muscle 1 and muscle physiology
1/133
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
134 Terms
how many human muscles are there
over 600
what precent of bodyweight do muscles take up
over half of bodyweight
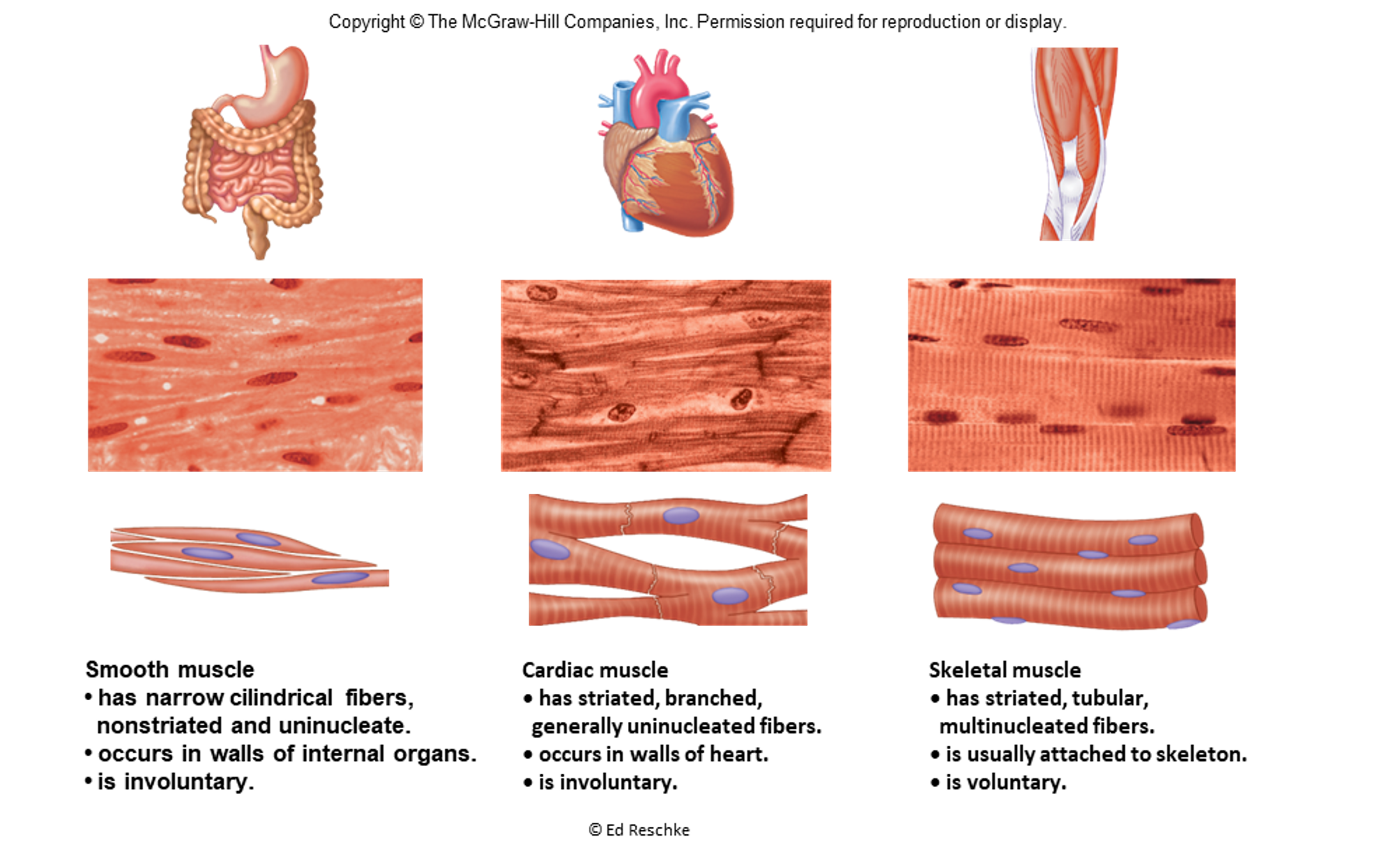
what are the 3 kinds of muscle
smooth, cardiac, and skeletal
what is the major purpose muscles are specialized for
converting chemical energy into mechanical energy
what kind of muscle does this describe:
has narrow cylindrical fibers non-striated and uninucleate
occurs in walls of internal organs
is voluntary
smooth muscle
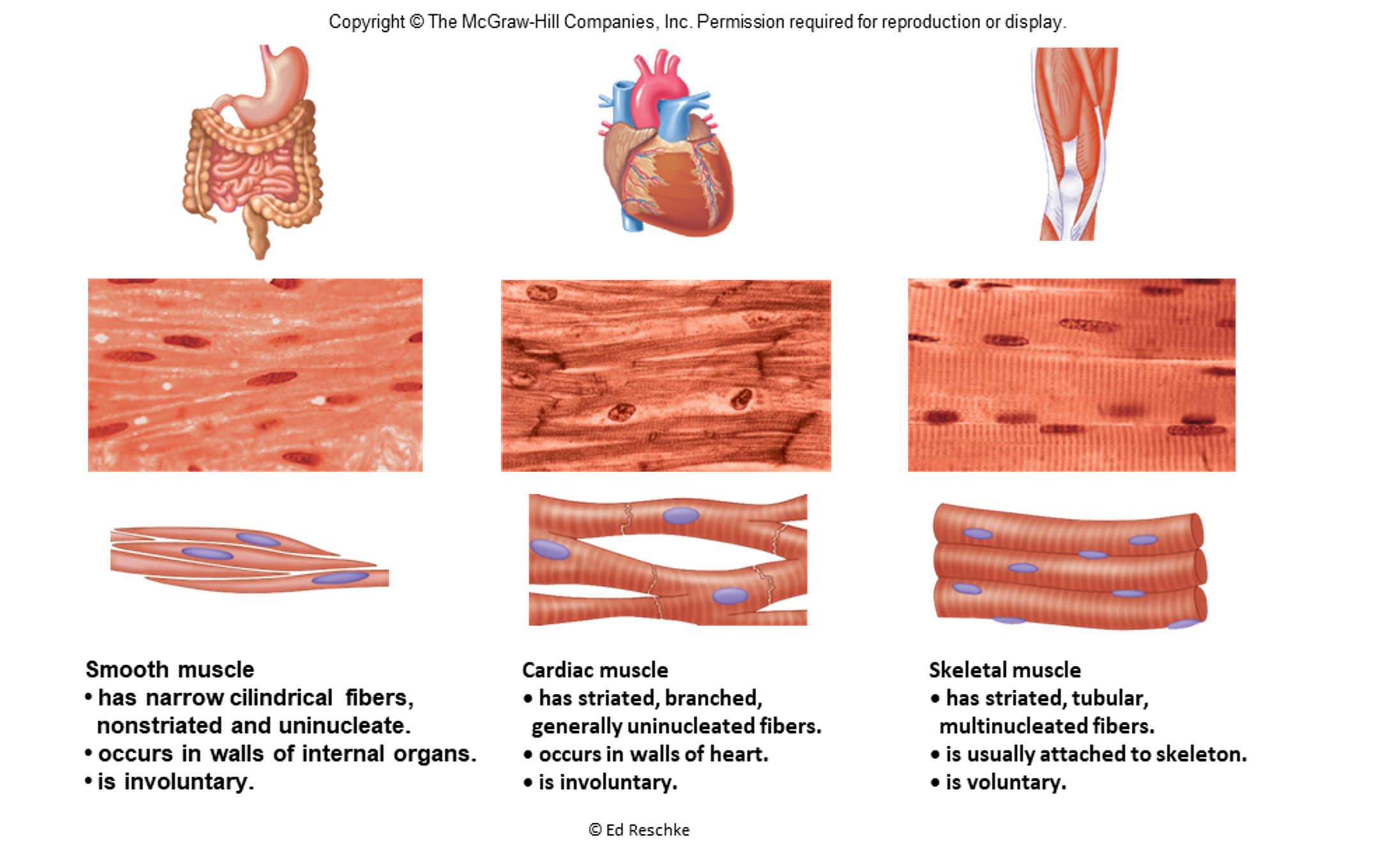
what type of muscle does this describe:
has striated, branched, generally uninucleated fibers
occurs in walls of heart
is involuntary
cardiac muscle
what type of muscle does this describe:
has striated, tubular, multinucleated fibers
is usually attached to skeleton
is voluntary
skeletal muscle
what are the functions of skeletal muscle?
body movement: move bones, make facial expressions, speak, breathe, swallow
maintenance of posture: stabilize joints, maintain body position
protection and support: package internal organs and hold them in place
regulating elimination of materials: circular sphincters control passage of material at orifices
heat production: help maintain body tempurature
what are the characteristics of skeletal muscle tissue? also the universal characteristics of muscle
excitability: ability to respond to a stimulus by changing electrical membrane potential
conductivity: involves sending an electrical change down the length of the cell membrane
contractility: exhibited when filaments slide past each other; enables muscle to cause movement
extensibility: ability to be stretched
elasticity: ability to return to original length following a lengthening or shortening
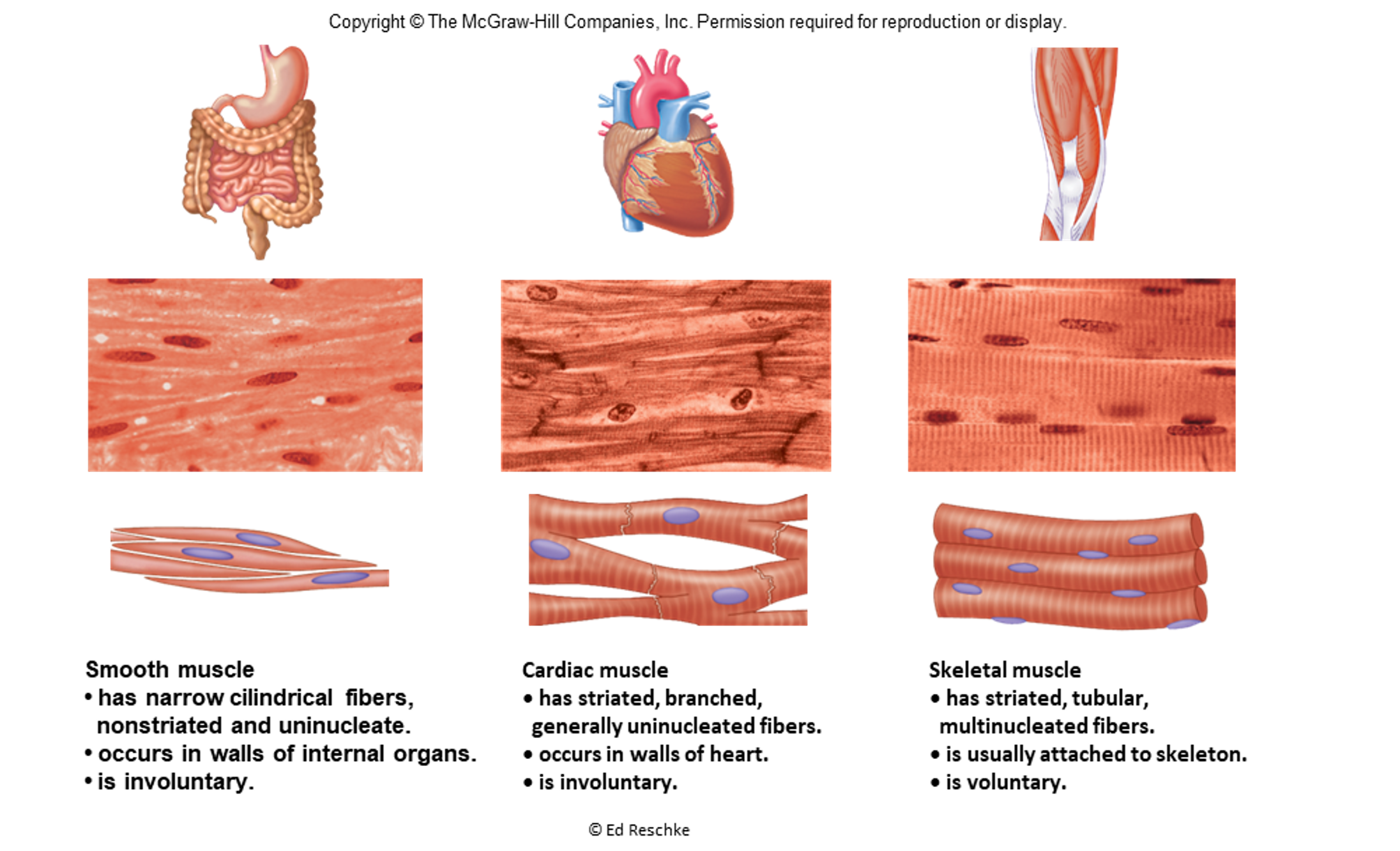
Each skeletal muscle is an _______. With multiple types of tissues working together: skeletal muscle fibers, connective tissue, blood vessels, and nerves.
organ
Muscle fibers bundled within a _____.
fascicle
a whole muscle contains many fascicles
a fascicle consists of many ____. A muscle fiber is a muscle cell.
muscle fibers
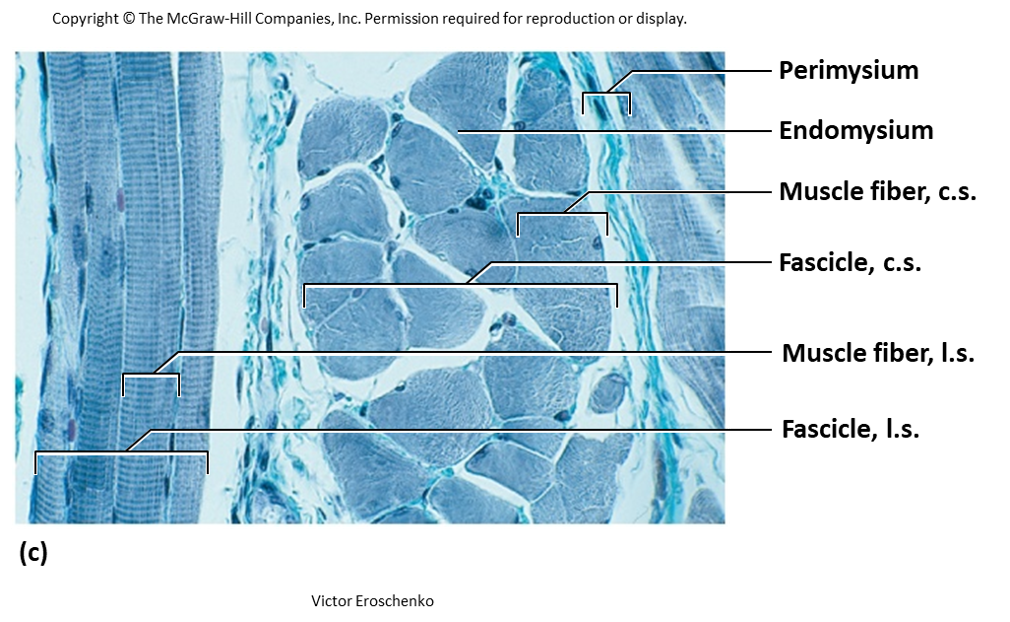
what are the 3 concentric layers of wrapping in skeletal muscle?
epimysium, perimysium, and endomysium
what layer of connective tissue concentric wrapping does this describe:
dense irregular connective tissue wrapping whole muscle
epimysium
what layer of connective tissue concentric wrapping does this describe:
dense irregular connective tissue wrapping fascicle
houses many blood vessels and nerves
perimysium
what layer of connective tissue concentric wrapping does this describe:
areolar connective tissue wrapping individual fiber
delicate layer for electrical insulation, capillary support, binding of neighboring cells
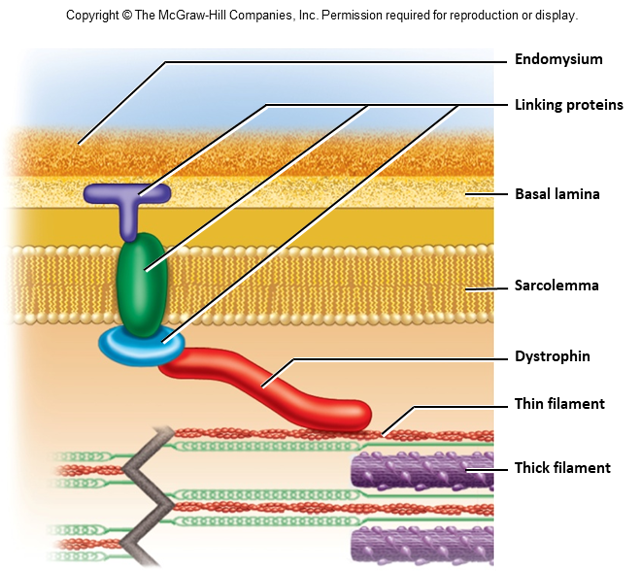
endomysium
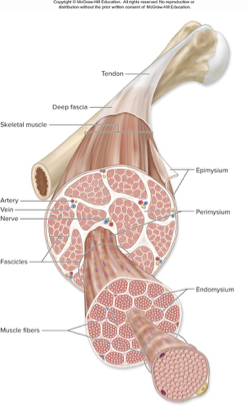
what two ways can muscles be attached to muscle or bone (or skin to another muscle)
tendon
aponeurosis
tendon
cordlike structure of dense regular connective tissue
aponeurosis
thin flattened sheet of dense irregular tissue
deep fascia
dense irregular connective tissue superficial to the epimysium
sperates individual muscles, binds muscles with similar functions
superficial fascia
areolar and adipose connective tissue superficial to deep fascia
separates muscles from skin
what does this describe:
tendons bridge the gap between muscle ends and bony attachment
collagen of the endo-, peri-, and epimysium continuous
connects into the periosteum and the matrix of the bone
aponeurosis - broad flat sheet (palmar aponeurosis)
retinaculum - connective tissue band that separate tendons from muscles underneath
indirect attachment to bone
what does this describe:
little separation between muscle and bone
muscle seems to immerge directly from bone: margins of brachialis, lateral head of triceps brachii
direct (fleshy) attachment to bone
some muscles insert on the fascia or tendon of another muscle or collagen fibers of the dermis
distal tendon of biceps brachii inserts on the fascia of teh forearm
facial muscles insert in the skin
origin
belly
insertion
origin: bony attachment at stationary end of muscle
belly: thicker, middle region of muscle between origin and insertion
insertion: bony attachment to mobile end of muscle
is skeletal muscle vascularized
yes, has extensive blood vessels that deliver oxygen and nutrients, and remove waste products
is skeletal muscle innervated by somatic neurons
yes
axons of neurons branch, terminate at neuromuscular junctions
can allow for voluntary control of contraction
what are the parts of a muscle cell (fiber)
sarcoplasm (cytoplasm)
multiple nuclei: individual cells are multinucleated
sarcolemma (plasma membrane)
myofibrils
sarcoplasmic reticulum
myofilaments
what part of a muscle cell does this describe:
has typical organelles plus contractile proteins and other specializations
sarcoplasm/cytoplasm
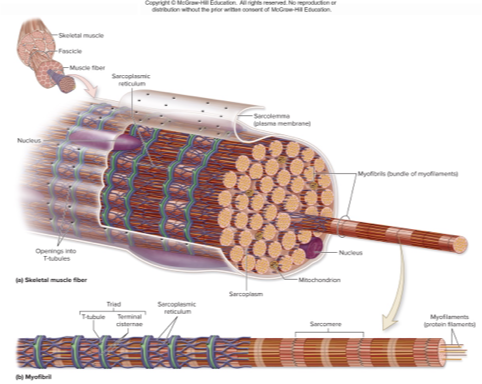
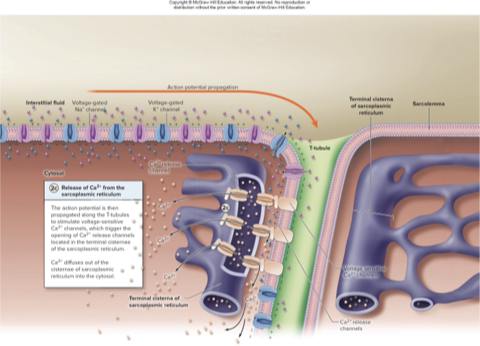
what part of a muscle cell does this descrbe:
has T-tubules (transverse tubules) that extend deep into the cell
sarcolemma and its t-tubules have voltage-gated ion channels that allow for conduction of electrical signalsihas voltage-sensitive calcium channels that are responsive to the electrical signals (action potentials)
sarcolemma/plasma membrane
what part of a muscle cell does this describe:
hundreds to thousands per cell
bundles of myofilaments enclosed in sarcoplasmic reticulum
myofibrils
what part of a muscle cells does this describe:
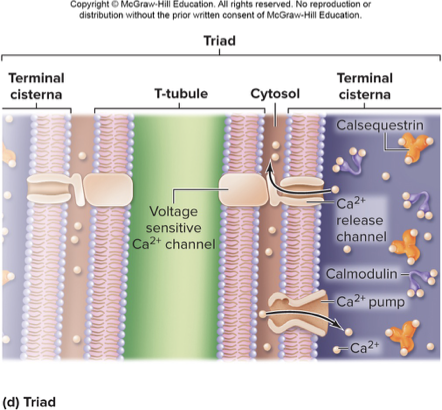
internal membrane complex similar to smooth ER
terminal cisternae: blind sacs of sarcoplasmic reticulum; serve as reservoirs for calcium ions; two cisternae with t-tubule inbetween = triad
contains calcium pumps that import calcium; binds to calmodulin and calsequestrin
contains calcium release channels; triggered by electrical signal traveling down T-tubule, calcium released into sarcoplasm
sarcoplasmic reticulum
what part of muscle cells does this describe:
contractile proteins within myofibrils; two types: thick and thin
myofilaments
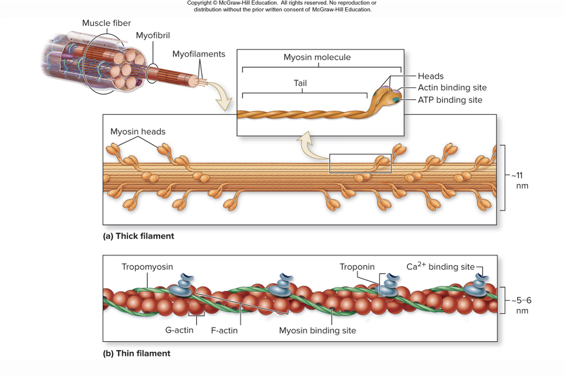
thick filaments
consist of bundles of many myosin protein molecules; myosin heads point toward ends of the filament
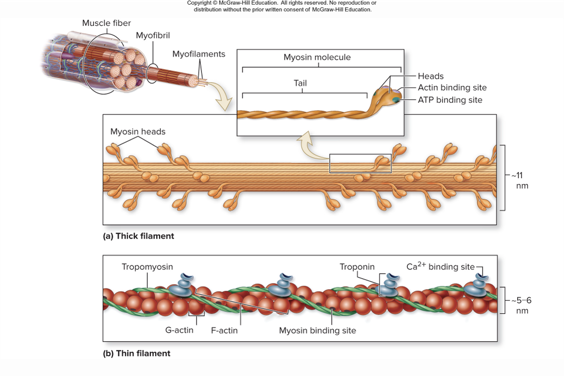
thin filaments
consist of bundles of many myosin protein molecules
twisted strands of F-actin; each F-actin composed of G-actin monomers
G-actin has myosin binding site where myosin heads attach
tropomyosin and troponin are present; regulator proteins
elastic filaments in myofilaments
titin (connectin)
attach thick filament to the z disc
prevent overstretching
at least 7 other accessory proteins
dystrophin is clinically important
describe the organization of a sarcomere
myofilaments arranged in repeating units called sarcomeres
composed of overlapping think and thin filaments
delineated at both ends by z-discs; specialized proteins perpendicular to myofilaments; anchors for thin filaments
the positions of thick and thin filaments gice rise to alternating I-bands and A-bands
what part of the sarcomere does this describe:
light-appearing regions that contain only thin filaments
bisected by Z disc
get smaller when muscle contracts (can disappear with maximal contraction)
I bands
what part of sarcomere does this describe:
dark-appearing region that contains thick filaments and overlapping thin filaments
contains H zone and M line
makes up central region of sarcomere
A band

what does this describe:
central portion of A bad
only thick filaments present; no thin filament overlap
disappears with maximal muscle contraction
H zone

what does this describe:
middle of H zone
protein meshwork structure
attachment site for thick filaments
M line
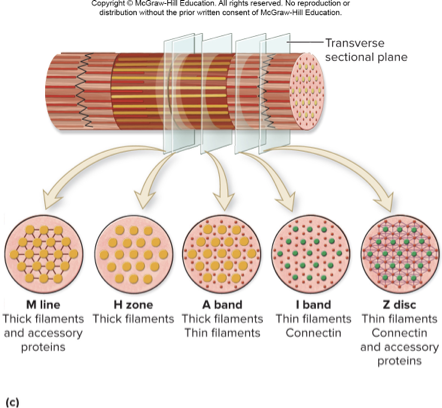
connectin
extends from z disc to m line
stabilizes thick filaments and has “springlike” properties (passive tension)
dystophin
anchors some myofibrils to carcolemme proteins
abnormalities of this protein cause muscular dystrophy
duchenne muscular dystrophy (DMD): most common type, defective or insufficient dystrophin; sarcolemma damaged during muscle contraction; problems begin early childhood; incurable, patients rarely live to be 30
muscle fibers have abundant ____ for aerobic ATP production
mitochondria
_____ within cells allows storage of oxygen used for aerobic ATP production
myoglobin
____ is stored for when fuel is needed quickly
glycogen
________ ________ can quickly give up its phosphate group to help replenish ATP supply
creatine phosphate
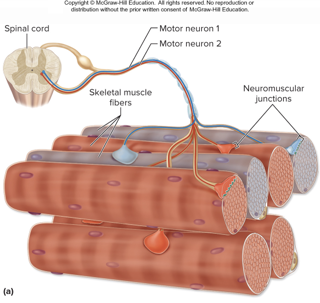
motor unit
a motor neuron and all the muscle fibers it controls
axons of motor neurons from spinal cord or brain innervate numerous muscle fibers
the number of fibers a neuron innervates varies: small motor units have less than 5 to allow for precise control of force output::: large motor units have thousands of muscle fibers to allow for production of large amounts of force but not precise control
fibers of a motor unit are dispersed throughout the muscle, not just in one clustered compartment
synaptic knob
expanded tip of the motor neuron axon
houses syaptic vesicles: small sacs filled with neurotransmitter acetylcholine
has Ca 2+ pumpsin plasma membrane; establish calcium gradient with more outside the neuron
has voltage-gated Ca2+ channels in membrane: Ca2_ flows into cell down conc, gradient if channels open
motor end plate
specialized region of sarcolemma with numerous folds
has many ACh receptors: plamsa membrane protein channels, opened by binding of ACh, allow Na+ entry and K+ exit
synaptic cleft
narrow fluid-filled space
seperates synaptic knob from motor end plate
acetylcholinesterase resides here: enzyme that breaks down ACh molecules
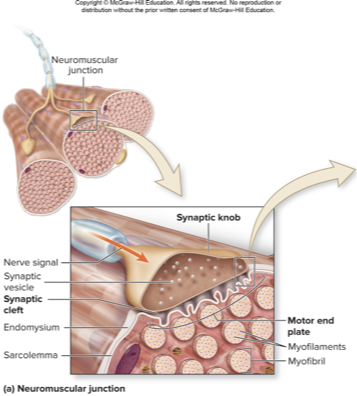
neuromuscular junction
location where motor neuron innervates muscle
usually mid-region of muscle fiber
has the following parts: synaptic know, synaptic cleft, motor end plate

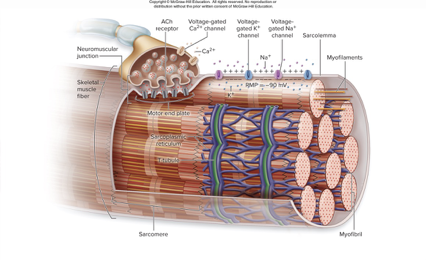
muscle fibers exhibit resting membrane potential (RMP)
fluid inside cell is negative compared to fluid outside the cell
RMP of muscle cell is about -90mV
RMP established by leak channels and Na+/K+ pumps (voltage-gated channels are closed)
Z line (disc)
anchor for thin filaments
M line
anchor for thick filaments
A band
dark area; extends length of the thick filaments
I band
light area; think myofilaments only (Z disc is center of I band)
H zone
thick myofilaments only (M line is center of H zone)
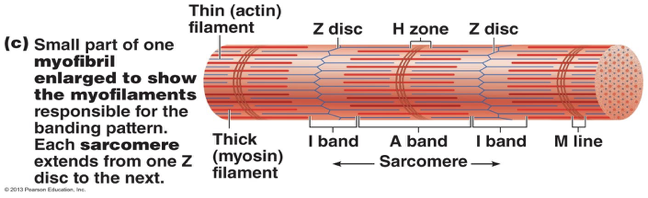
sarcomere
funcational unit of skeletal muscle; Z disc to Z disc; aligned end to end within myofibril
what does this describe:
makes up thick myofilaments (~300 myosin molecules per thick myofilament)
rodlike tail & 2 globular heads
heads contain binding sites for actin and ATP
myosin
what does this describe:
makes up thin myofilaments
made of G-actin (polypeptide subunits): contain binding sites for myosin heads; G-actin strung together; 2 twisting strands make up thin myofilaments
actin
what does this describe:
in thin myofilaments
rod-shaped protein that runs along actin
blocks myosin-inding sites on actin when muscle relaxed
tropomyosin
what does this describe:
in thin myofilaments
3 polypeptide subunit complex: 1 subunit boud to actin, 1 subunit bound to tropomyosin, 1 subunit binds Ca2+
troponin
what does this describe:
special type of smooth endoplasmic reticulum
stores and regulates intracellular Ca tha is necessary for contraction
has interconnecting tubules that surround each myofibril
most tubules run longitudinally alonf myofibril
sarcoplasmic reticulum
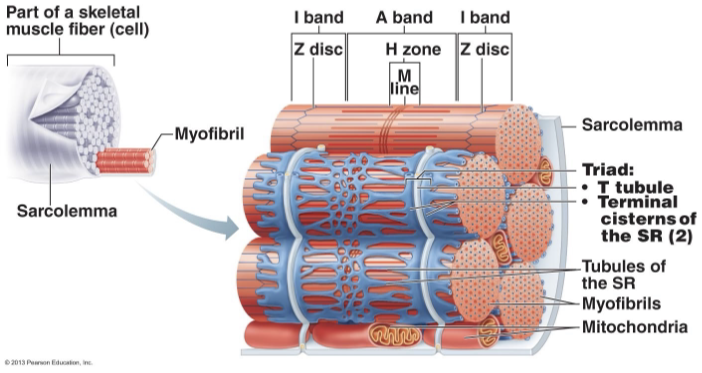
what forms a traid
sarcoplasmic reticulum: stores and regulates intracellular Ca
terminal cisternae: as each A band/I band junction
T tubules: invaginations of sarcolemma
integral proteins protruding from t-tubule into space between t-tubule and terminal cisternae act as ______ _______.
voltage sensors
integral proteins in terminal cisternae that form ___ channels
Ca
how do muscles contract
1 muscle fiber stimulated by nerve ending: causes change in membrane potential
2 generate and propagate electrical impulse: an electrical impulse has to be generated and propagated along the muscle fibers
3 increase in intracellular Ca: increase in intracellular Ca is the trigger for contraction to occur
it takes both ____ and ____ for contrcation of muslces to occur
nervous and muscular systems
4 major phases of contraction/relaxation
excitation: nerve action potentials→ musclel actions potentials
excitation-contraction coupling: series of events leading to changes in myofilaments
contraction: muscle fiber develops tension and may shorten
relaxation: muscle fiber relaxes and returns to its resting length
voltage (electrical potential)
a difference in electrical charge from one point to another
resting membrane potential
about -90mV
more anions on inside of plasma membrane compared to outside
excess sodium ions (Na+) in the extracellular fluid (ECF)
excess potassium ions (K+) in the intracellular fluid (ICF)
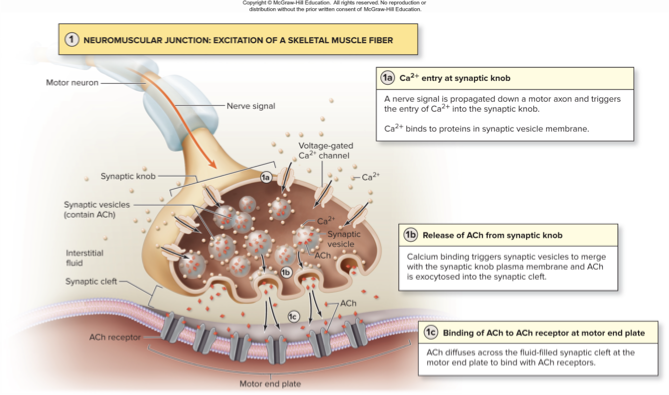
explain the steps of excitation
1: calcium enters at the synaptic knob; nerve signal travels down axon, opens voltage-gated Ca2+ channels, Ca2+ diffuses into synaptic knob, Ca2+ binds to proteins on surface of synaptic vesicles
2: release of ACh from synaptic knob; vesicles merge with cell membrane at synaptic knob: exocytosis; thousands of ACh molecules released from about 300 vesicles
3: binding of ACh at motor end plate; ACh diffuses across celft, binds to receptors, excites fiber
excitation contraction coupling
stimulation of the fiber is coupled with the sliding of filaments
coupling includes the end-plate potential (EPP), muscle action potential, and release of Ca2+ from the sarcoplasmic reticulum
describe end-plate potential (EPP)
ACh receptors are chemically gateed channels that open when ACh binds to them
Na+ diffuses into the cell through the channels, while a little K+ diffueses out
cell membrane breifly becomes less negative at the end-plate region
EPP is local but it does lead to the opening of voltage gated ion channels in the adjacent region of the sarcolemma
describe initiation and propagation of action potential along the sarcolemma and t-tubules
an action potential (AP) is a rapid rise (depolarization) and fall (repolarization) in the charge of the membrane: EPP reaches threshhold by causing nearby voltage-gated channels to open
Na+ diffuses into the cell through voltage-gated channels: cell depolarizes/becomes less negative eventually +30mV; this results in opening of adjacent voltage-gated Na+ channels and more Na+ entry; a chain reaction occurs as a depolarization is propogated down teh membrane and t-tubules
just after Na+ channels open, they close and voltage-gated K+ channels open; K+ diffuses out of the cell; cell repolarizes to -90mV; repolarization is then propogated down the membrane and t-tubules
while the cell is depolarizing and repolarizing it is in a refractory period-unable to respond to another stimulation
describe what happens when AP travels down t-tubules and the release of Ca2+ from sarcoplasmic reticulum
causes voltage-sensitive calcium channels in T-tubule membrane to trigger the opening of calcium release channels in SR terminal cisternae
Ca2+ interacts with myofilaments triggering contraction
cross-bridge cycling
when Ca2+ binds to troponin, it triggers crossbridge cycling
troponin and tropomyosin move so actin is exposed
cycling continues as long as Ca2+ and ATP are present
results in sarcomere shortening as Z discs move closer together
narrowing or disappearance of H zone and I band
thick and thin filaments remian the same length but slide past each other
4 repeating steps of crossbridge cycling
1: crossbridge formation: myosin head attaches to exposed binding site on actin
2: power stroke: myosin head pulls thin filament toward center of sarcomere; ADP and Pi released
3: release of myosin head: ATP binds to mysoin head casuing its release from actin
4: reset myosin head: ATP split into ADP and Pi by myosin ATPase; provides energy to cock the myosin head
describe steps of sliding filament model of contraction
1 thin filaments slide past thick filaments due to crossbridge formation
2 the I-bands shorten
3 sarcomeres chorten
4 H-zones disappear
5 A-bands move closer together but length is same
events of muscle relaxation
termination of nerve signla and ACh release from motor neuron
hydrolysis of ACh by acetylcholinesterase
closuer of ACh receptor causes cessation of end plate potential
no further action potential generation
closure of calcium channels in sarcoplasmic reticulum
return of Ca 2+ to sarcoplasmic reticulum by pumps
return of troponin to original shape
return of tropomyosin blockade of actin’s myosin binding sites
return of muscle to original position due to elasticity
electrical excitation of a muscle fiber follows all-or-none law
muscle fiber twitches do not
muscle twitch strength is dependent upon:
muscle size
fascicle arrangement
temporal summation
multiple motor unit summation
how stretched muscle was before it was stimulated
temperature of the muscles
lower than normal pH of sarcoplasm
state of hydration of muscle
fatigue
tetanus
spastic paralysis caused by toxin
blocks release of inhibitory neurotransmitter in spinal cord resulting in overstimulation of muscle
vaccination prevents this
botulism
muscular paralysis caused by toxin
prevents release of ACh at synaptic knobs
although toxin ingestion can be fatal, careful injections of it can treat spasticity or can be use for cosmetic purposes
muscle tension
tension is the force generated when a muscle is stimulated to contract
lab experiments measure tension and graph it (myogram)
muscle twitch
a breif contraction to a single stimulus: the minimum voltage that a triggers a twitch is the threshold
what are the periods of a twitch
latent period
contraction period
relaxation period
latent period
time after stimulus but before contraction begins
no change in tension
contraction period
time when tension is increasing
begins as power strokes pull thin filaments
relaxation period
time when tension is decreasing to baseline
begins with release of crossbridges
generally lasts a little longer than contraction period
recruitment or multiple motor unit summation
muscle is stimulated repeatedly
as voltage increase, more units are recruited to contract
it explains how muscles exhibit varying degerees of force: recruit few motor units to lift pencil vs many to life suitcase
above certain voltae, all units are recruited and so maximum contractions occurs regardless of how much higher voltage is
recruitement order is based on size of motor units: small first, large last
wave summation (temporal summation)
if stimulus frequency set at about 20 per second, relaxation is not comlpeted between twitches
contractile forces add up to produce higher tensions
incomplete tetany and tetany
if frequency is increased further, myogram exhibits incomplete tetany: tension increases and twitches partially fuse
if frequency is incresed furtehr still (40-50 per sec) myogram exhibits tetany:tension trace is a smooth line without relaxation
high frequency stimuli lead to fatigue, decrease tension production
muscle tone
resting tension in a muscle
generated by involuntary nervous stimulation of muscle
some motor units stimulated randomly at any time
change continuously so units not fatigued
do not generate enough tension for movement
decreases during deep sleep
isometric contraction
although tension is increased, it is insufficient to overcome resistance
muscle length stays the same
ex: holding a weight while arm doesnt move
isotonic contraction
muscle tension oversomes resistance resulting in movement
tone stays constant, but length changes
concentric contraction
muscle shortens as it contracts
eg: biceps brachii when lifting