Injury Response and Therapeutic Modalities in Athletic Training
1/83
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
84 Terms
What is the primary role of therapeutic modalities in injury treatment?
To provide an optimal environment for healing to occur.
What is a therapeutic modality?
A form of stress applied to the body to elicit an involuntary physiological response.
What can happen if a modality is applied at an improper point in recovery?
It may hinder or set back the healing process.
What does the Physical Stress Theory describe?
How tissues react relative to the amount of stress they receive compared to normal.
What is the tissue response to low physical stress?
Decreased tolerance, such as atrophy.
What is the tissue response to moderate physical stress?
Increased tolerance, such as hypertrophy.
What are the three stages of the General Adaptation Syndrome?
Alarm Stage, Resistance Stage, and Exhaustion Stage.
What occurs during the Alarm Stage of stress response?
The body's initial sudden reaction to a change in homeostasis.
What characterizes the Resistance Stage of the General Adaptation Syndrome?
The body adapts to the stressor using homeostatic resources to maintain integrity.
What happens during the Exhaustion Stage?
The body cannot withstand stresses, potentially leading to traumatic or overuse injuries.
What is the relationship between physical stress and trauma?
Harmful stress can cause acute injuries (macrotrauma) and repeated low-intensity forces can lead to chronic conditions (microtrauma).
What does Wolff's Law state?
Bone adapts to the forces placed on it.
What is the consequence of applying a modality with too low intensity?
Little or no benefit is gained from the treatment.
What is an example of ineffective modality application?
A 60-degree cold pack applied for 5 minutes may not penetrate deeply enough to effect change.
What can occur if the magnitude of a modality is too great?
Further injury can occur if applied at the wrong point in the healing process.
What is an example of a modality that can cause further injury if misapplied?
A moist heat pack applied without covering.
What layers must therapeutic modalities penetrate to affect deeper tissues?
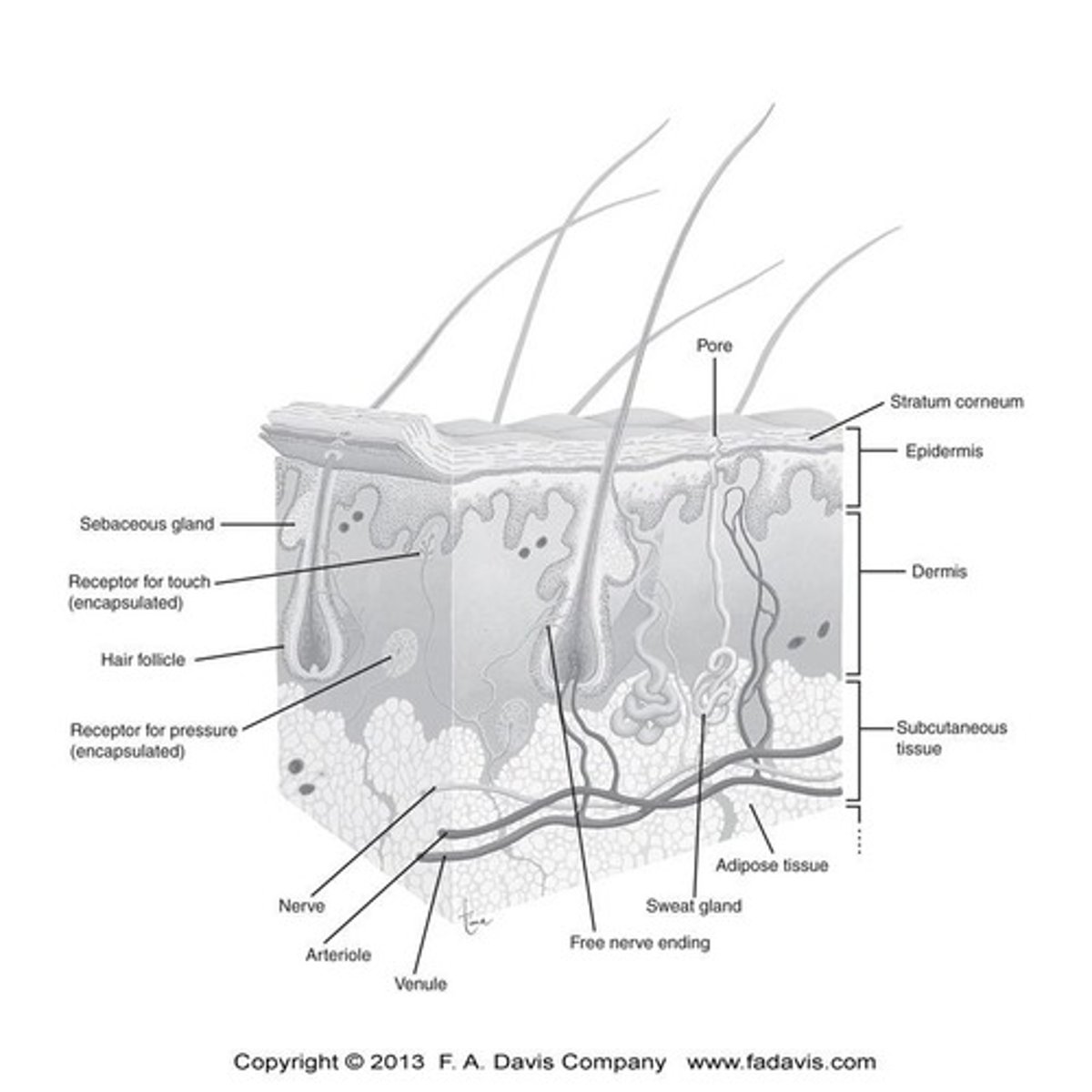
Epidermis, dermis, and subcutaneous adipose tissue.
What are the potential outcomes of harmful stress?
Acute injuries like sprains, strains, and fractures.
What can repeated low-intensity forces lead to?
Stress fractures, chronic inflammatory conditions, and muscle soreness.
What is the significance of the treatment duration in modality application?
If too short, it may not provide sufficient benefit.
What is the longest phase of the General Adaptation Syndrome?
The Resistance Stage, lasting many days, months, or years.
What are the main types of soft tissue found in the body?
Adipose tissue, epithelial tissue, muscle, nervous tissue, and connective tissue.
What is the primary function of adipose tissue?
Adipose tissue consists of fat cells and has a high water content.
What is a key characteristic of epithelial tissue?
Epithelial tissue secretes and absorbs various substances and is devoid of blood vessels.
What is the outer layer of skin formed by epithelial tissue?
The stratum corneum, which is composed of flat, densely packed dead cells.
How does adipose tissue affect the effectiveness of thermal agents?
The effectiveness of thermal agents such as cold packs or moist heat packs is reduced when applied over thick layers of adipose tissue.
What are the three types of muscle tissue?
Smooth muscle, cardiac muscle, and skeletal muscle.
What are the two types of muscle fibers and their characteristics?
Type I (slow-twitch) fibers are slow to fatigue and prevalent in postural muscles; Type II (fast-twitch) fibers generate high force quickly.
What are the two main divisions of nervous tissue?
The central nervous system (CNS) and the peripheral nervous system (PNS).
What is the basic functional unit of the nervous system?
The neuron, which consists of dendrites, the nerve body, and the axon.
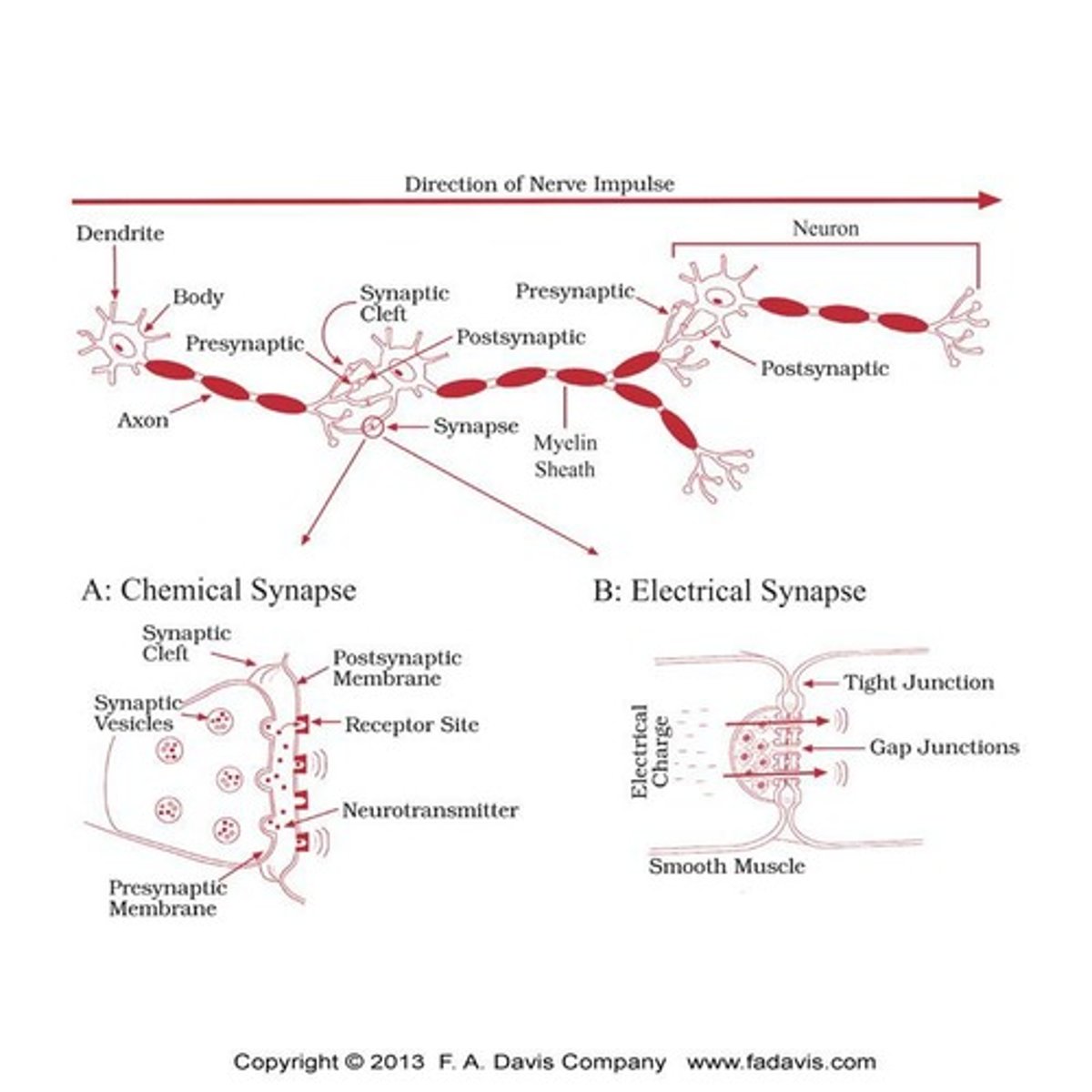
What is the role of neurotransmitters in nerve transmission?
Neurotransmitters are released from the presynaptic nerve, cross the synaptic cleft, and bind to receptor sites on the postsynaptic neuron.
What type of synapse is most common in the body?
Chemical synapses.
How do thermal agents and ultrasound influence nerve function?
They alter conduction velocities, slowing the rate of painful nerve transmission.
What is connective tissue primarily produced by?
Fibroblasts.
What components make up connective tissue?
Ground substance (cell matrix) and collagen fibers.
What determines the elasticity of connective tissue?
The ratio of inelastic collagen fibers to elastic yellow elastin fibers.
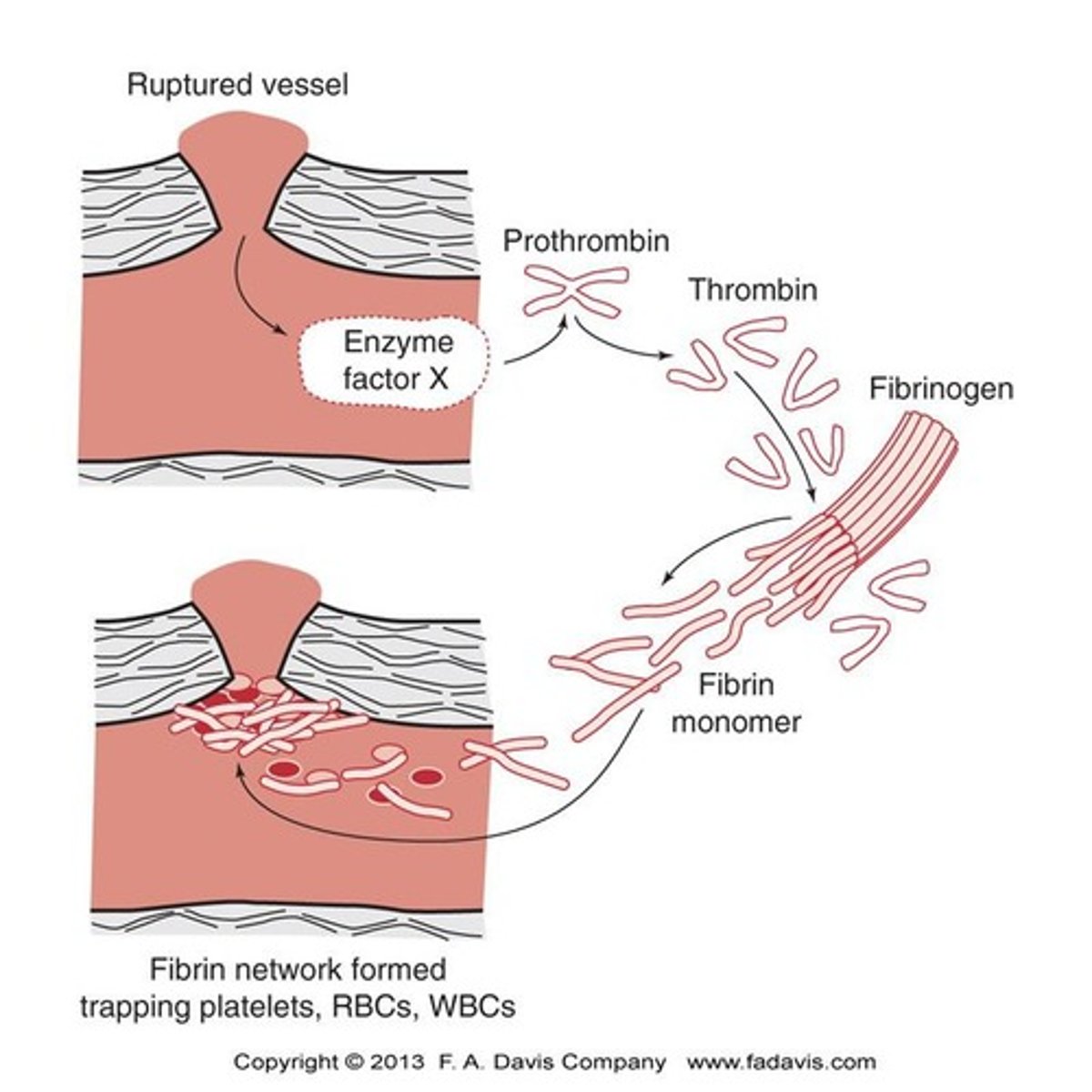
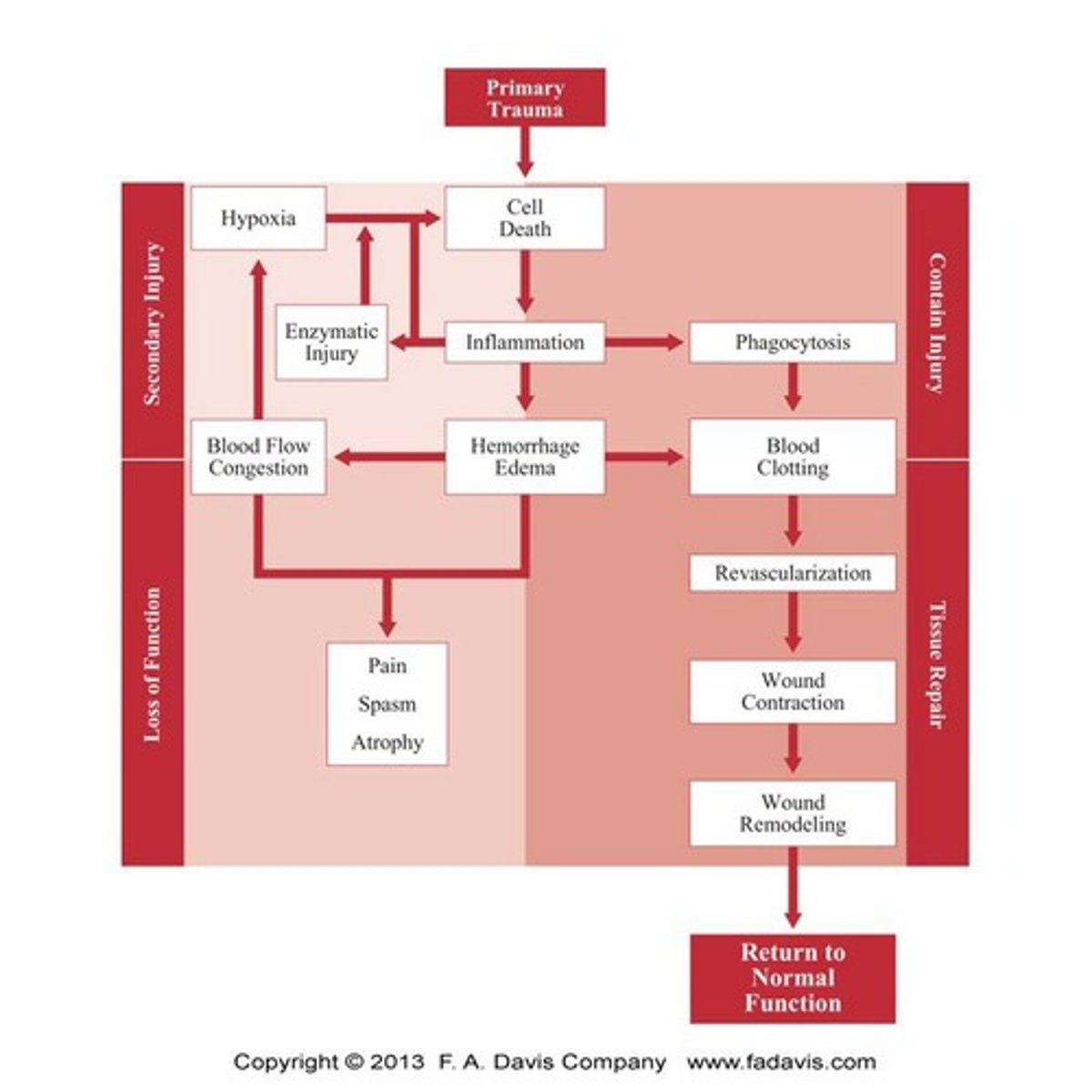
What is primary injury in the context of acute injury?
Tissue destruction directly resulting from the traumatic force.
What causes secondary injury?
Cell death due to blockage of oxygen supply (ischemia) or enzymatic damage and mitochondrial failure.
What is the purpose of treatment efforts after trauma?
To limit the amount of secondary injury.
What occurs when dead and damaged cells release their contents?
It causes an inflammatory reaction in the surrounding tissues.
What complications arise from the buildup of fluids after an injury?
Hemorrhage and edema cause mechanical pressure and chemical irritation of nerve receptors.
What is the pain-spasm cycle?
Further cell death due to lack of oxygen to surviving tissues, leading to increased pain and muscle spasms.
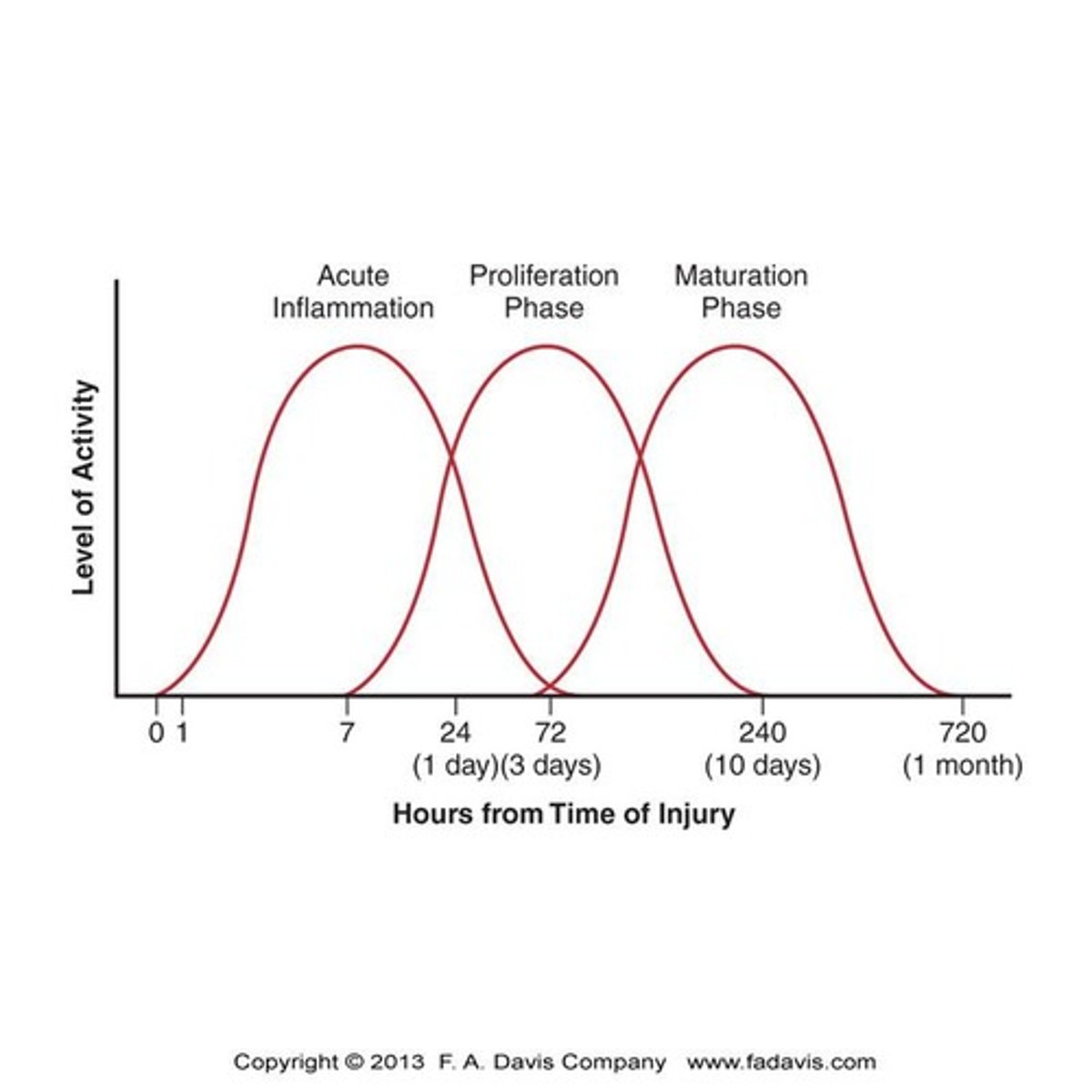
What are the three phases of the healing process for acute injuries?
Acute inflammatory response, Proliferation phase, Maturation phase.
What is the role of inflammation in the healing process?
Inflammation is necessary for healing, involving the migration of phagocytes and fibroblasts to the area and the formation of granulation tissue.
What happens to capillary permeability during the acute inflammatory response?
Histamine released from traumatized cells increases capillary permeability, causing swelling as proteins and water leak into tissues.
What are the stages of inflammation after an injury and their corresponding time frames?
Acute (0-14 days), Subacute (14-31 days), Chronic (>31 days past expected resolution).
What occurs during the proliferation phase of healing?
Increased number and size of fibroblasts, formation of ground substance and collagen, revascularization, and wound contraction.
What is the role of fibroblasts in the proliferation phase?
Fibroblasts increase in number and size, laying down collagen and preparing to rebuild damaged tissues.
What are myofibroblasts and their function during the proliferation phase?
Myofibroblasts accumulate at the margins of the wound and help decrease the size of the original fibrin clot.
What type of collagen is initially laid down during the proliferation phase?
Weak Type III collagen.
What happens to the collagen in the scar during the maturation phase?
The initial collagen is replaced with new and stronger types.
What is the significance of revascularization in the proliferation phase?
It forms new capillary beds around the margins of the wound, essential for healing.
What is the purpose of granulation tissue in the healing process?
It isolates and localizes the trauma, facilitating healing.
What is wound contraction and its role in healing?
Wound contraction decreases the size of the original fibrin clot and helps close the wound.
What cells are involved in the acute inflammatory response?
Phagocytes and fibroblasts.
What is the expected time frame for symptoms to diminish after an acute injury?
Symptoms typically diminish between 14 to 31 days after the injury.
What is unwarranted inflammation in the context of the chronic phase?
It refers to inflammation that persists beyond 31 days past the expected resolution.
How does external stress affect the remodeling of a wound?
External stress causes the alignment of fibers to remodel the wound.
What is the role of mast cells in the proliferation phase?
Mast cells stimulate fibroblasts to aid in tissue repair.
What happens to the size of the original fibrin clot during wound contraction?
The size of the original fibrin clot decreases.
What is the significance of collagen in scar development?
Collagen provides structural support and is essential for the strength of the scar.
What are the key components involved in the formation of granulation tissue?
Migration of phagocytes, fibroblasts, and the accumulation of ground substance and collagen.
What type of collagen starts to be replaced by Type I collagen 5-11 days after injury?
Type III collagen
What effect does early active range of motion (ROM) have on tensile strength?
It can increase tensile strength.
What is the maturation phase of the injury response process?
The final phase that may last a year or more, where fibroblasts, myofibroblasts, and macrophages reduce to preinjury levels.
What happens to the number of capillaries and overall vascularity during the maturation phase?
They are reduced.
How does the proportion of Type I collagen change during the maturation phase?
It continues to increase, replacing Type III collagen.
What is secondary injury in the context of acute injury?
Cell death due to a decrease in oxygen supply, often caused by ischemia.
What are some causes of secondary hypoxic injury?
Haemorrhaging, reduced blood flow, hydropic swelling, and pressure from hematoma and muscle spasm.
When is secondary injury first observed after primary trauma?
Within 30 minutes.
How can the application of cold packs help after musculoskeletal trauma?
It can decrease the amount of secondary injury.
What is edema?
An increase in the volume of a body part due to fluid build-up.
What causes increased capillary permeability after an injury?
Injury itself, which makes it easier for fluids and solid matter to leave the vessels.
What is the primary goal during early injury management regarding edema?
To decrease the formation of edema and remove swelling from the injury site.
How can ice application affect edema formation?
It reduces edema formation.
What is Starling's Law?
It describes the movement of fluids across the capillary membrane, affecting swelling formation or removal.
What forces fluids from the capillary outward to the tissues according to Starling's Law?
Vascular hydrostatic pressure and interstitial fluid colloid osmotic pressure.
What can cause muscle spasm?
Involuntary contraction of muscle fibers, often due to injury.
What is muscle atrophy and what can cause it?
A decrease in muscle mass caused by disuse or neurological dysfunction.
What is chronic inflammation?
A prolonged inflammatory response often caused by low-intensity irritants.
What are some signs of chronic inflammation?
Production of fibrous connective tissue, granulation tissue, and infiltration of mononuclear cells.
How does chronic inflammation differ from acute inflammation?
Vascular changes like vasodilation and fluid exudation are less pronounced or absent in chronic inflammation.
What is arthrogenic muscle inhibition (AMI)?
A condition where muscle inhibition occurs due to joint injury or inflammation.
What role does the lymphatic system play in edema?
It removes solid waste and helps regulate fluid balance in tissues.