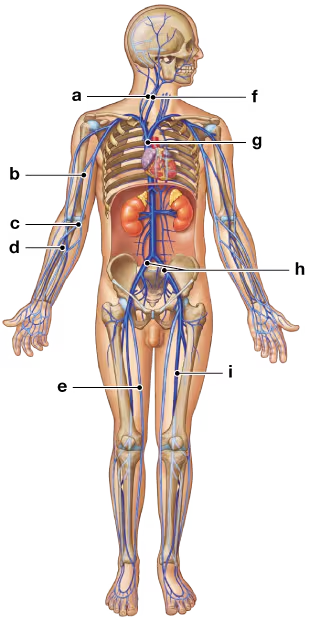
b
brachial
c
median cubital
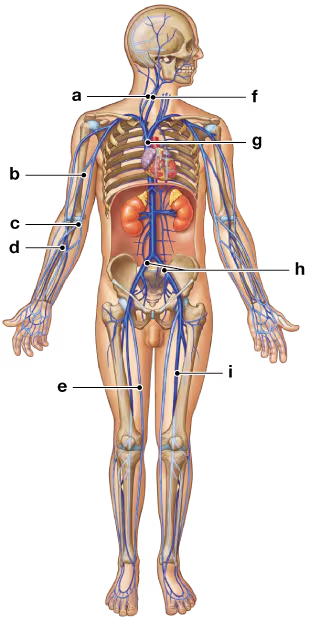
d
radial
e
great saphenous
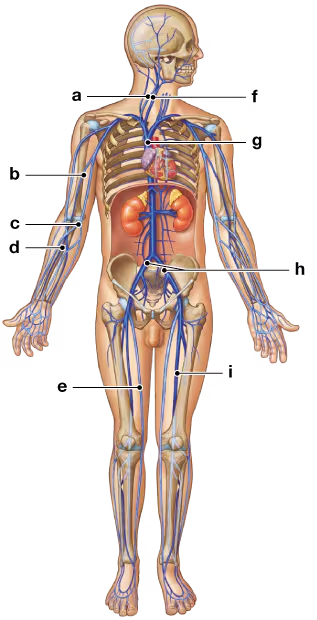
f
internal jugular
g
superior vena cava
h
left and right common iliac
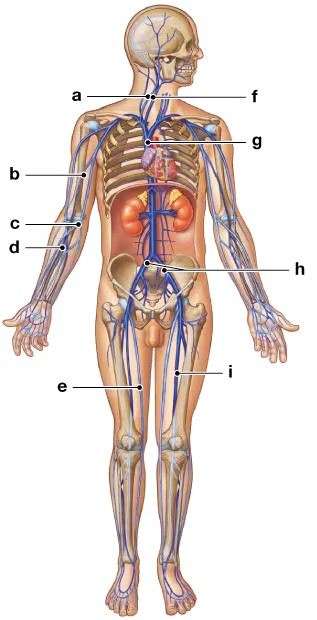
i
femoral
10 The most important factor in vascular resistance is (a) the viscosity of the blood, (b) the diameter of the lumen of blood vessels, (c) turbulence due to irregular surfaces of blood vessels, (d) the length of the blood vessels.
b
11 Net hydrostatic pressure forces water a capillary; net osmotic pressure reabsorbs water a capillary
out of, into
12 The two arteries formed by the division of the brachiocephalic trunk are the (a) aorta and internal carotid, (b) axillary and brachial, (c) external and internal carotid, (d) common carotid and subclavian.
d
13 The unpaired arteries supplying blood to the visceral organs include (a) the adrenal, renal, and lumbar arteries, (b) the iliac, gonadal, and femoral arteries, (c) the celiac and superior and inferior mesenteric arteries, (d) all of these.
c
14 The paired arteries supplying blood to the body wall and other structures outside the abdominopelvic cavity include the
iliac, femoral, and lumbar arteries
15 The vein that drains the dural sinuses of the brain is the
internal jugular vein
16 The vein that collects most of the venous blood inferior to the diaphragm is the
inferior vena cava
17 What are the primary forces that cause fluid to move (a) out of a capillary at its arterial end and into the interstitial fluid, (b) into a capillary at its venous end from the interstitial fluid?
(a) Capillary hydrostatic pressure forces fluid out of a capillary at the arterial end. (b) Blood colloid osmotic pressure causes the movement of fluid back into a capillary at its venous end.
18 What cardiovascular changes occur at birth?
When an infant takes its first breath, the lungs expand and pulmonary vessels dilate. The smooth muscles in the ductus arteriosus contract, due to increased venous return from the lungs, isolating the pulmonary and aortic trunks, and blood begins flowing through the pulmonary circuit. As pressure increases in the left atrium, the valvular flap closes the foramen ovale, completing the vascular remodeling.
19 A major difference between the arterial and venous systems is that (a) arteries are usually more superficial than veins, (b) in the limbs there is dual venous drainage, (c) veins are usually less branched compared to arteries, (d) veins exhibit a much more orderly pattern of branching in the limbs, (e) veins are not found in the abdominal cavity.
b
20 Which of the following conditions would have the greatest effect on peripheral resistance?
doubling the diameter of a vessel
21 Which of the following is greater? (a) the osmotic pressure of the interstitial fluid during inflammation, (b) the osmotic pressure of the interstitial fluid during normal conditions, (c) neither is greater.
a
22 Relate the anatomical differences between arteries and veins to their functions.
Artery walls are generally thicker and contain more smooth muscle and elastic fibers, enabling them to resist and adjust to the pressure generated by the heart. Venous walls are thinner; the pressure in veins is less than that in arteries. Arteries constrict more than veins do when not expanded by blood pressure, due to a greater degree of elastic tissue. Finally, the endothelial lining of an artery has a pleated appearance because it cannot contract and so forms folds. The lining of a vein looks like a typical endothelial layer.
23 Why do capillaries permit the diffusion of materials, whereas arteries and veins do not?
Capillary walls are thin, so distances for diffusion are short. Continuous capillaries have small gaps between adjacent endothelial cells that permit the diffusion of water and small solutes into the surrounding interstitial fluid but prevent the loss of blood cells and plasma proteins. Fenestrated capillaries contain pores that permit very rapid exchange of fluids and solutes between interstitial fluid and plasma. The walls of arteries and veins are several cell layers thick and are not specialized for diffusion.
24 How is blood pressure maintained in veins to counter the force of gravity?
Contraction of the surrounding skeletal muscles squeezes venous blood toward the heart. This mechanism, the muscular pump, is assisted by the presence of valves in the veins, which prevent backflow of the blood. The respiratory pump, which results from the increase in internal pressure of the thoracic cavity during exhalation, pushes venous blood into the right atrium.
25 How do pressure and resistance affect cardiac output and peripheral blood flow?
Cardiac output and peripheral blood flow are directly proportional to blood pressure. Blood pressure is closely regulated by a combination of neural and hormonal mechanisms. The resistance of the vascular system opposes the movement of blood, so blood flow is inversely proportional to the resistance. Sources of peripheral resistance include vascular resistance, blood viscosity, and turbulence.
26 Why is blood flow to the brain relatively continuous and constant?
The brain receives arterial blood from four arteries that form anastomoses within the cranium. An interruption of any one vessel will not compromise the blood flow to the brain.
27 Compare the effects of the cardioacceleratory and cardioinhibitory centers on cardiac output and blood pressure.
The cardioacceleratory and vasomotor centers are stimulated when general sympathetic activation occurs. The result is an increase in cardiac output and blood pressure. When the parasympathetic division is activated, the cardioinhibitory center is stimulated, reducing cardiac output.
28 Bob is sitting outside on a warm day and is sweating profusely. Mary wants to practice taking blood pressures, and he agrees to play the patient. Mary finds that Bob’s blood pressure is elevated, even though he is resting and has lost fluid from sweating. (She reasons that fluid loss should lower blood volume and, thus, blood pressure.) Why is Bob’s blood pressure high instead of low?
Fluid loss lowers blood volume, leading to sympathetic stimulation, which elevates blood pressure. So, Bob’s blood pressure is high instead of low.
29 People with allergies commonly take antihistamines with decongestants to relieve their symptoms. The container warns that individuals who are being treated for high blood pressure should not take the medication. Why not?
Antihistamines and decongestants are sympathomimetic drugs; they have the same effects on the body as does stimulation of the sympathetic nervous system. In addition to the desired effects of counteracting the symptoms of the allergy, these medications can produce an increased heart rate, increased stroke volume, and increased peripheral resistance, all of which will contribute to elevating blood pressure. In a person with hypertension (high blood pressure), these drugs would aggravate this condition, with potentially hazardous consequences.
30 Jolene awakens suddenly to the sound of her alarm clock. Realizing that she is late for class, she jumps to her feet, feels light-headed, and falls back on her bed. What probably caused this reaction? Why doesn’t this happen all the time?
When Jolene stood up rapidly, gravity caused her blood volume to move to the lower parts of her body away from the heart, decreasing venous return. The decreased venous return resulted in a decreased end-diastolic volume (EDV), leading to a decreased stroke volume and cardiac output. In turn, blood flow to the brain decreased, so the diminished oxygen supply caused her to be light-headed and feel faint. This reaction doesn’t happen all the time because as soon as the pressure drops due to inferior movement of blood, baroreceptors in the aortic arch and carotid sinuses trigger the baroreceptor reflex. Action potentials are carried to the medulla oblongata, where appropriate responses are integrated. In this case, we would expect an increase in peripheral resistance to compensate for the decreased blood pressure. If this doesn’t compensate enough for the drop, then an increase in heart rate and force of contraction would occur. Normally, these responses occur so quickly that changes in pressure following changes in body position go unnoticed.
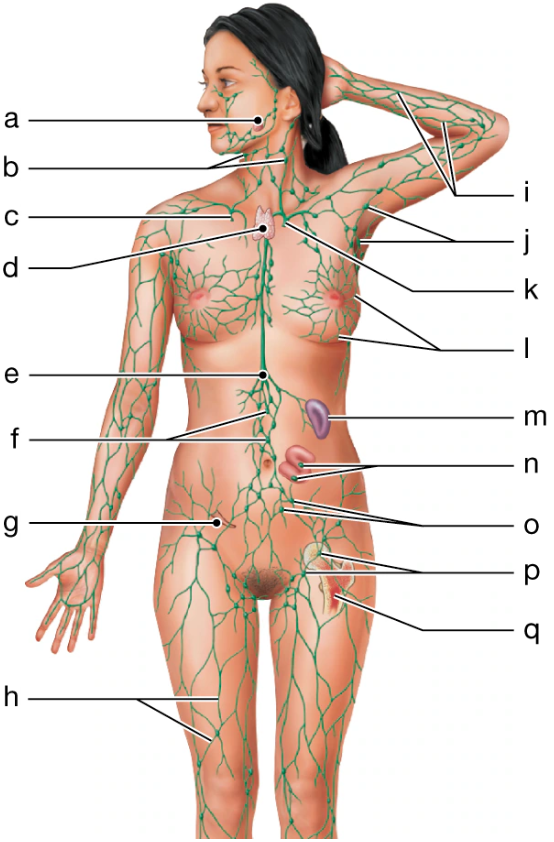
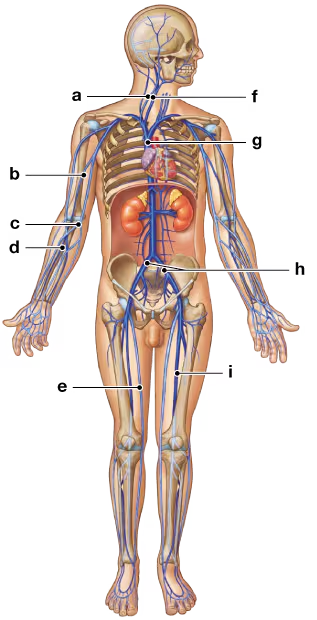
a
Tonsil
b
cervical lymph nodes
c
right lymphatic duct
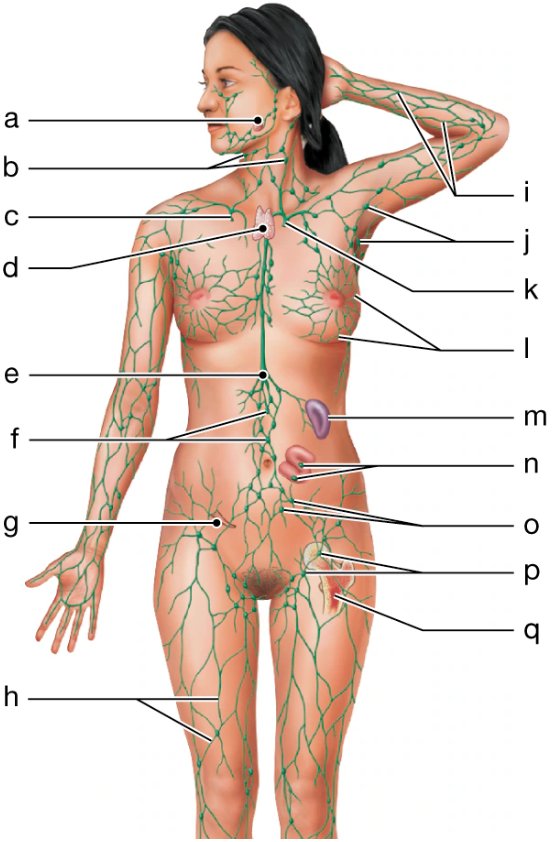
d
thymus
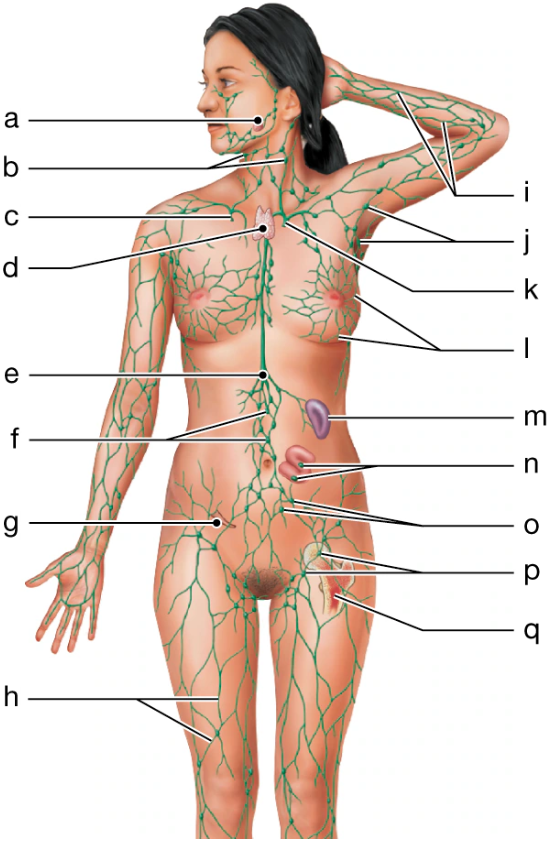
e
cisterna chyli
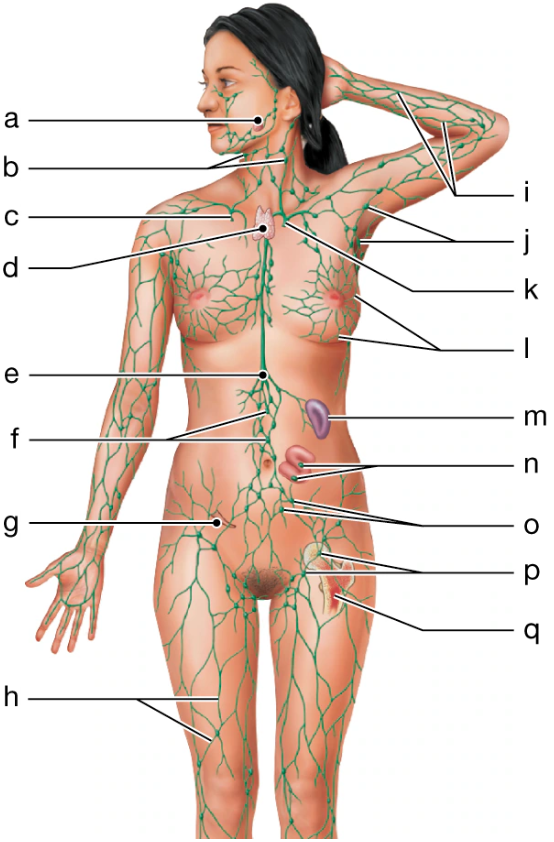
f
lumbar lymph nodes
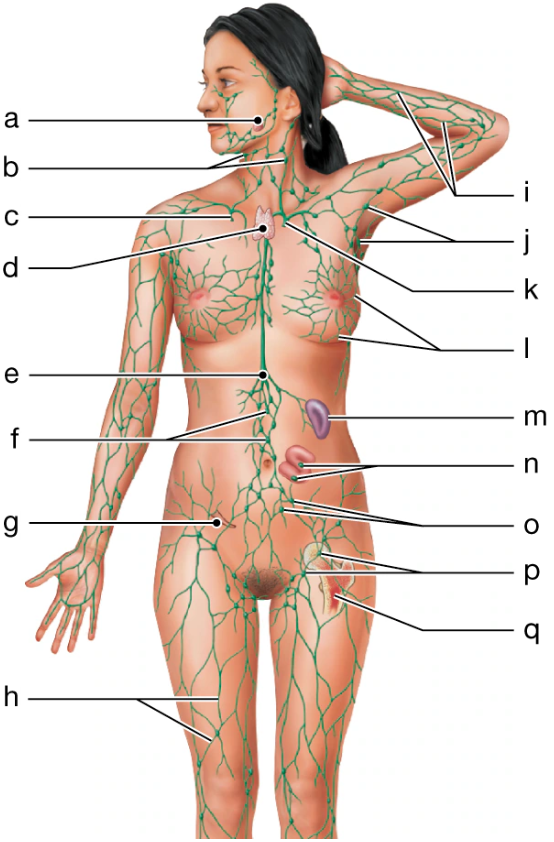
g
appendix
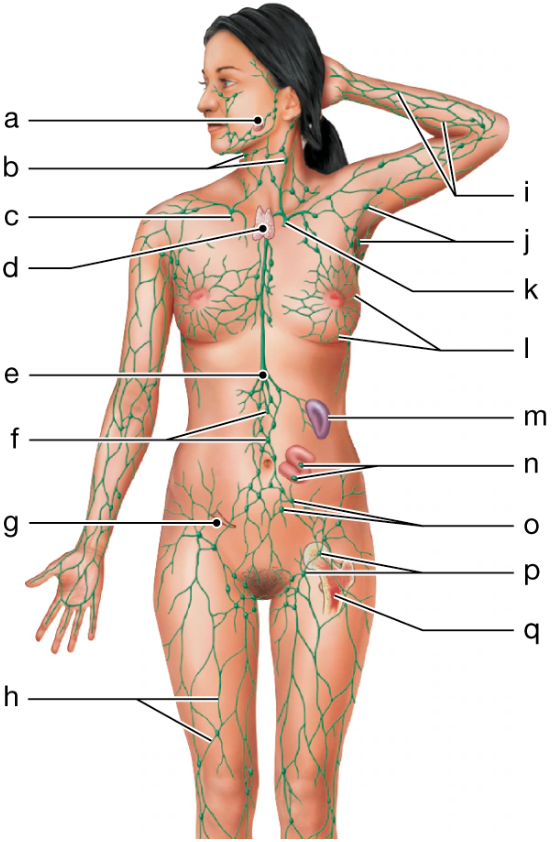
h
lymphatics of lower limb
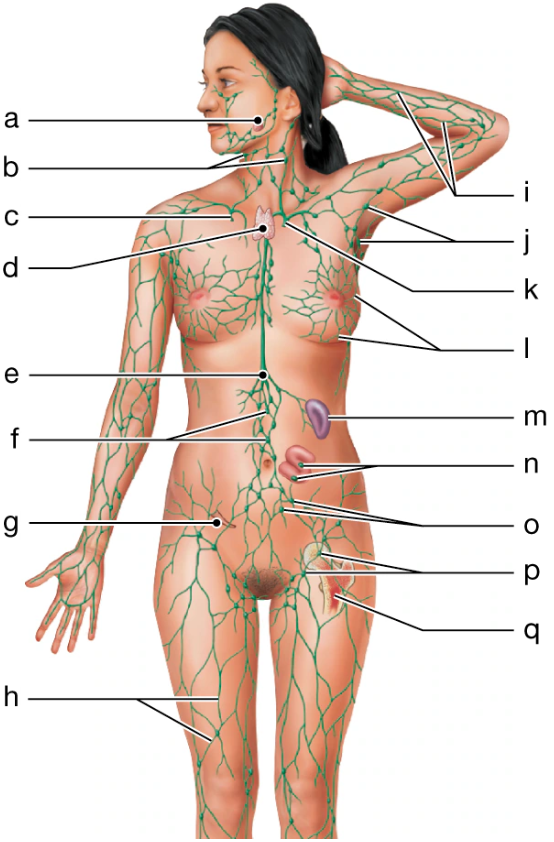
i
lymphatics of upper limb
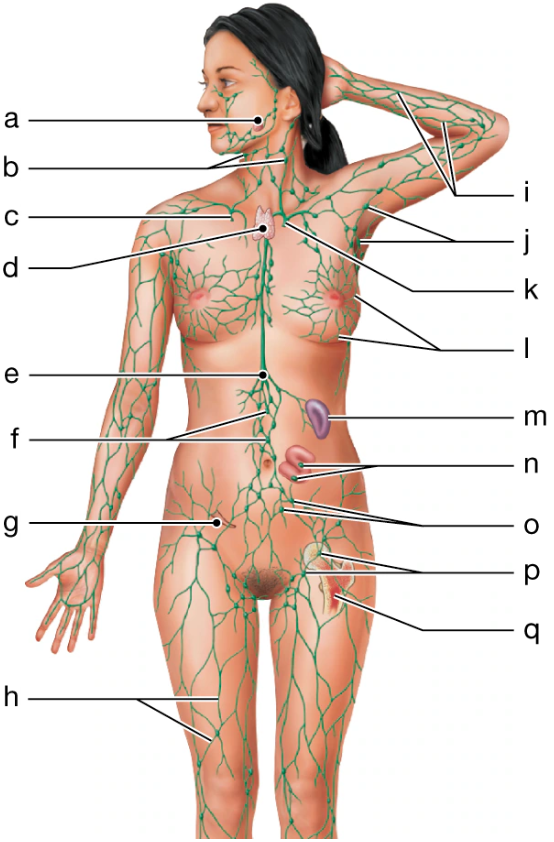
j
axillary lymph nodes
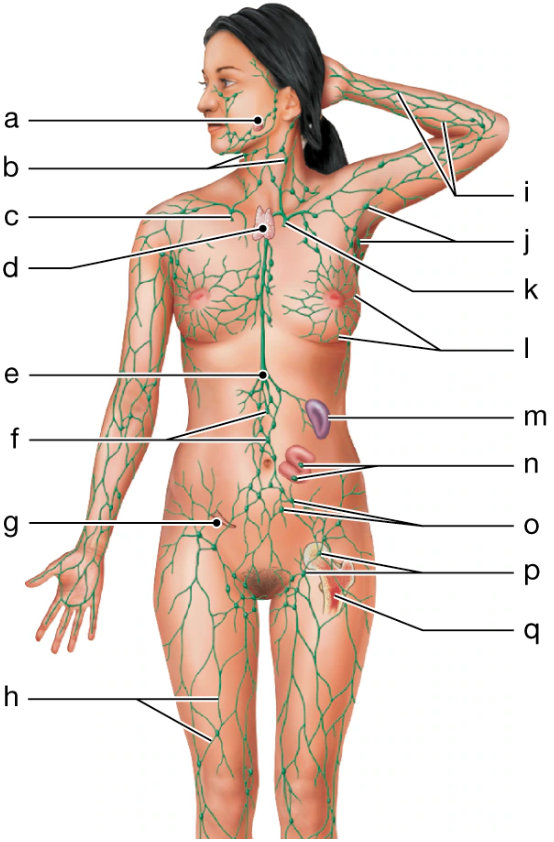
k
thoracic duct
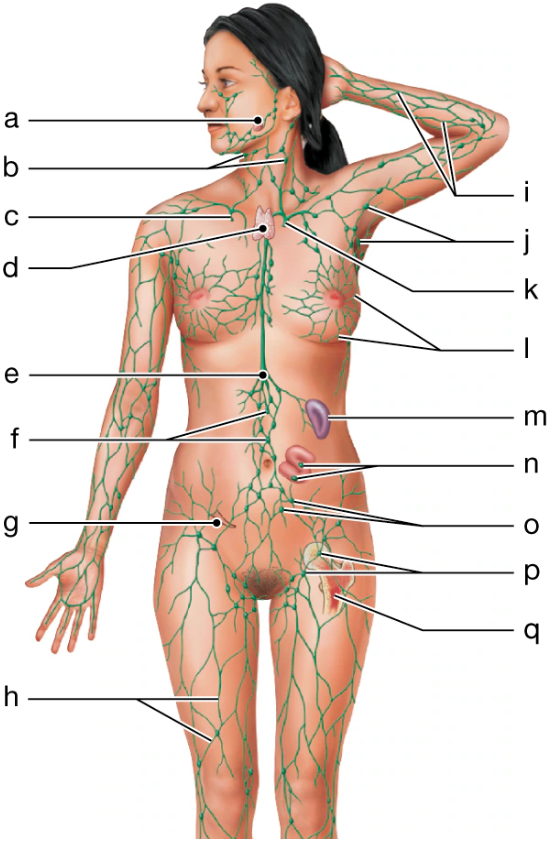
l
lymphatics of mammary gland
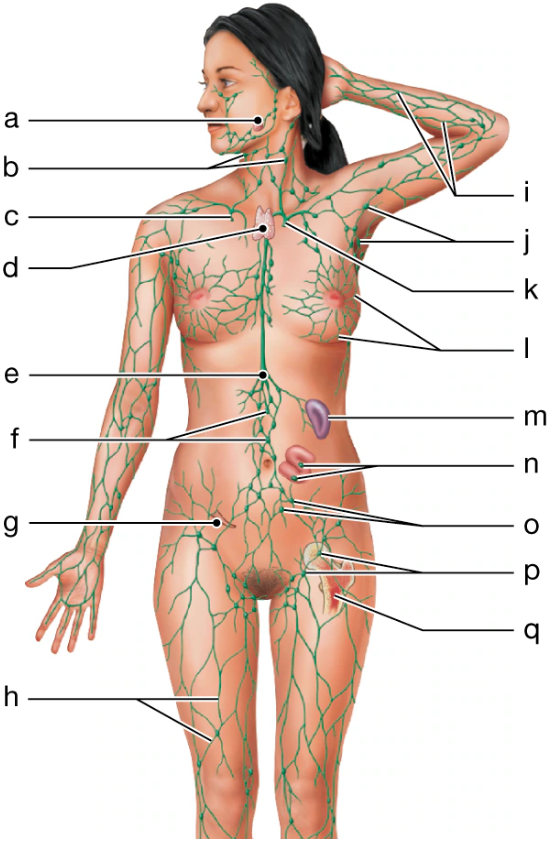
m
Spleen
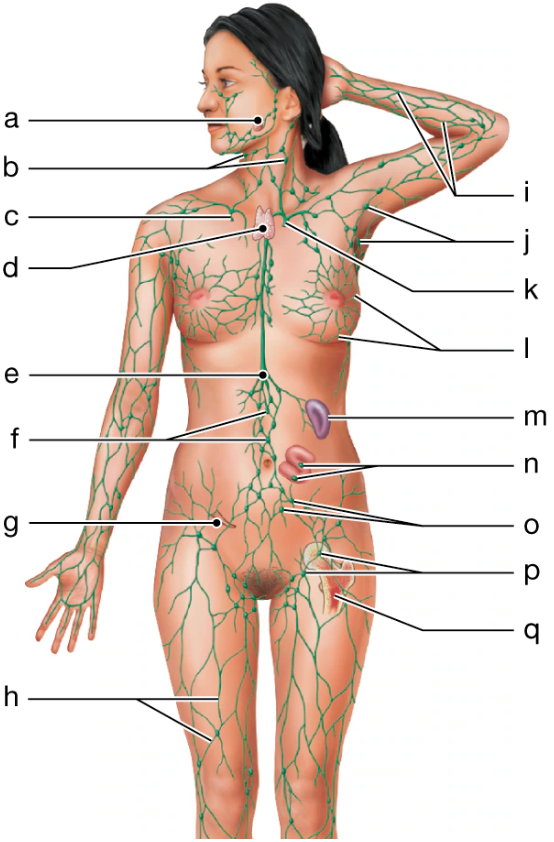
n
mucosa-associated lymphoid tissue

o
pelvic lymph nodes

p
inguinal lymph nodes
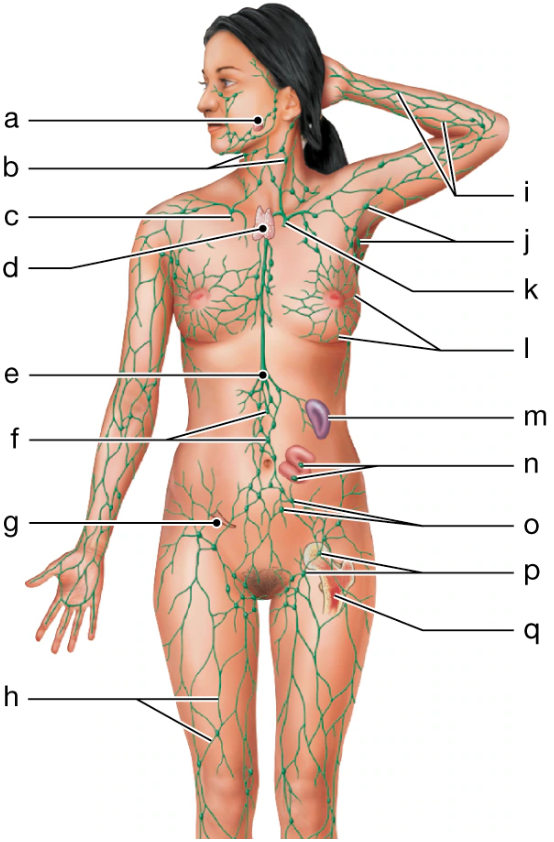
q
red bone marrow
Lymph from the right arm, the right half of the head, and the right chest is received by the
right lymphatic duct
Anatomically, lymphatic vessels resemble
medium veins