NURS271 - Liver Problems
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
cirrhosis of the liver
- severe medical condition where scar tissue in the liver replaces functional tissue.
- widespread destruction of hepatocells
major causes of cirrhosis
- chronic alcoholism and hepatitis C in the UA
- Hep B and Hep D in other countries
pathophysiology of cirrhosis
- fibrotic bands (scar tissue) of connective tissue change normal liver composition
- hepatic inflammation d/t toxins from destroyed cells
- destruction of hepatocells (liver cells)
- nodular tissue → block bowel ducts → block blood flow
liver function tests
- increased AST (aspartate transaminase)
- increased ALT (alanine transaminase)
- increased alkaline phosphatase
- increased total bilirubin (RBC breakdown byproduct)
> high levels indicated rapid breakdown or liver isn't able to cleanse bilibrun from body properly
> s/sx: yellow eyes and skin
- decreased albumin
> largest protein in body which maintain oncotic pressure
> indicates chronic liver disease
oncotic pressure
The pressure of water to move, typically into the capillary, as the result of the presence of plasma proteins.
relationship between albumin and oncotic pressure
- albumin maintains oncotic pressure
- decreased albumin → decreased oncotic pressure
> allows for leakage of intravascular fluid into the peritoneal cavity → ascites → abdomen swells and puts pressure on diaphragm
>> pt must sit in high fowler's to breath
s/sx of liver cirrhosis
- usually none
- hepatomegaly
> liver is palpable, hard, and enlarged
> present only at the beginning of CLD
- liver shrinks as disease develops and function decreases
types of liver cirrhosis
- laennec's or alcoholic cirrhosis (most common type)
- post necrotic cirrhosis (rare)
> caused by viral hepatitis and certain hepatotoxic drugs/abx such as tylenol, monitor liver function
- biliary cirrhosis (rare)
> caused by chronic biliary bowel obstruction
- cardiac cirrhosis (rare)
> caused by heart failure
complications of cirrhosis
- portal hypertension
- bleeding esophageal varices
- jaundice
portal hypertension
- degeneration of liver tissue and cirrhosis
- fluids back up into spleen
- resistance increases causing splenomegaly
- pressure in portal vein increased
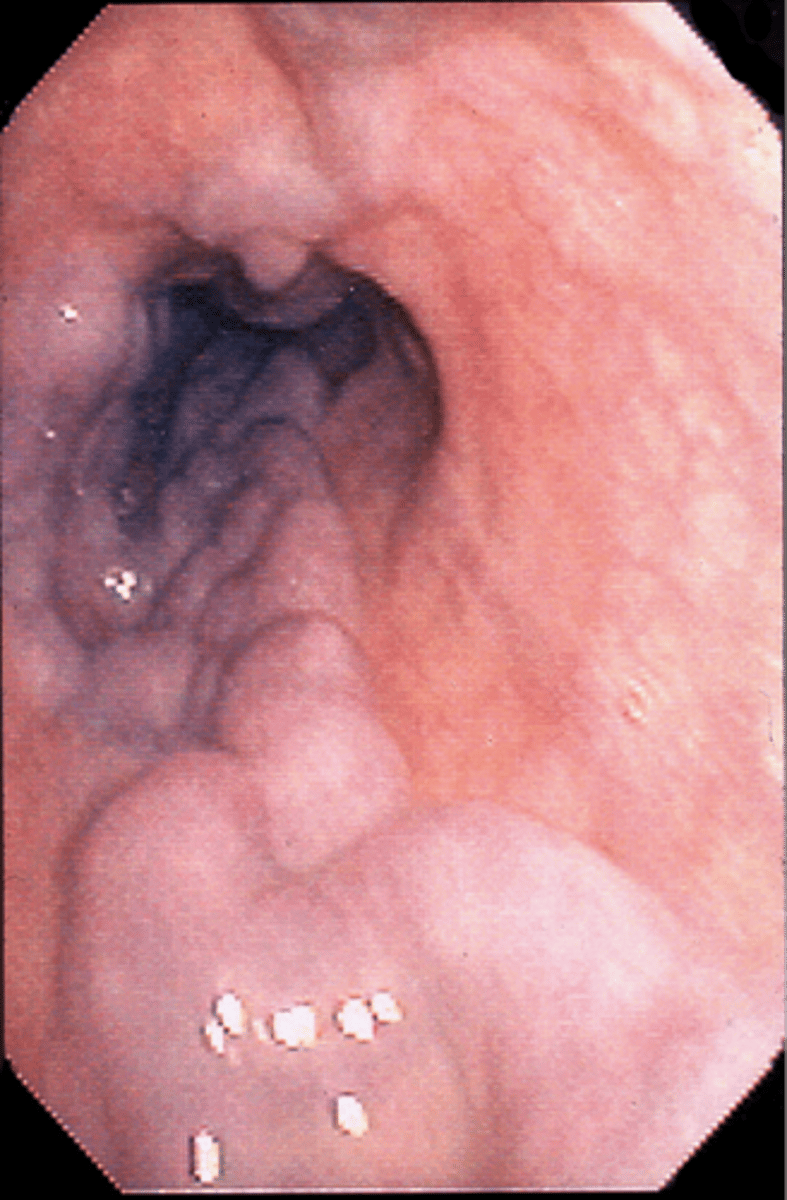
bleeding esophageal varices
- involves ruptures and bleeding of enlarged veins in the esophagus, causing significant blood loss and potential complications like shock and death.
- causes decreased bile → decreased absorption of fat-soluble vitamins (A, D, E, K) → decreased vit K = decreased clot factor production (2, 7, 9, 10) → increased bleeding risk d/t inability to clot
- also happens in the stomach (gastric) and rectum (hemorrhoids)
jaundice
- yellowing of the skin and eyes caused by an accumulation of bile pigment (bilirubin) in the blood
- complication of cirrhosis of the liver
- two mechanisms: hepatocellular disease or intrahepatic obstruction

hepatocellular disease
- classification of liver disease where hepatocytes are the primary problem
- the liver is unable to excrete excess bilirubin circulating in blood which then causes jaundice
intrahepatic obstruction
- alterations in hepatocyte function and obstruction of bile canaliculi d/t edema, fibrosis, or scarring of hepatic bowel channels
- bile and bilirubin build up which causes jaundice
ascites
- collection of fluid in the peritoneal cavity caused by:
> decreased circulating plasma protein
> decreased album production (holds fluid in the vessels, decrease causes shift)
> decreased colloid osmotic pressure (maintains fluid between blood vessels and intravascular spaces)
> fluid shift from the vascular system to the abdomen
- results in a form of 3rd spacing

s/sx of esophageal varices
- hematemesis: vomiting blood confirms pt is bleeding
- melena: black tarry stools
> 30% of pts will hemorrhage w/in 2 years of diagnosis
> mortality rate of 50% for those that hemorrahe
- LIFE THREATENING MEDICAL EMERGENCY
- affects 50% of pts w/ cirrhosis
tx for esophageal varices
- fluid resuscitation w/ NS (isotonic, crystalloid) remains in extracellular spaces and increases BP
- blood transfusions
- platelets if pt has decreased clotting ability
> NR 150k-450k, <150k = thrombocytopenia, admin plts
- fresh frozen plasma
- vasopressin (pitressin) to control bleeding
> affects posterior pituitary gland by mimicking ADH which constricts the blood vessels to help stop bleeding
- beta blockers: propranolol (inderal), nadolol (corgard)
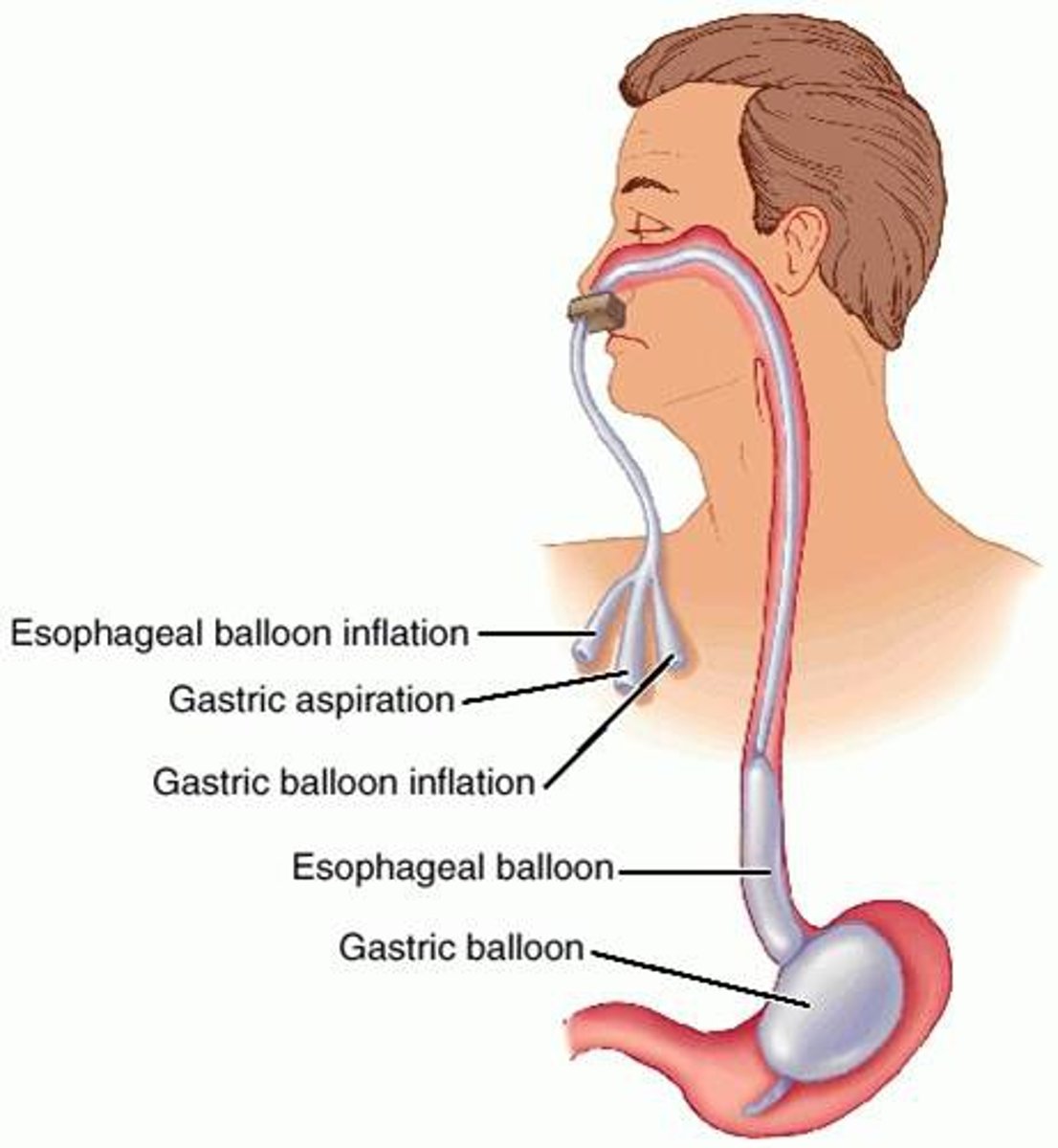
- sengstaken-blakemore tube
> mechanical ventilation if pt is placed on tube
sengstaken-blakemore tube
- three-lumen tube used to hold pressure on the bleeding esophageal varices
- obstructs breathing so pt must be placed on mechanical ventilation
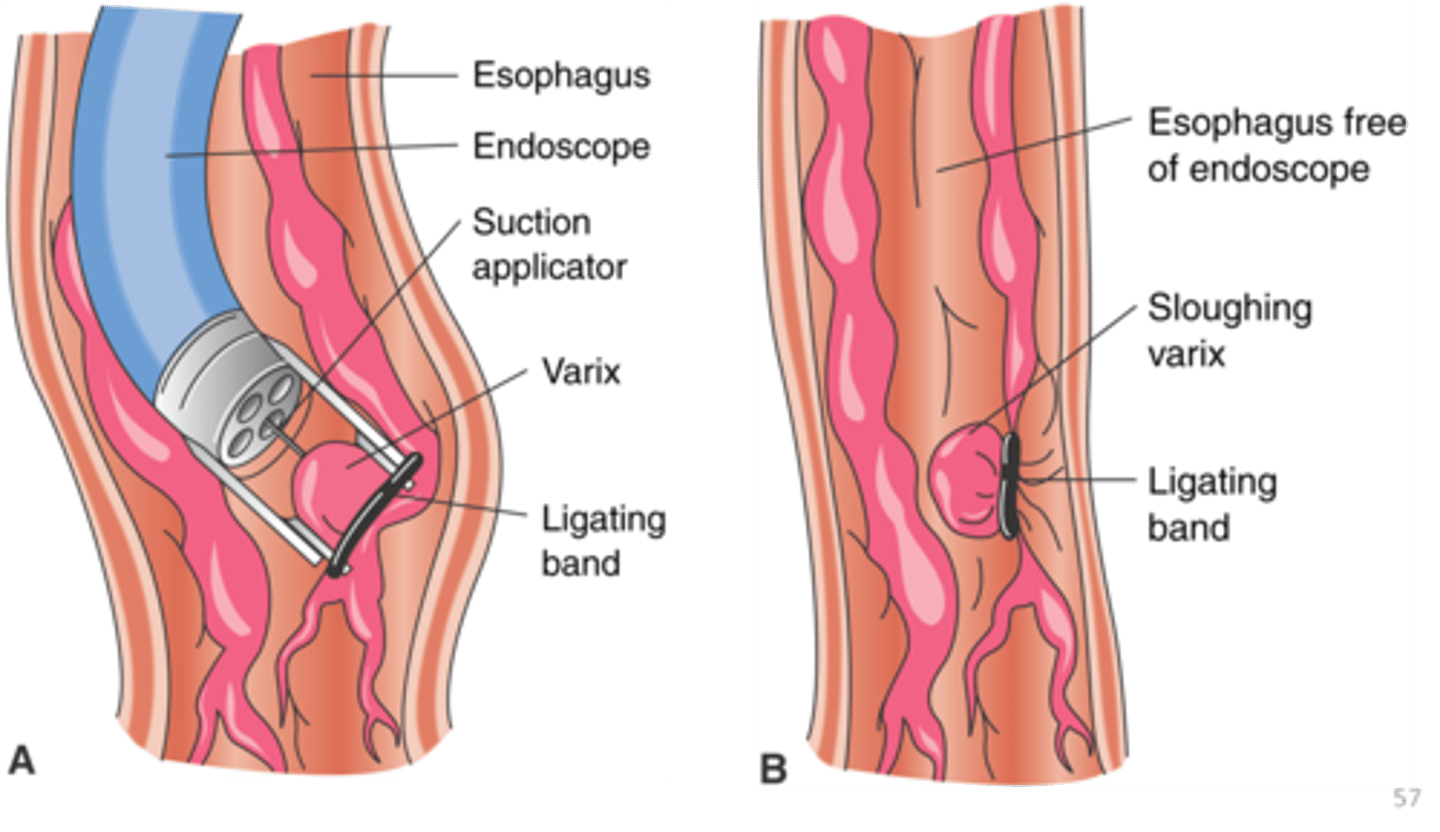
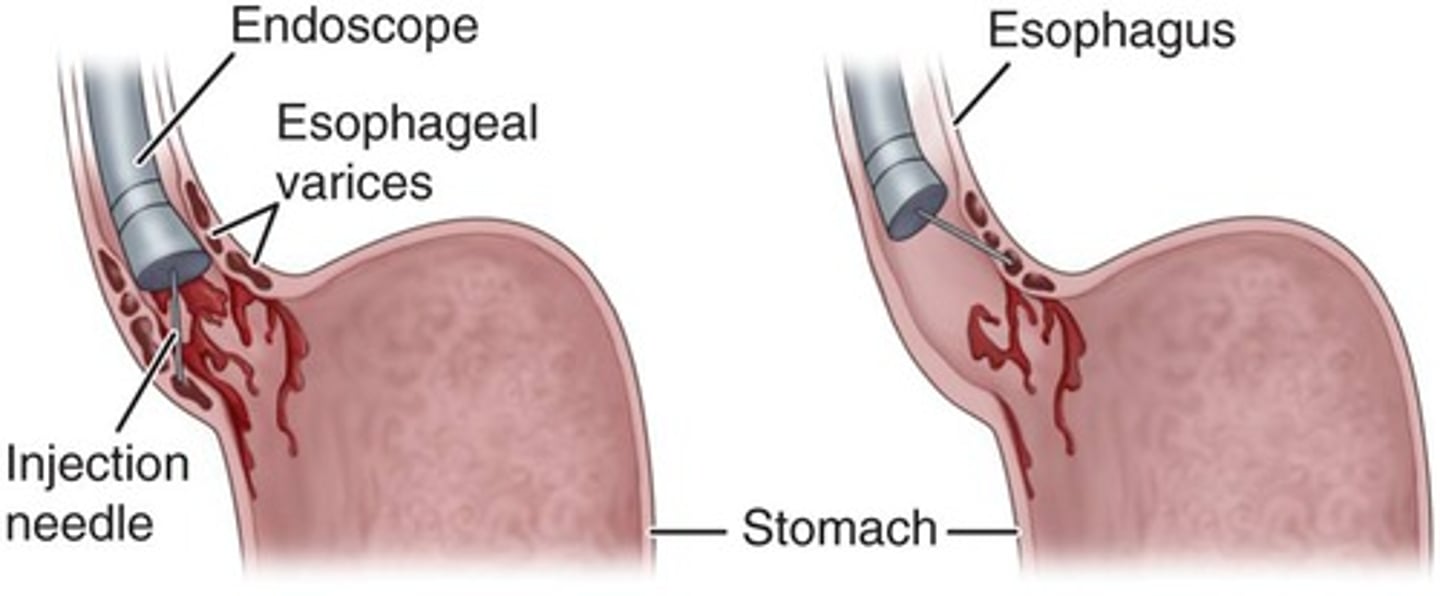
endoscopic procedures for bleeding varices
- endoscopic variceal ligation (EVL)
- endoscopy sclerotherapy (EST)
endoscopic variceal ligation (EVL)
- bands placed on base of varices → decrease blood flow to varices → stops the bleeding
- pt does not notice bands
endoscopy sclerotherapy (EST)
- sclerosing agent injected
> agent that shrinks the blood vessels to stop bleeding
- may cause mucosal ulcerations which would increase bleeding
portal systemic encephalopathy
- complication of cirrhosis that causes cognitive and behavioral changes
- mechanism is unclear
- pt will have high levels of ammonia
> byproduct of protein → liver usually converts it to urea and it is excreted through the kidneys → diseased liver is unable to → ammonia reaches the brain and decreases brain function
- collaborate w/ dietician to decrease protein in diet to decrease ammonia levels (only limit, never completely prohibit protein intake)
nutritional therapy for portal systemic encephalopathy
- moderate intake of protein and fats
- collaborate with nutritionist
- include families in conversation
- cultural sensitivity!
tx for encephalopathy
- used sparingly in cirrhosis of the liver (pt diven lower doses) d/t decreased ability to breakdown drugs
- lactulose (lactitol)
> first choice laxative
- neomycin sulfate (mycifradin)
> broad spectrum abx
- metronidazole (flagyl)
> similar to neomycin sulfate but less damaging to the kidneys
lactulose (lactilol)
- first choice tx for encephalopathy
- laxative that decreases ammonia and rids the intestines of toxins
- may cause hyperkalemia and dehydration
- give cirrhosis pt lower dose
- never to be given with neomycin sulfate
neomycin sulfate (mycifradin)
- broad spectrum abx that can clear the GI tract
> increased diarrhea, decreased protein breakdown and ammonia production
- but it destroys normal GI flora → C. diff → increased diarrhea, decreased protein breakdown and ammonia production
- nephrotoxic, monitor BUN and creatinine
- give cirrhosis pt lower dose
- never to be given with lactulose
nursing management of cirrhosis
- assess for LOC
> pt may be confused, agitated, etc.
- check for asterixis aka liver flap
> tremors of the hands and feet
- check for hepaticus aka liver breath/the breath of death
> foul smelling breath CLD pts often have
- inform pt to stop drinking alcohol, recognize noncompliance
viral hepatitis
- cause: liver injury, liver toxic drug, or d/t secondary infection
- hepatitis A virus (HAV)
- hepatitis B virus (HBV)
- hepatitis C virus (HCV)
- hepatitis D virus (HDV)
- hepatitis E virus (HEV)
hepatitis A virus (HAV)
- transmission: fecal oral, oral anal, from sexual activity, and contaminated food/water
- incubation: 2-4 weeks
- may be asymptomatic
> other s/sx: GI upset, jaundice, decreased appetite, RUQ pain, low grade fever
- not life threatening but prevalent in 3rd world countries w/o sanitation requirements
- diagnosis done through serological testing
serological testing for HAV
- blood testing for the presence of 2 antibodies
> IgG antibodies indicate immunity to the virus d/t past infection or receiving the vax
> IgM antibodies indicate recent exposure or possible infection
hepatitis B virus (HBV)
- transmission: parenteral contact, infected blood and blood products, contaminated needles, unprotected sex, mother to child during birth
- incubation: 3-6 months
- s/sx: dark urine, fatigue, RUQ pain, usually asymptomatic
- virus usually cleared on its own and the pt gains immunity or they become a chronic carrier which leads to liver cirrhosis and liver cancer later in life
- prevalent worldwide
> ~300 million people have this as a chronic infection and can infect others even when they dont feel sick
> more than 1 million chronic cases in the US
hepatitis C virus (HCV)
- transmission: blood to blood, not casual contact. IV drug needle sharing, needle stick injury with contaminated blood, intranasal cocaine sharing
- unable to clear the body on its own → chronic carrier → cirrhosis of the liver → CLD → liver cancer
- liver transplant is optional tx but pharmacological tx must be done first to clear the body of the virus, or the new liver will be reinfected
pharmacological tx for HCV
- 1 of the following tx must be completed in full and the virus must be cleared from the body before liver transplant surgery is an option
- epclusa for 12 weeks, 95-98% cure tare
- harvoni for 12 weeks, 97-99% cure rate
- cost is expensive!
> $26k/month x 3 months = $78k
> generic version is $10k/month
> copay is $9600, insurance pays $300
hepatitis D virus (HDV)
- requires the presence of HBV to replicate, does not clear on its own
- transmission: blood and/or sex w/ infected person
- clinical course is more severe than the other viruses
> s/sx: clay colored stool d/t livers inability to excrete bilirubin and dark urine
- vax for B gives immunity to this virus
how to protect yourself from HDV
- safe sex practices
- screening blood products
- avoid IV drug abuse
- get vaccinated for HBV
hepatitis E virus (HEV)
- one of the most common causes of acute hepatitis but is very rare
- no vax available, goes away on its own
- transmission: fecal oral, waterborne
- prevalent in asia, africa, middle east, south america, and central america
> only found in international travelers in the US
how to protect yourself from HEV
- careful handwashing, hand sanitizer
- drink clean bottled water when traveling
- avoid street good when traveling
cancer of the liver
- usually caused by Hep virus or alcoholism
- early stage is w/o s/sx
- later s/sx: weight loss, anorexia, weakness, RUQ pain, jaundice, bleeding
later signs of liver cancer
- weight loss
- anorexia
- weakness
- RUQ pain
- jaundice
- bleeding
tx for liver cancer
- surgical intervention
> if cancer is in only one lobe of the liver, it can be removed (resectioning), increases lifespan up to 5 years
- transplantation
- radiation therapy is not an option
- chemotherapy, but it doesn't really work
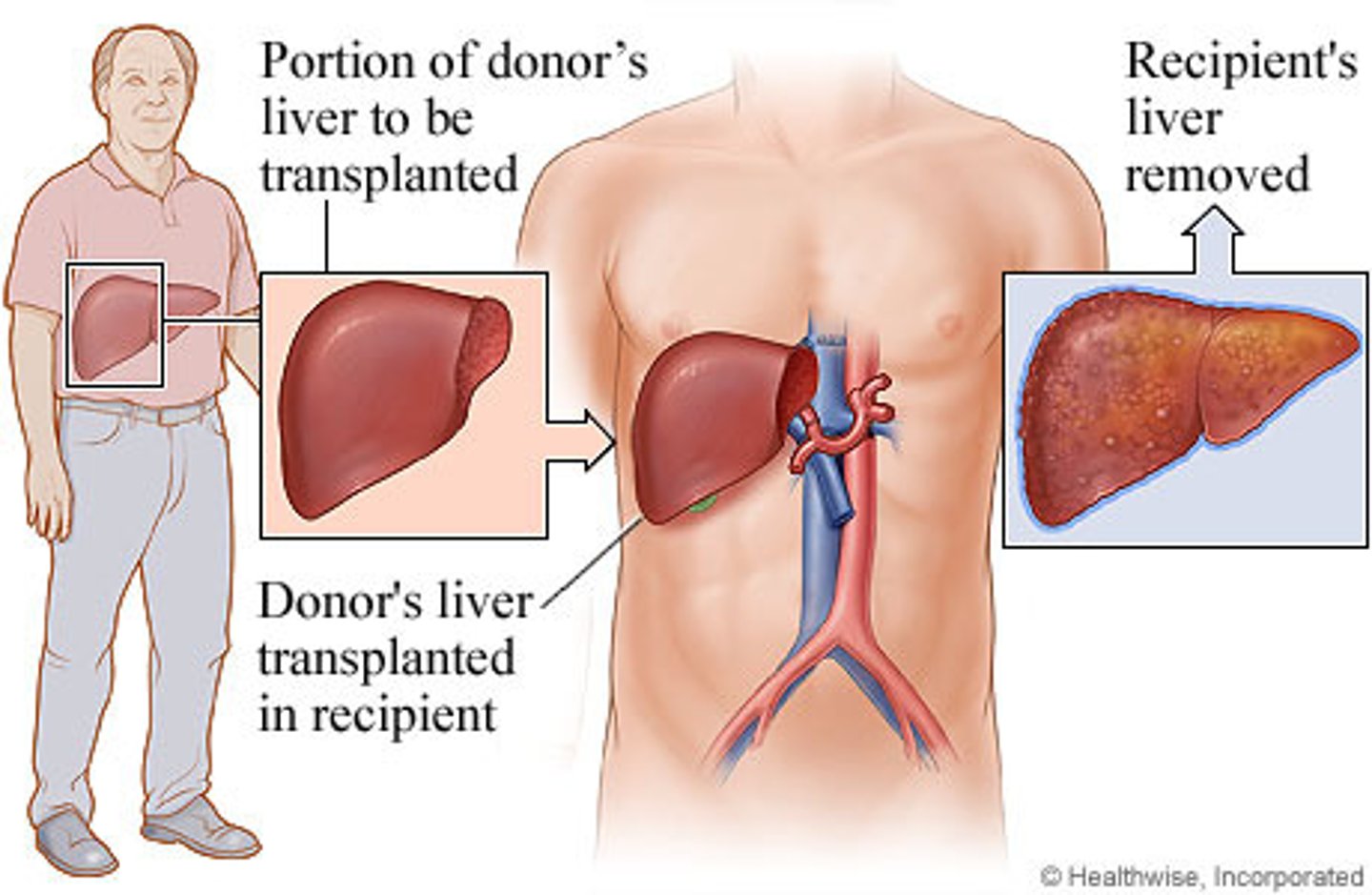
liver transplantation
- lobe of liver can be donated (only once in a lifetime)
- liver regenerates/grows back to full function for the receiver and donor
- best candidates: end stage liver disease or primary liver cancer
- pts not considered: active alcoholics, active substance abusers, those w/ metastatic tumors
post liver transplantation
- common complication → graft rejection and infection
- immunosuppressant therapy to prevent rejection
> cyclosporine and tacrolimus
> side effects: HTN and renal insufficiency
- high dose steroids
> prednisone
> side effects: HTN and hyperglycemia
>> insulin as needed
- vaccinations and abx
> COVID-19 vax before transplantation as well as a negative C-19 test
> abx should be administered postoperatively if infection develops
- pt usually feels great by day 4!