Immunology 20 | Antibodies
1/53
Earn XP
Description and Tags
Helpful Video(s): https://www.youtube.com/watch?v=oHA0l3EKT1o
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
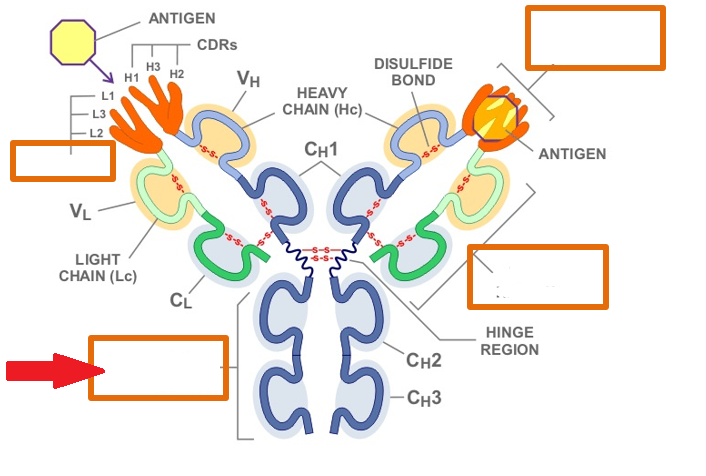
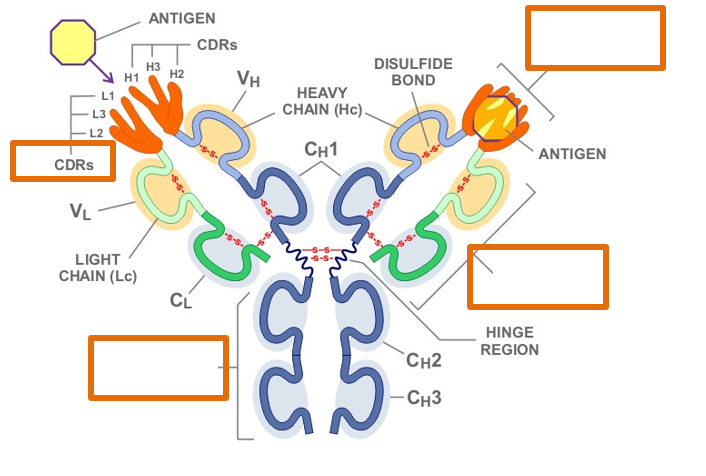
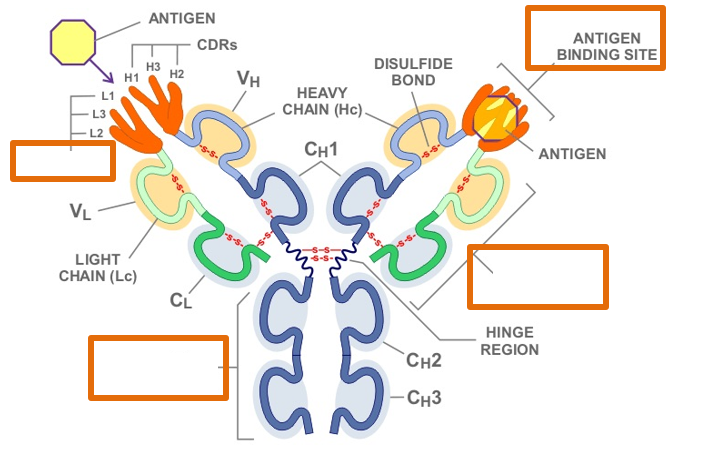
Which region of the antibody is highlighted by the red arrow?
Fc region
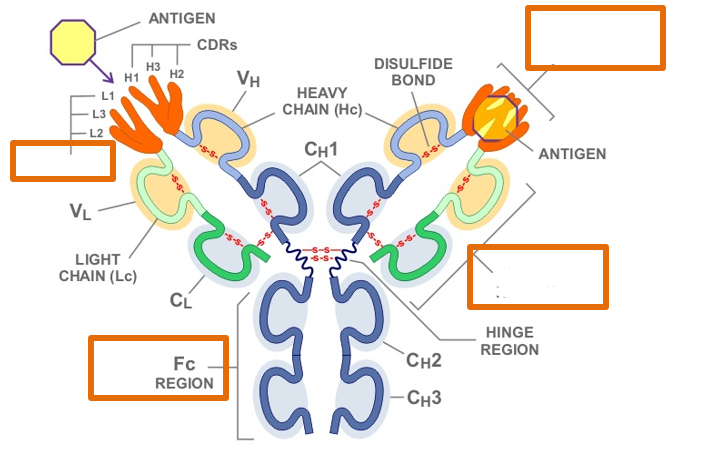
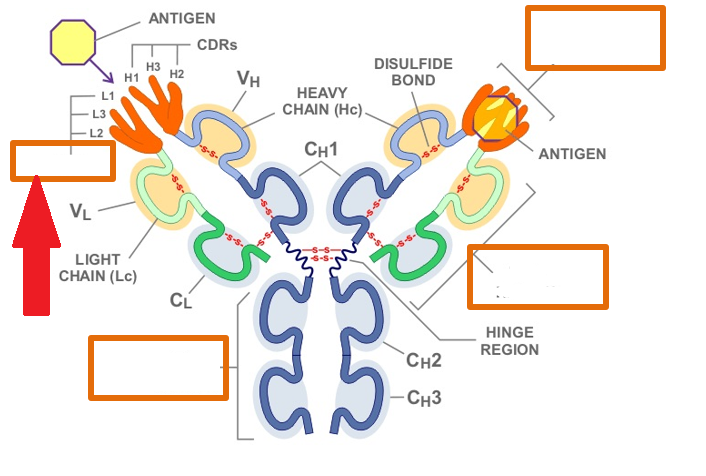
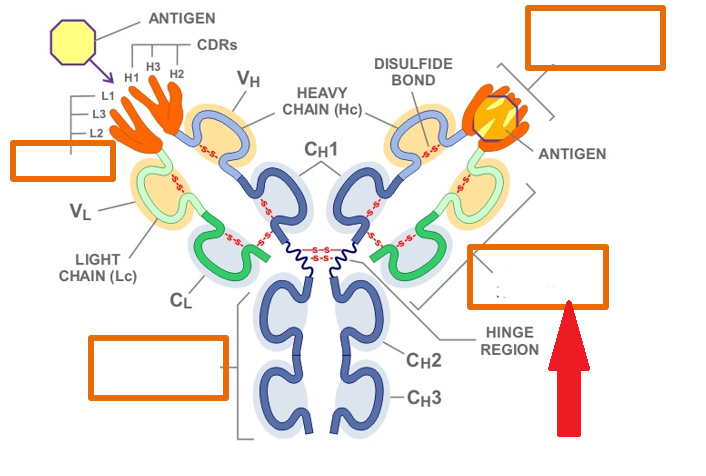
Which region of the antibody is highlighted by the red arrow?
Complementary Determining Regions
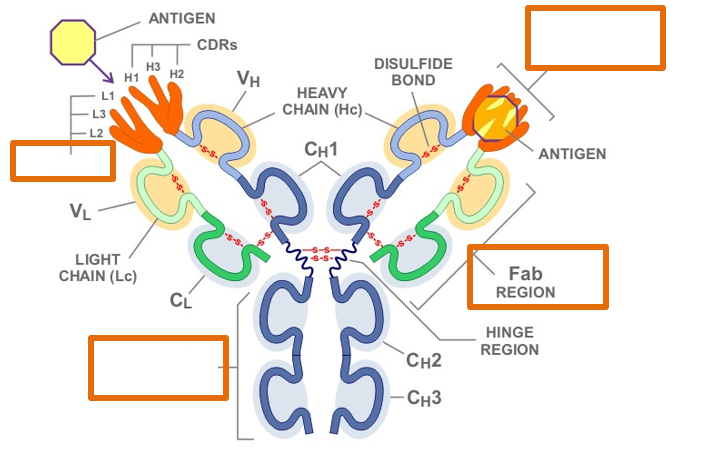
Which region of the antibody is highlighted by the red arrow?
Fab region
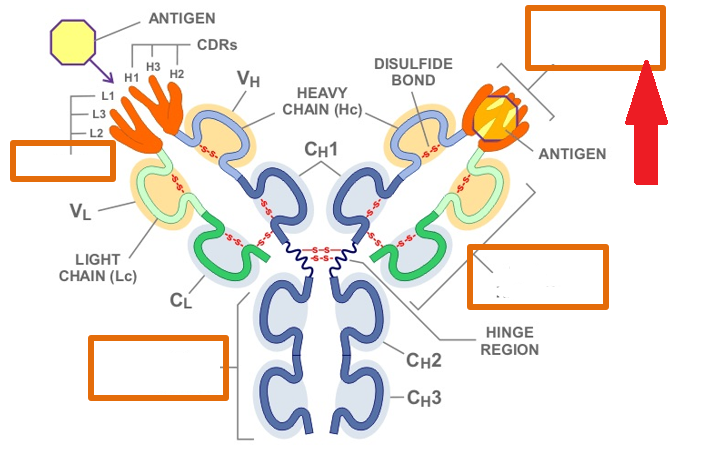
Which region of the antibody is highlighted by the red arrow?
Antigen Binding Site
What is valency?
the number of binding sites
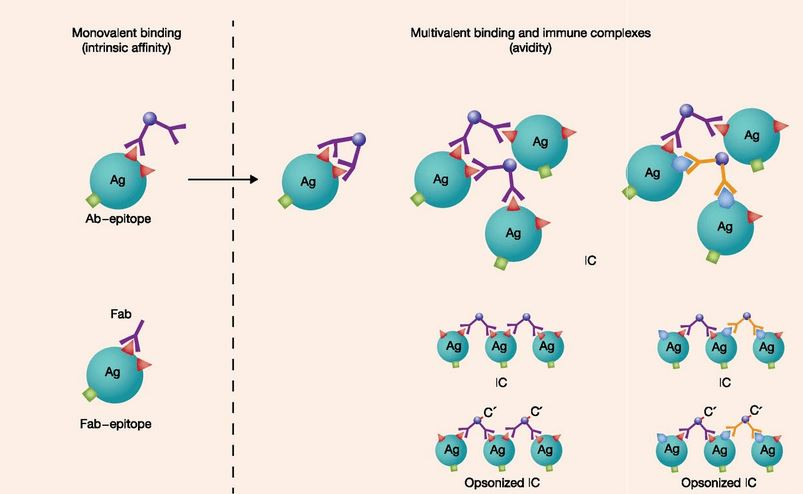
What is affinity?
The binding strength between a single antigenic determinant (epitope) and a single antibody binding site. It measures how strongly an antibody binds to one specific site on an antigen.
Note: not all antibody binding sites have equal affinity

What is avidity?
the overall binding strength between an antibody and a multivalent antigen, which has multiple binding sites (epitopes). It is the cumulative strength resulting from multiple individual antigen-antibody interactions.

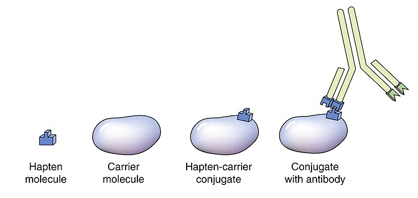
What are haptens?
Small molecules that, by themselves, are not capable of inducing an immune response because they are too small to be recognized by the immune system. However, when they attach to a larger carrier molecule, usually a protein, they form a complex that becomes immunogenic. This complex can then be recognized by antibodies and elicit an immune response. Video
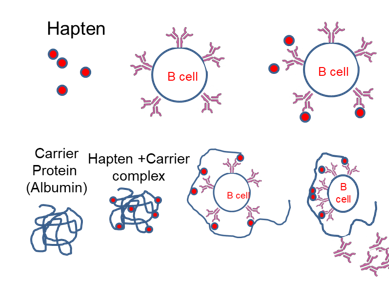
Are haptens able to initiate an immune response by themselves?
No
What must haptens be attached to to become immunogenic?
They must be attached to a large molecule often called the carrier and is typically a protein.
A substance that can be recognized by the immune system, typically provoking an immune response.
Antigen
An antigen that specifically induces an immune response
Immunogen
The specific part of an antigen that is recognized and bound by an antibody or receptor on immune cells.
Epitope (or Antigenic Determinant):
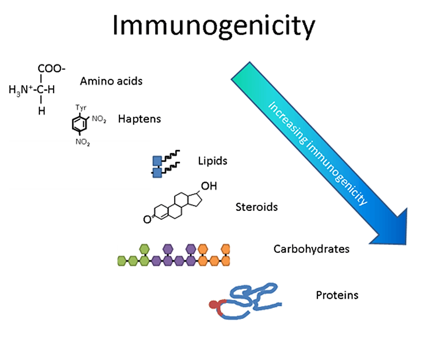
What is the general order of immunogenicity from most to least immunogenic?
Proteins, carbohydrate, lipid, haptens, amino acids, DNA
What are the characteristics that make a good antigen to induce a stronger signal in B cells?
Highly folded
Unevenly charged
Greater than 1kD in size (most are over 100kD)
What is cross reactivity or molecular mimicry?
When an antibody (Ab) is produced against a specific antigen (Ag), it is designed to bind to a particular epitope on that antigen. However, if a different antigen has a structurally similar epitope (enough resemblance in shape or chemical properties), the antibody might also bind to this different antigen.

What conditions are necessary for cross-reactivity to occur?
There must be enough similarity in the binding sites to generate sufficient affinity (binding strength) to activate a B cell. If the cross-reactive binding is strong enough, the immune system may mistakenly target the structurally similar antigen.
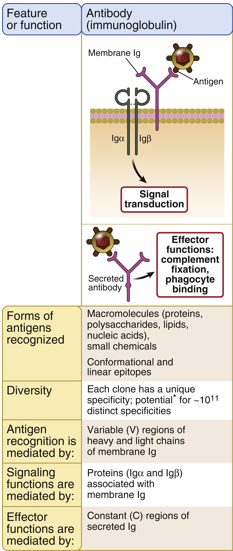
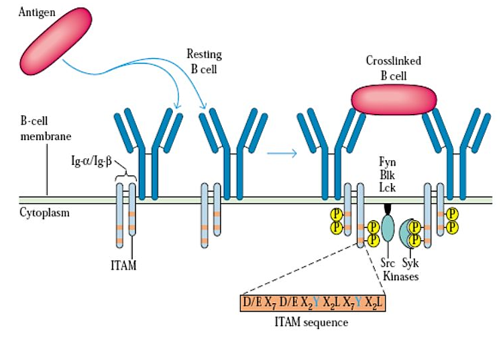
What are the roles of BCR accessory molecules Igα and Igβ in B cell activation?
They transmit activation signals due to the presence of an ITAM domain in their cytoplasmic tails and interact with the Fc portion of the BCR.
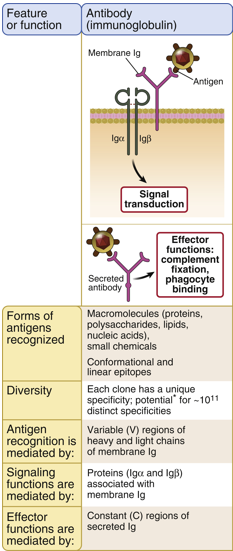
Why are Igα and Igβ necessary for B cell receptor (BCR) signaling?
The cytoplasmic tail of the BCR is too short to allow docking and assembly of signaling molecules needed to transmit B cell activation signals, so Igα and Igβ provide the necessary signaling capacity.
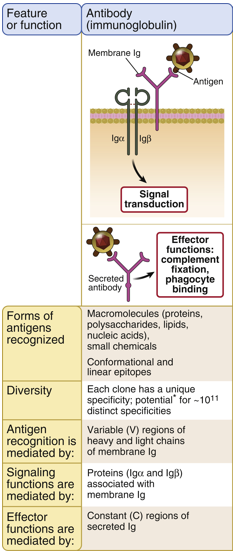
What is the significance of the ITAM domain in Igα and Igβ?
Allows these molecules to transmit activation signals for B cell activation.
What cell marker is found on all B cells?
CD19 is a marker found on the surface of B cells.
A 7-month-old boy presents with recurrent sinusitis and pharyngitis. The parents say that the child has had these symptoms multiple times in the past couple of months, and a throat swab sample reveals the presence of Streptococcus pneumoniae. Upon workup for immunodeficiency, it is noted that serum levels of immunoglobulins are extremely low, but T-cell levels are normal. Which of the following molecules is a marker on the cells that are lacking in this patient?
CD4
CD8
CD3
CD19
NKG2D
CD19
This patient likely has a type of B cell immunodeficiency, as indicated by the low levels of immunoglobulins and recurrent infections. The key detail here is that the patient has low immunoglobulin levels but normal T cell levels. This points to an issue with B cells rather than T cells.
What are the major differences between B cells and T cells regarding receptor editing and maturity?
B cells undergo receptor editing in the bone marrow to modify self-reactive receptors, allowing them multiple chances to produce a functional B-cell receptor (BCR) and optimize its function through affinity maturation and isotype switching. B cells are not fully mature when they leave the bone marrow and require further selection in peripheral lymphoid organs.
T cells do not undergo receptor editing; instead, they rely on thymic selection to ensure their T-cell receptors are functional and non-self-reactive. T cells do not experience affinity maturation or isotype switching but differentiate into various subsets based on cytokine signals.
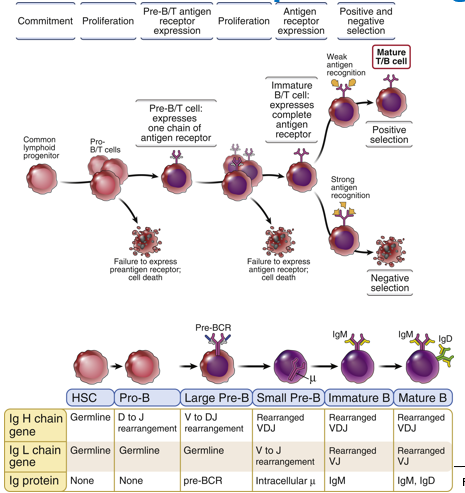
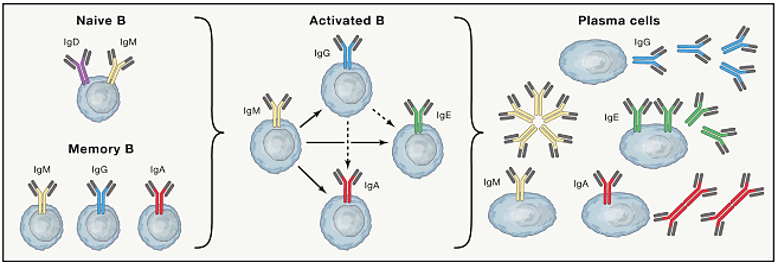
What three things occur when a B cell undergoes maturation in the periphery?
Clonal expansion (next hour)
Affinity maturation
Isotype switching
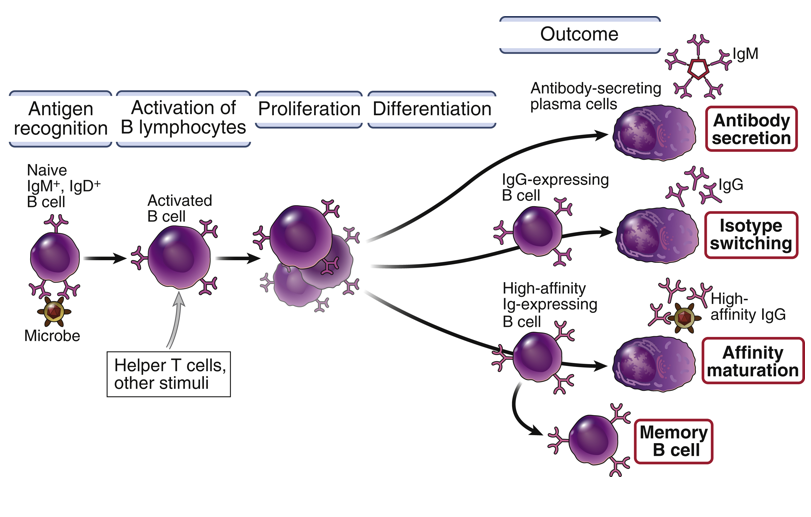
What triggers clonal expansion of B cells, and how does this process contribute to the immune response?
Clonal expansion is triggered when a B cell encounters its specific antigen and receives the necessary signals from helper T cells. This process involves the rapid division of the B cell to produce many identical clones, all with the same antigen specificity. This increases the number of B cells capable of producing antibodies against the pathogen, thereby enhancing the immune response
How does affinity maturation improve antibody effectiveness, and where does this process occur?
Affinity maturation improves antibody effectiveness by introducing mutations in the B-cell receptor genes through a process called somatic hypermutation. The result is antibodies with stronger binding to the antigen, leading to more efficient neutralization and clearance of the pathogen.
What is the significance of isotype switching in the immune response, and how does it differ from the initial antibody type produced?
Isotype switching allows B cells to change the class of antibody they produce (e.g., from IgM to IgG, IgA, or IgE) while maintaining the same antigen specificity. This is important because different antibody classes have distinct functions; for example, IgG is effective in opsonization and neutralizing toxins, while IgA is important for mucosal immunity. Isotype switching tailors the antibody response to better suit the needs of different stages of infection or types of pathogens.
What happens to B cells that acquire mutations that decrease their affinity for the antigen?
They do not receive survival signals. As a result, they lose the competition for binding and undergo apoptosis due to neglect, thereby being eliminated from the immune response.
Does affinity maturation change the antigen specificity of the antibody?
No, affinity maturation does not change the antigen specificity of the antibody. It only improves the binding affinity for the same antigen, making the antibody more effective at recognizing and binding to that specific antigen.
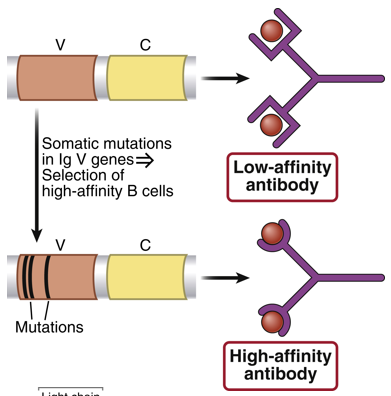
Why is affinity maturation important for the immune response over time and with repeated exposures to an antigen?
It ensures that with each exposure to the antigen, the antibodies produced have higher affinity and are more effective at neutralizing the pathogen. This optimization over time enhances the efficiency and effectiveness of the immune response, leading to better pathogen clearance.
What is the role of the IgM isotype?
Complement activation (C’), which is crucial for the initial stages of the immune response.
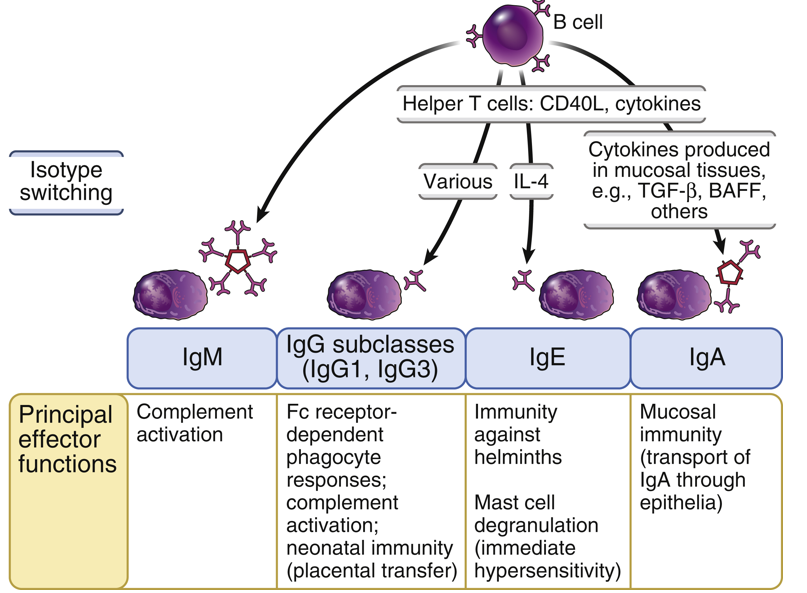
What is the role of the IgG1, IgG2, IgG3, IgG4 isotype?
Opsonization (coating pathogens to enhance phagocytosis) and complement activation, each engaging different pathways and having different levels of effectiveness.
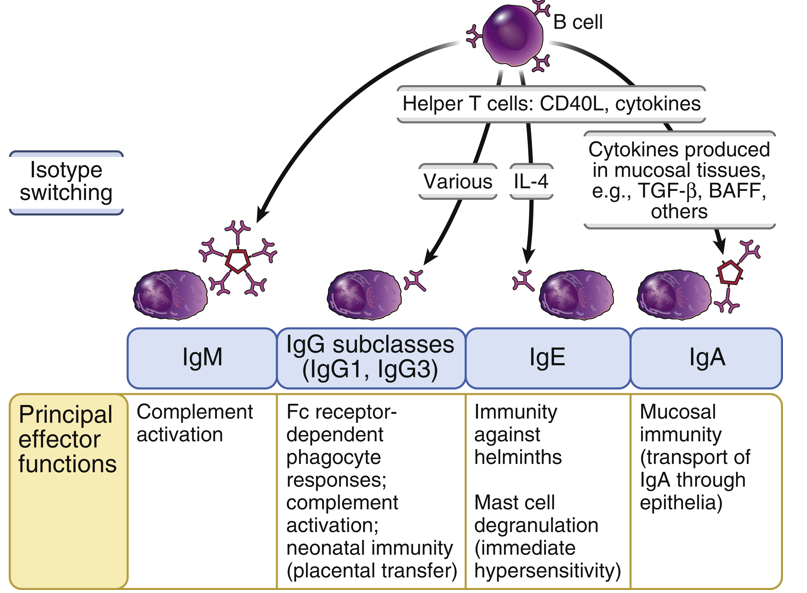
What is the role of the IgA1 and IgA2 isotype?
Mucosal immune responses, providing protection in mucosal areas like the gastrointestinal and respiratory tracts. They have limited differences between their subtypes (IgA1 vs. IgA2).
What is the role of the IgE isotype?
Associated with mast cell responses and plays a critical role in allergic reactions and defense against parasitic infections.
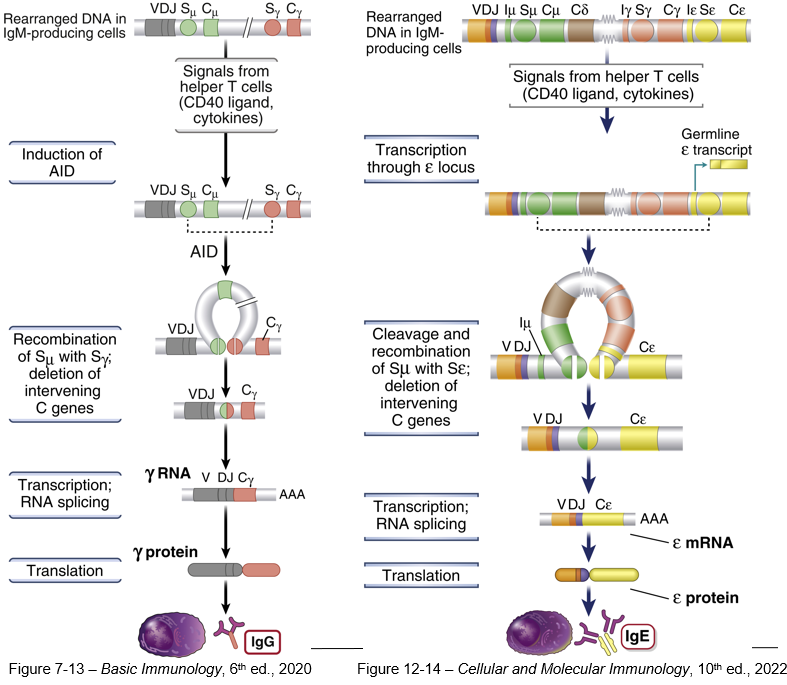
What is Activation-induced Cytidine Deaminase?
An enzyme that plays a important role in the adaptive immune response by facilitating two key processes in B cells: isotype class switching and somatic hypermutation.
Why do B cells initially produce IgM antibodies upon activation?
Because IgM is the default antibody isotype produced by naïve B cells before any class switching occurs. IgM is effective for early immune responses because it is a pentamer, providing strong antigen binding and effective activation of the complement system, which helps to clear pathogens.
What role do CD4+ T helper (Th) cells play in the class-switching process of B cells?
CD4+ T helper cells provide essential co-stimulation signals and secrete cytokines that are necessary for initiating the class-switching process in B cells. These signals activate the B cells to produce Activation-Induced Cytidine Deaminase (AID), which is required for the DNA recombination that allows switching from IgM to other antibody isotypes.
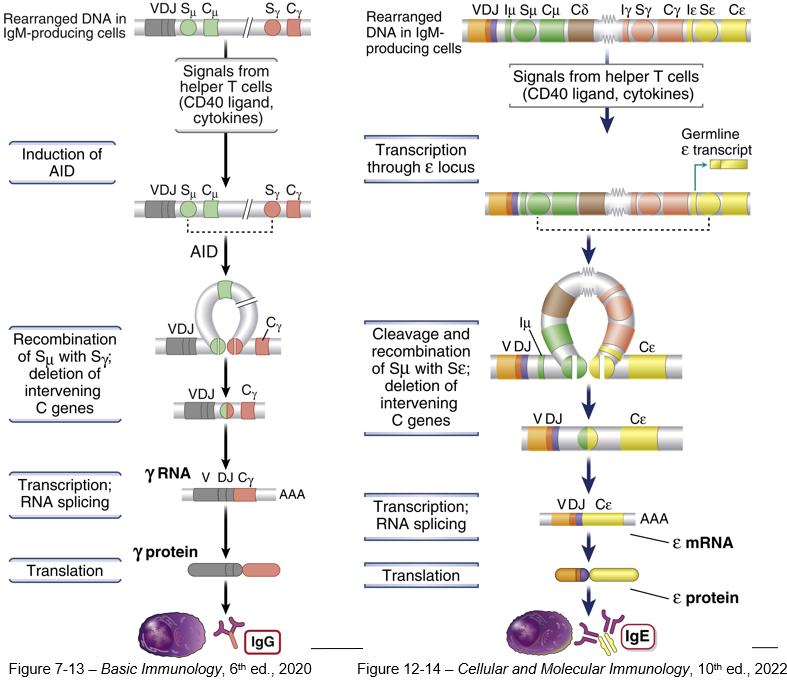
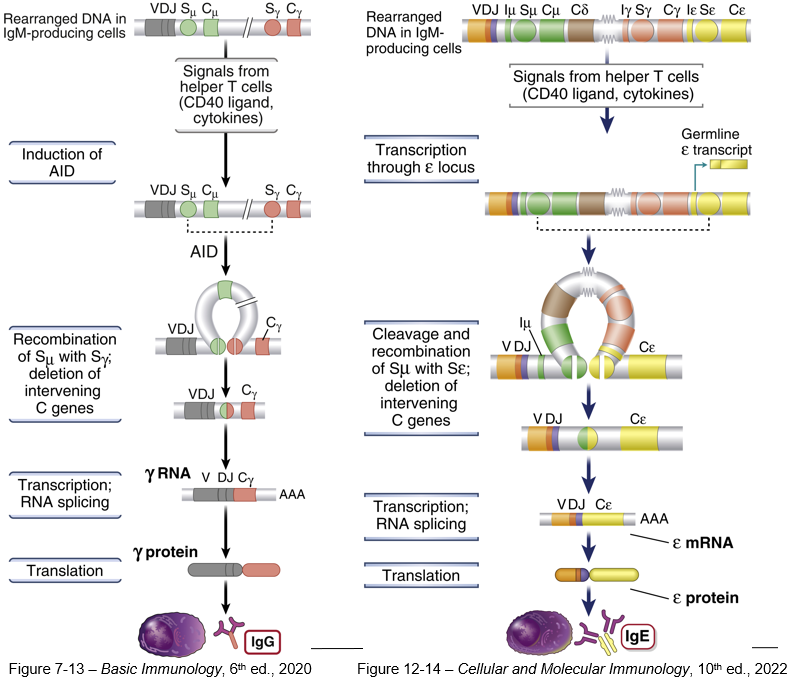
How does Activation-Induced Cytidine Deaminase (AID) contribute to isotype switching in B cells?
By deaminating cytidine bases in the DNA at specific "switch" (S) regions of the immunoglobulin heavy chain locus. This deamination leads to DNA breaks that facilitate recombination of the VDJ gene segment with a new constant region gene segment, thereby changing the antibody isotype without altering its antigen specificity.
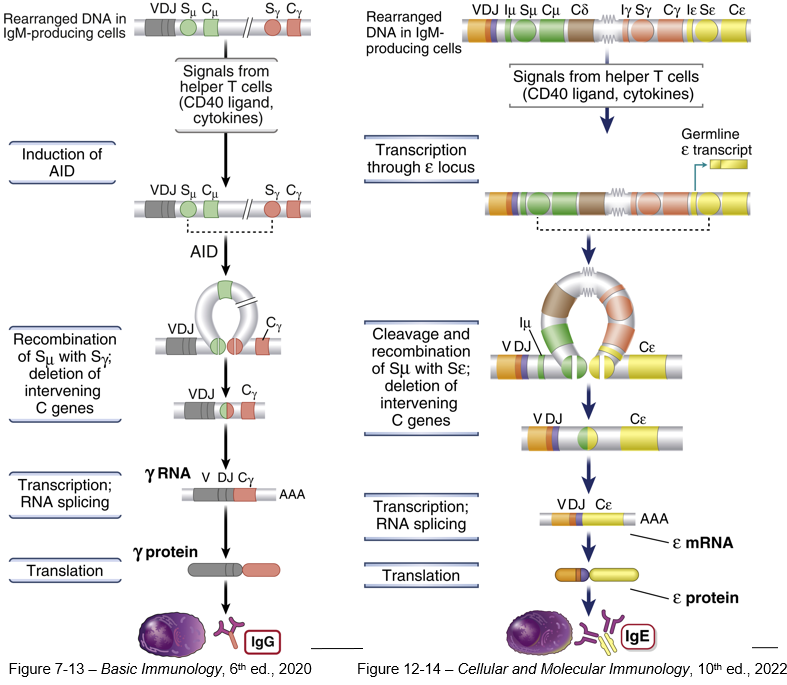
What happens to the intervening DNA during the class-switching process, and why is this process irreversible?
During class switching, the intervening DNA between the VDJ segment and the new constant region gene is looped out and excised. This DNA, which contains the constant region genes not being used, is permanently removed from the B cell's genome. Because the excised DNA cannot be restored, the process is irreversible, and the B cell cannot revert to producing the original IgM or other lost isotypes.
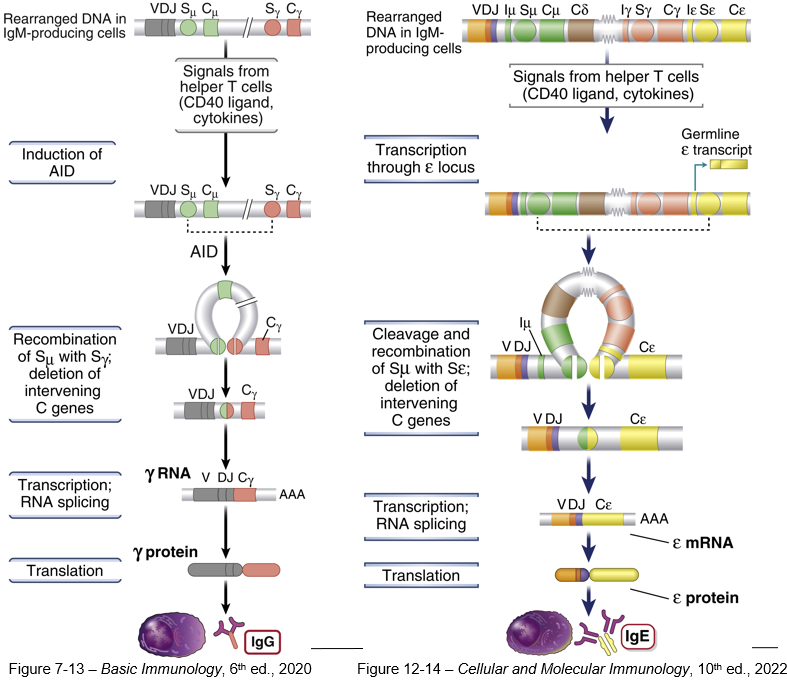
What is the outcome of the class-switching process for the antibody produced by a B cell?
The production of a new antibody isotype (e.g., IgG, IgA, or IgE) that retains the same antigen specificity as the original IgM but possesses different functional properties.
Isotype switching results in antibodies that have the same antigen-binding domain (Fab) but different ______ ?
constant (Fc) regions
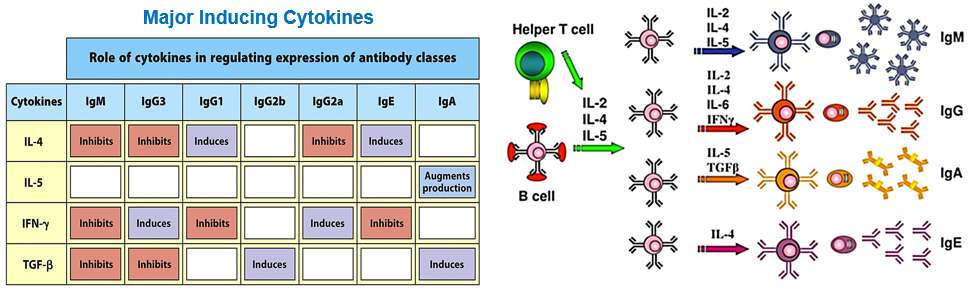
What determines the isotype to which a B cell switches?
The cytokine environment
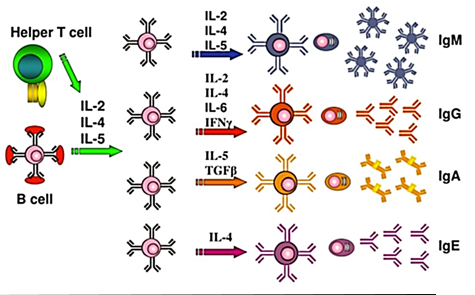
Similar to CD4 Th cells, B cells have a 3-signal activation process, which is the third (last) signal
Cytokine-induced signaling then turns on signals to activate or inhibit particular isotype switching
What are the structural forms of antibodies?
Antibodies can exist as monomers (single Ig molecules) or multimers (multiple Ig molecules joined together).
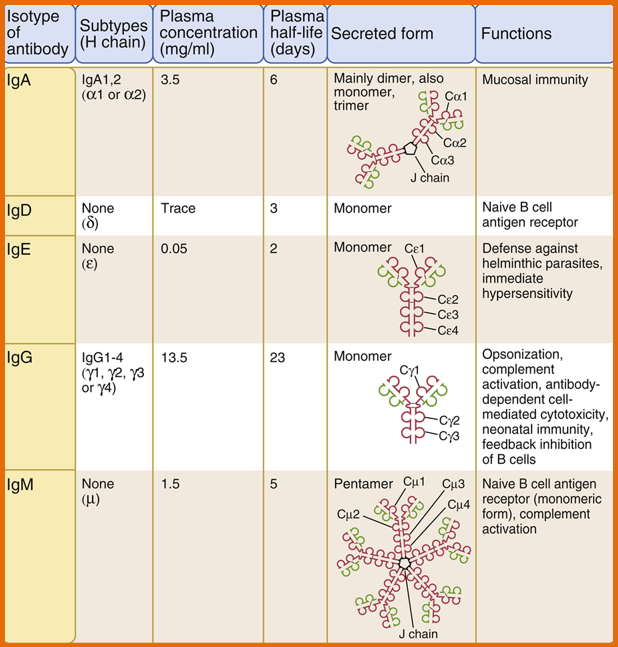
Which antibody isotypes are typically found as monomers in the blood?
IgG, IgE, IgA, and IgD.
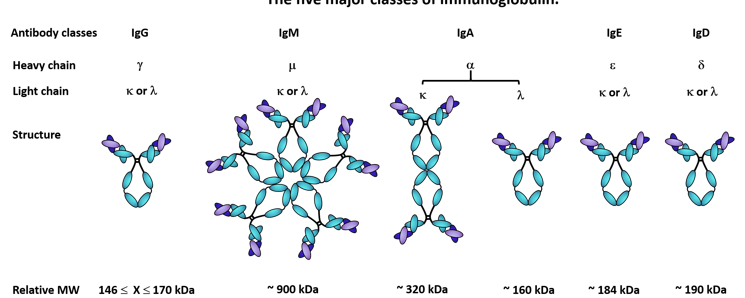
What is the significance of the J chain in multimeric antibodies, and which antibody isotypes use it?
It helps link multiple antibody molecules together, forming multimeric structures. It is found in multimeric forms of antibodies such as IgM and IgA
How does the structure of IgM as a pentamer contribute to its function in the immune response?
The pentameric structure of IgM, which consists of five IgM molecules linked together, allows it to be highly effective at agglutinating antigens and activating the complement system. This multimeric form enhances its ability to bind to pathogens.

Why is IgA secreted as a dimer in mucosal areas, and what role does this form play in mucosal immunity?
To enhance its ability to protect mucosal surfaces. The dimeric form, which includes two IgA molecules linked by a J chain, is effective at neutralizing pathogens and toxins at mucosal sites such as the gut and respiratory tract.
Remember: IgA is a monomer in the serum and dimeric at mucosal surfaces

More mature antibodies have a lower or higher affinity?
More mature antibodies have higher affinity for their specific antigen due to affinity maturation, which involves somatic hypermutation and selective pressure. B cells undergo mutations in their antibody genes, and those producing higher-affinity antibodies are preferentially selected. This process refines the antibodies' binding strength, resulting in more effective antigen recognition and response.
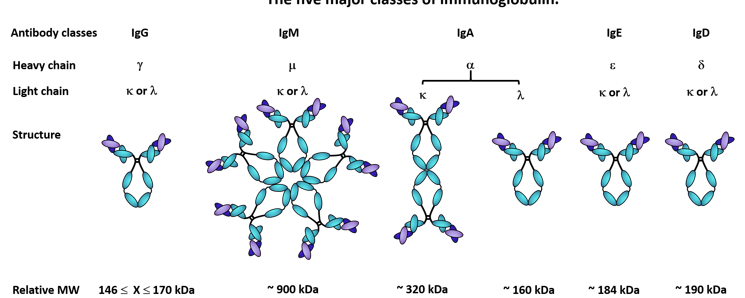
What are T cell-dependent and T cell-independent antigens
T-dependent antigens are typically proteins or glycoproteins that require T cell assistance for B cell activation. B cell activation includes affinity maturation and isotype switching.
T-independent antigens are usually polysaccharides or glycolipids, and rarely proteins, and can activate B cells directly without T cell help. They typically crosslink the B cell receptor and almost always produce IgM and don’t undergo affinity maturation or isotype class switching.
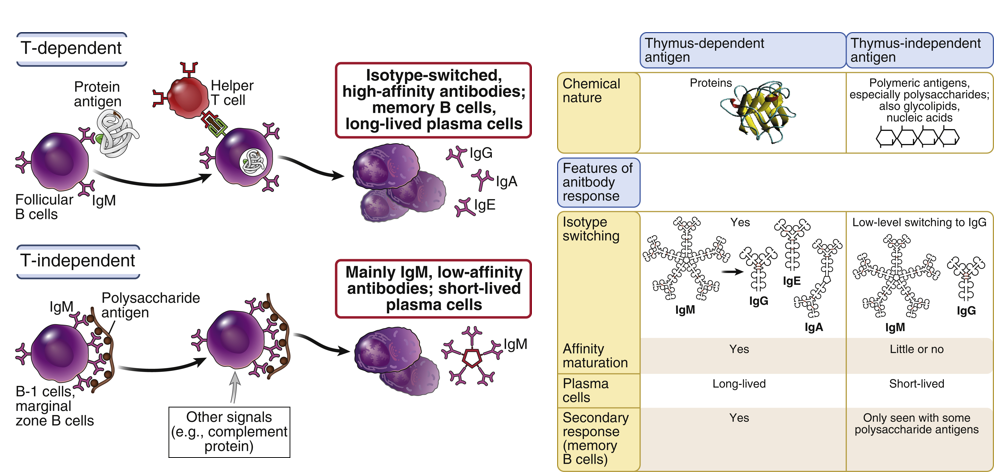
Explain the process of T dependent antigen activation
The antigen, typically a protein or glycoprotein, binds to a B cell, which processes and presents it on MHC class II. The antigen is also processed and presented by macrophages or dendritic cells.
The antigen-loaded B cell interacts with an activated CD4+ T helper cell. The T cell provides essential costimulation and cytokines that are important for B cell activation.
Activated B cells initially secrete IgM antibodies. They then undergo isotype switching to produce IgG, IgE, or IgA antibodies, and differentiate into long-lived memory B cells.
Explain the process of T independent antigen activation
In T-independent B cell activation, the antigen binds to multiple receptors on the B cell surface, causing receptor crosslinking. This direct activation leads to the B cell's immediate secretion of IgM antibodies.
Does T independent B Cell Activation isotype switch and differentiate into memory cells?
No. The response primarily produces IgM antibodies. It also does not result in the formation of long-lived memory B cells.
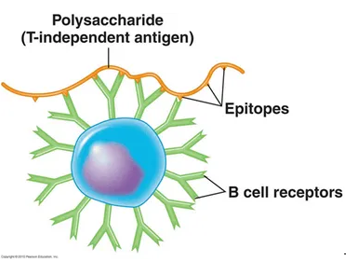
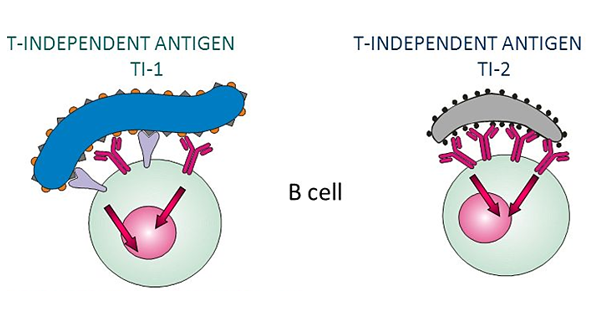
How do T-independent 1 (TI-1) and T-independent 2 (TI-2) antigens differ in their mechanisms of B cell activation?
T-independent 1 (TI-1) antigens activate B cells by cross-linking the B cell receptor (BCR) along with additional receptors. BCR+ another receptor
T-independent 2 (TI-2) antigens activate B cells solely through cross-linking the BCR without involving other receptors. BCR ONLY