Papillomaviruses
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
Papillomaviruses
-non-enveloped, dsDNA virus with small circular genome, and an icosahedral capsid
-associated with warts and cancer (especially cervical cancer)
Prevalence of Papillomaviruses
• Widespread in nature, infecting many vertebrates including monkeys, dogs, cattle, and rabbits
• Highly species specific, so can't use the human virus in animal experiments
• 150+ human papilloma virus (HPV) types, based on nucleic acid homology
• HPV is the most common sexually transmitted infection in the United States.
• More than half of sexually active people are infected with one or more HPV types in their lives
• At any point in time, 43% of women have genital HPV, and 7% of adults have oral HPV
Which 2 strains of HPV cause the vast majority of cervical cancers?
HPV-16 and HPV-18
Why are HPV-16 and HPV-18 more likely to cause cancer than others?
-most other strains clear over time, but these stick around, making them more likely to be the ones to cause cancer
-also production of high levels of E6 and E7
Transmission of skin HPVs
transmitted via direct contact with an infected individual or a virus-contaminated surface
Transmission of genital tract HPVs
transmitted via sexual contact, where mucosal epithelial cells serve as reservoirs
HPV tissue specificity
most HPV strains can infect either skin OR mucosa (genital tract, oral, nasal...)
Which 2 HPV strains cause 90% of all genital warts, but are considered "low risk" because they're not associated with development of cancer?
HPV-6 and HPV-11
HPV virion
-small, icosahedral, non-enveloped
-Two capsid proteins- L1 and L2 (Mostly L1, making it a good vaccination target)
-72 capsomeres
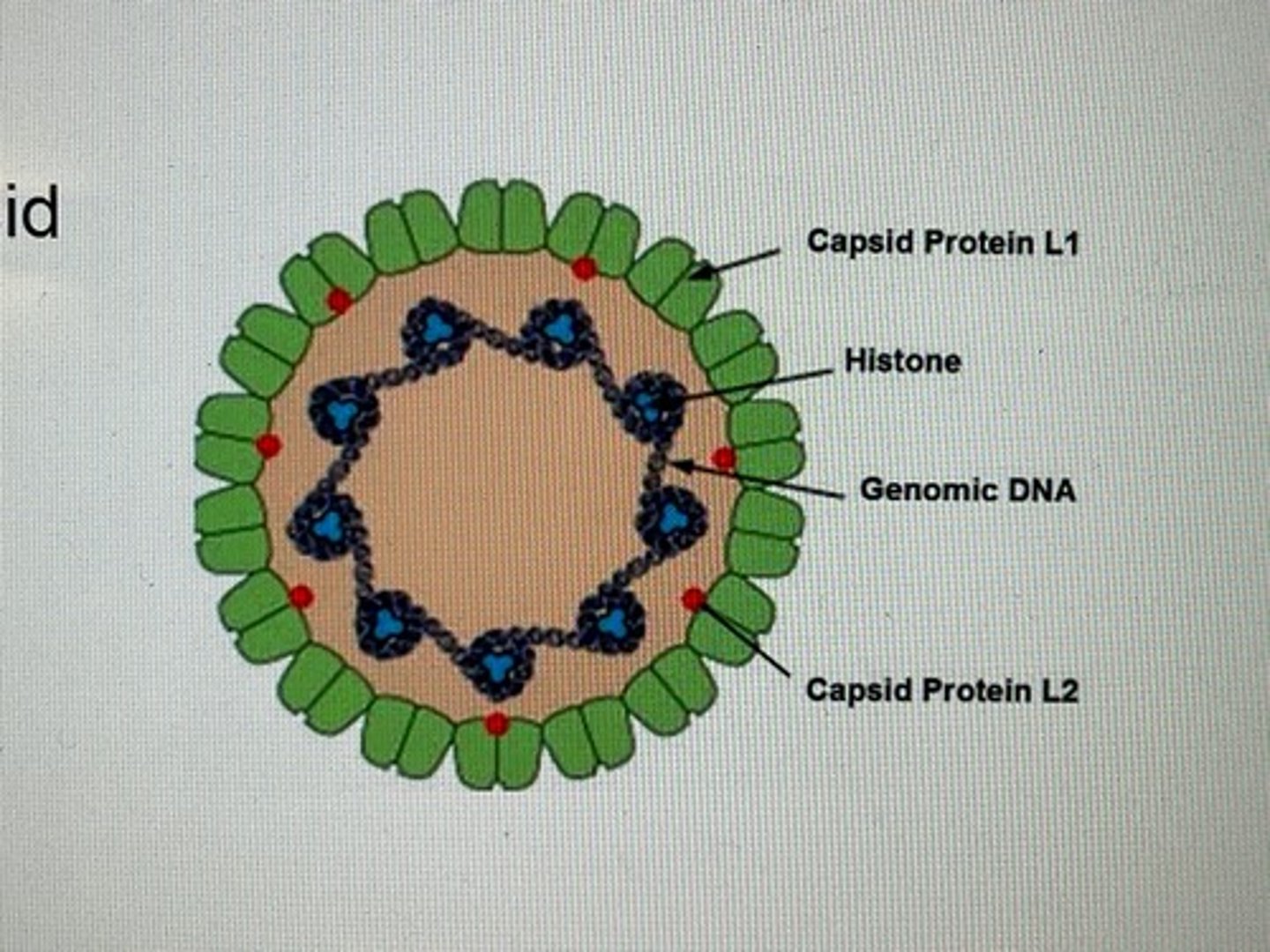
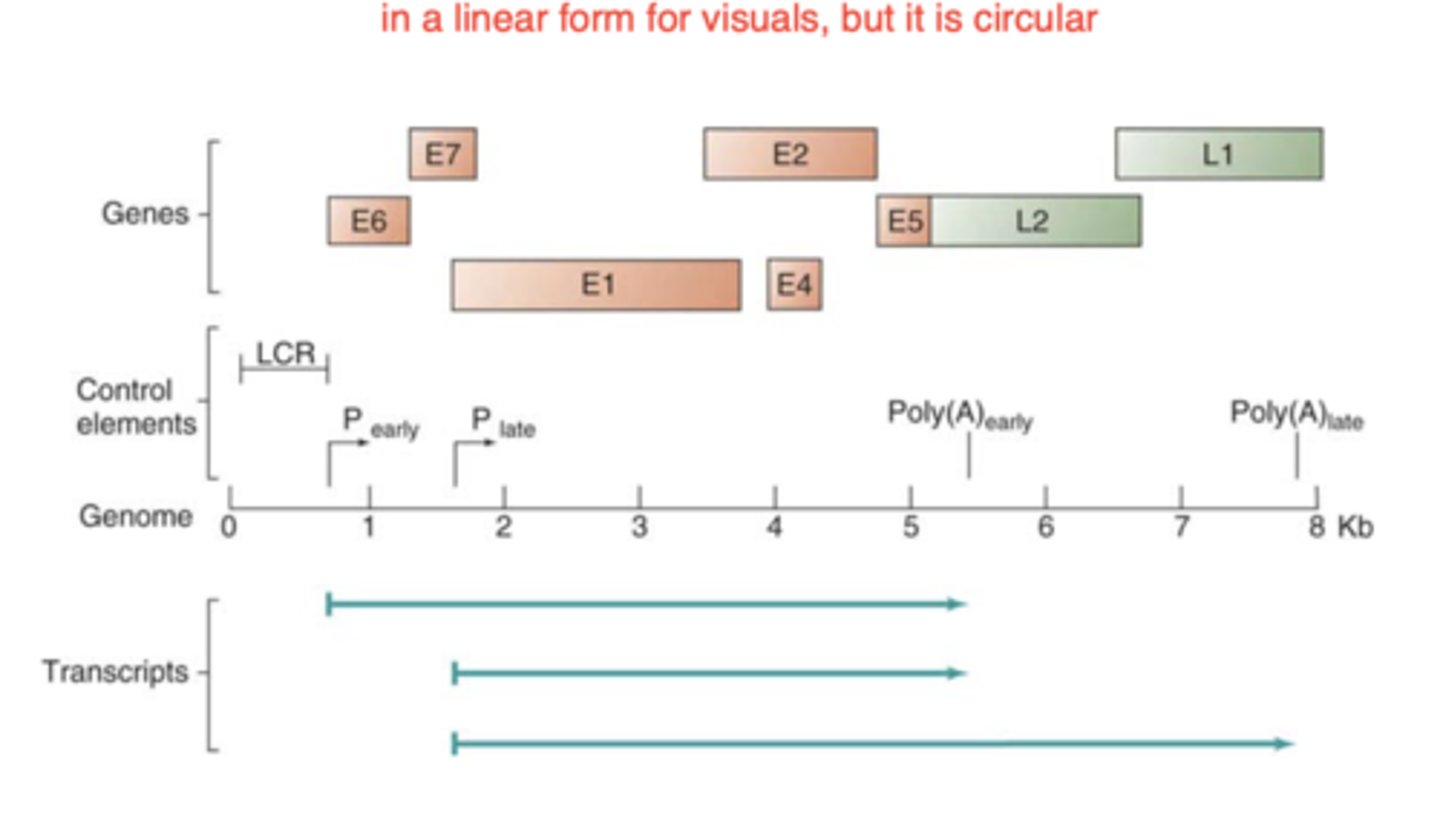
HPV-16 genome
-small, closed circular dsDNA complexed with histones in nucleosome structure
-8 genes (6 early, 2 late)
-LCR (long control region) contains replication origin and cis acting signals
What cell type do papillomaviruses infect in the epithelium?
stem cells (so it has to get through a break in the outer layers to access these cells)
Early gene expression of papillomavirus happens in...
basal cells
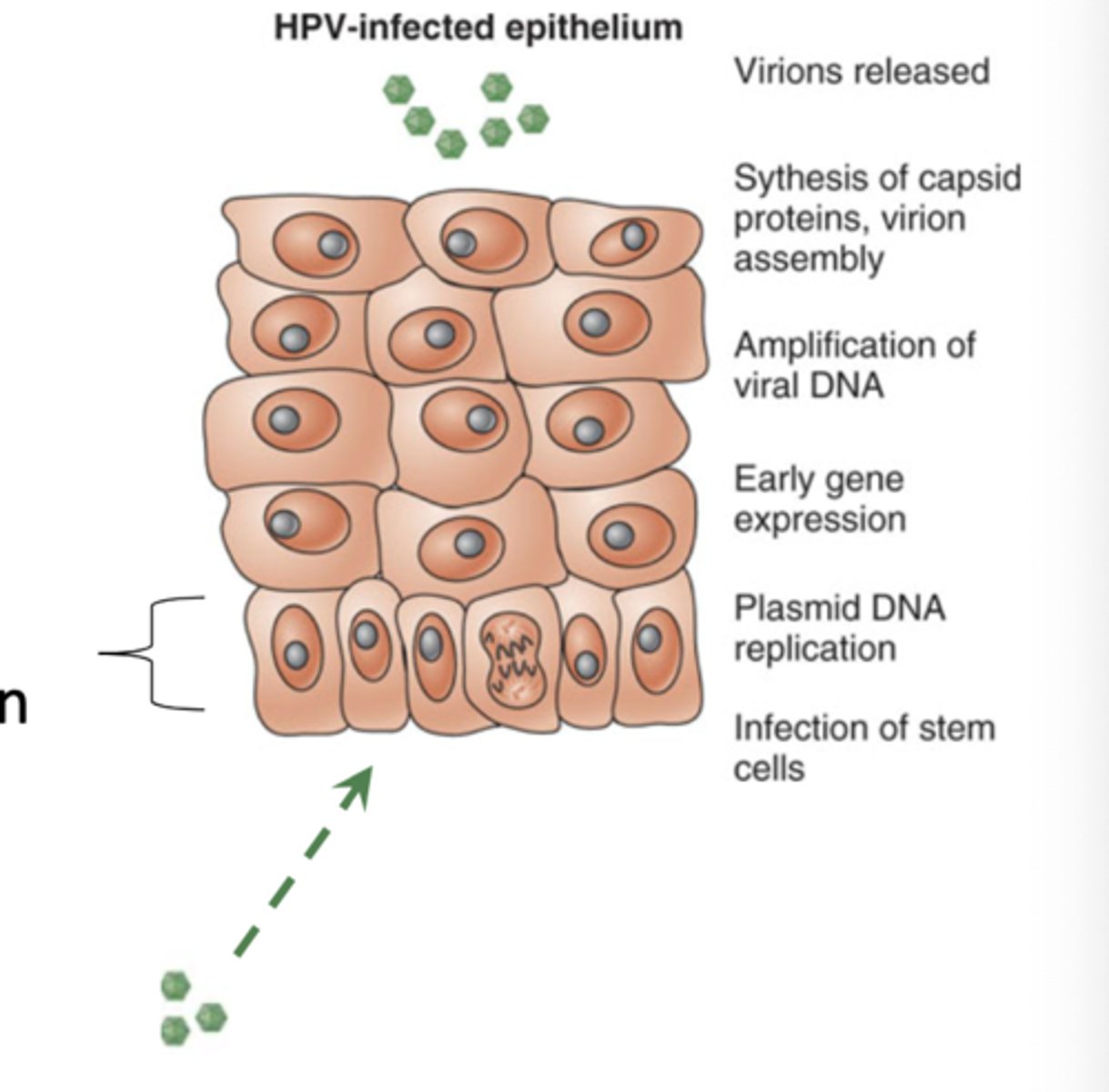
Late gene expression and assembly of viral particles of papillomavirus happens in...
keratinocytes
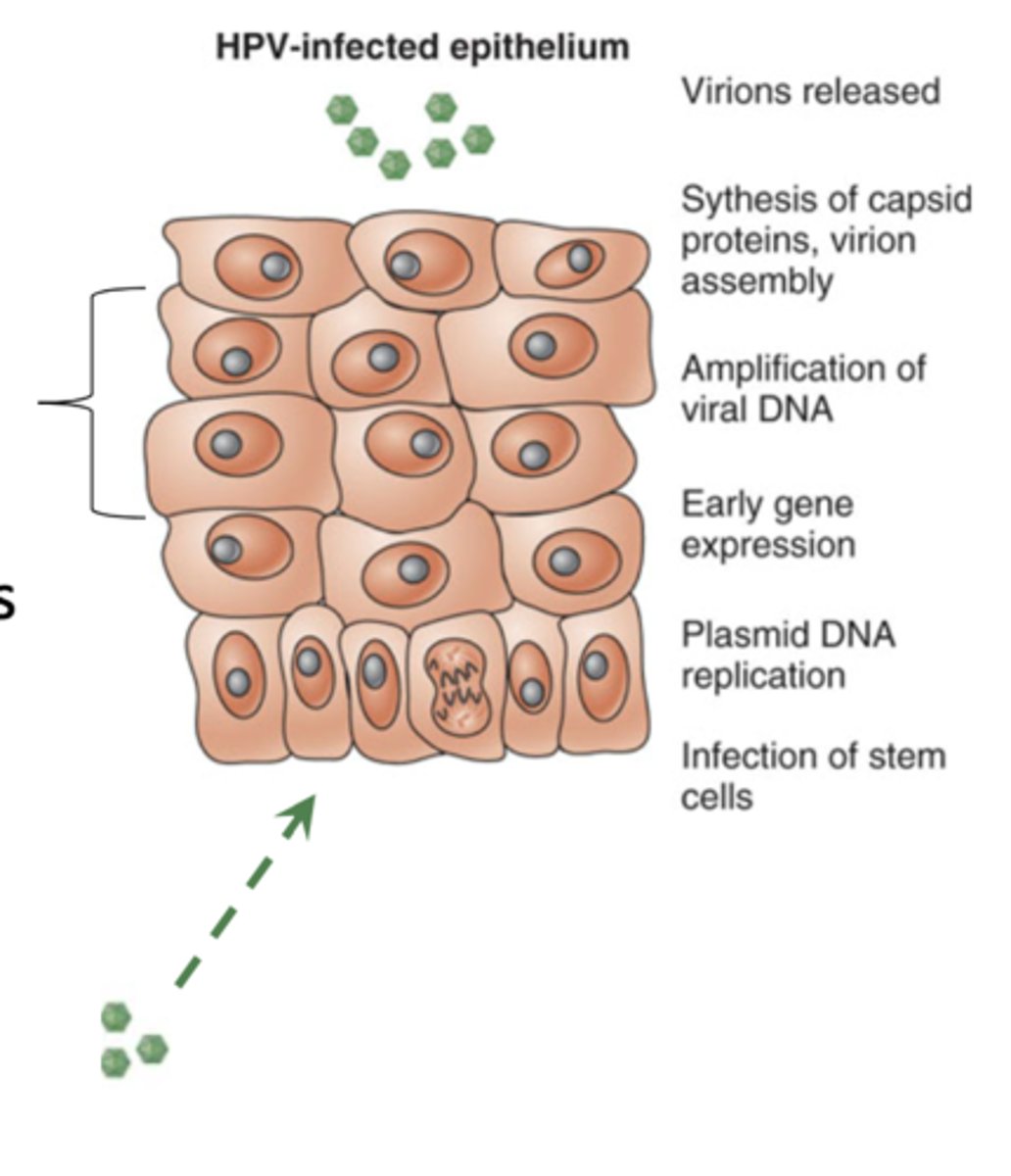
end of Papillomavirus life cycle
-virus keeps the cell cycle going and makes the cells keep their nuclei, so cells are still dividing and piling up on each other
-at the end, the cells on the outer layer begin to break and release virus
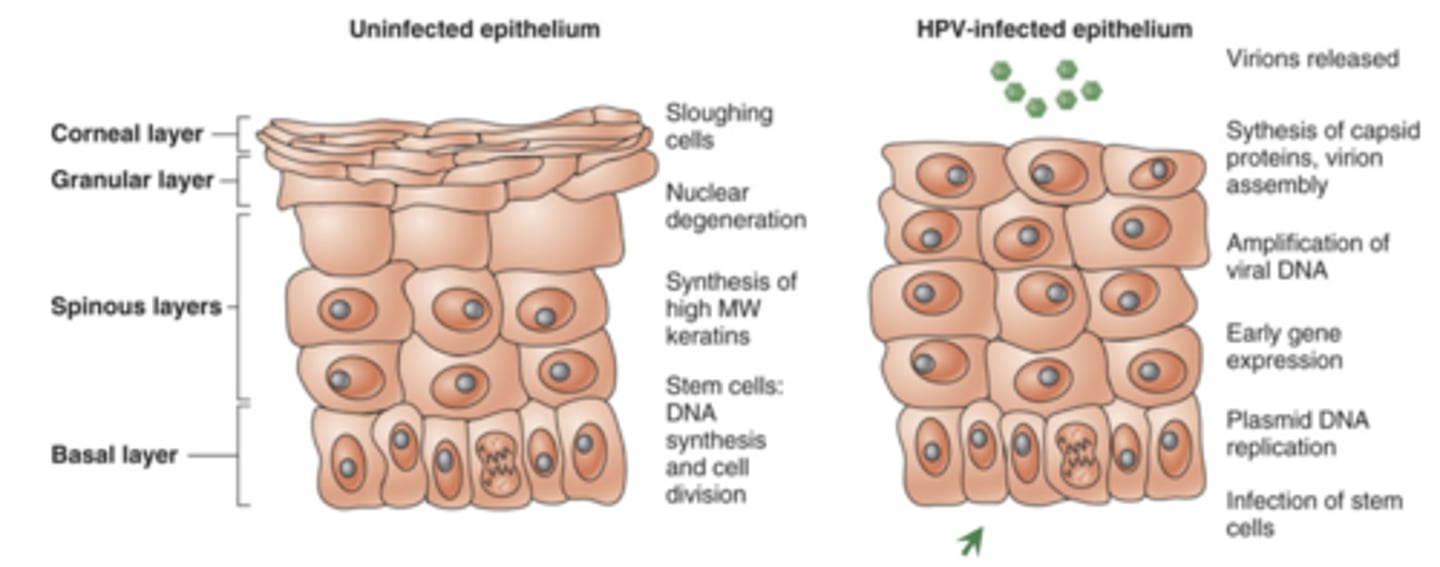
Hyperkeratosis
piling up of these papillomavirus infected skin cells due to continuous division induced by the virus, leading to worts
Papillomavirus early genes
6 total, important for replication (E1-7, skips 3)
Papillomavirus late genes
2 total, capsid proteins L1 and L2
E7
-activates cell cycle progression by binding Rb
-in an infected cell: E7 binds up Rb (a tumor-supressor protein), leaving E2F free and able to continue the cell cycle
-cancer-inducing strains have a really active E7 protein that can degrade Rb
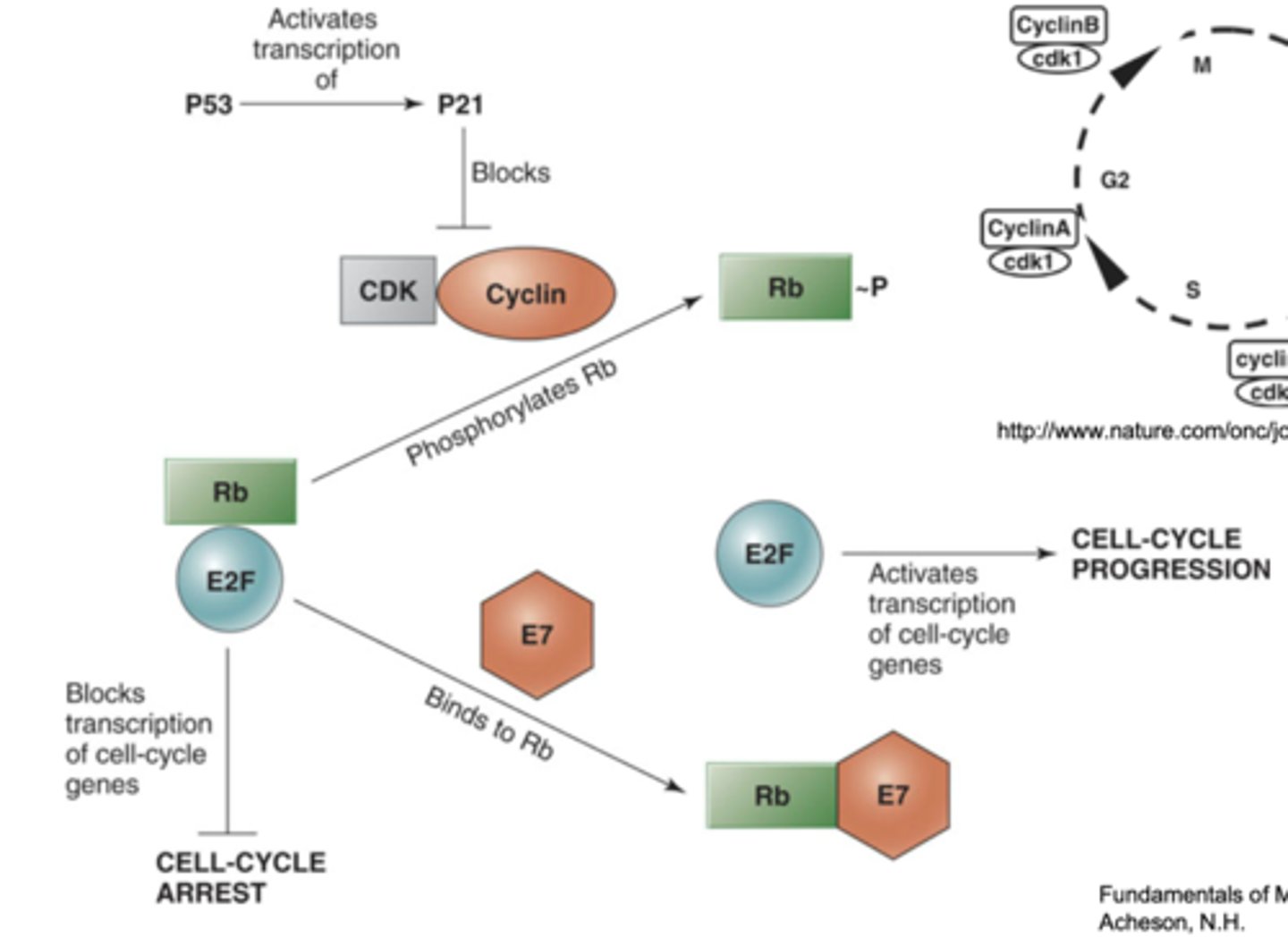
Rb
-a tumor supressor protein
-in a normal cell: Rb binds to E2F, preventing it from doing anything and causing arrest of the cell cycle
-if Rb is phosphorylated, it releases E2F and cell cycle can continue
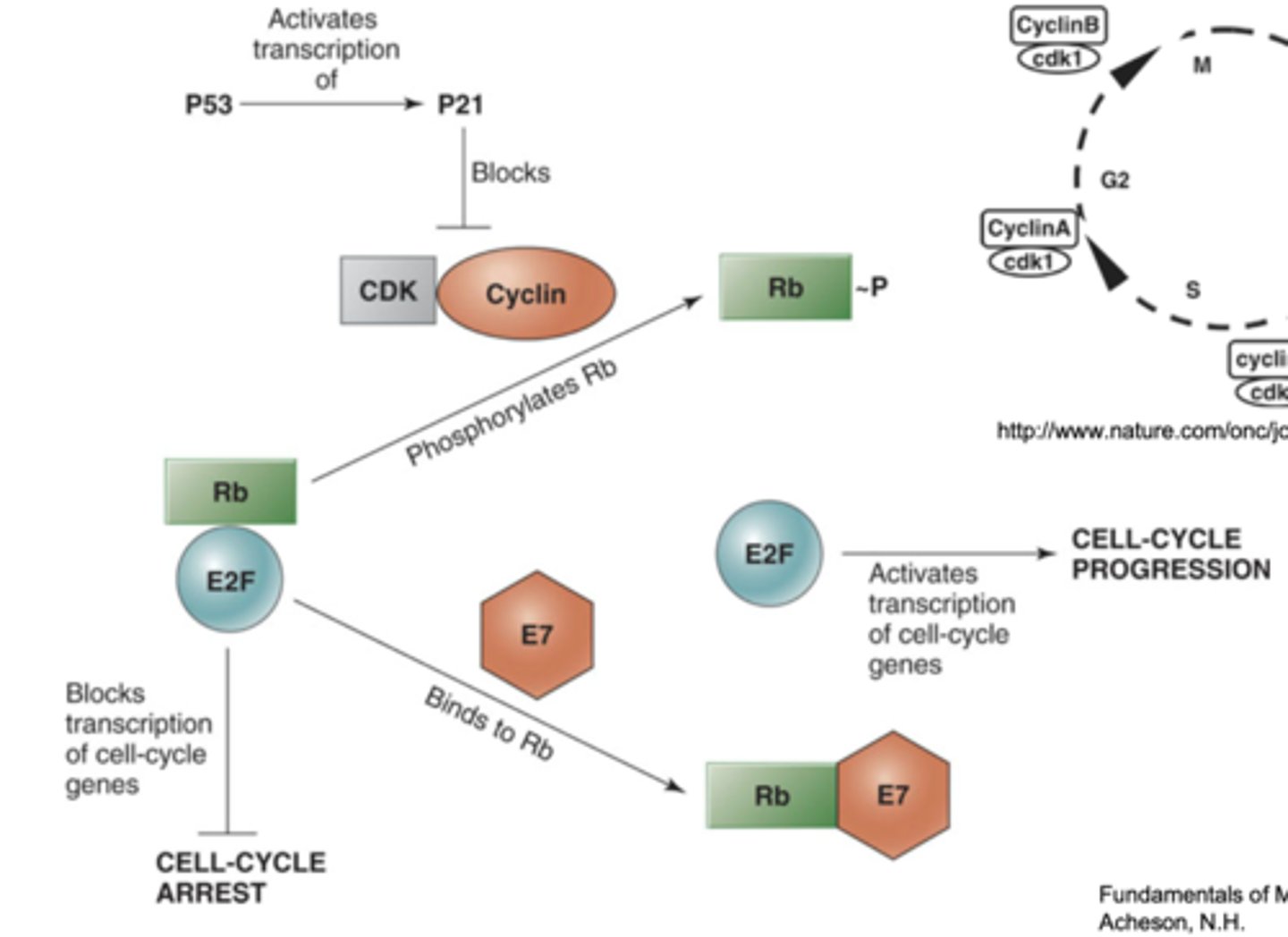
E2F
an important transcription factor, bound by Rb to stop the cell cycle
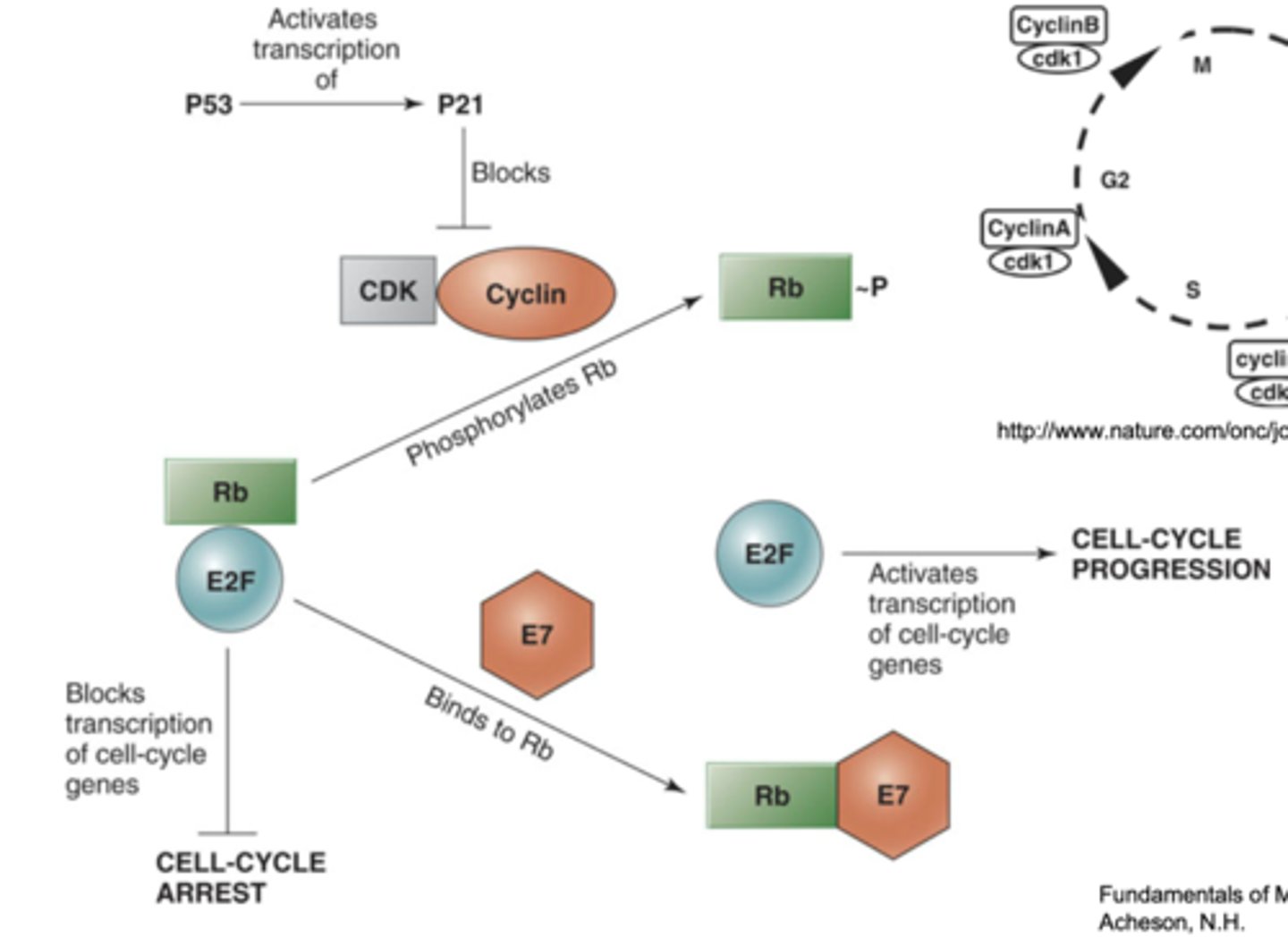
E6
-blocks apoptosis by inducing p53 degradation
-activated p53 induces apoptosis, so E6 (with cell protein E6AP) binds to p53 and degrades it
-E7 turns on cell cycle, but incidentally also activates P53, so E6 counteracts this
-cancer-inducing strains are very good at this process
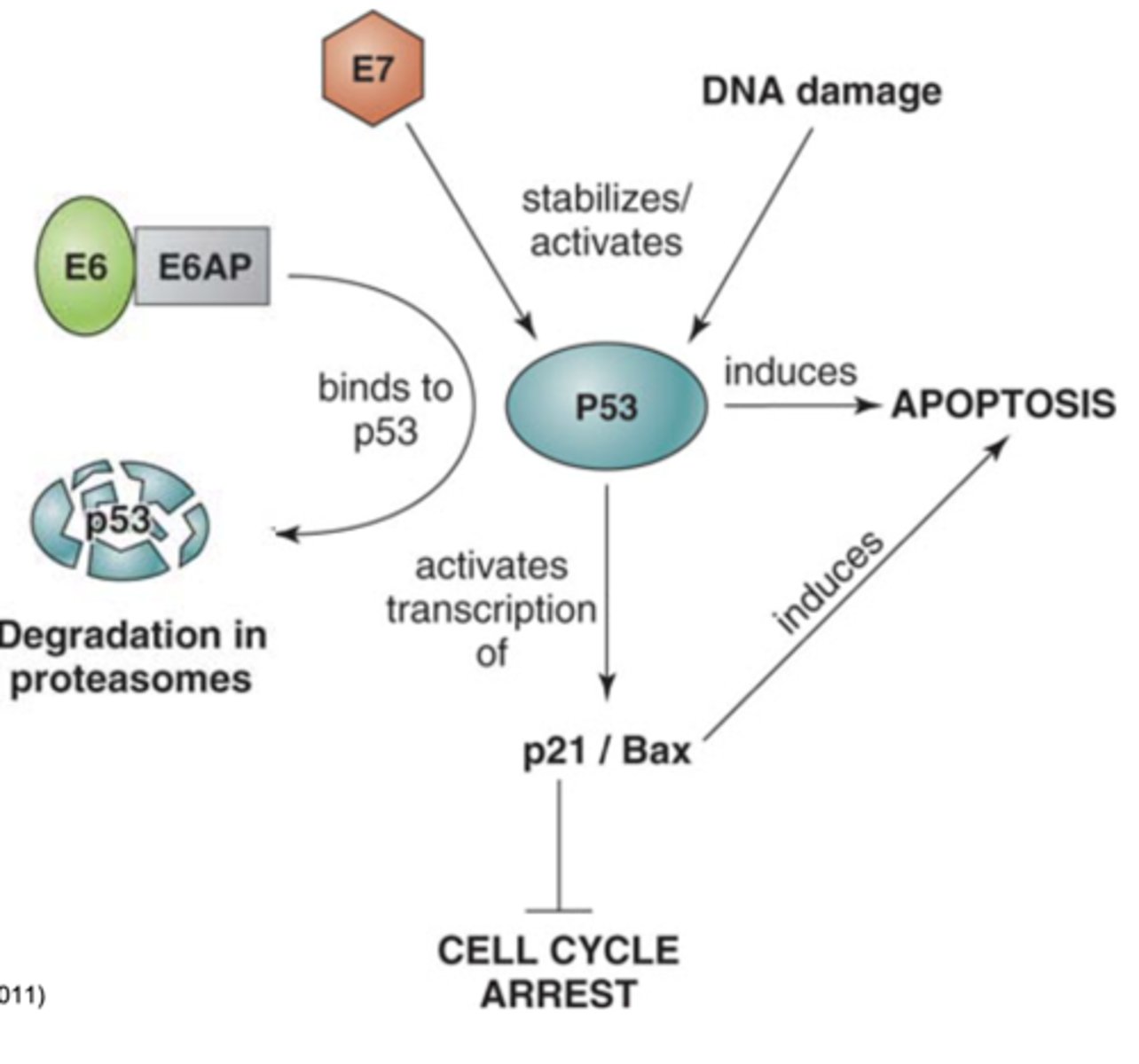
E7 + E6 = ______________________
oncogenesis
-block 2 key cell cycle checkpoint proteins, resulting in uncontrolled proliferation and loss of the ability of the cell to kill itself
-this is normal for HPV replication, as it must "transform" the cell to replicate
T/F: Most people who become infected with HPV will get cancer.
False - most people clear the virus over time
1 multiple choice option
Pathogenesis of warts
hyperkeratosis (buildup/replication of cells)
Pathogenesis of cervical cancer
-transformation to cancer happens between 10-15 years after initial acquisition of HPV
-progresses from benign cervical lesions to invasive cancer, triggered by viral DNA integration into host cells, followed by production of high levels of E6 and E7
How does HPV genome integration lead to increased levels of E6 and E7?
-During genome integration, the circular DNA is often broken at the E2 gene, and most of it is deleted during insertion
-E2 regulates E6 and E7
-So with E2 gone, E6 and E7 expression increase and cell growth can go out of control ---> malignancy
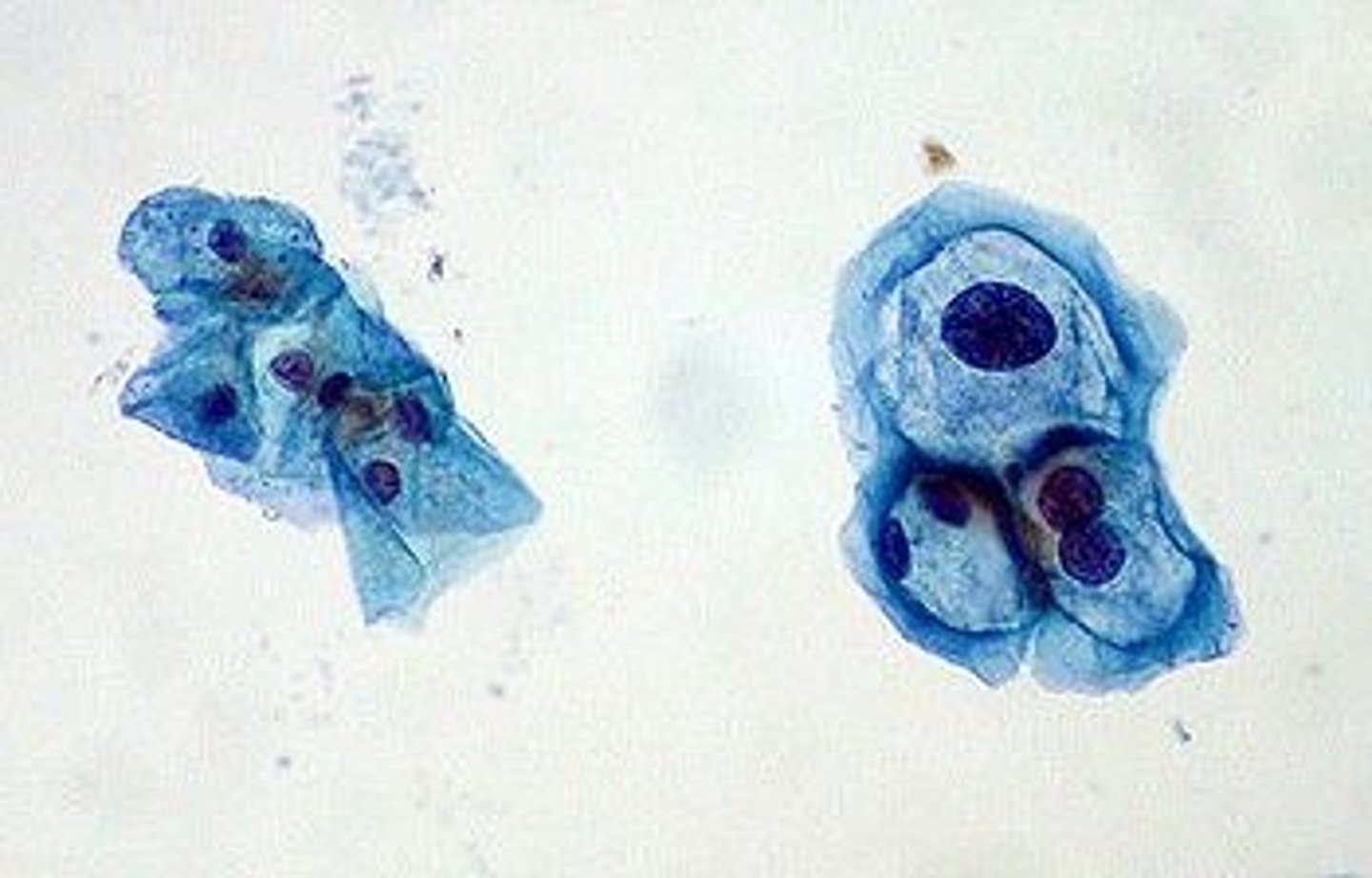
Dysplastic cervical epithelium
PAP smears can detect dysplastic changes to the epithelium, that way you can be treated early before the growth becomes cancerous
Squamous cell carcinoma
cells grow out and inward, leading to invasion
Diagnosis of HPV
-Pap smear (pathology, cytology)
-immunochemistry, serology
-nucleic acid (PCR, hybridization; can identify specific strain to help evaluate prognosis and treatment)
Koilocytes
cells with empty open-looking cytoplasm seen on a Pap smear, always precede cancer
Where is the global burden of cervical cancer the greatest?
developing countries, where Pap smears are not performed
Prevention of HPV
vaccines like Gardasil and Cervarix (recombinant virus-like particle vaccines made with the L1 capsid protein)
Therapeutic options for HPV treatment
freezing, electro-diathermy, cone biopsy