The pharynx. Anatomy of deglutition
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
104 Terms
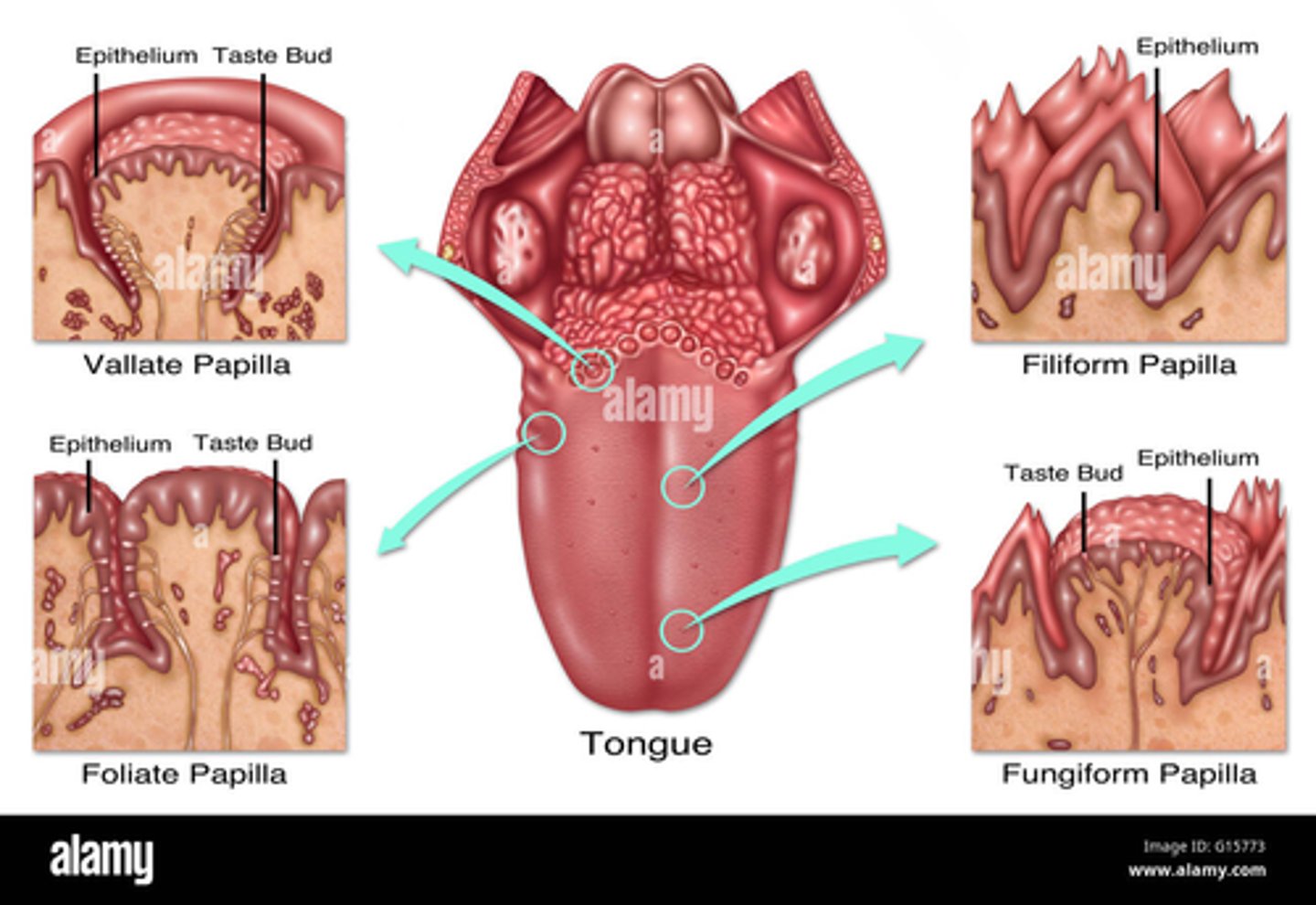
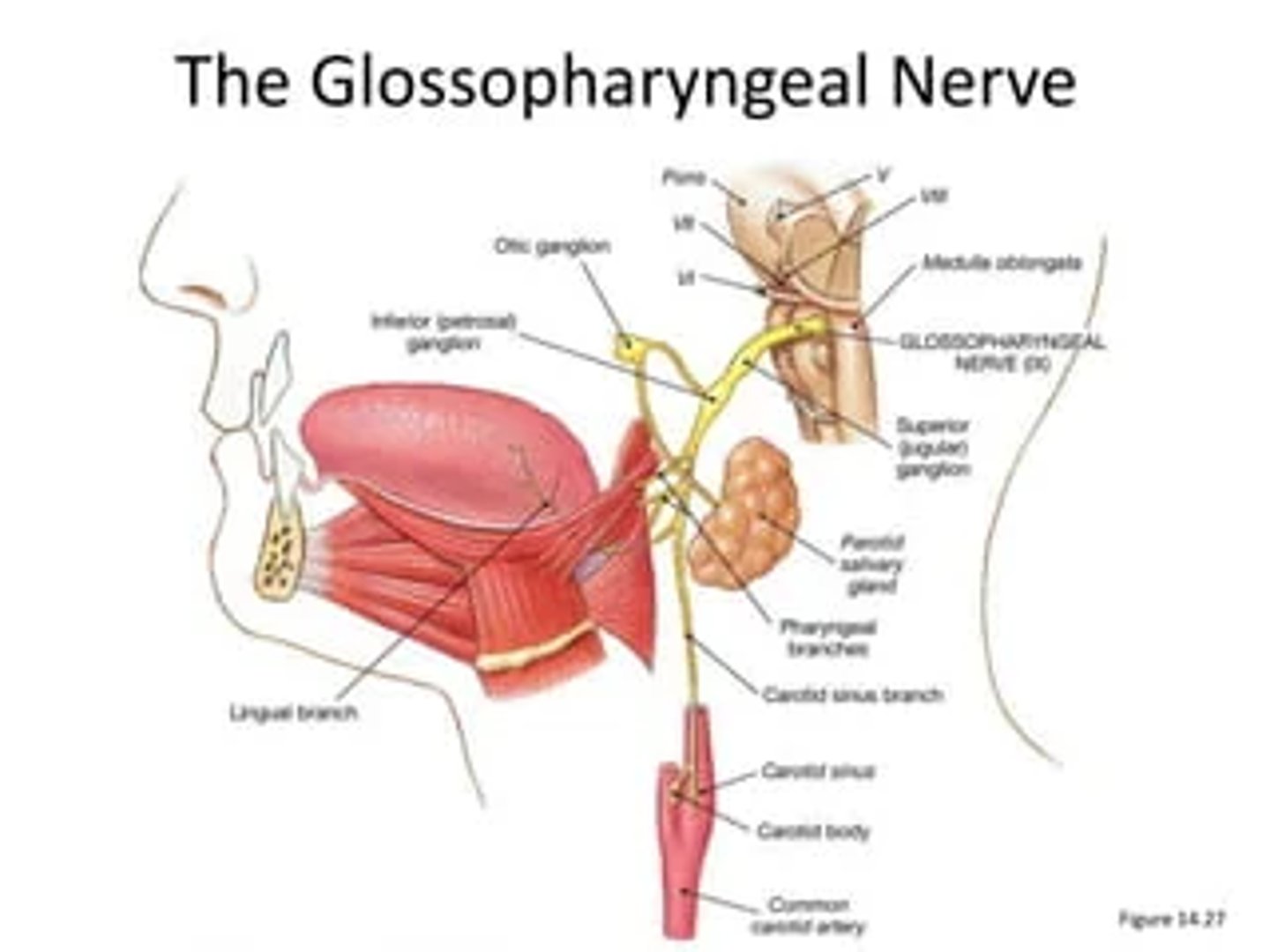
What is the glossopharyngeal nerve also known as?
CN IX
The glossopharyngeal nerve is also known as the ninth cranial nerve (IX CN).
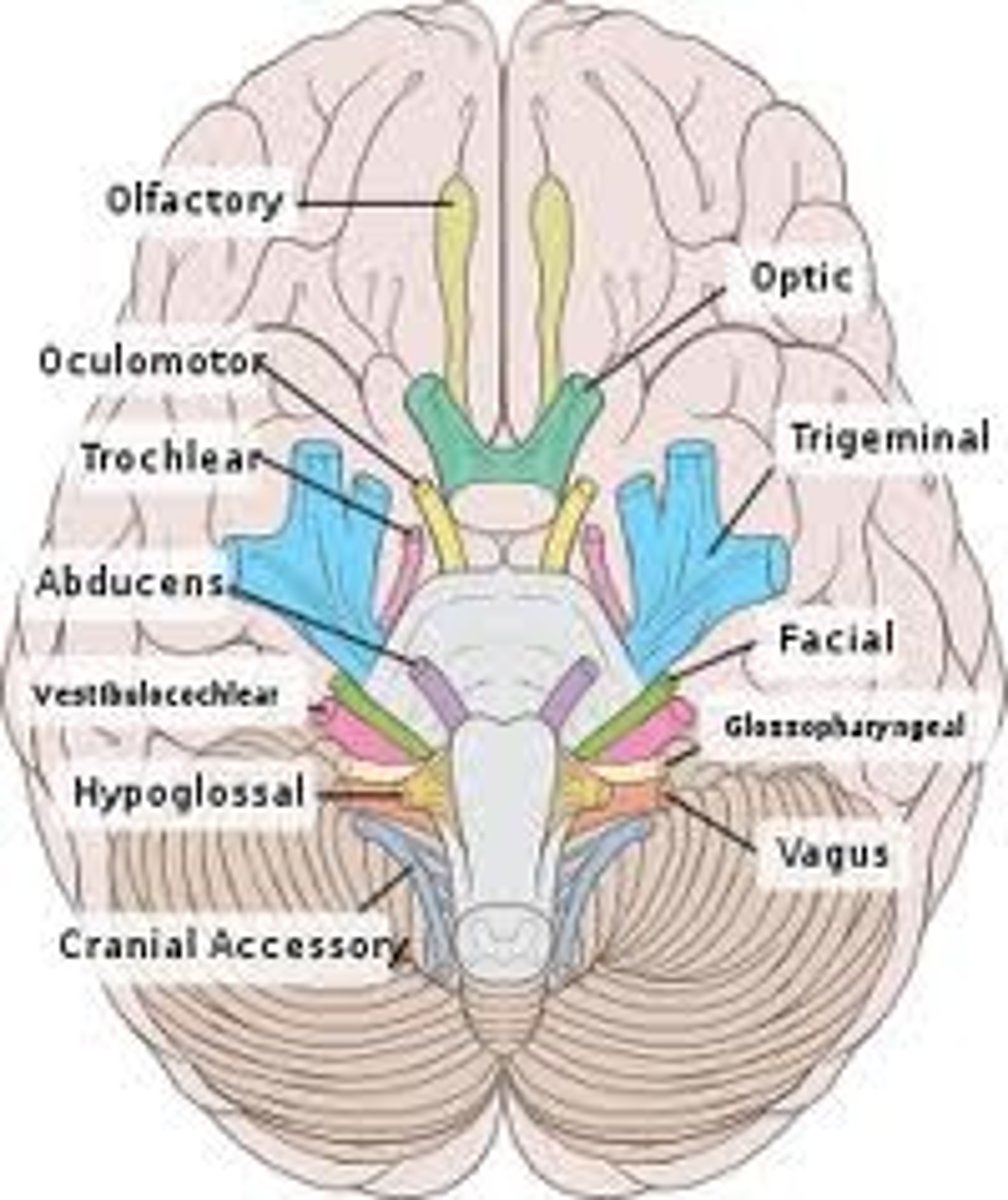
Where does the glossopharyngeal nerve originate?
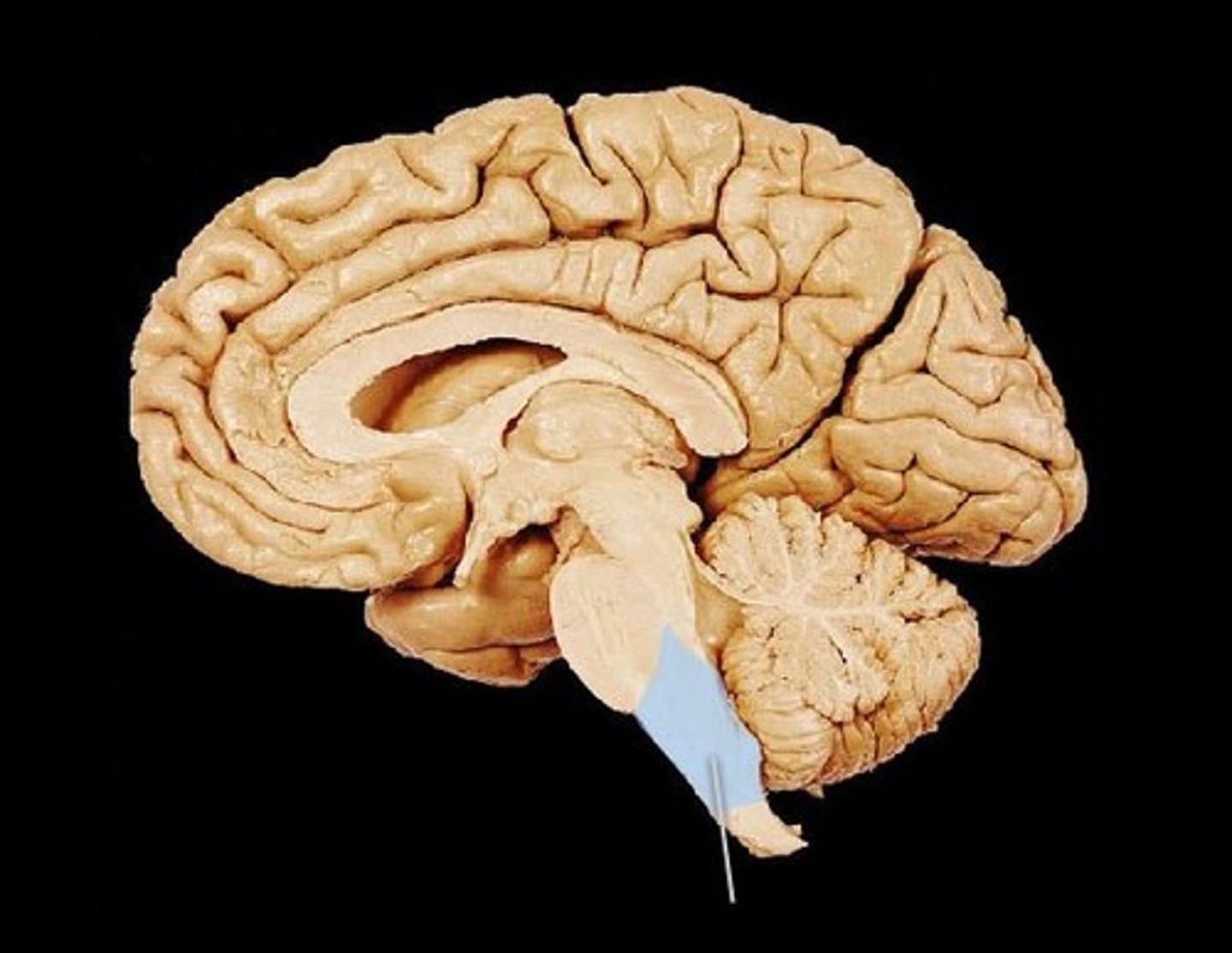
The glossopharyngeal nerve originates from the medulla oblongata in the brainstem.
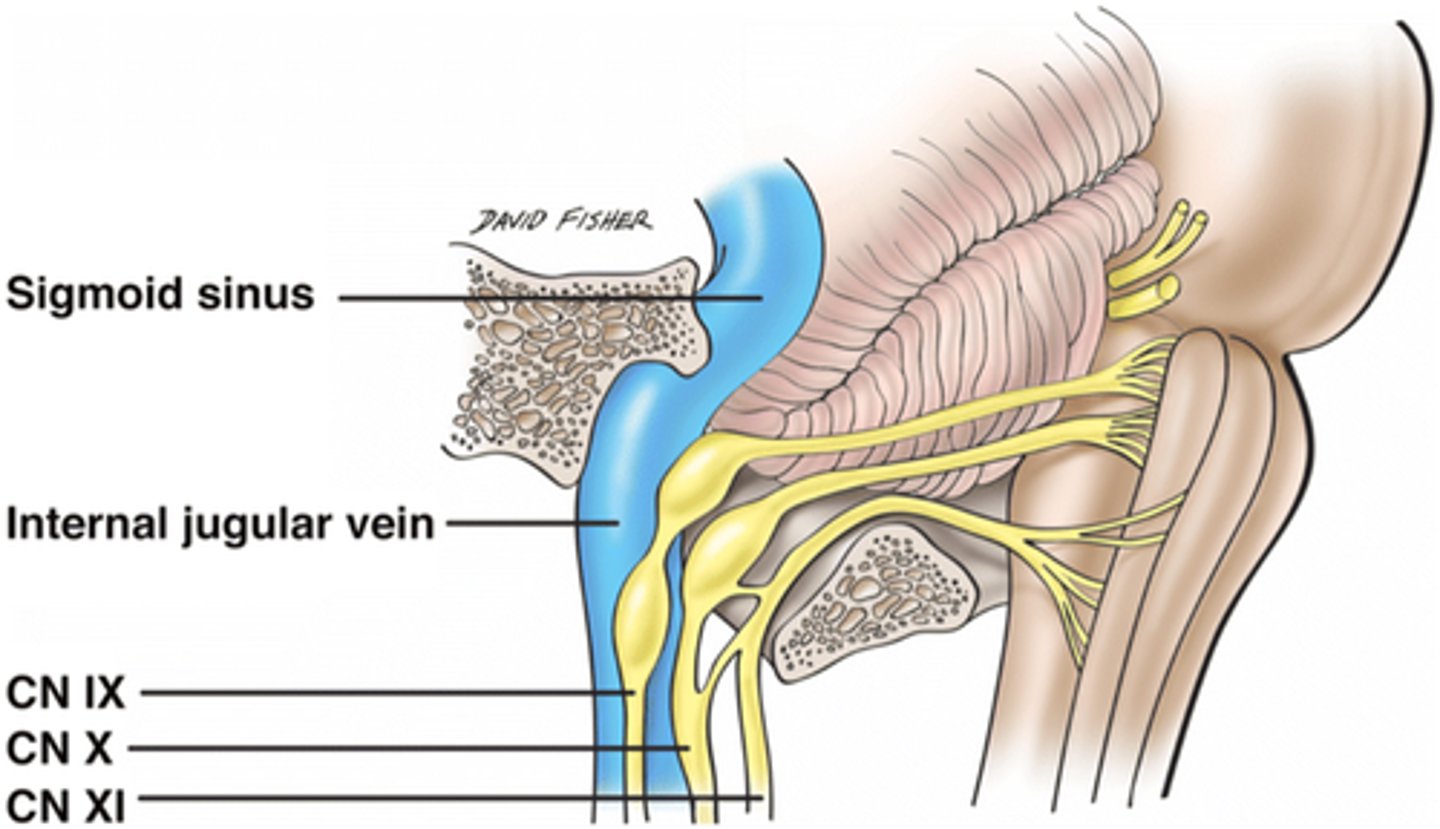
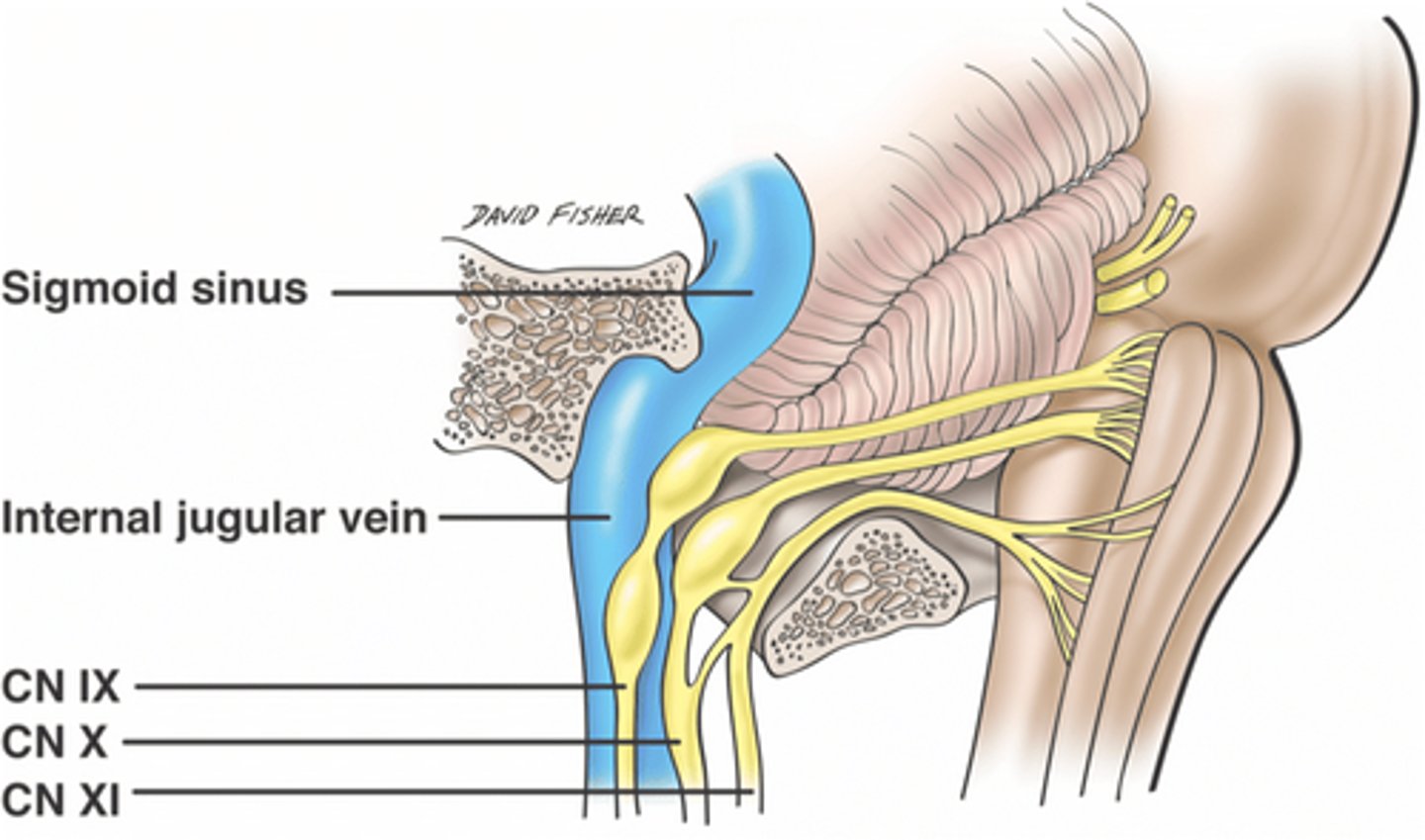
Through which foramen does the glossopharyngeal nerve exit the skull?
The glossopharyngeal nerve exits the skull through the jugular foramen.
Which muscles and nerves form the pharyngeal plexus?
The pharyngeal plexus is formed by contributions from the glossopharyngeal, vagus, and sympathetic nerves.
pharyngeal plexus:
1. glossopharyngeal
2. vagus
3. sympathetic
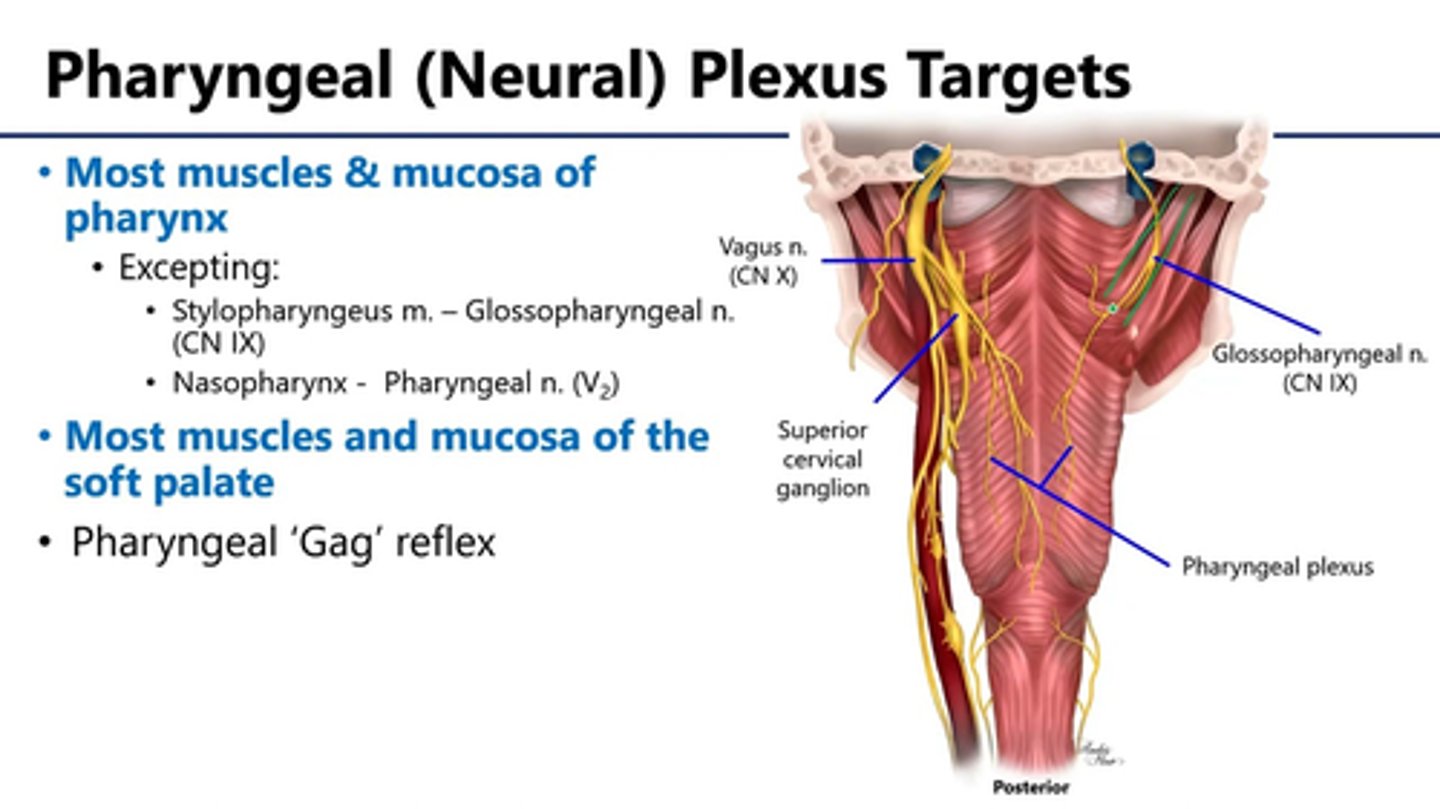
What is the role of the pharyngeal plexus?
The pharyngeal plexus innervates the muscles and mucosa of the pharynx, playing a crucial role in swallowing and sensation.
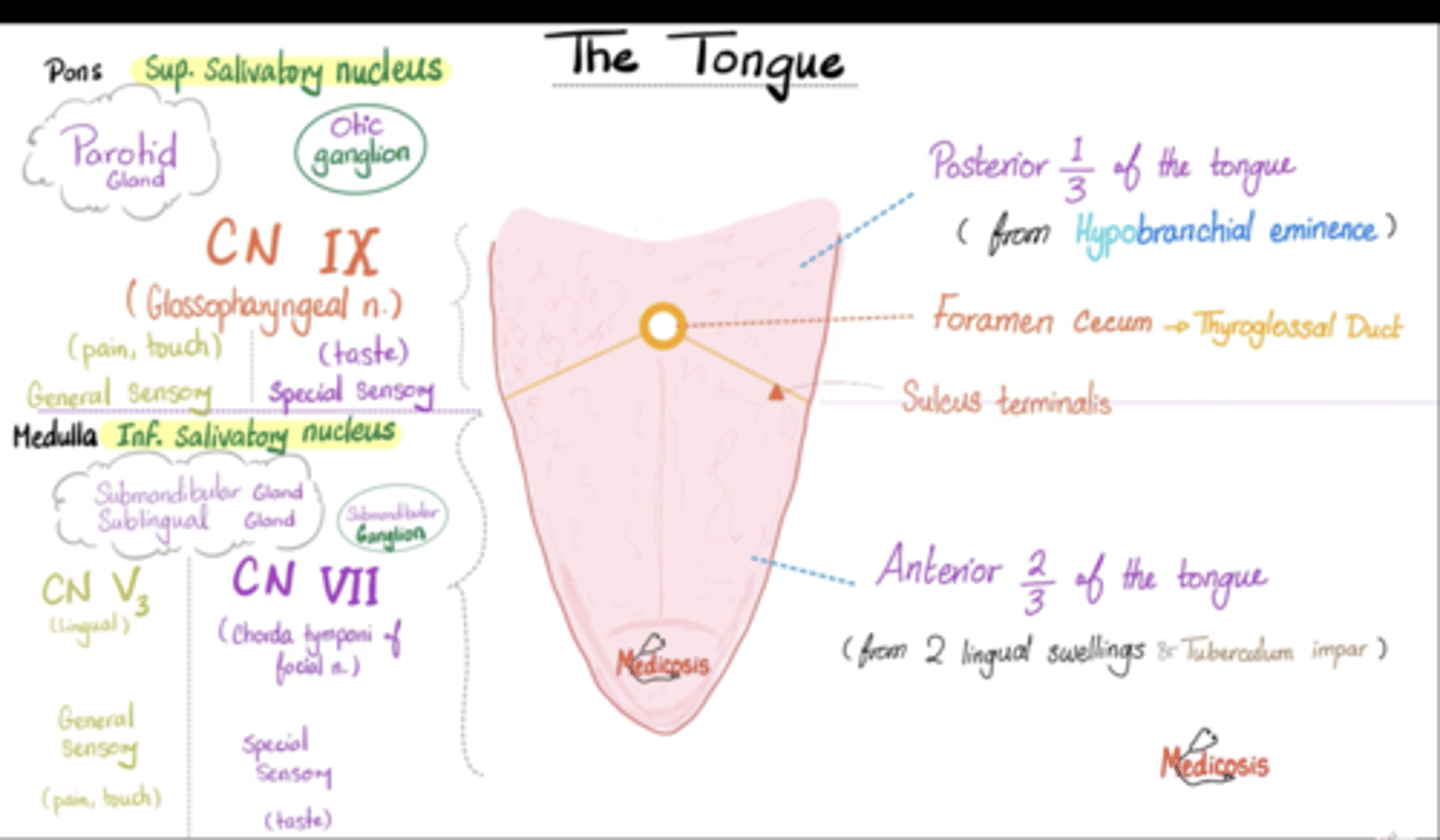
What sensations do the somatic afferent fibers from the posterior 1/3 of the tongue convey?
They convey general sensations like pain, temperature, and touch from the posterior third of the tongue.
posterior 1/3
CN IX glossopharyngeal
general sensory: (pain, touch)
special sensory: (taste)
anterior 1/3
CN V trigeminal
general sensory: (pain, touch)
CN XII hypoglossal
special sensory: (taste)
To which gland do the visceral efferent (parasympathetic) fibers of the glossopharyngeal nerve travel?
They travel to the parotid gland, stimulating saliva production.
great auricular nerve innervates the skin over the parotid gland but THE GLOSSOPHARYNGEAL NERVE PARASYMPATHETICALLY INNERVATES THE PAROTID GLAND
reminder 1973- glossopharyngeal: 9
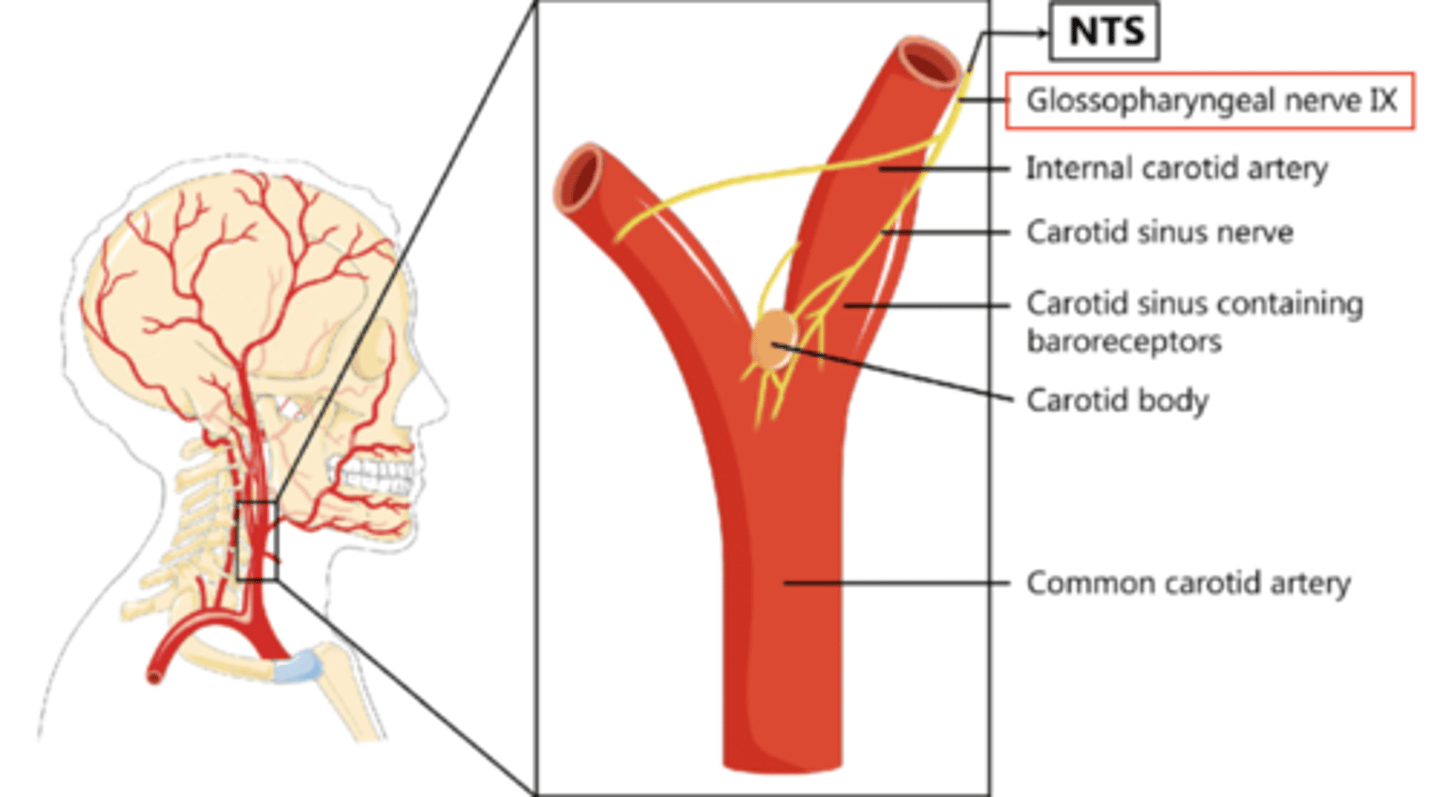
What type of information do the visceral afferent fibers from the carotid body and sinus carry?
They carry information related to blood pressure and oxygen levels.
REMEMBER- the solitary nucleus contains visceral sensory (afferent) info:
1. carotid body chemoreceptors
2. carotid sinus baroreceptors
3. taste- taste buds located on the posterior 1/3 of tongue
Apart from the carotid body and sinus the visceral afferent fibers of the glossopharyngeal nerve also convey sensory information to?
TASTE- TASTE BUDS LOCATED ON THE POSTERIOR 1/3 OF TONGUE
They convey sensory information from the tonsils.
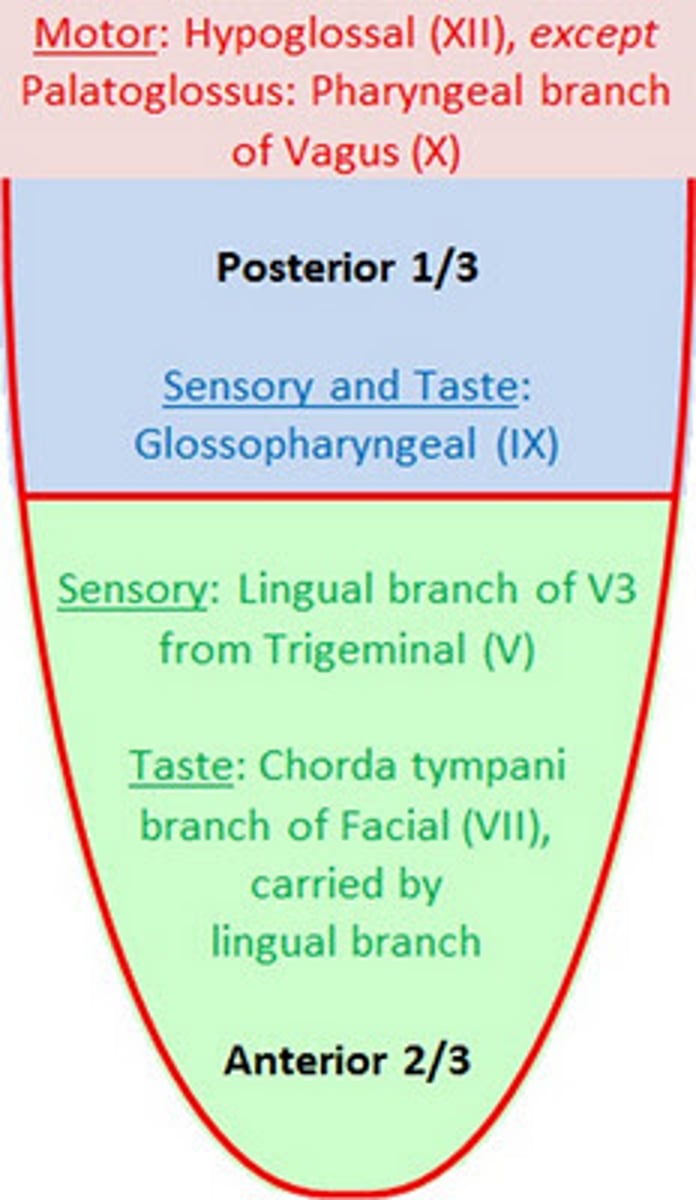
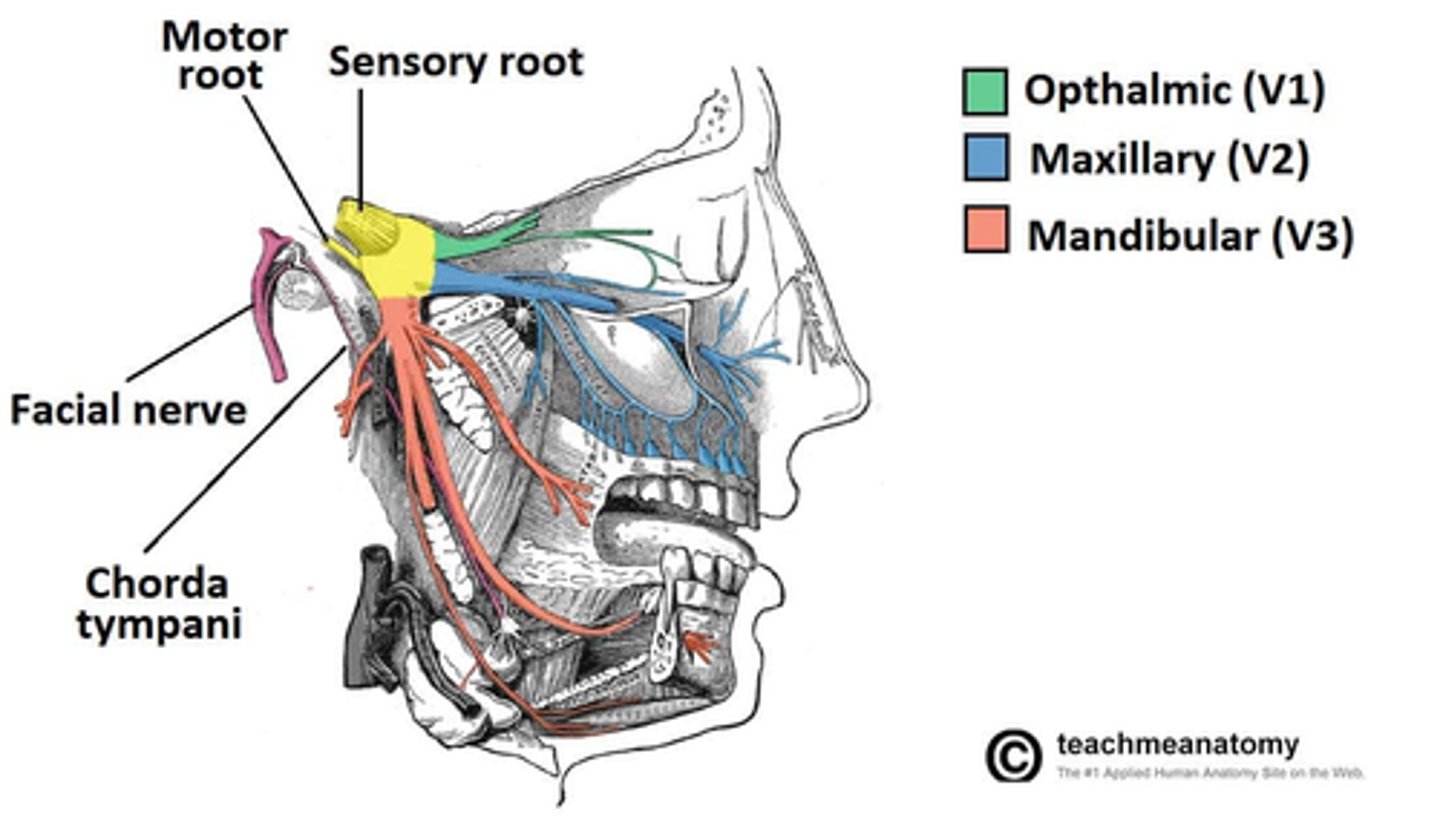
Which portion of the tongue's taste sensation is not served by the glossopharyngeal nerve?
The anterior 2/3 of tongue's taste sensation is served by the facial nerve (VII CN), not by the glossopharyngeal nerve.
Taste (special sensory): CN VII, facial nerve
General sensory: CN V, trigeminal nerve
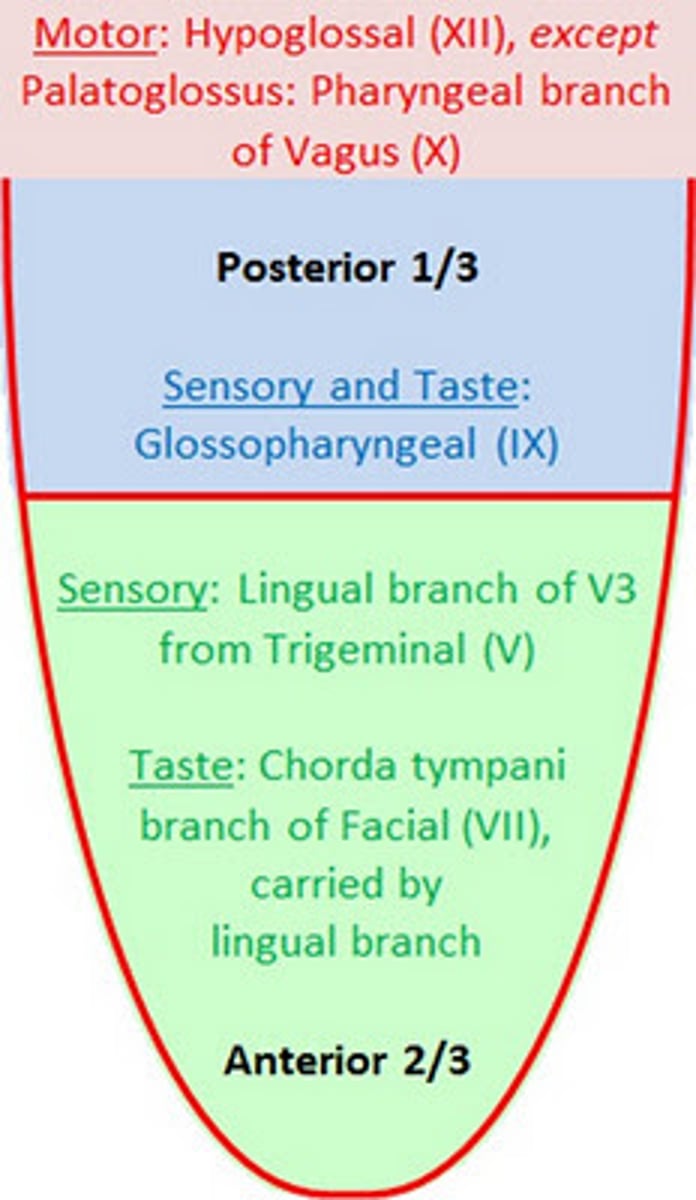
Which papillae on the tongue do the special visceral afferents from the glossopharyngeal nerve gather taste information from?
They gather taste information from the foliate and vallate papillae.
types of papillae:
1. foliate
2. vallate
What is the clinical significance of damage to the glossopharyngeal nerve?
1. Loss of taste sensation from the (1/3) posterior tongue
2. Dysphagia, impairing swallowing reflexes.
3. Loss of gag reflex (diminishes or disappears)
4. Salivation alters (reduced production by parotid gland) impaired parasympathetic fibers
5. Damage to cardiovascular reflexes, BP/ O2... disregulation
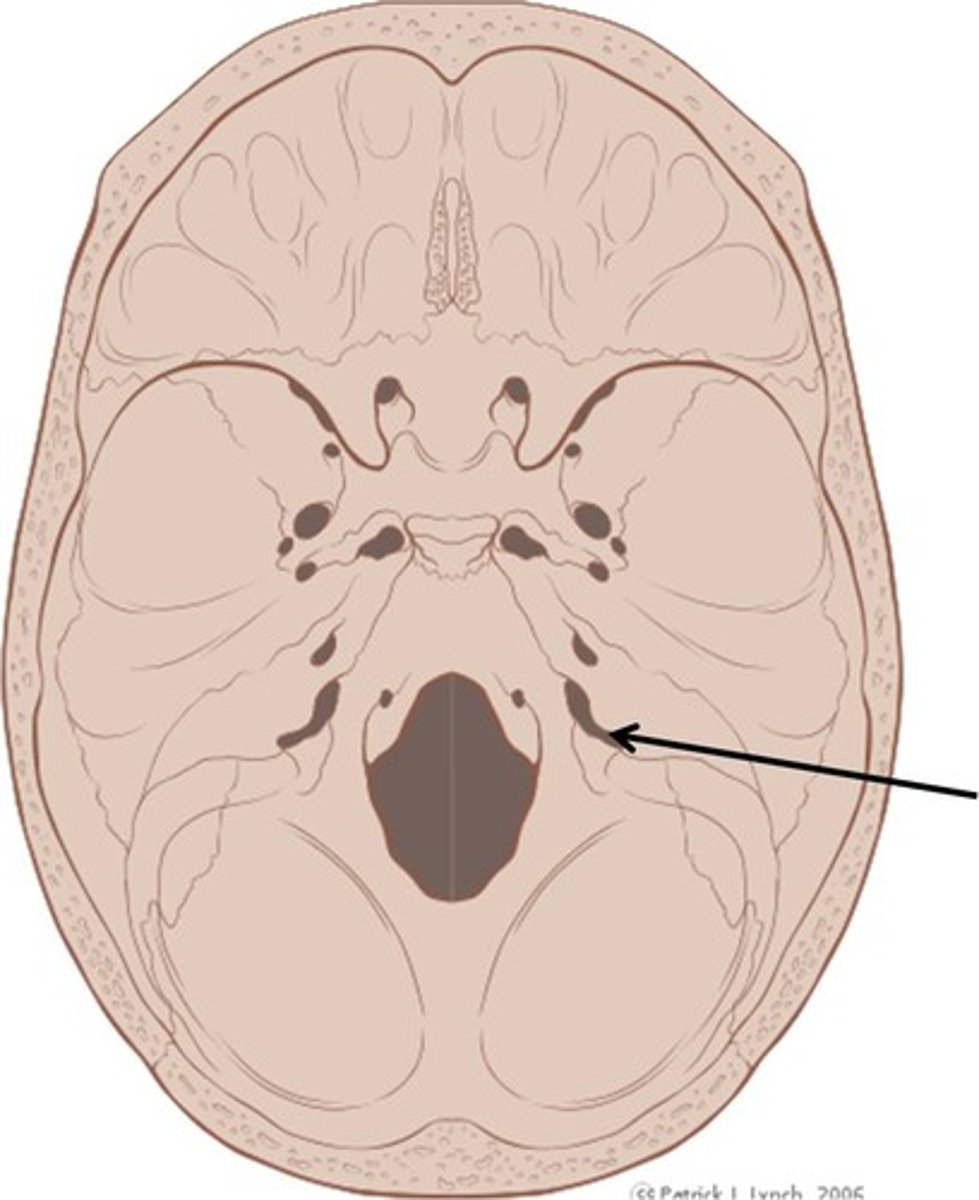
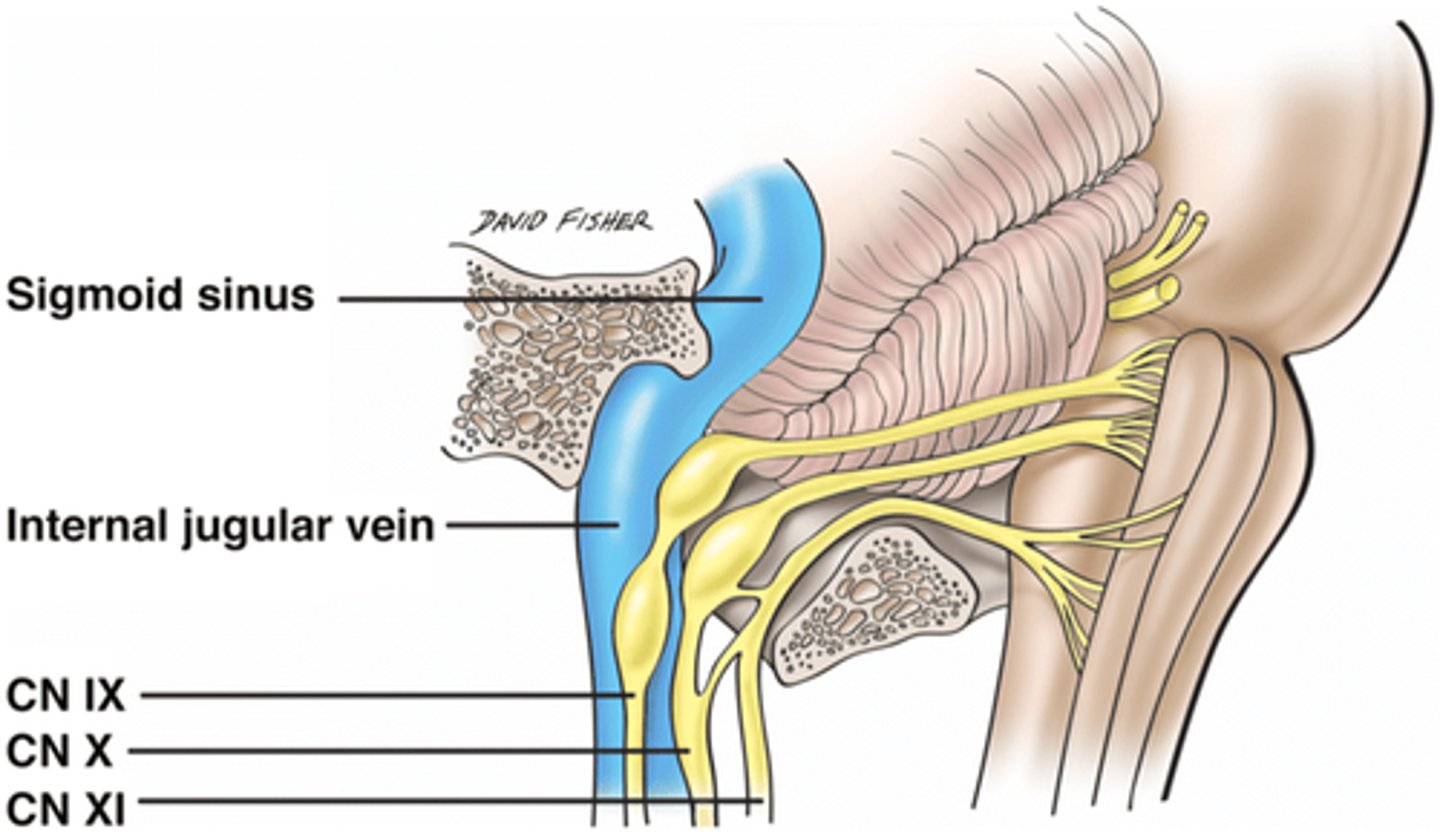
Which cranial nerves share the jugular foramen with the glossopharyngeal nerve?
Nerves that pass through the jugular foramen:
1. vagus nerve
2. accessory nerve
3. glossopharyngeal nerve
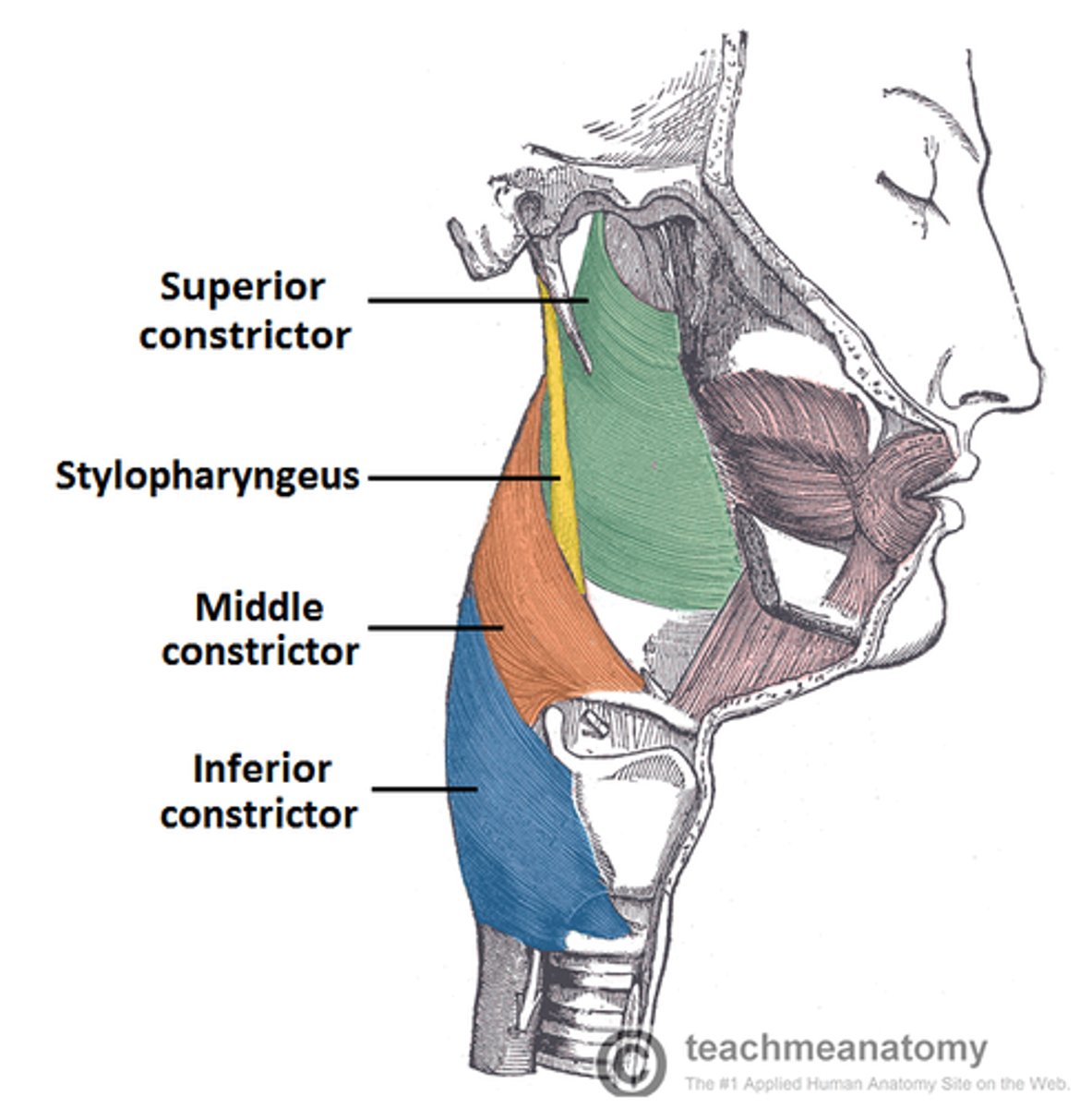
What type of fibers innervate the stylopharyngeus muscle?
CN IX
Somatic efferent fibers from the glossopharyngeal nerve innervate the stylopharyngeus muscle.
What is the primary function of the stylopharyngeus muscle?
It elevates the pharynx during swallowing and speaking.
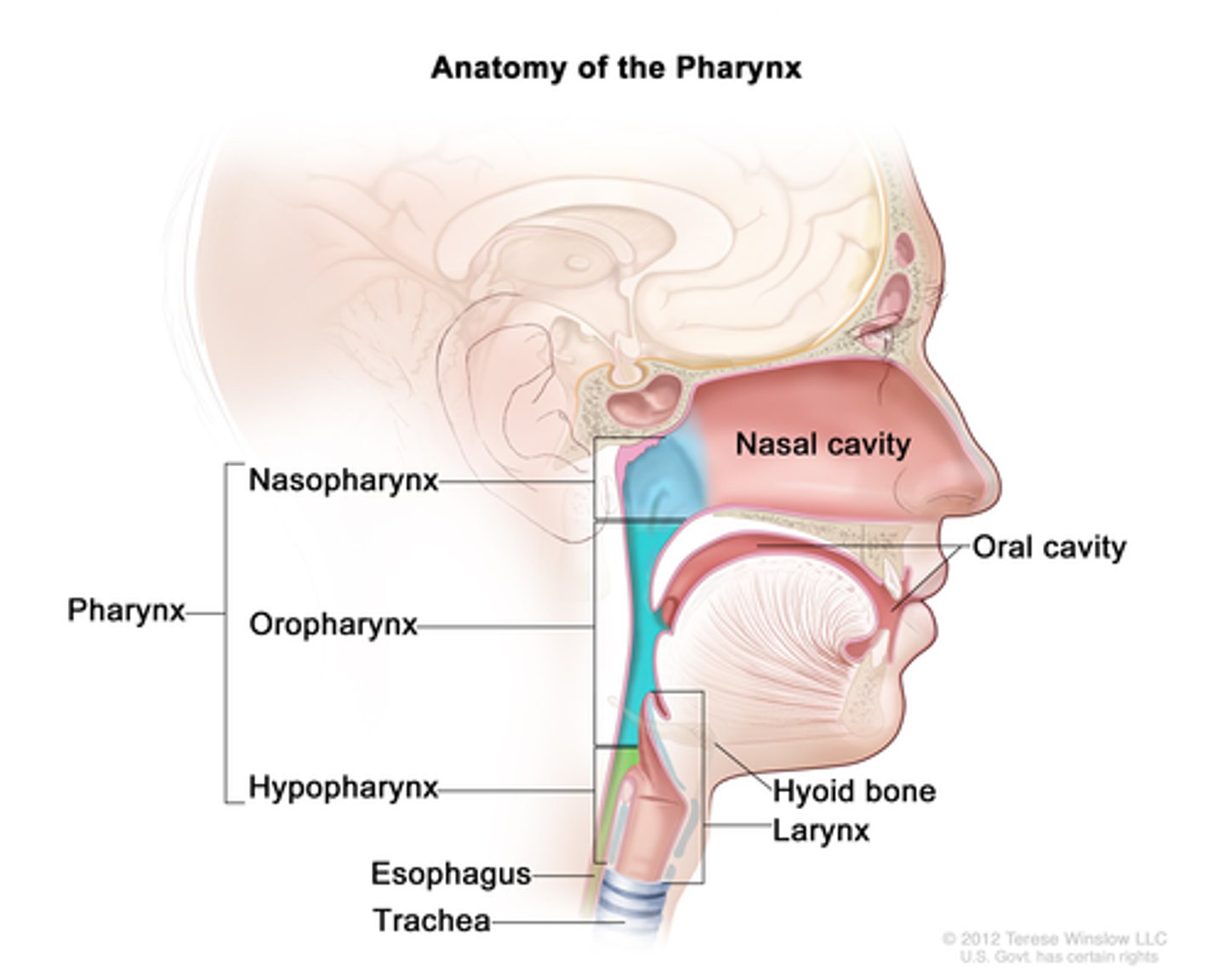
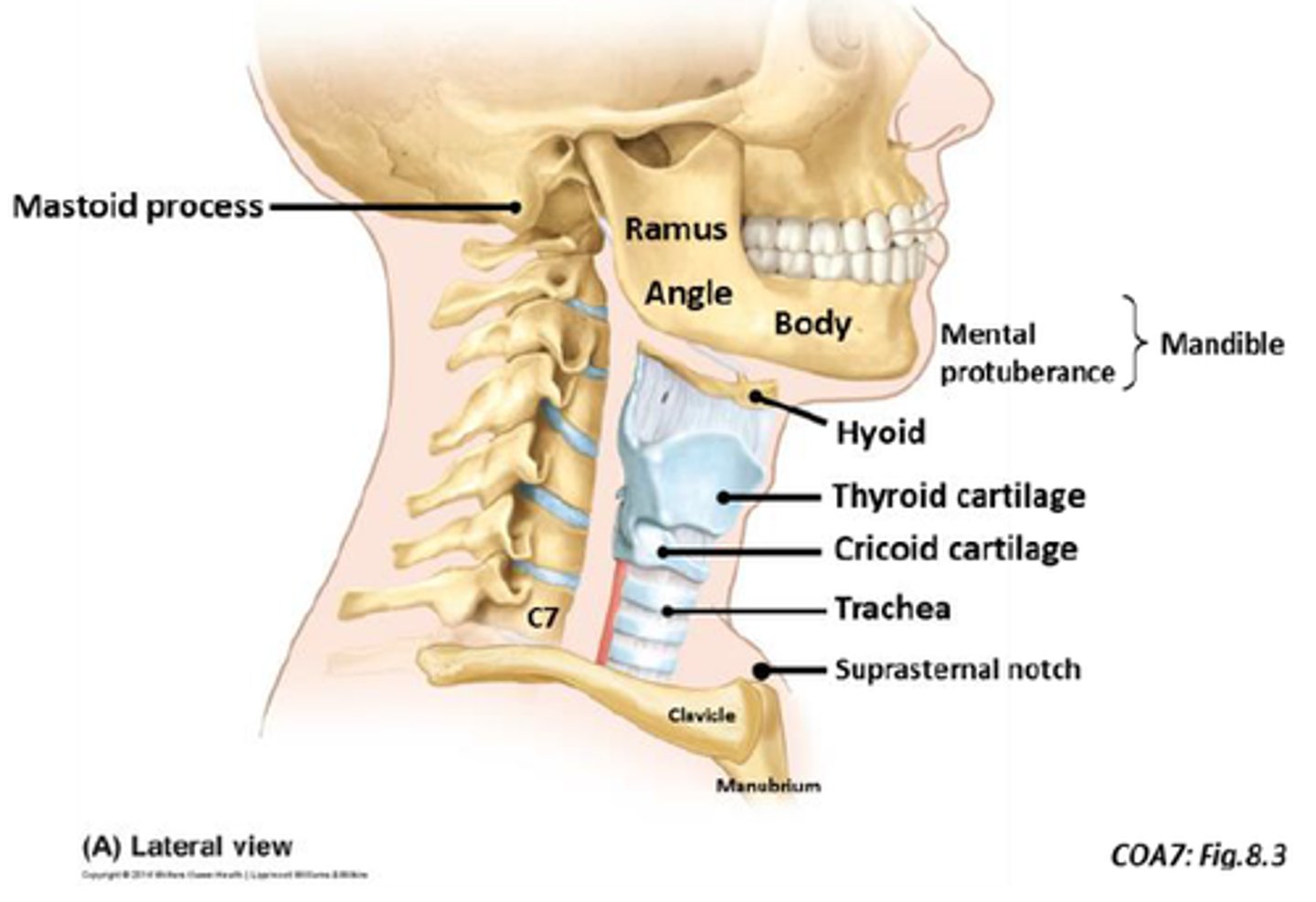
Where is the pharynx located?
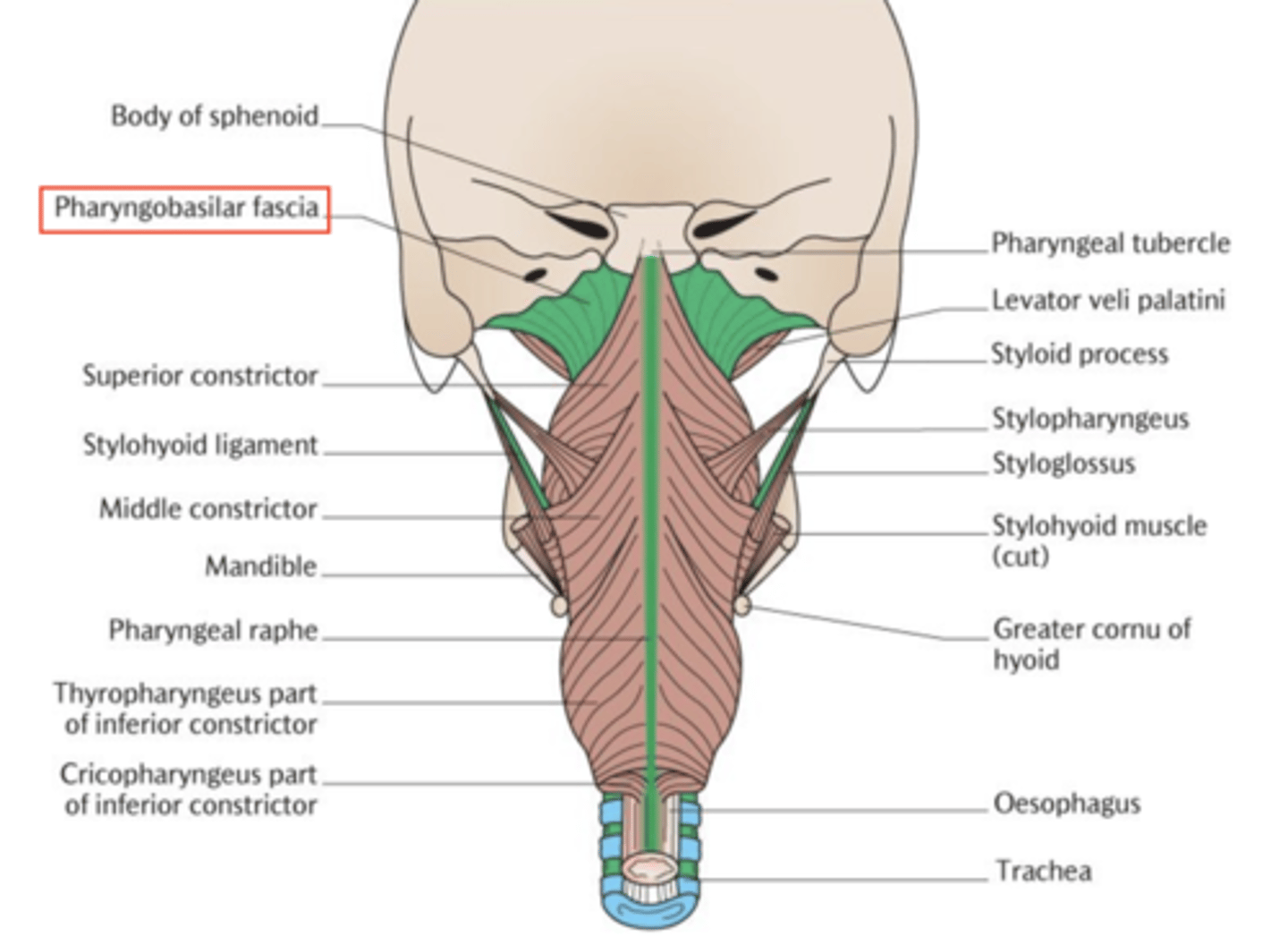
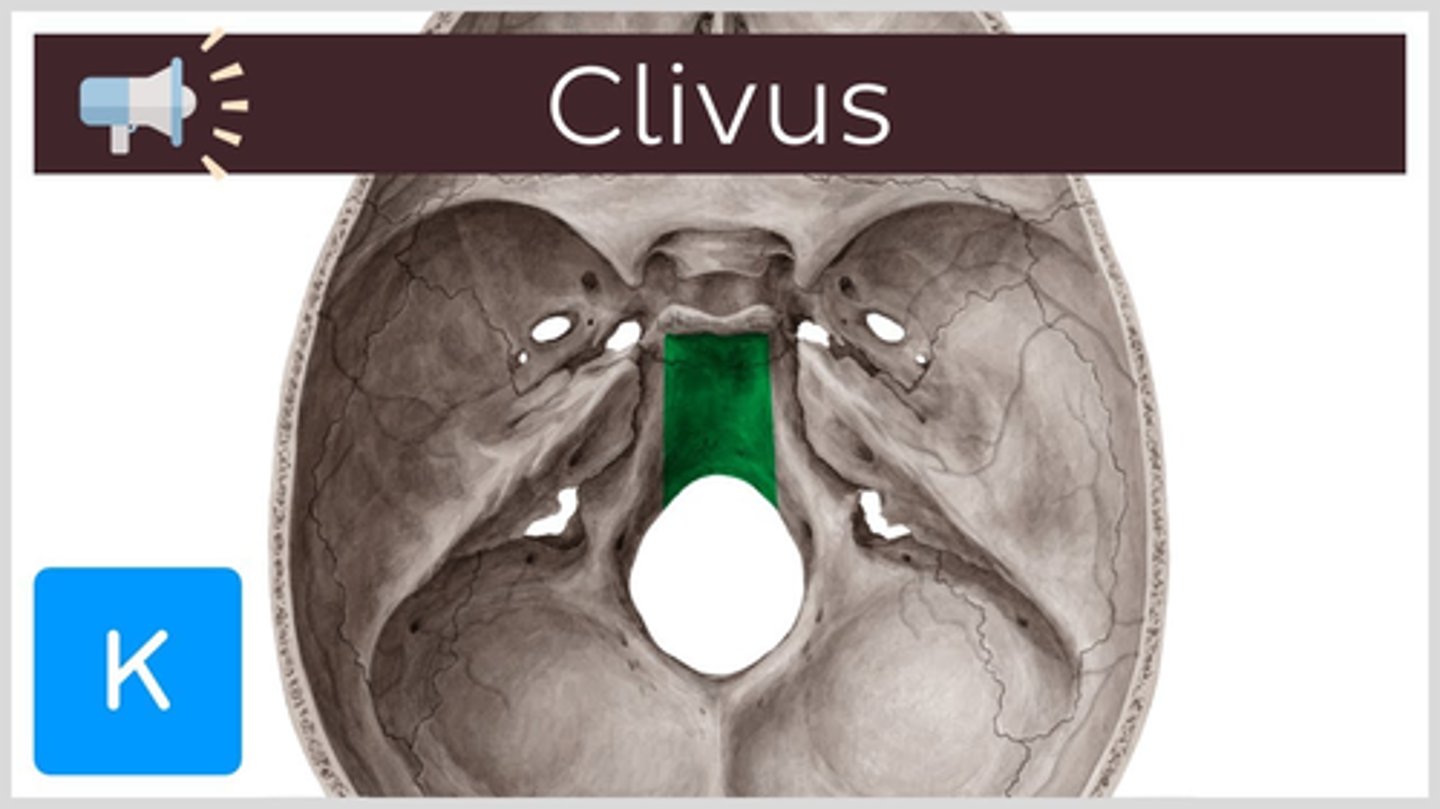
The pharynx extends from the base of the skull (clivus) to approximately the inferior border of the C6 vertebra.
top: base of skull (clivus)
bottom: inferior border of C6 vertebra
What bony structures is the anterior part of the pharynx attached to?
Anteriorly, the pharynx is attached to the cranium, mandible, and hyoid bone.
1. cranium
2. mandible
3. hyoid bone
, thyroid cartilage and cricoid cartilage
What is the middle pharyngeal raphe?
It's a fibrous seam where the bilateral muscles of the pharynx join posteriorly, providing a central point of muscle attachment.
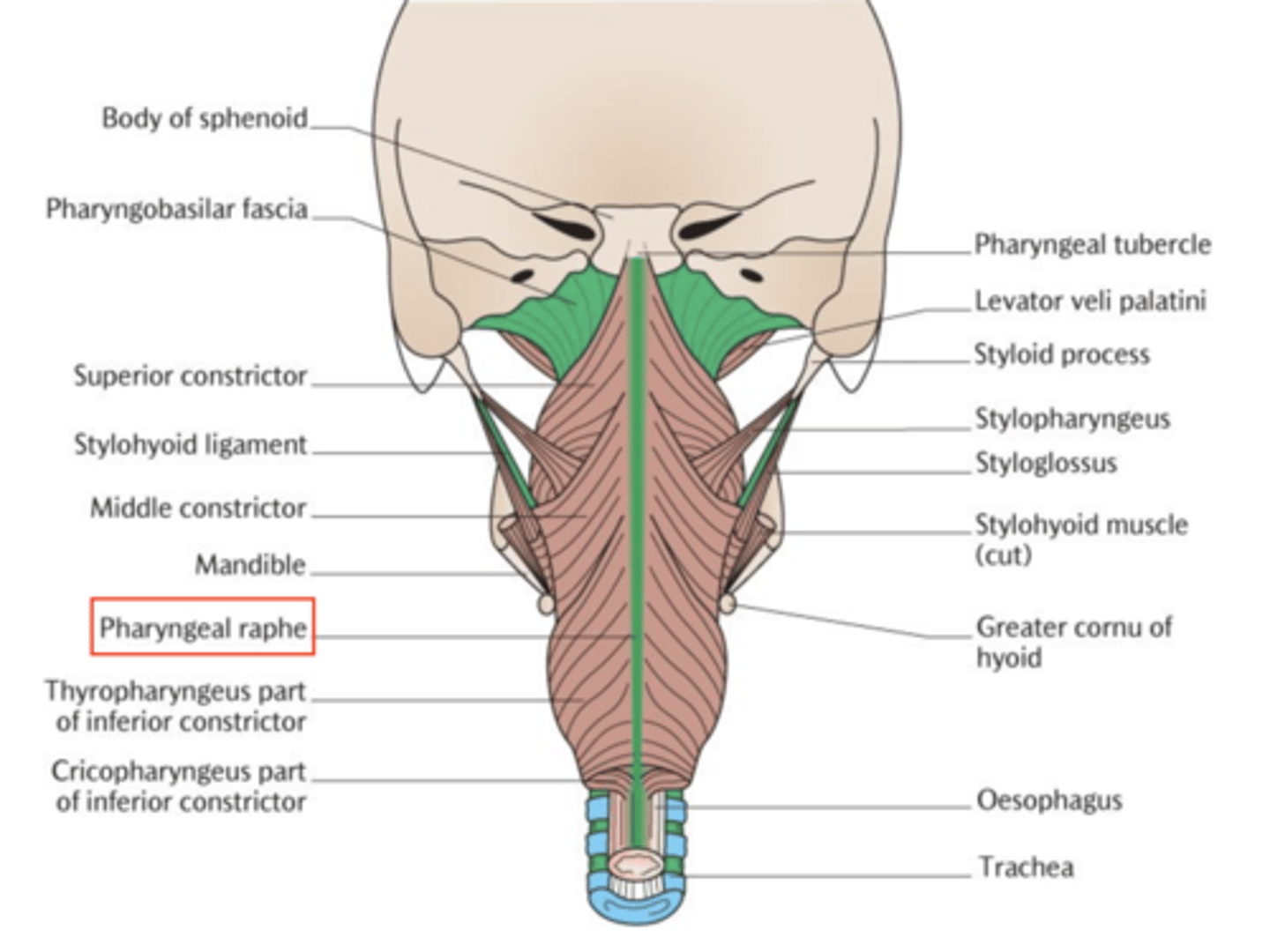
Why are there no muscles in the uppermost part of the pharynx?
This region only contains the pharyngobasilar fascia attaching to the skull, which is sufficient for its function at that level.
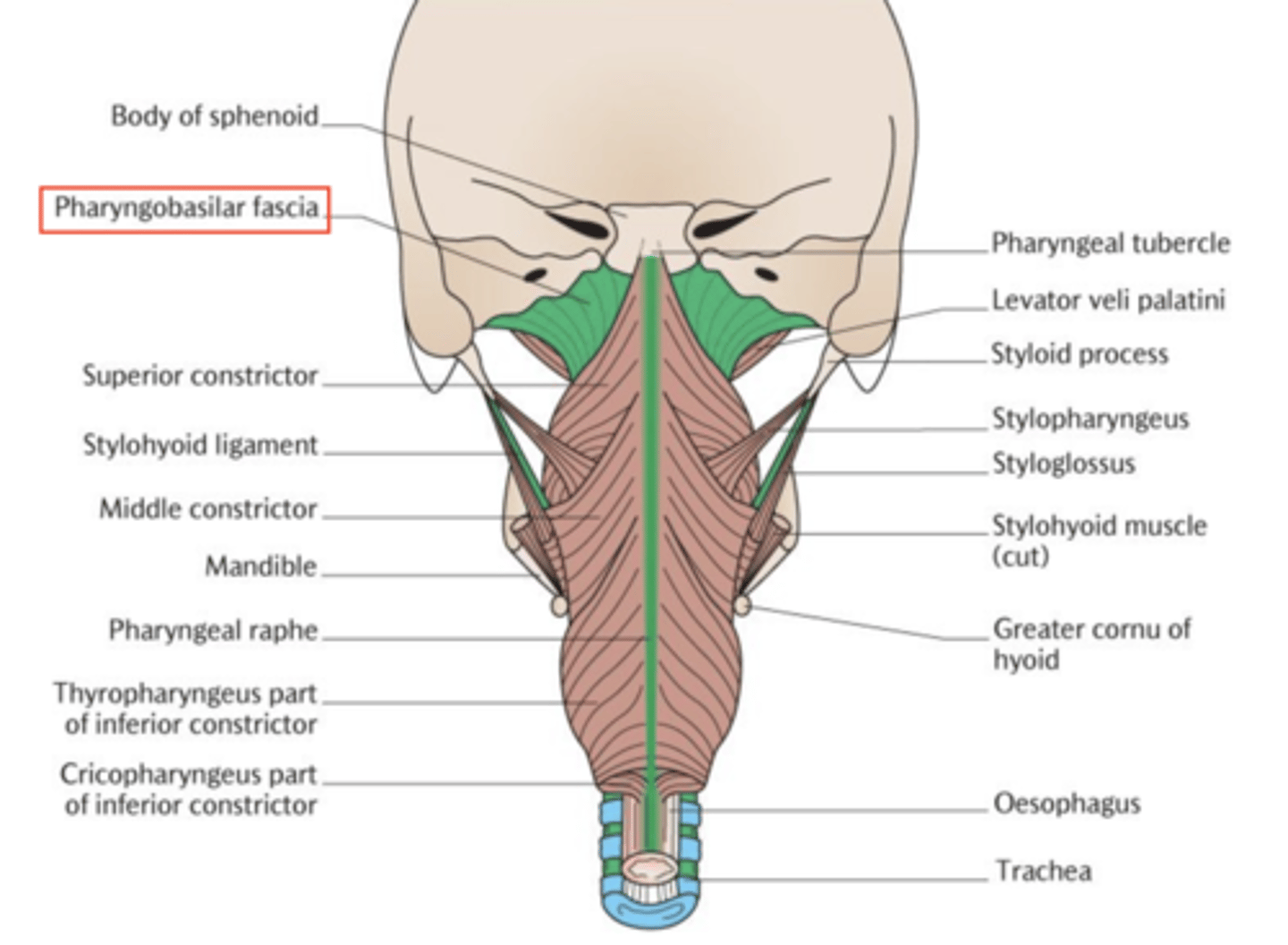
What is the pharyngobasilar fascia?
It's a sheet of connective tissue separating the muscular layer from the mucosal lining of the pharynx.
SEPARATES MUSCULAR LAYER BOTTOM FROM MUCOSAL LINING TOP (CLIVUS)
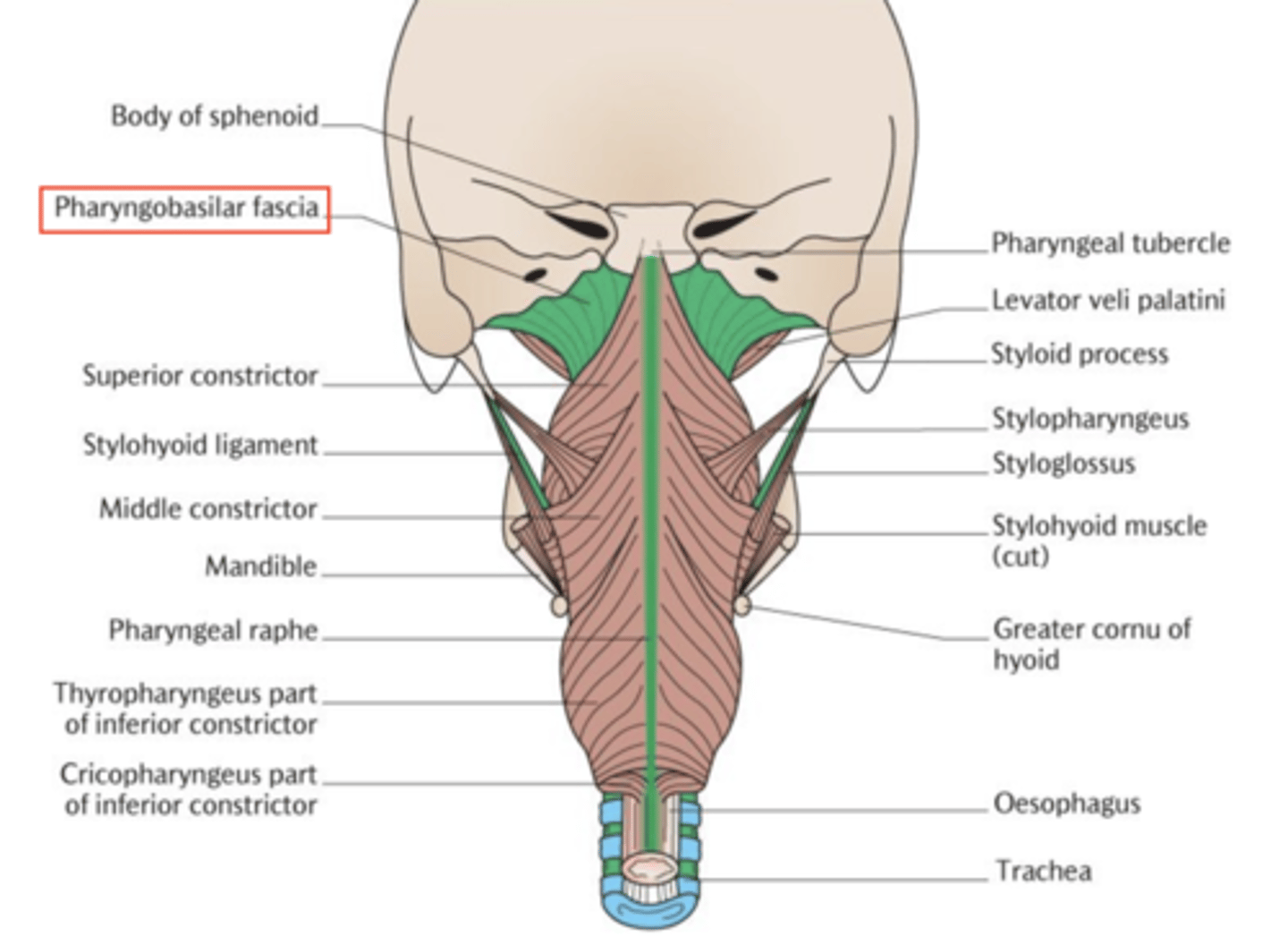
What separates the pharyngeal muscular layer from the mucosal lining?
The pharyngobasilar fascia.
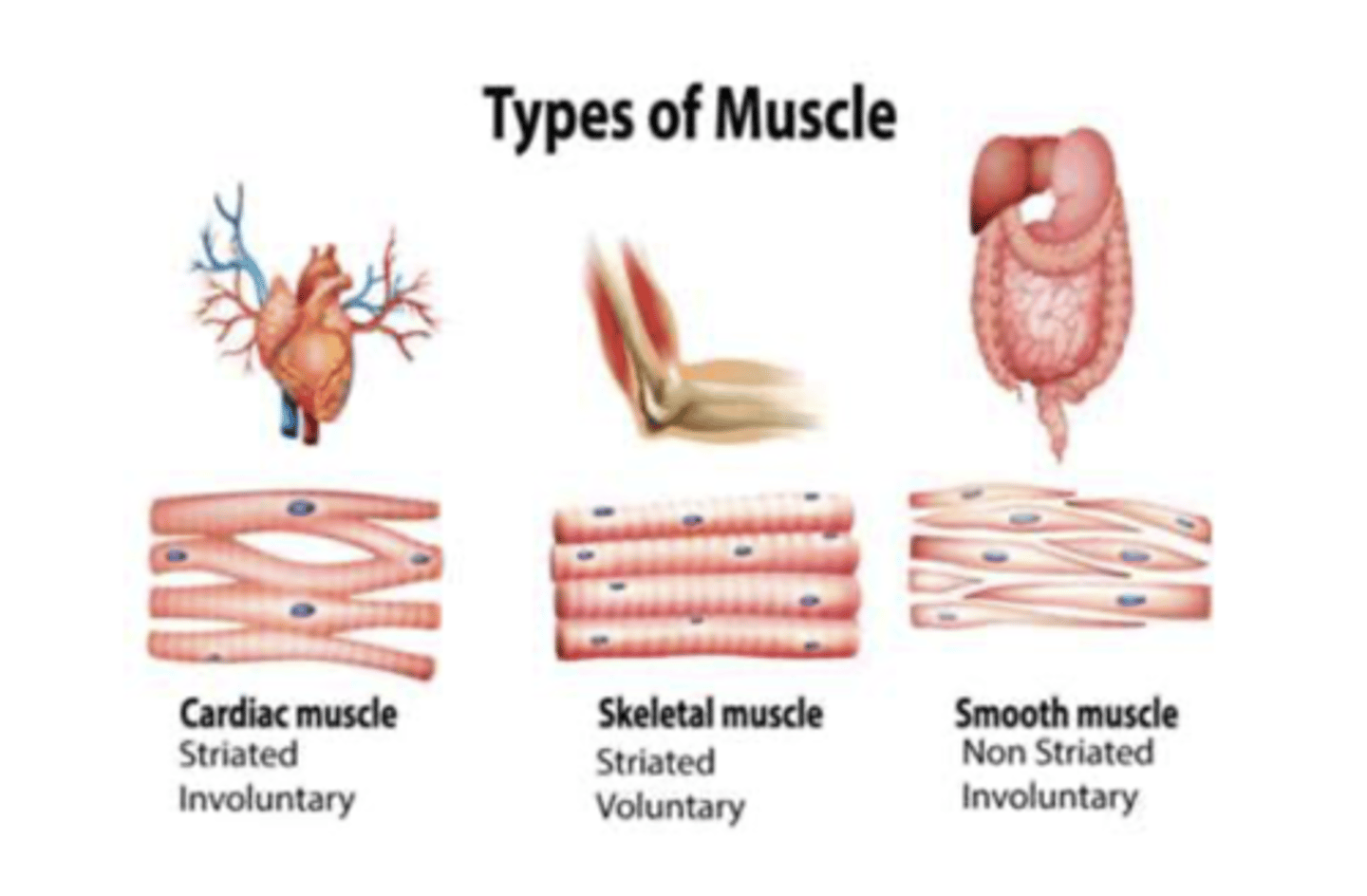
How does the pharynx's structure differ from the rest of the GI tract?
The pharynx contains striated (skeletal) muscles for voluntary control, unlike the smooth muscles found in the rest of GI tract.
VOLUNTARY CONTROL: STRIATED MUSCLE
INVOLUNTARY CONTROL: SMOOTH MUSCLE
Describe the mobility of the pharynx.
posterior: free and mobile
anteriorly: anchored to bony structures
Its mobility facilitates expansive and contractile movements during swallowing.

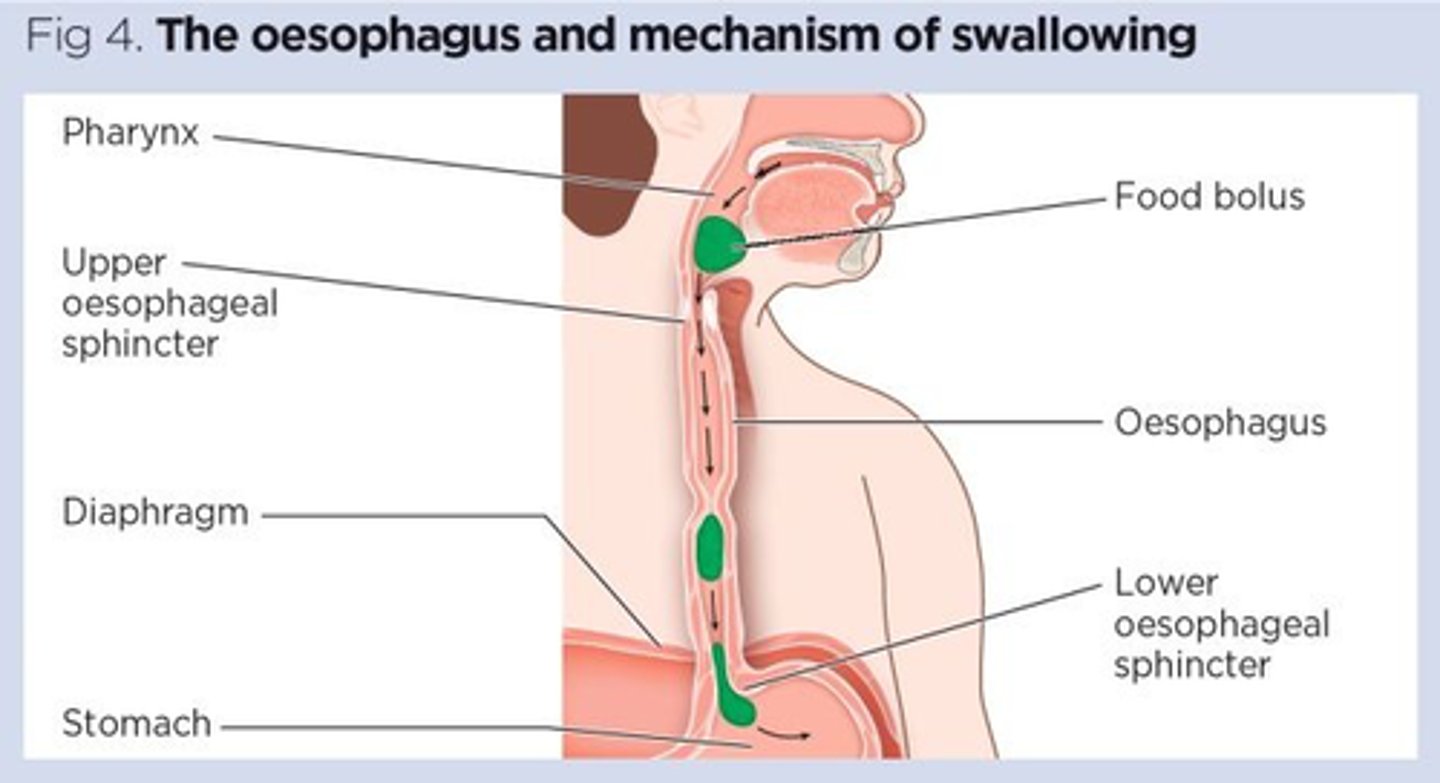
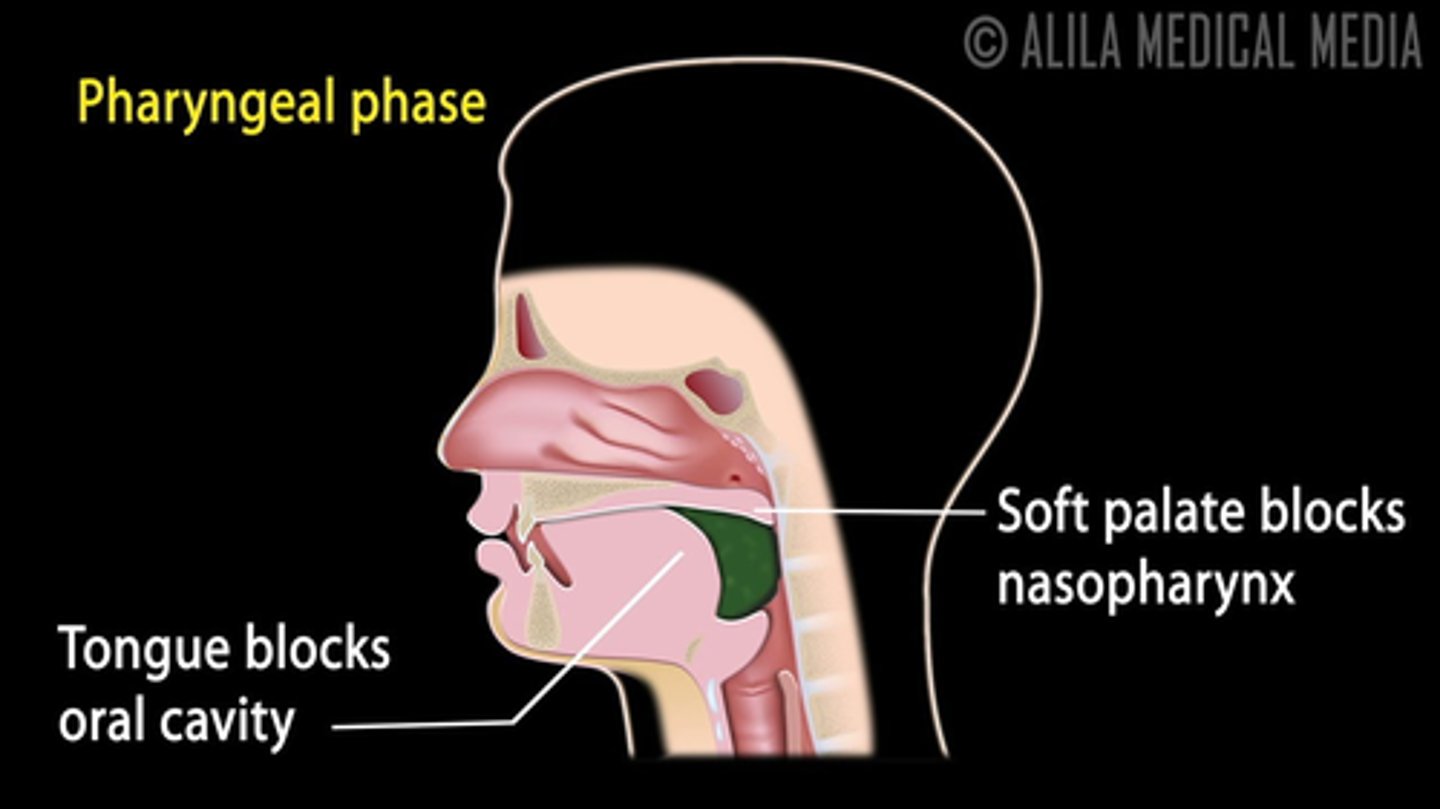
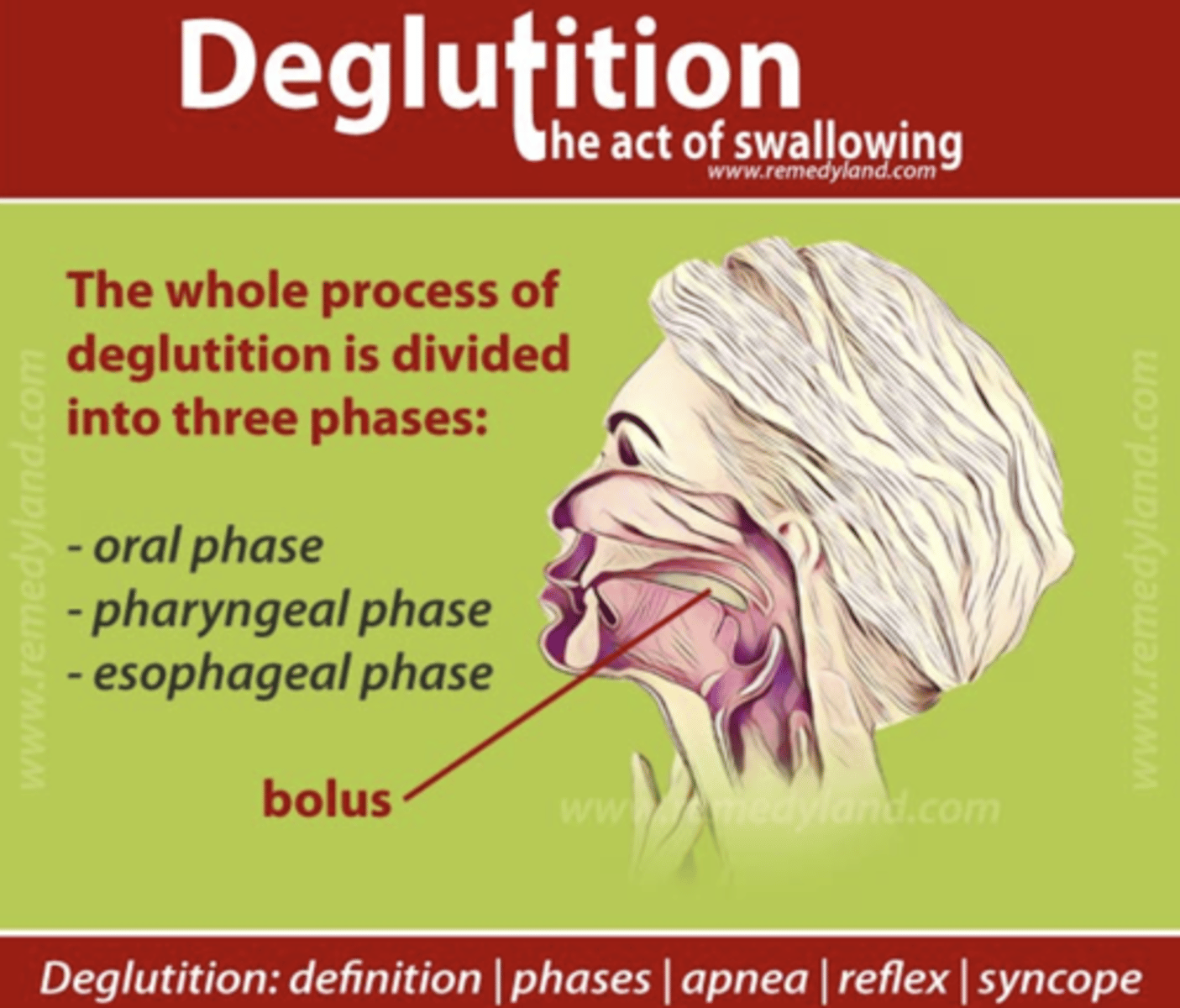
What happens in the pharynx during the act of swallowing (pharyngeal constrictor muscles)?
The pharyngeal muscles contract to move the food bolus mouth -> oesophagus
the initial phase of swallowing, which involves the voluntary contraction of pharyngeal muscles to propel the bolus into the esophagus, is known as the oral or voluntary phase.
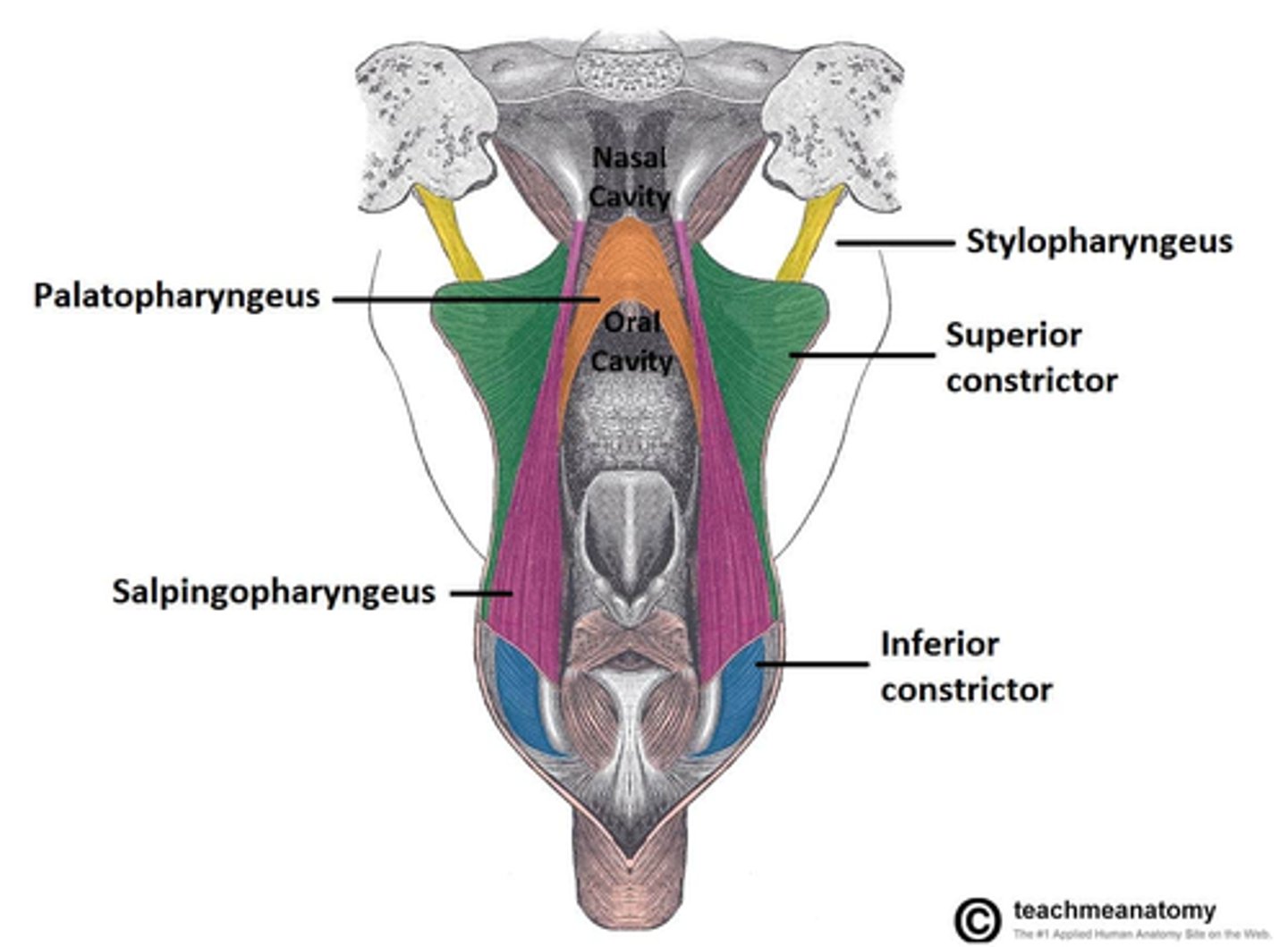
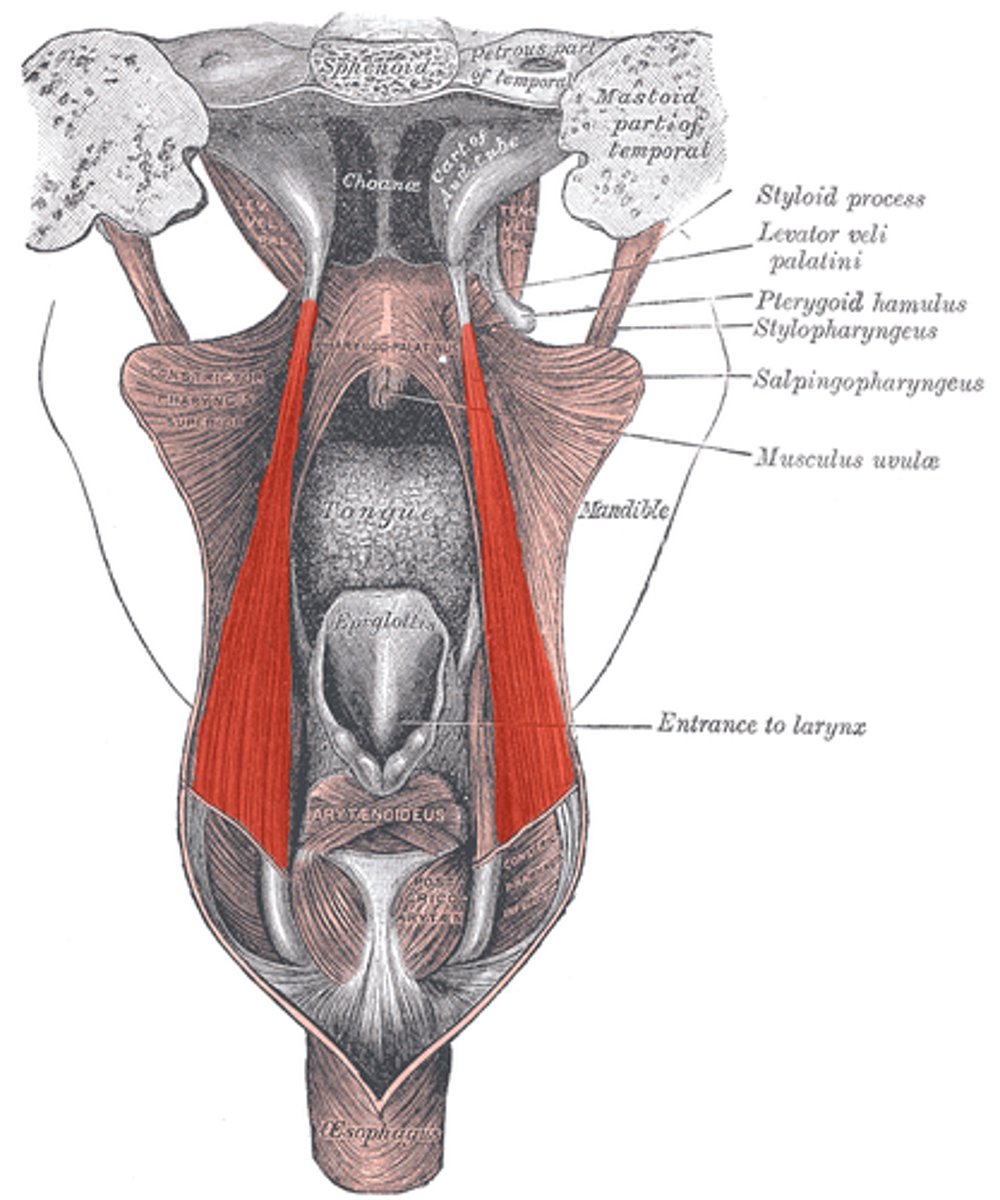
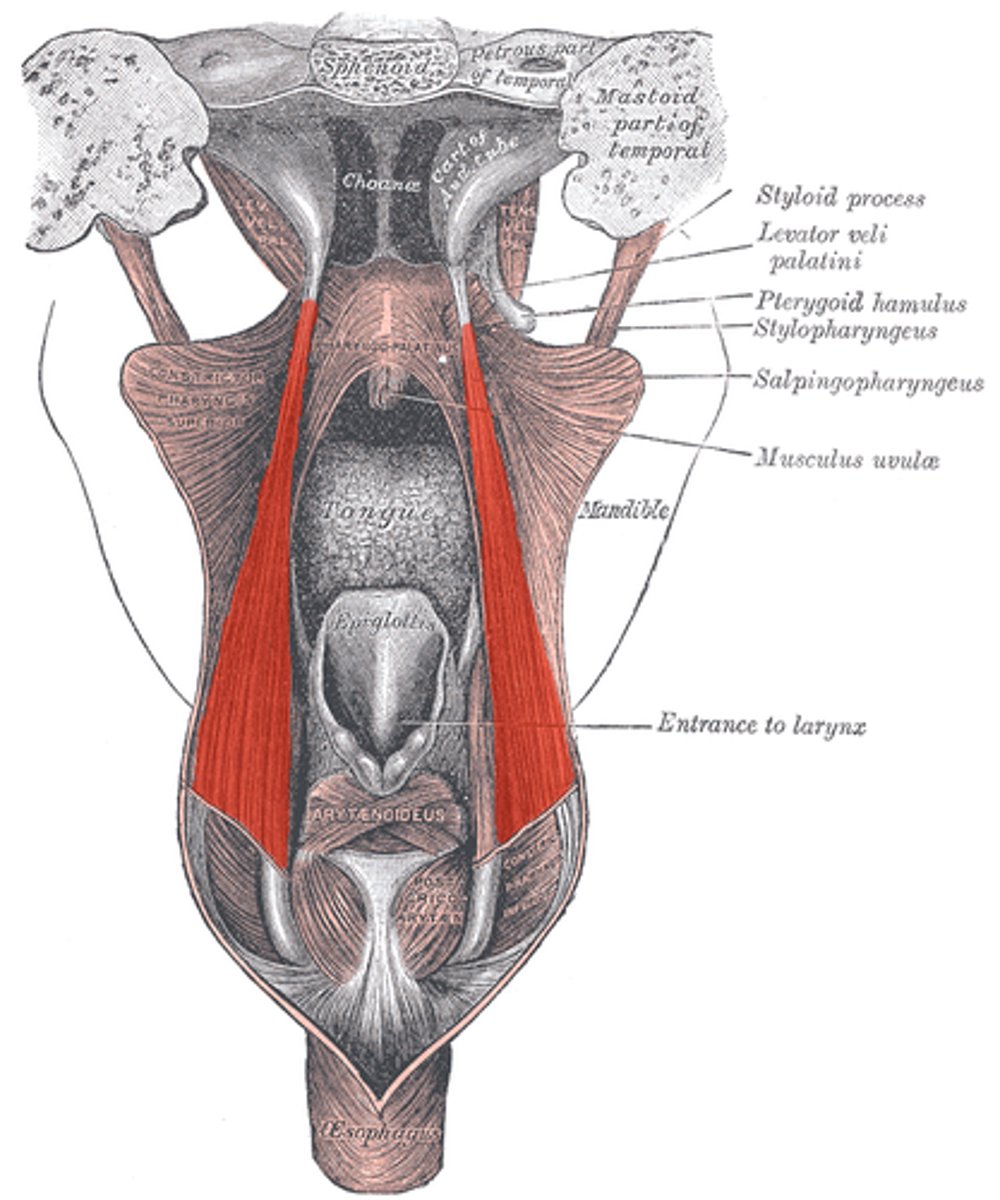
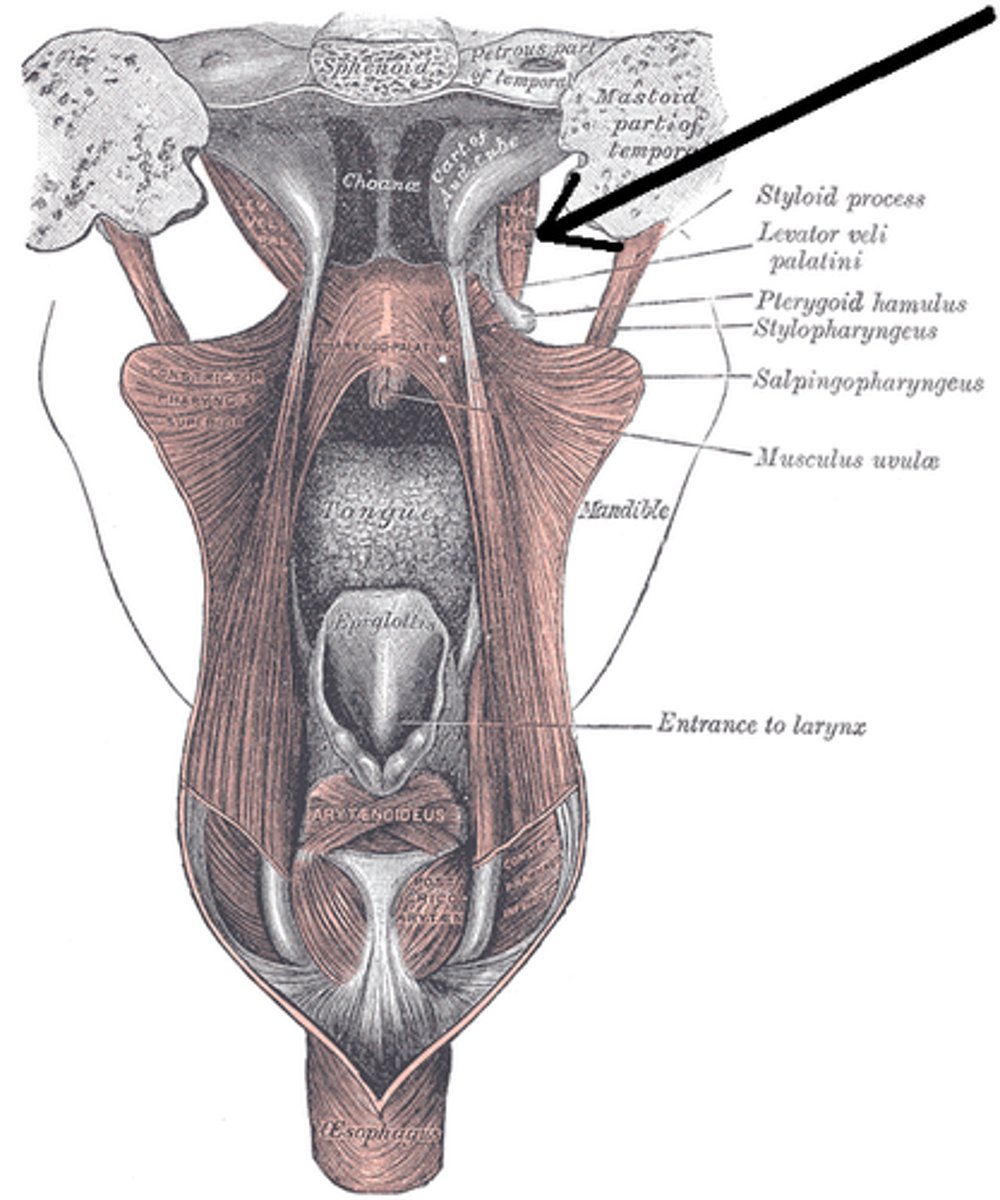
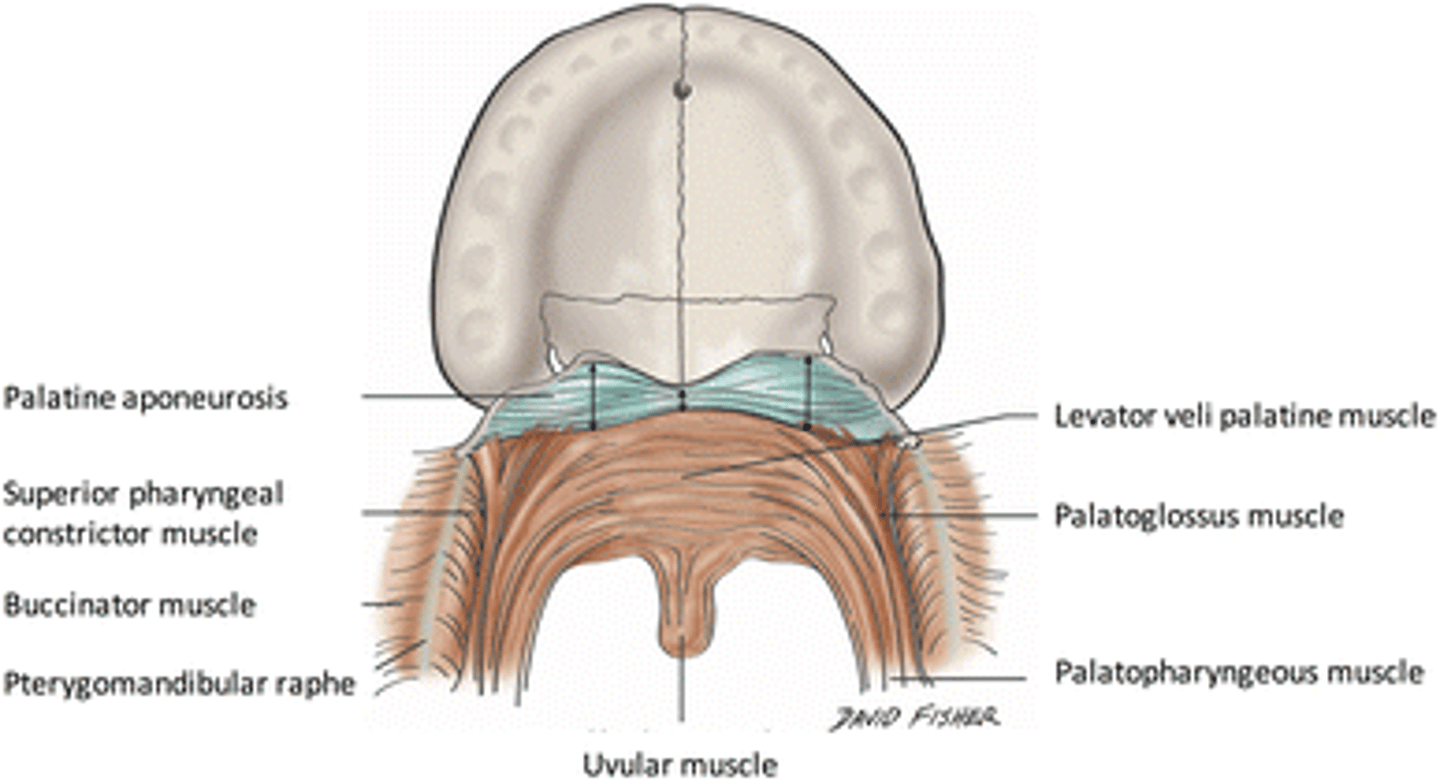
What are the two groups of pharyngeal muscles?
The pharyngeal muscles are categorized into circular and longitudinal layers.
1. circular
2. longitudinal
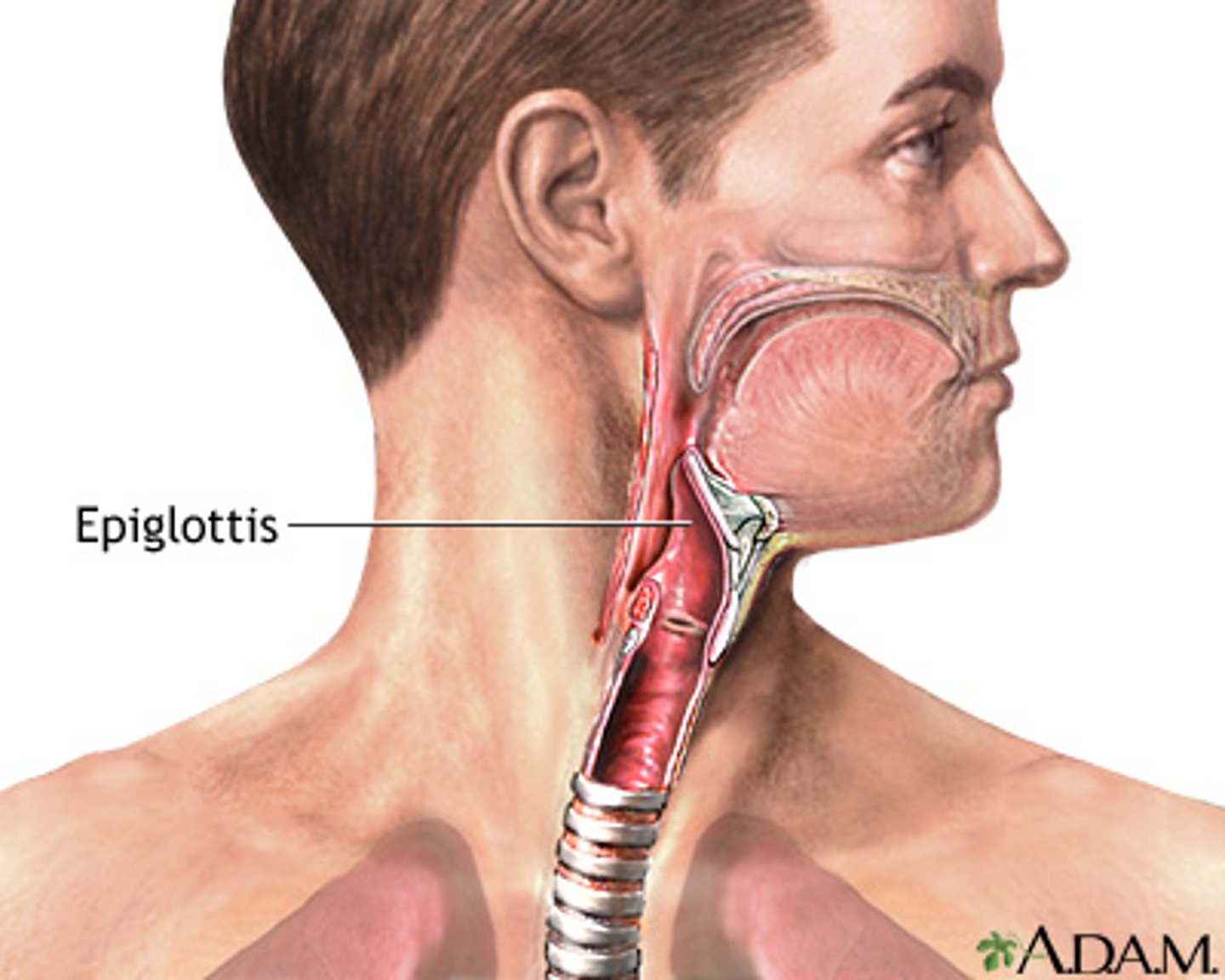
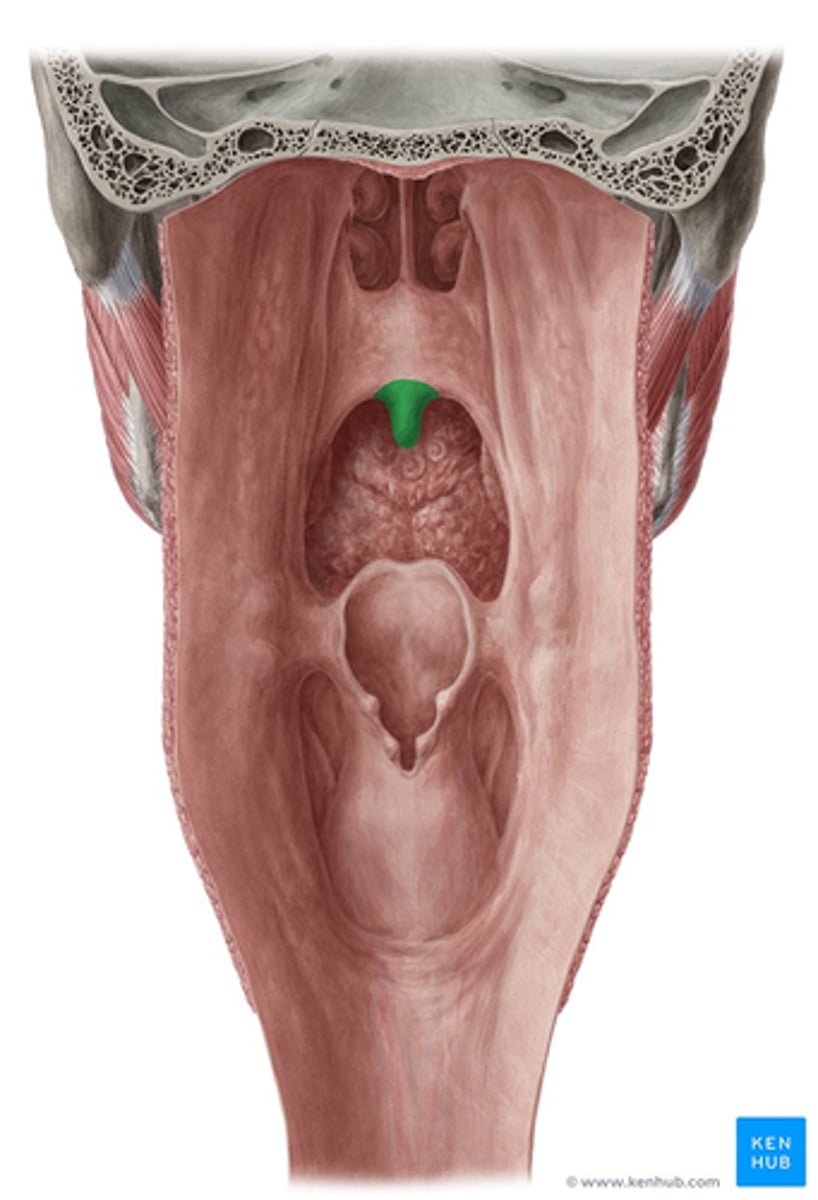
What role does the epiglottis play in the pharynx's function?
The epiglottis prevents food from entering the airway during swallowing.
What is the clivus?
A bony structure formed by the basilar part of the occipital bone and the sphenoid bone: where the pharynx begins.
BASILAR PART OF OCCIPITAL, SPHENOID BONE
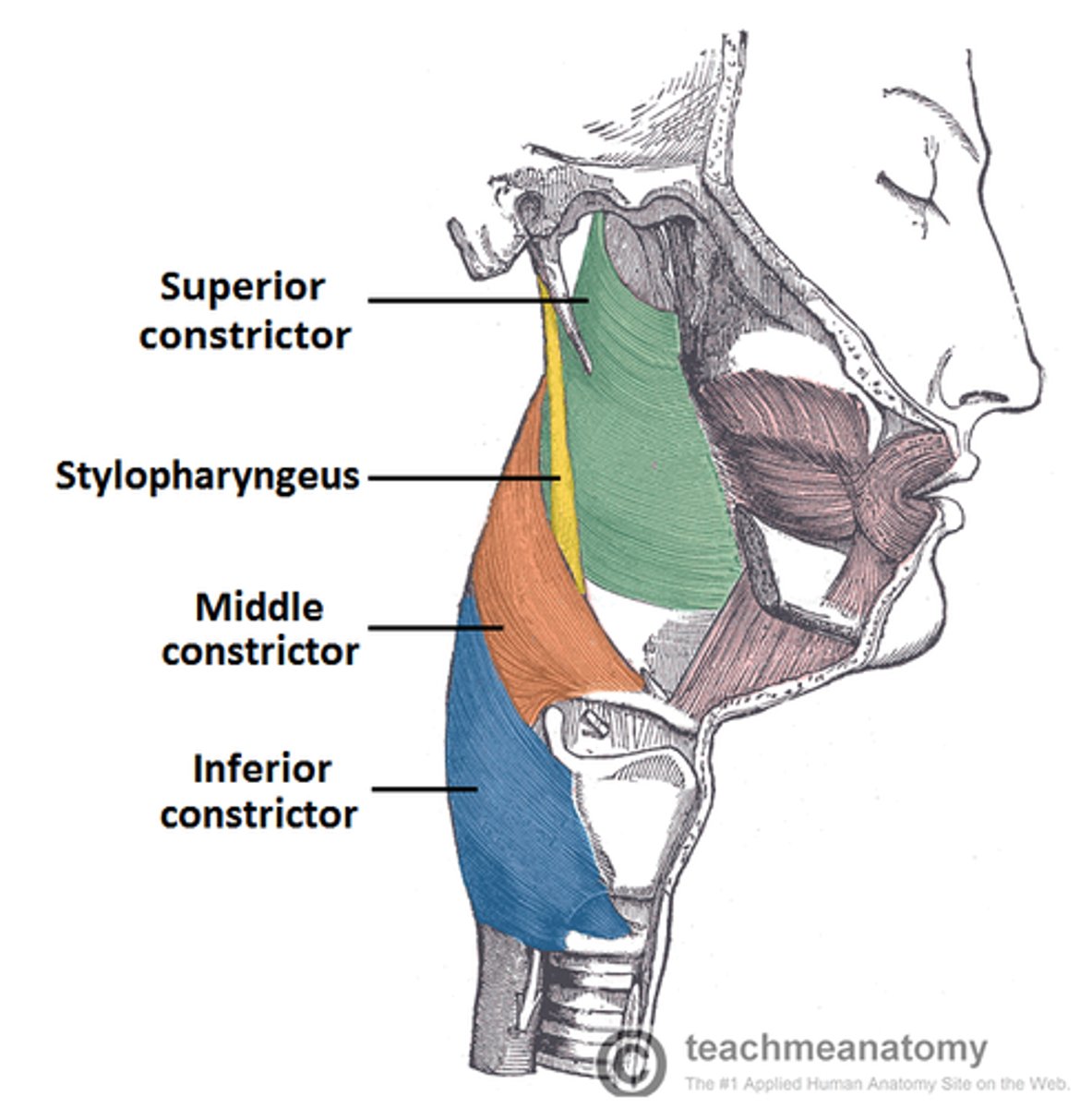
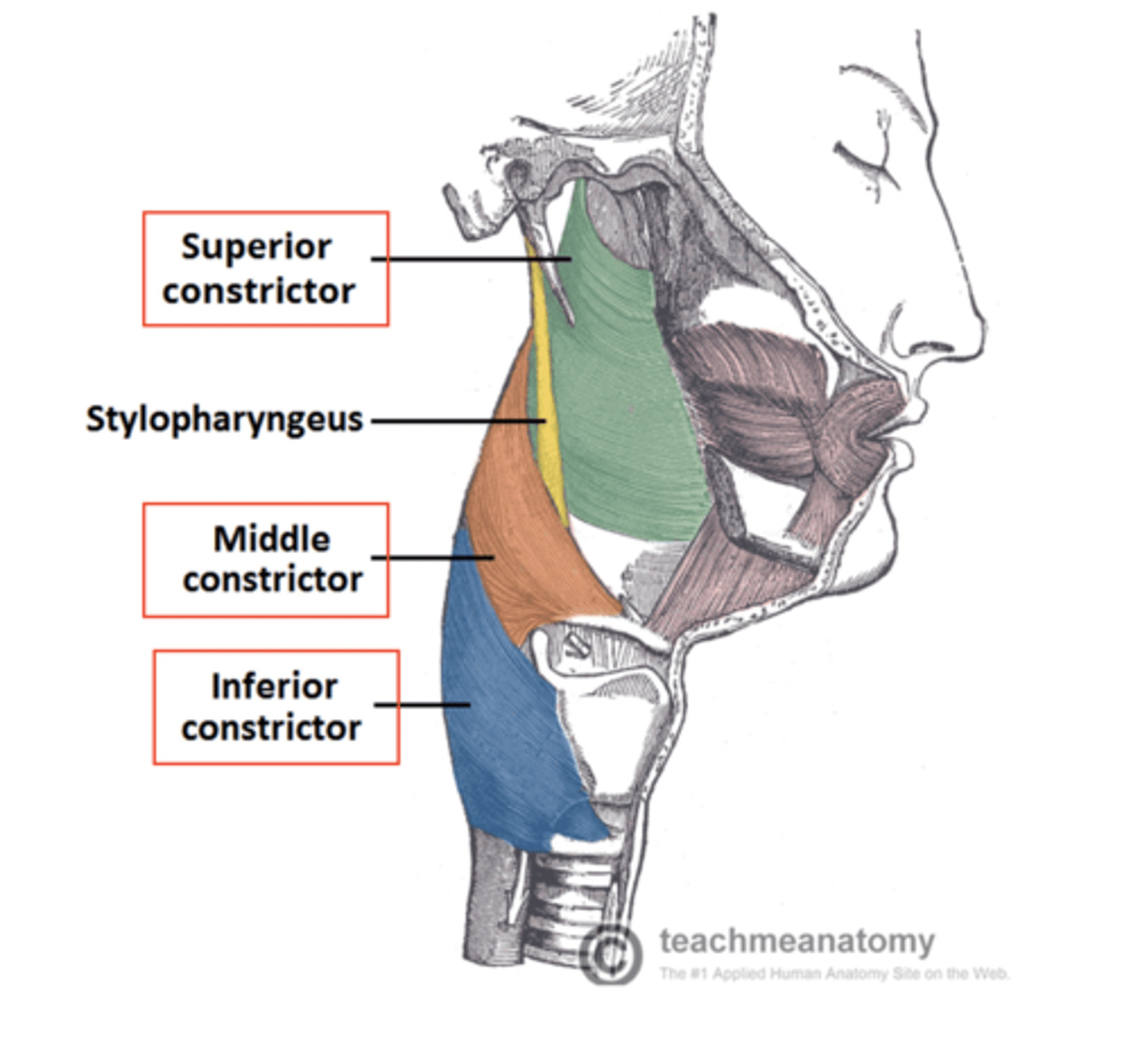
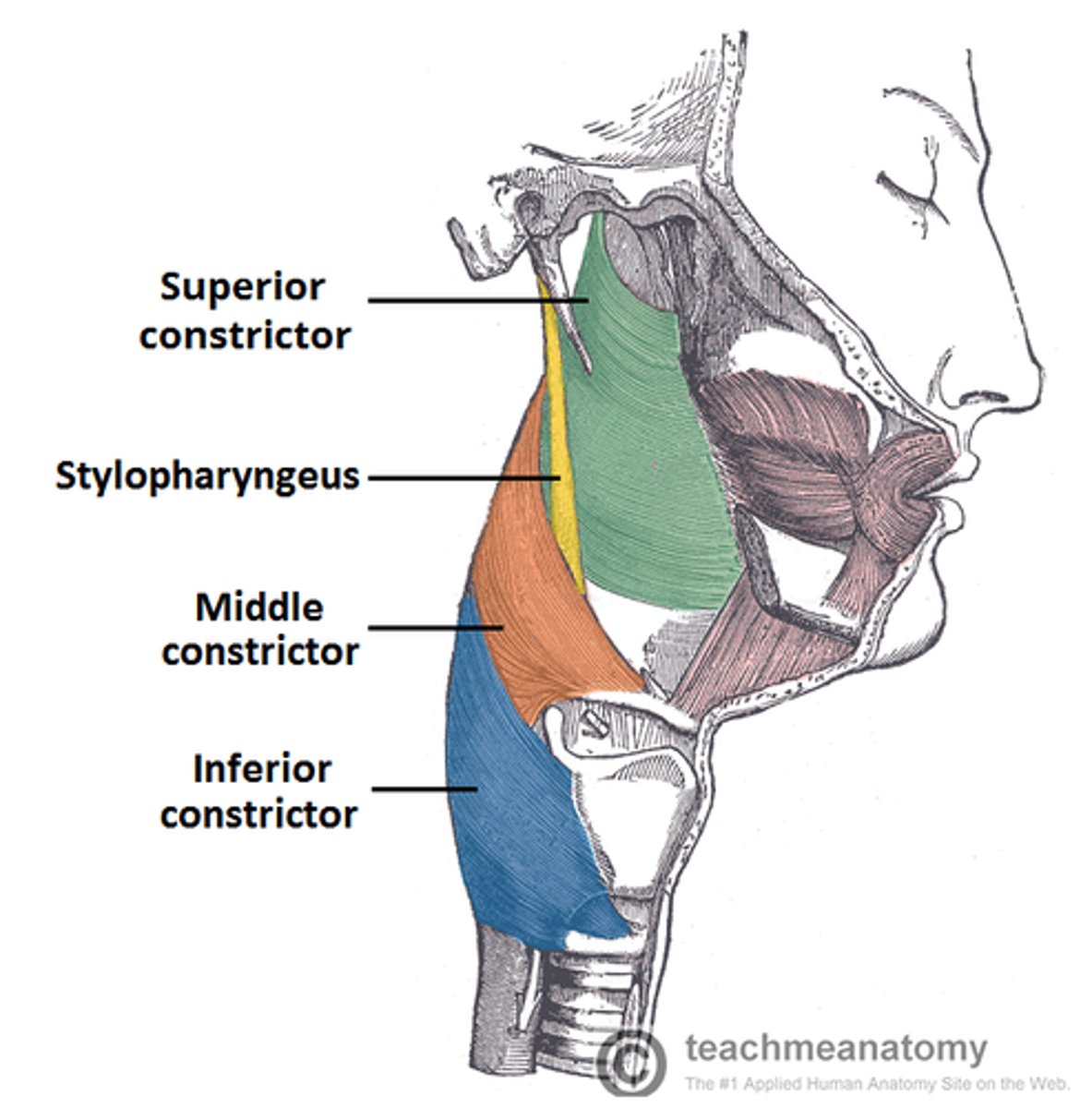
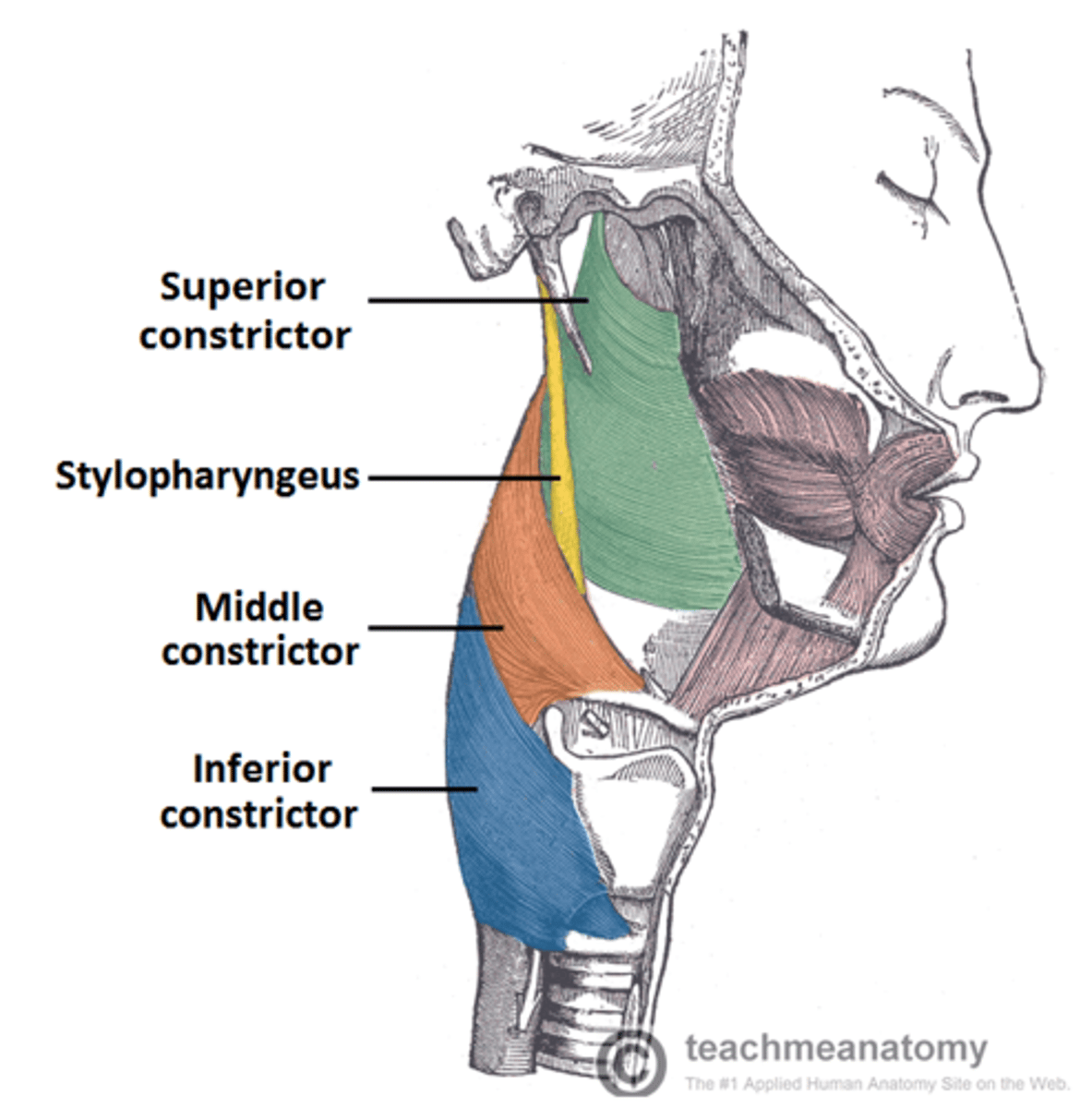
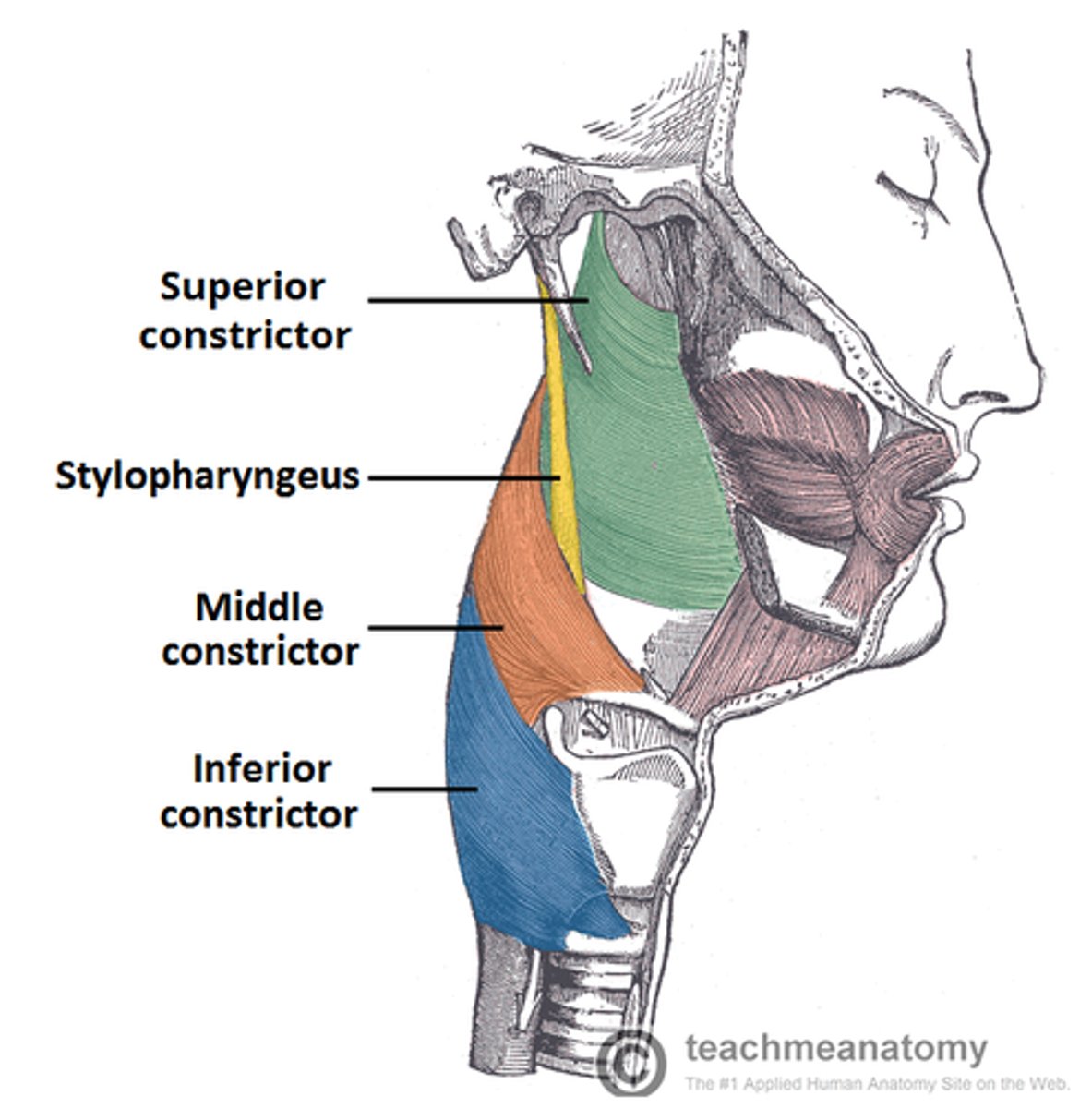
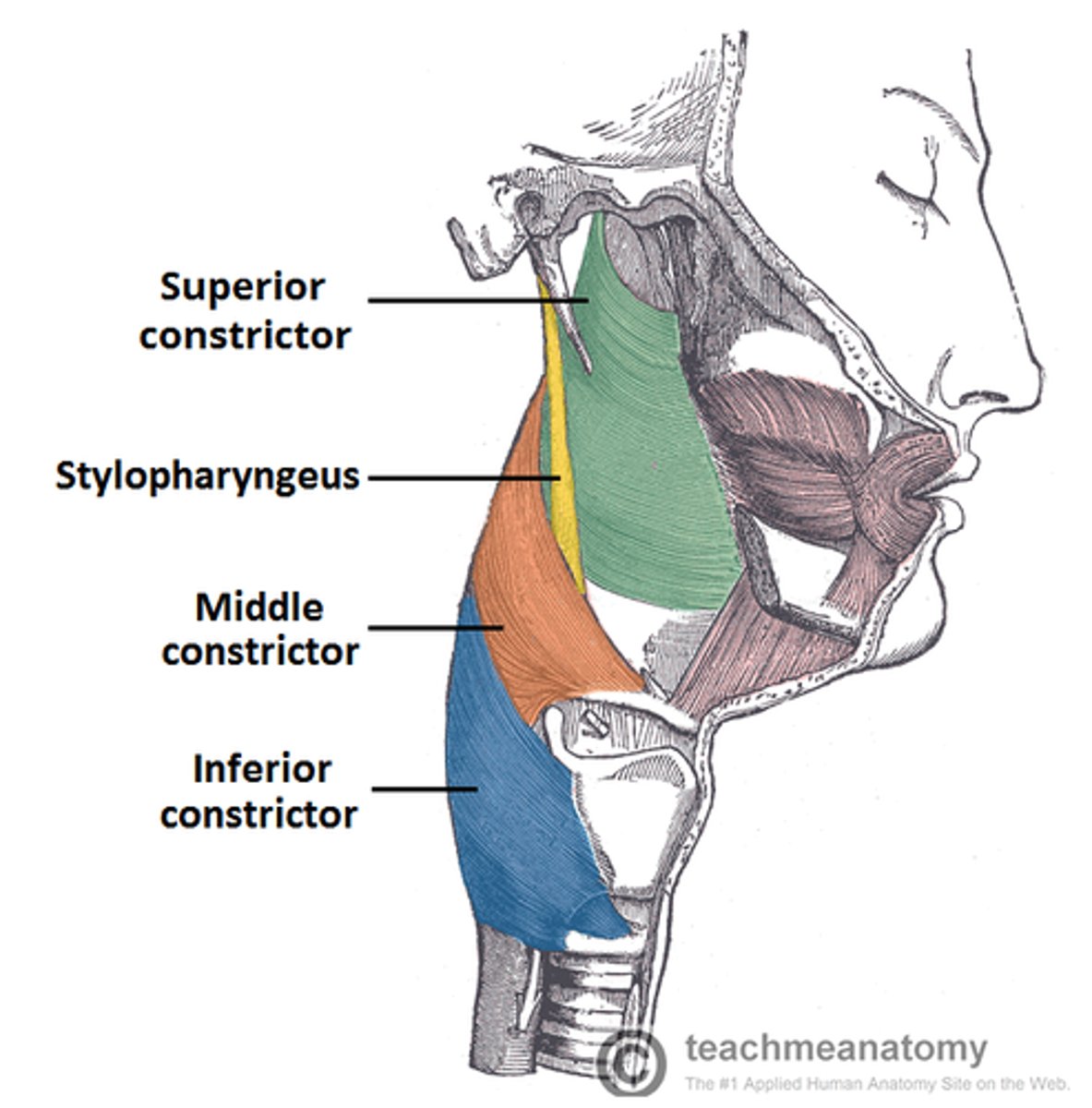
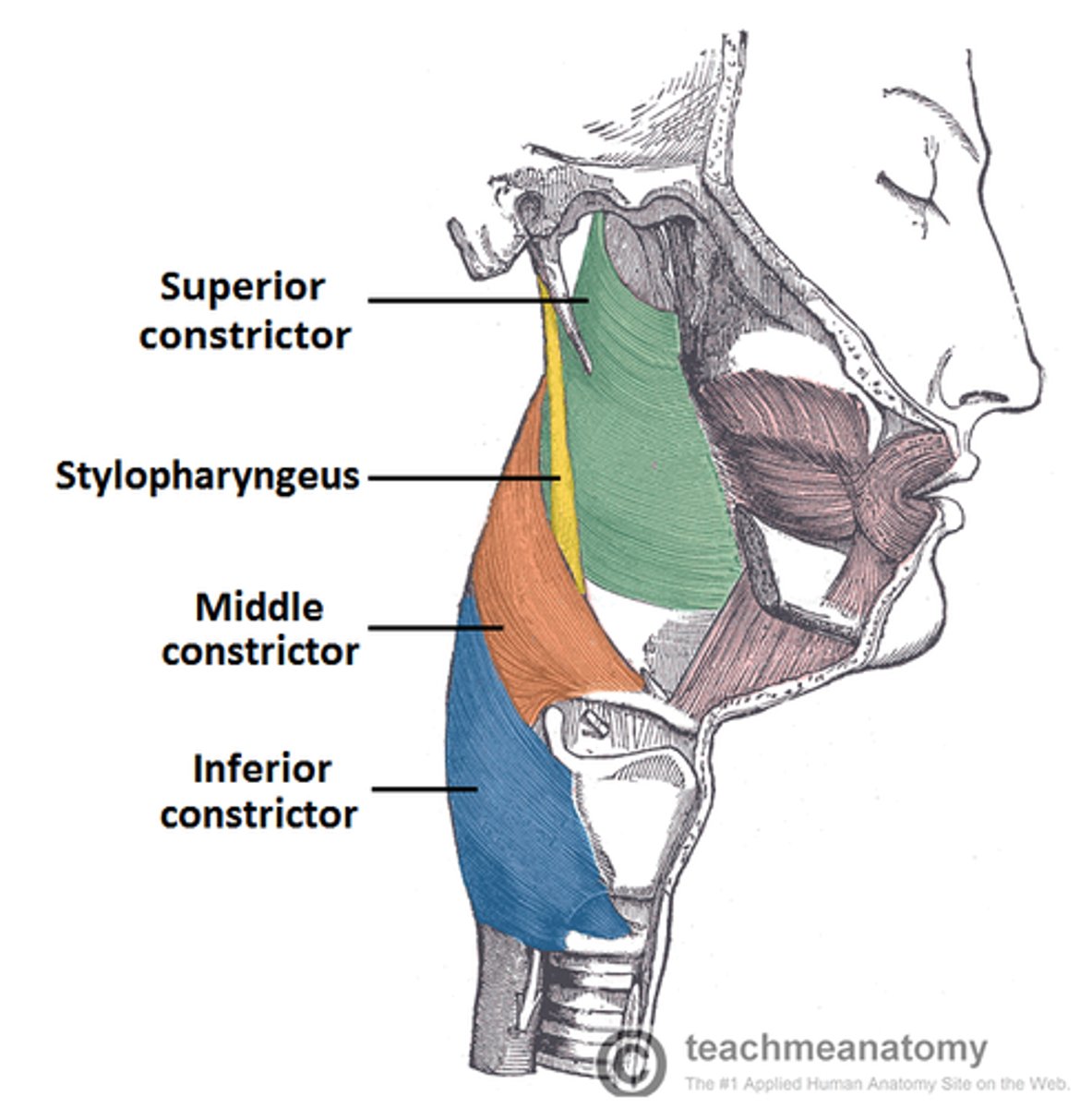
Name the three principal constrictor muscles of the pharynx.
The superior, middle, and inferior pharyngeal constrictors.
1. superior constrictor
2. middle constrictor
3. inferior constrictor
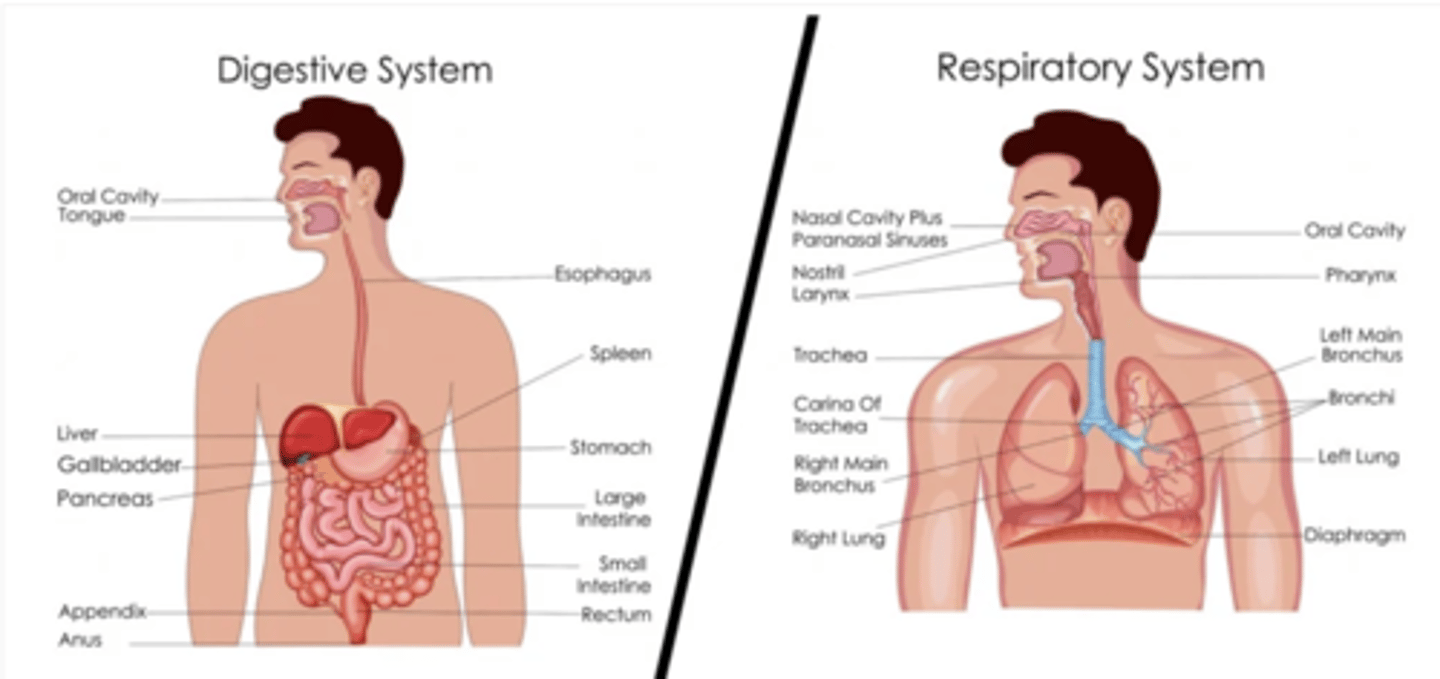
Why is the pharynx considered a part of both the digestive and respiratory systems?
It facilitates the passage of both:
1. air (to the lungs)
2. food (to the esophagus)
serves as a pathway for inhaled and exhaled air, connecting the nasal and oral cavities to the larynx.
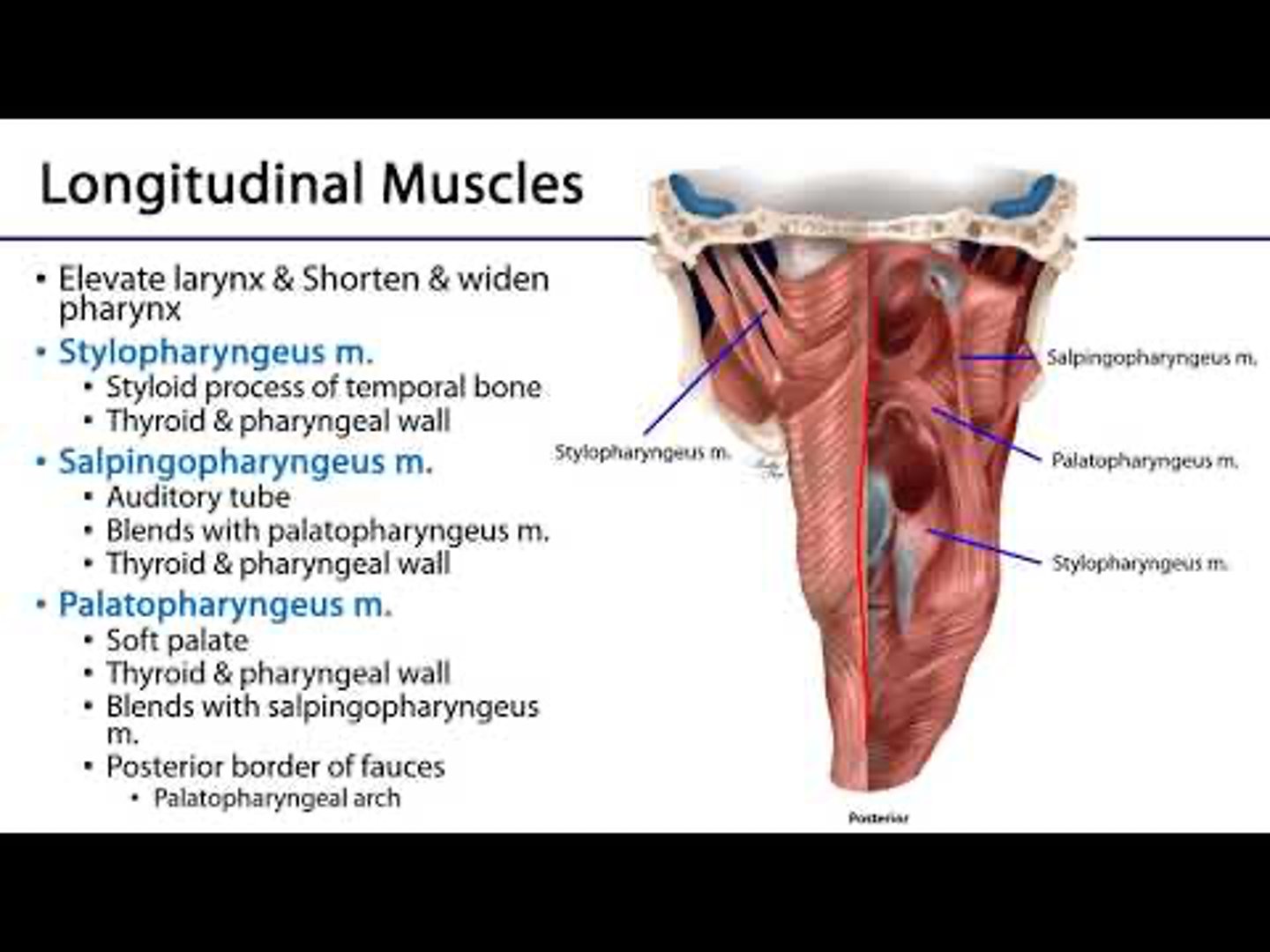
What is the function of the longitudinal muscles in the pharynx?
They elevate the pharynx and larynx during swallowing and speaking.
The inner longitudinal layer consists of the palatopharyngeus, salpingopharyngeus, and stylopharyngeus muscles.
1. palatopharyngeus
2. salpingopharyngeus
3. stylopharyngeus
How does the pharynx contribute to speech?
It resonates voiced sounds produced by the larynx, adding depth and richness to the voice.

Stylopharyngeus muscle origin and insertion:
Origin: styloid process (temporal bone skull)
Insertion:
- internal aspect of the pharyngeal wall
- superior portion of the thyroid cartilage
Stylopharyngeus muscle function:
Function:
During swallowing, it elevates the pharynx and larynx, this aids in the descent of the bolus.
ELEVATION OF PHARYNX + LARYNX: DESCENT OF BOLUS
Palatopharyngeus muscle origin and insertion:
Origin: palatine aponeurosis of the soft palate.
Insertion: lateral walls of the pharynx.
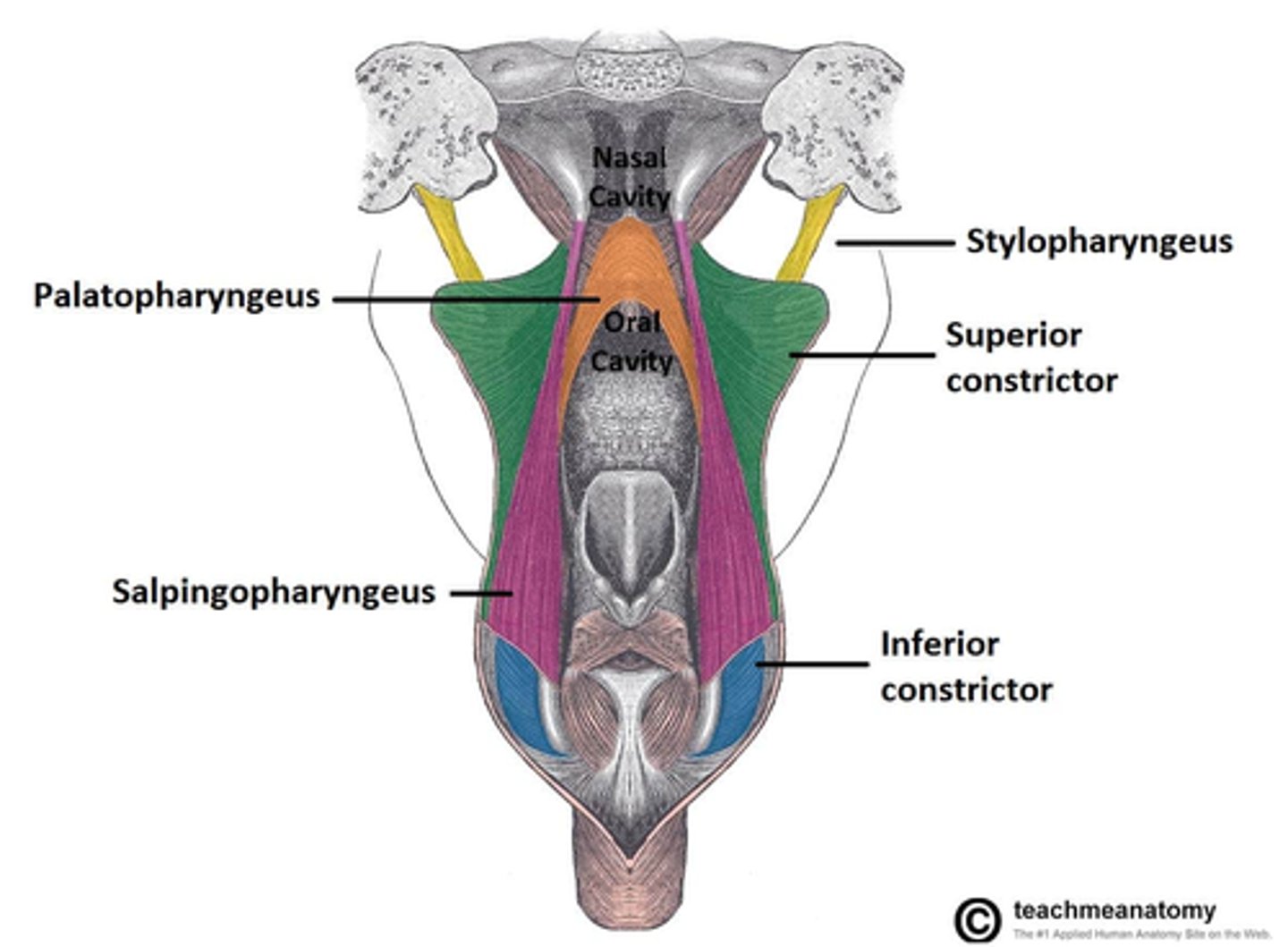
Palatopharyngeus muscle function:
Function:
narrows the pharyngeal cavity and elevates the pharynx and larynx aiding in swallowing and speaking
1. narrows the pharyngeal cavity.
2. elevates the pharynx and larynx.
Salpingopharyngeus muscle origin and insertion:
Origin: originates from the lower part of the cartilage of the auditory tube (Eustachian tube).
Insertion: walls of the pharynx.
Its fibers blend with those of the constrictor and palatopharyngeus muscles.
Salpingopharyngeus muscle function:
Function:
The salpingopharyngeus muscle aids in elevating the pharynx, particularly during the act of swallowing.
- elevates pharynx
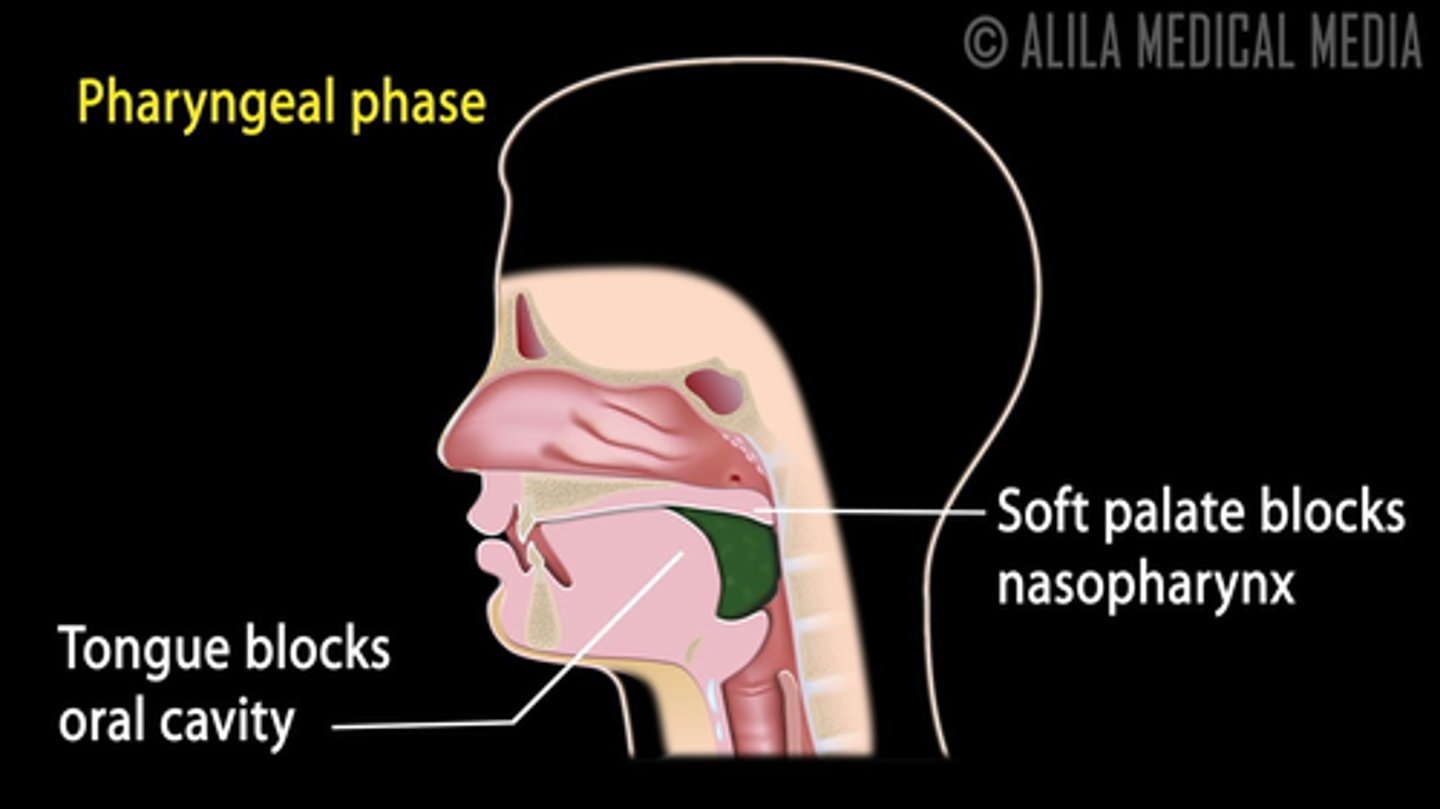
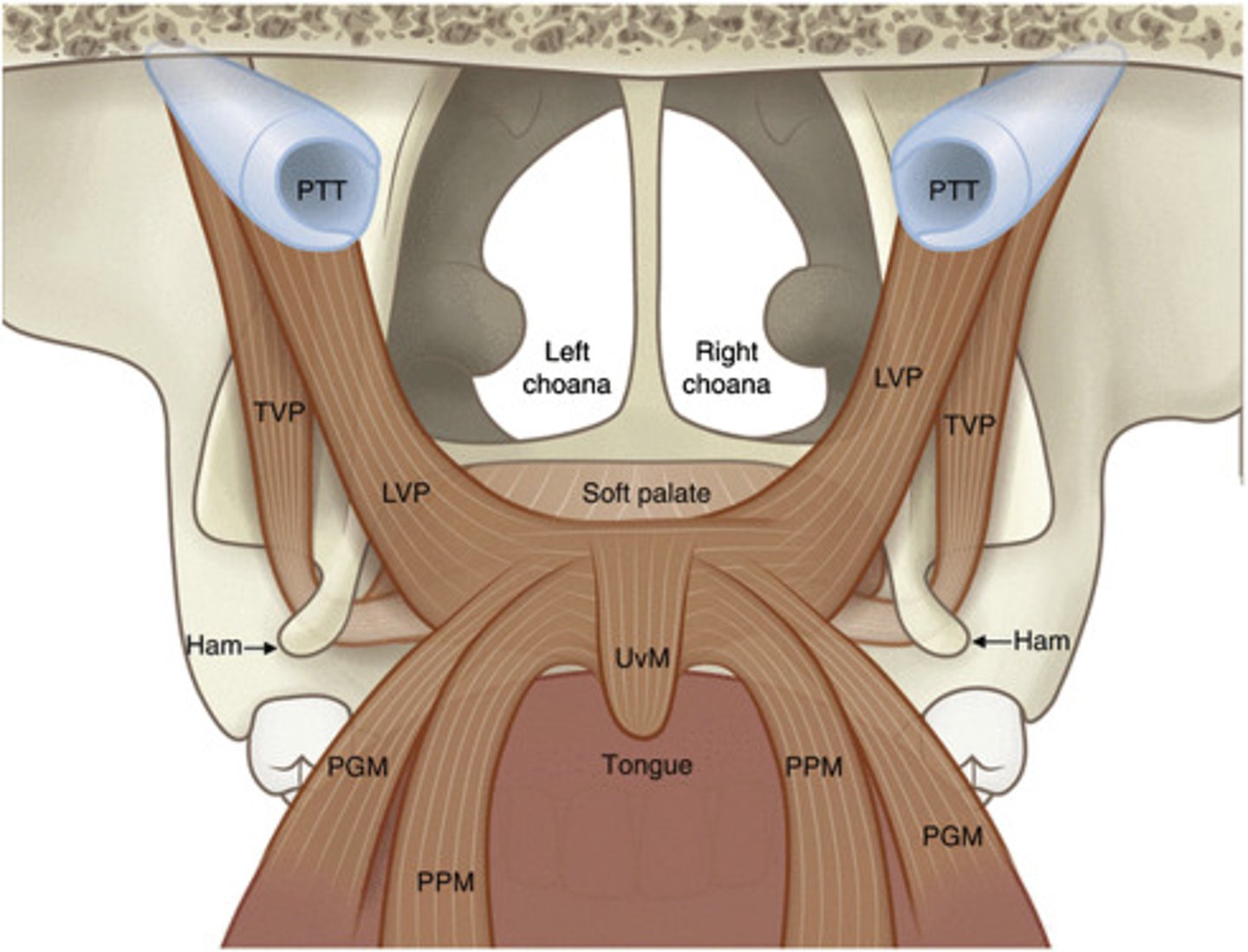
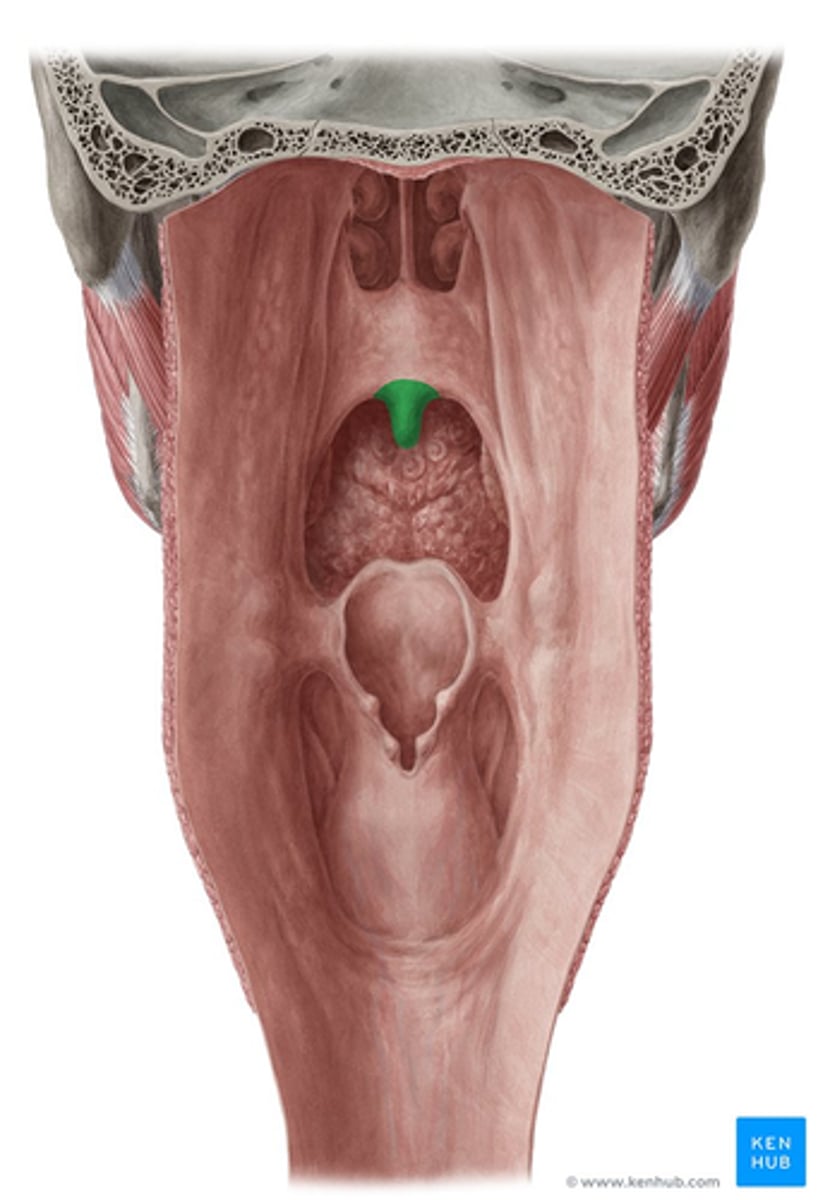
What is the primary function of the soft palate during swallowing?
During swallowing it closes off the nasopharynx to prevent food from entering the nasal cavity.
soft palate: bony structure at front of the roof of the mouth
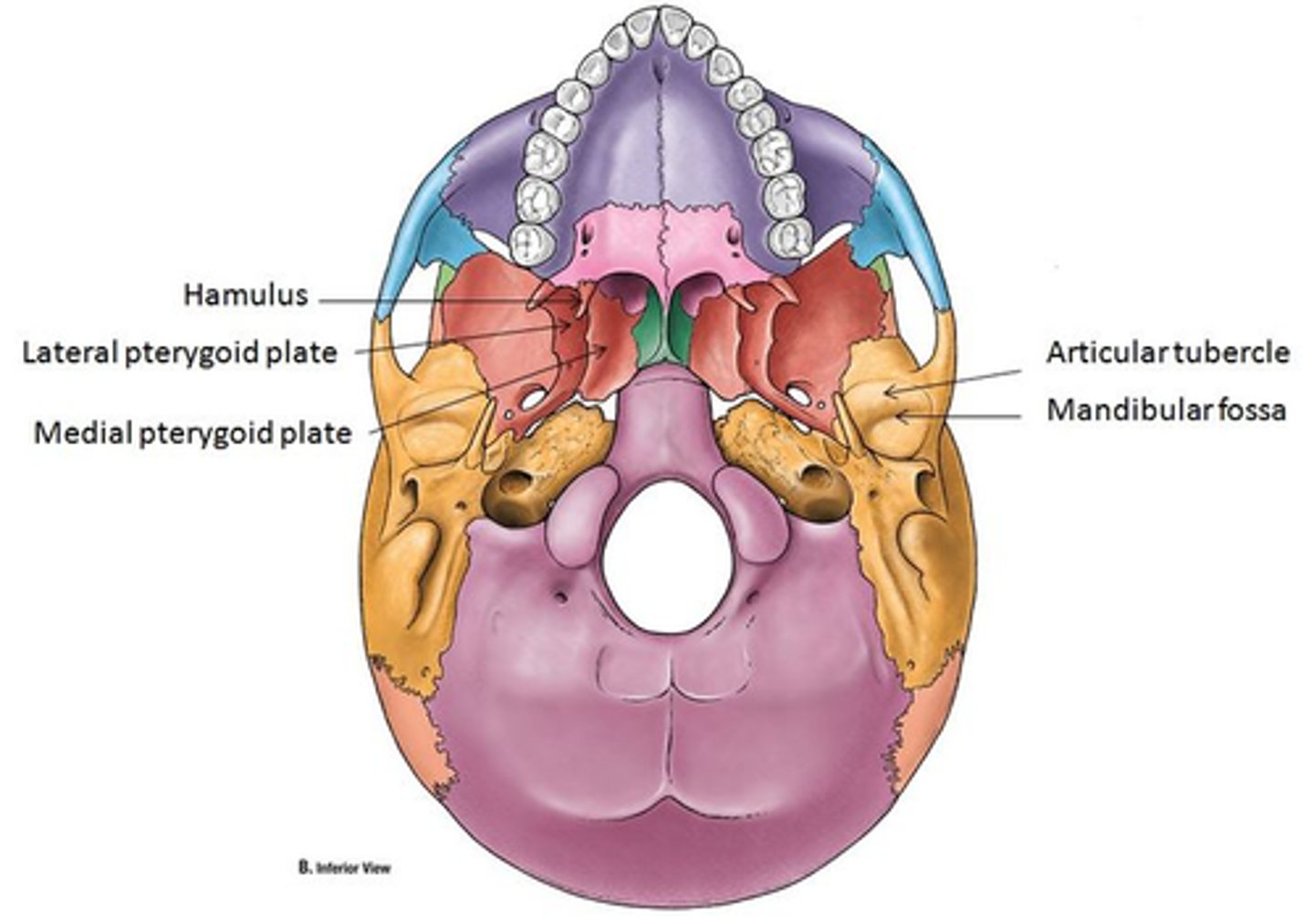
Tensor veli palatini origin and insertion:
Origin: scaphoid fossa, between medial and lateral pterygoid plates.
Insertion: palatine aponeurosis, tendinous sheet that spans soft palate.
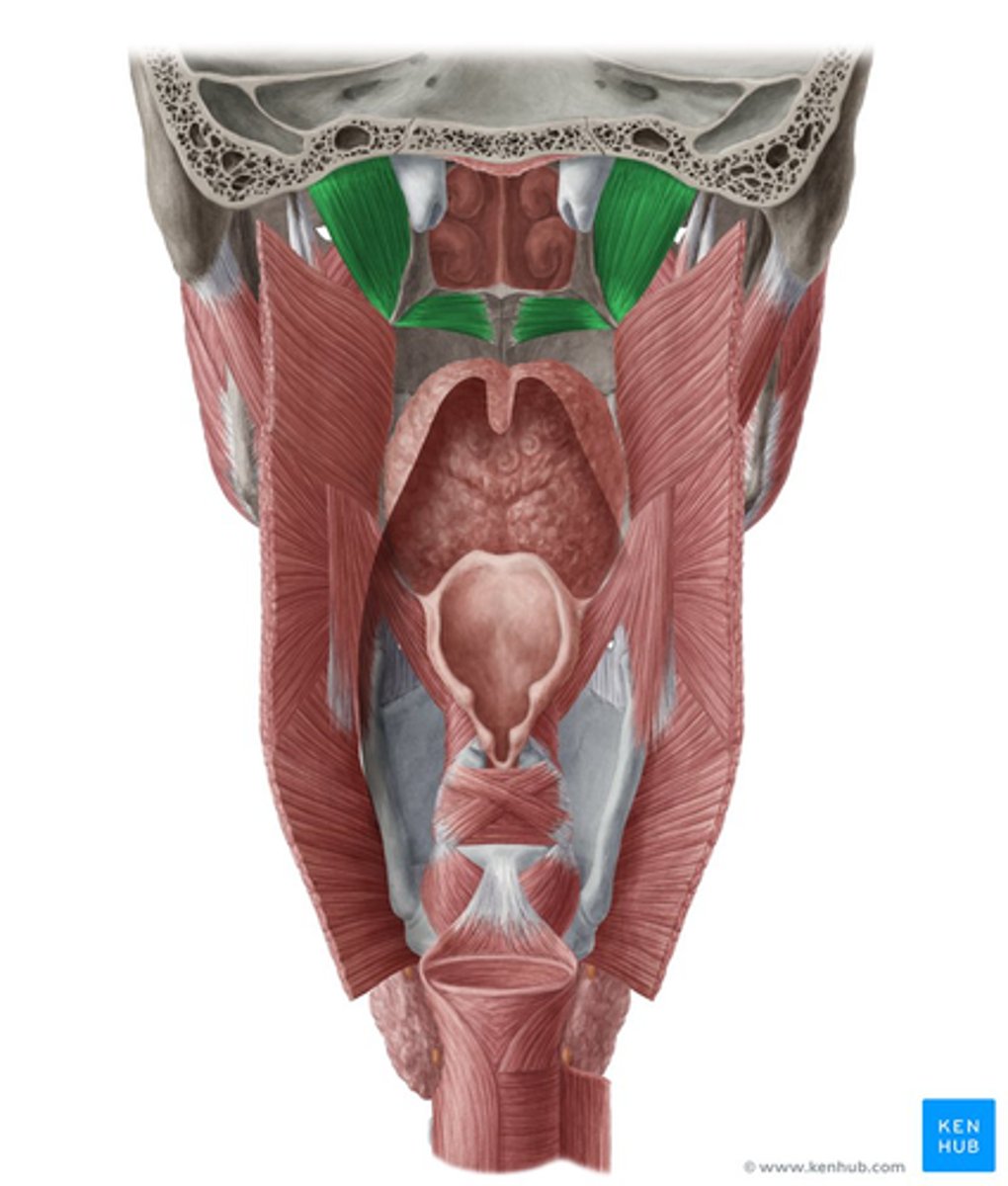
Tensor veli palatini function:
Function:
The tensor veli palatini muscle tenses the soft palate, aiding in its elevation during swallowing.
The tensor veli palatini muscle is involved in opening the Eustachian tube and tensing the soft palate.
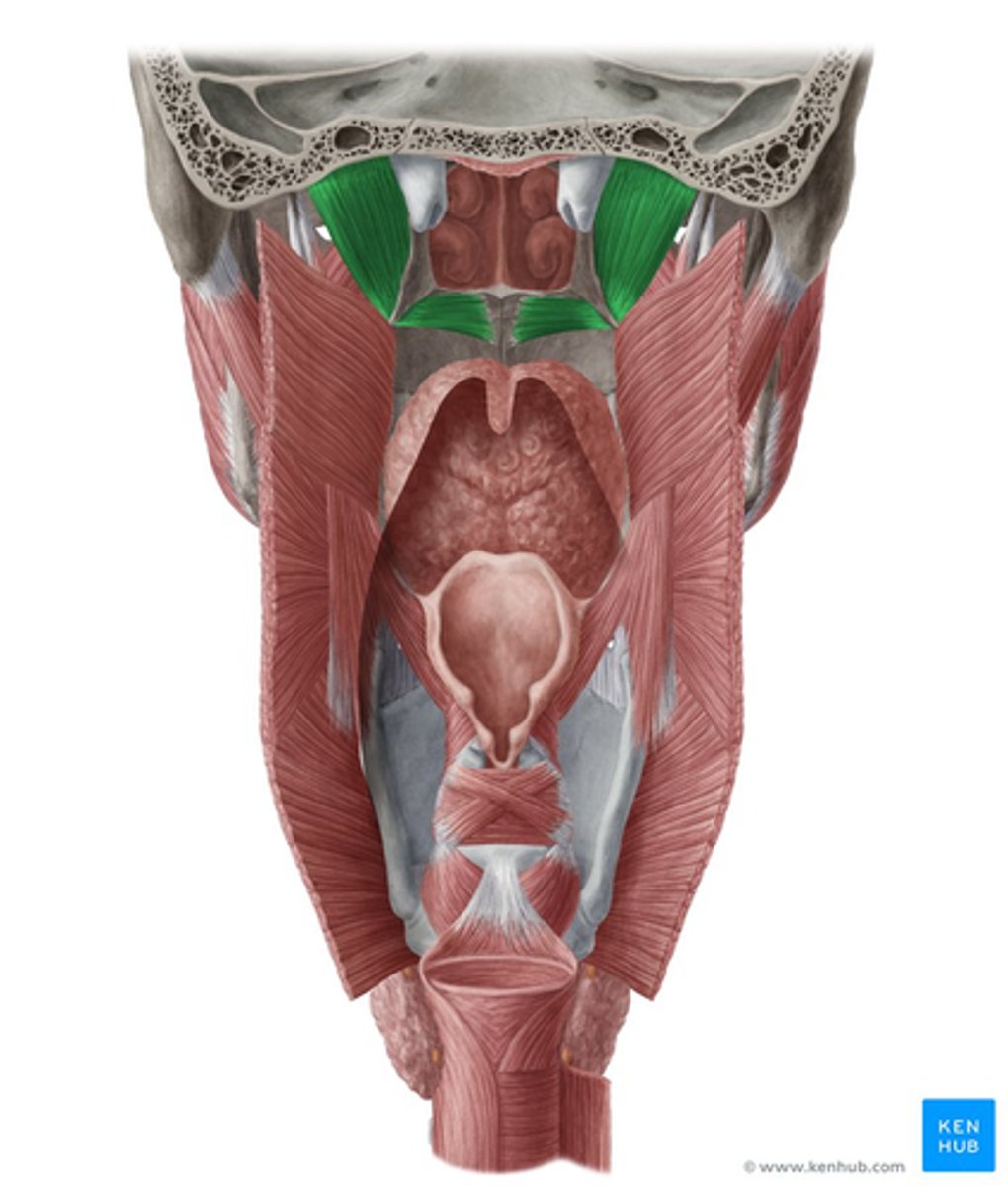
Describe the pathway of the tensor veli palatini muscle after its origin:
The tensor veli palatini muscle extends downward⬇️, becomes tendinous, and gives a 90-degree turn around the pterygoid hamulus⤵️.
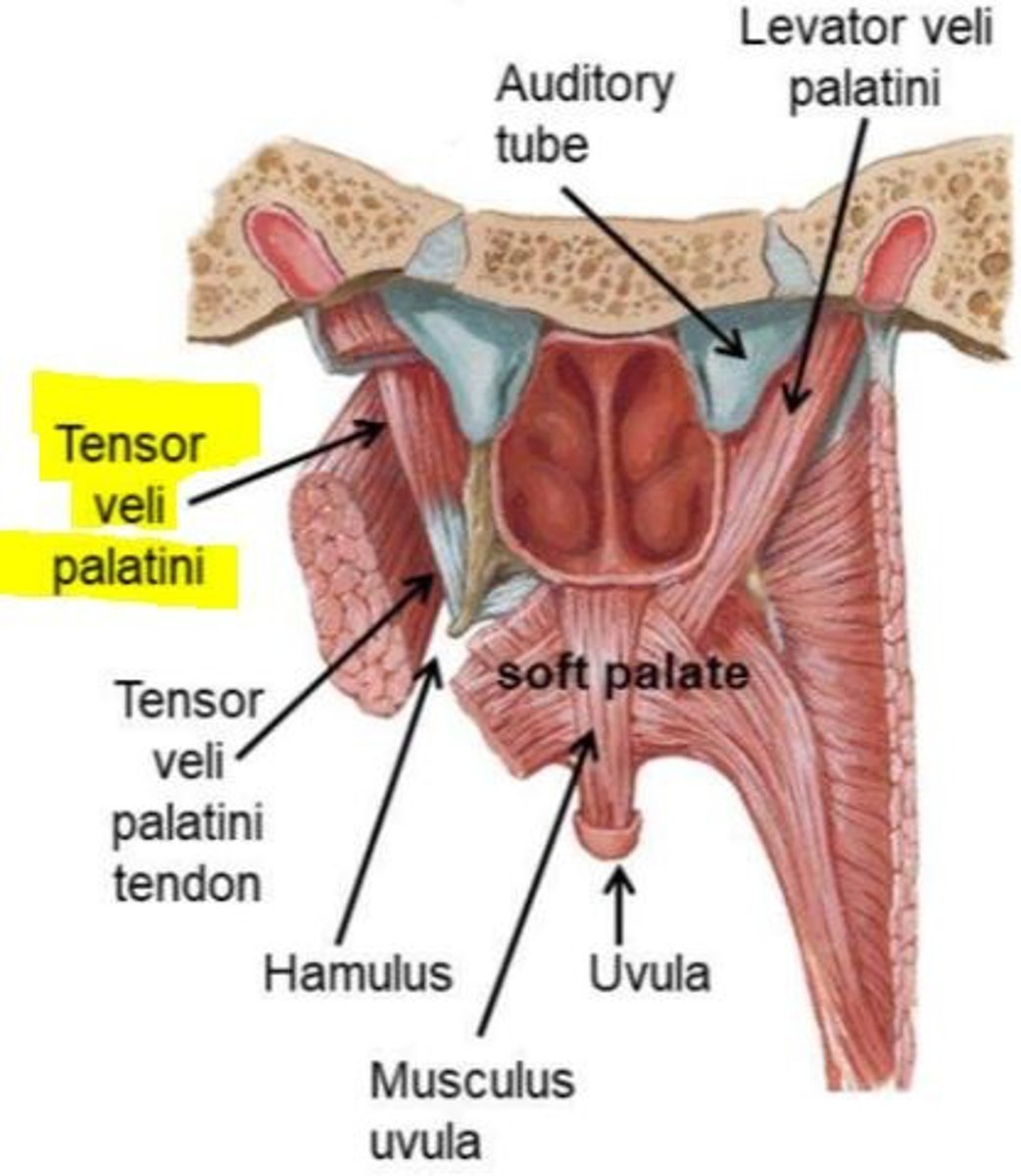
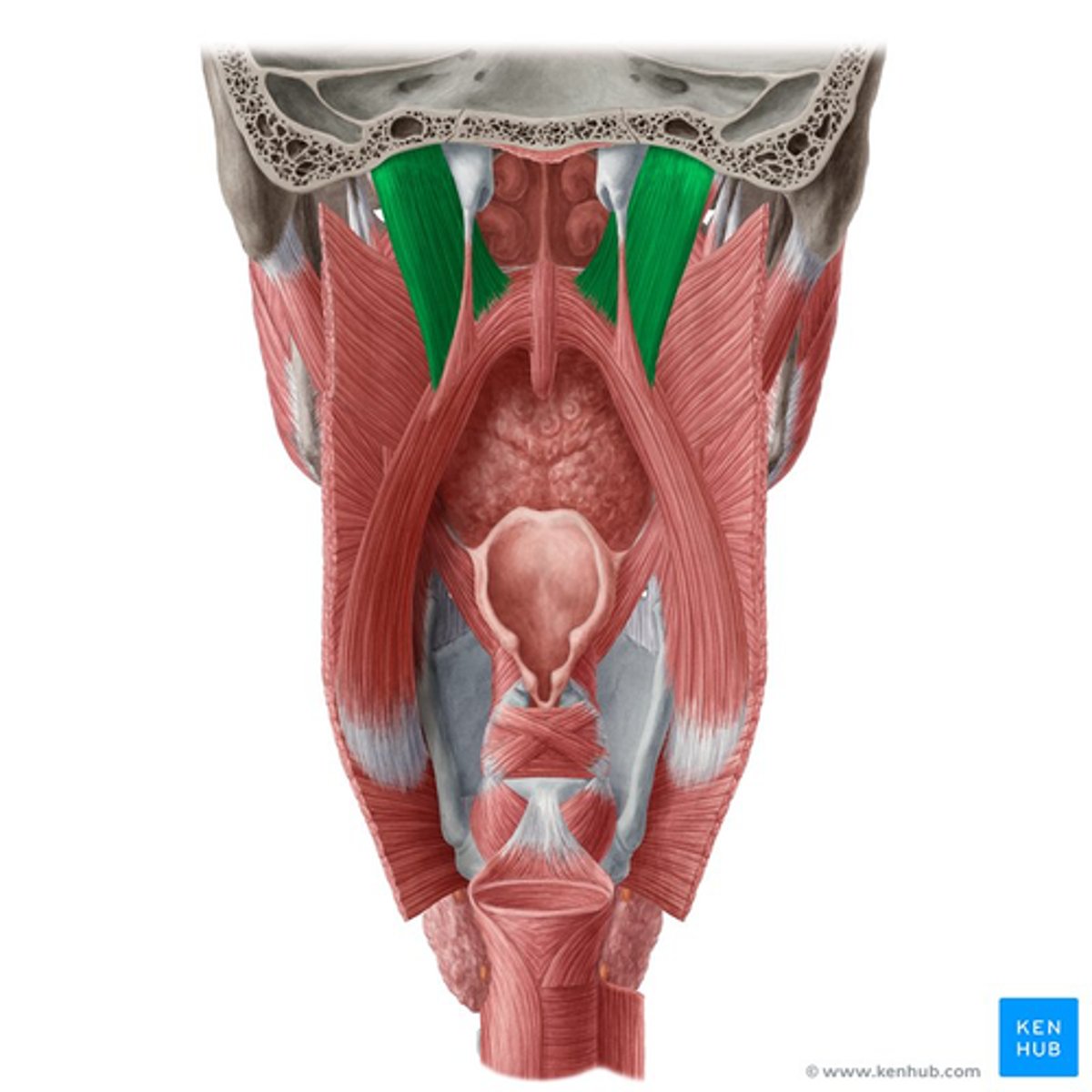
Levator veli palatini muscle origin and insertion:
Origin: petrous portion of the temporal bone and anterior aspect of the carotid opening in the base of the cranium.
Insertion: palatine aponeurosis, blending with the fibers of the tensor veli palatini.
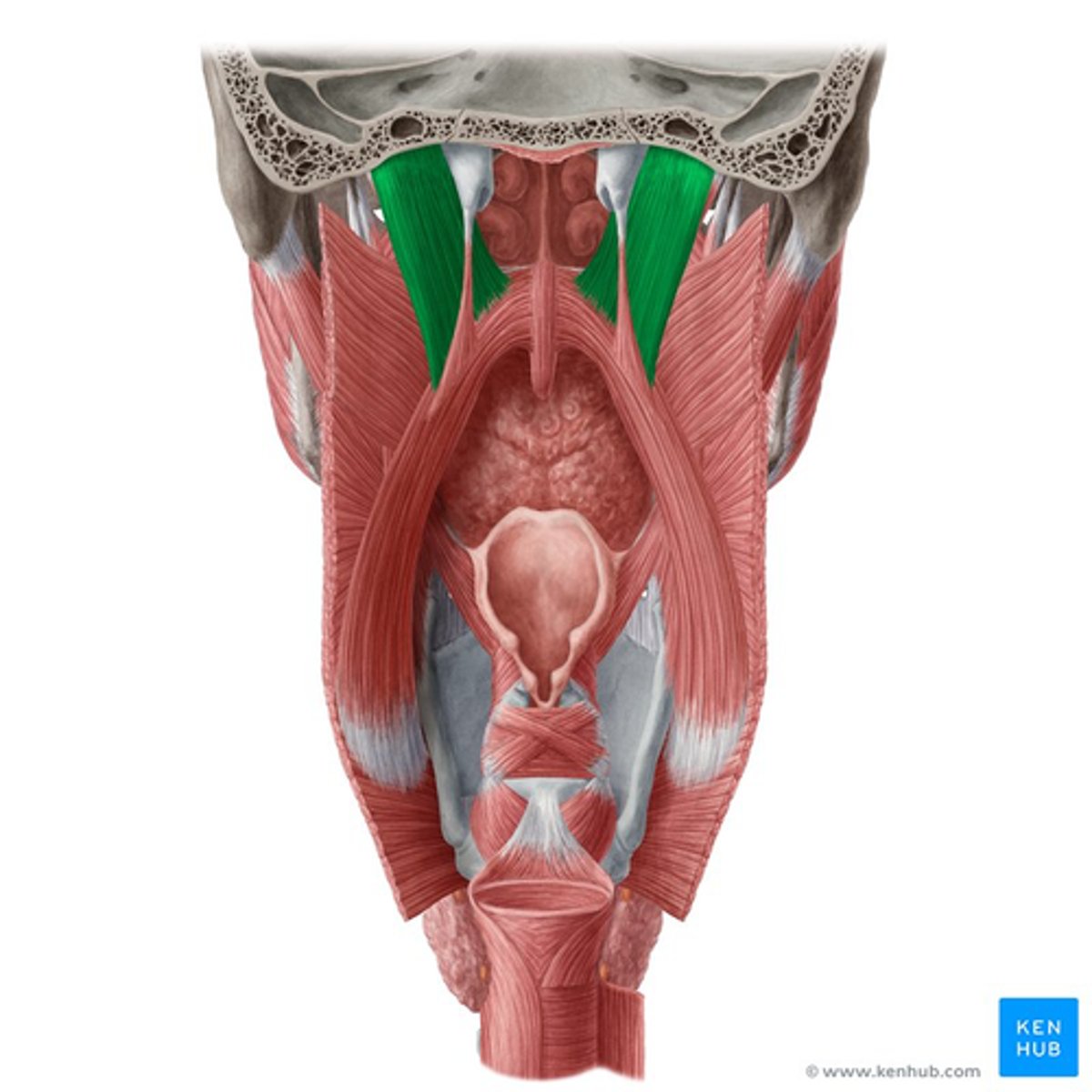
Levator veli palatini muscle function:
Function:
The levator veli palatini muscle's primary role is to elevate the soft palate during swallowing.
- elevates soft palate during swallowing
Musculus uvulae origin and insertion:
The musculus uvulae originates from the posterior margin of the hard palate, specifically from the palatine bone.
The musculus uvulae forms the uvula, the structure that hangs from the posterior edge of the soft palate.
What is the function of the musculus uvulae?
It contributes to the movement and function of the uvula: effective closure of nasopharynx during swallowing.
What happens to the soft palate during deglutition apnea?
During deglutition apnea, the soft palate is elevated to close off the nasopharynx, and after swallowing, it descends to allow breathing to resume.
what is Deglutition apnea
Deglutition apnea refers to a temporary cessation or pause in breathing that occurs during swallowing.
The elevation is crucial to prevent food or liquid from entering the nasal passages, directing it instead towards the oropharynx.
What muscle also blends into the tendinous portion of the tensor veli palatini AND contributes to soft palate function?
The palatopharyngeus muscle blends into the tendinous portion of the tensor veli palatini, contributing to the function of the soft palate.
What is the course of the palatopharyngeus muscle in relation to the soft palate?
The palatopharyngeus muscle originates from the soft palate and descends towards the pharynx, inserting into the walls of the pharynx.
What is the significance of the tensor veli palatini's turn around the hamulus?
The 90-degree turn of the tensor veli palatini around the hamulus is crucial for its function, allowing it to change direction and effectively tense the soft palate.
90 DEGREE TURN
How do the tensor veli palatini and levator veli palatini muscles interact?
1. Levator Veli Palatini Originates (petrous part of the temporal bone and the medial wall of the auditory tube (eustachian tube)
2. Levator Veli Descends downwards↓
3. Levator Veli Inserts into the Palatine Aponeurosis
4. Once inserted to the Palatine Aponeurosis the Levator Veli blends with the Tensor Veli Palatini
TOGETHER THEY ELEVATE THE SOFT PALATE
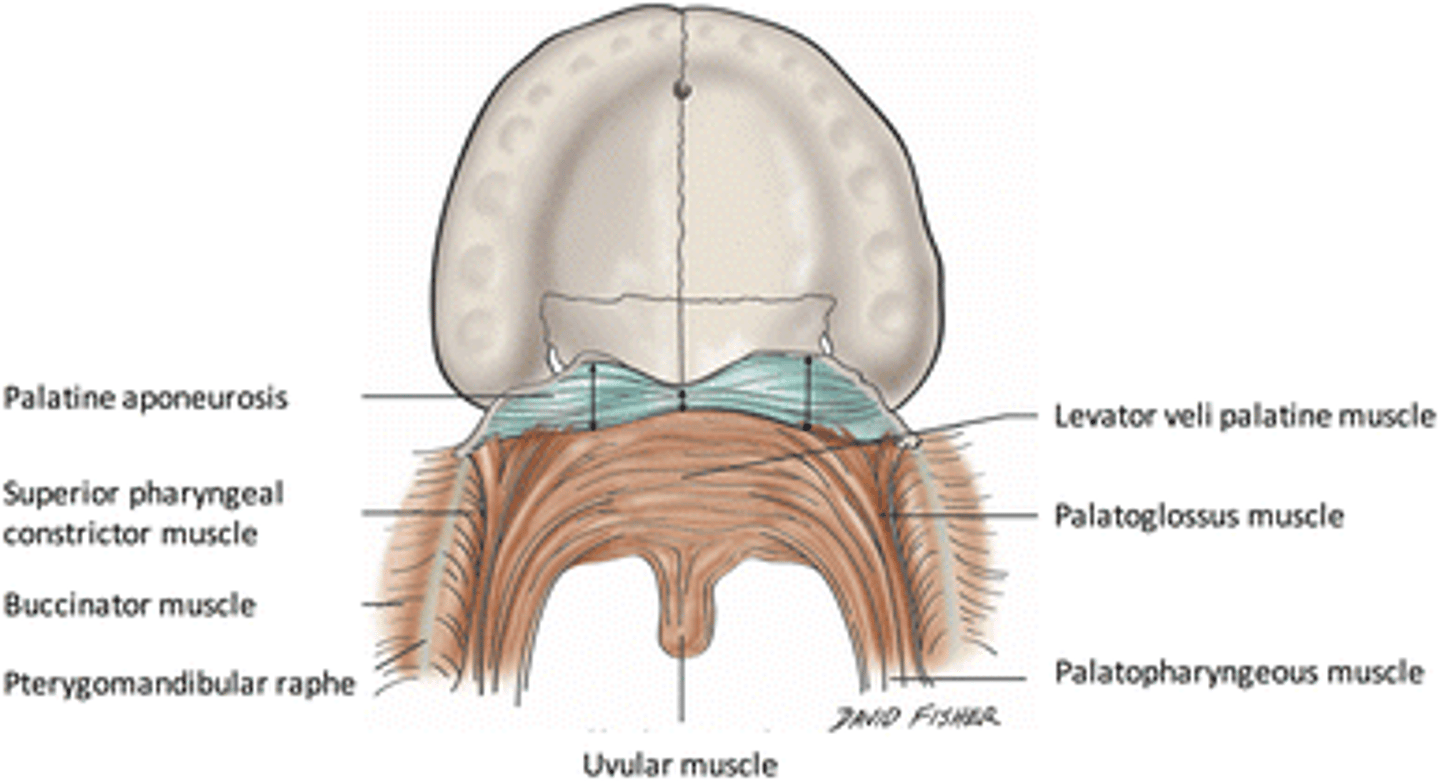
What structural feature of the soft palate is continuous with the tensor veli palatini muscle?
The palatine aponeurosis is continuous with the tensor veli palatini muscle, providing a structure for muscle attachment and function.
How does the function of the musculus uvulae contribute to the overall action of the soft palate during swallowing?
The musculus uvulae, by forming the uvula and contributing to its movement, aids in sealing the nasopharynx effectively during swallowing.
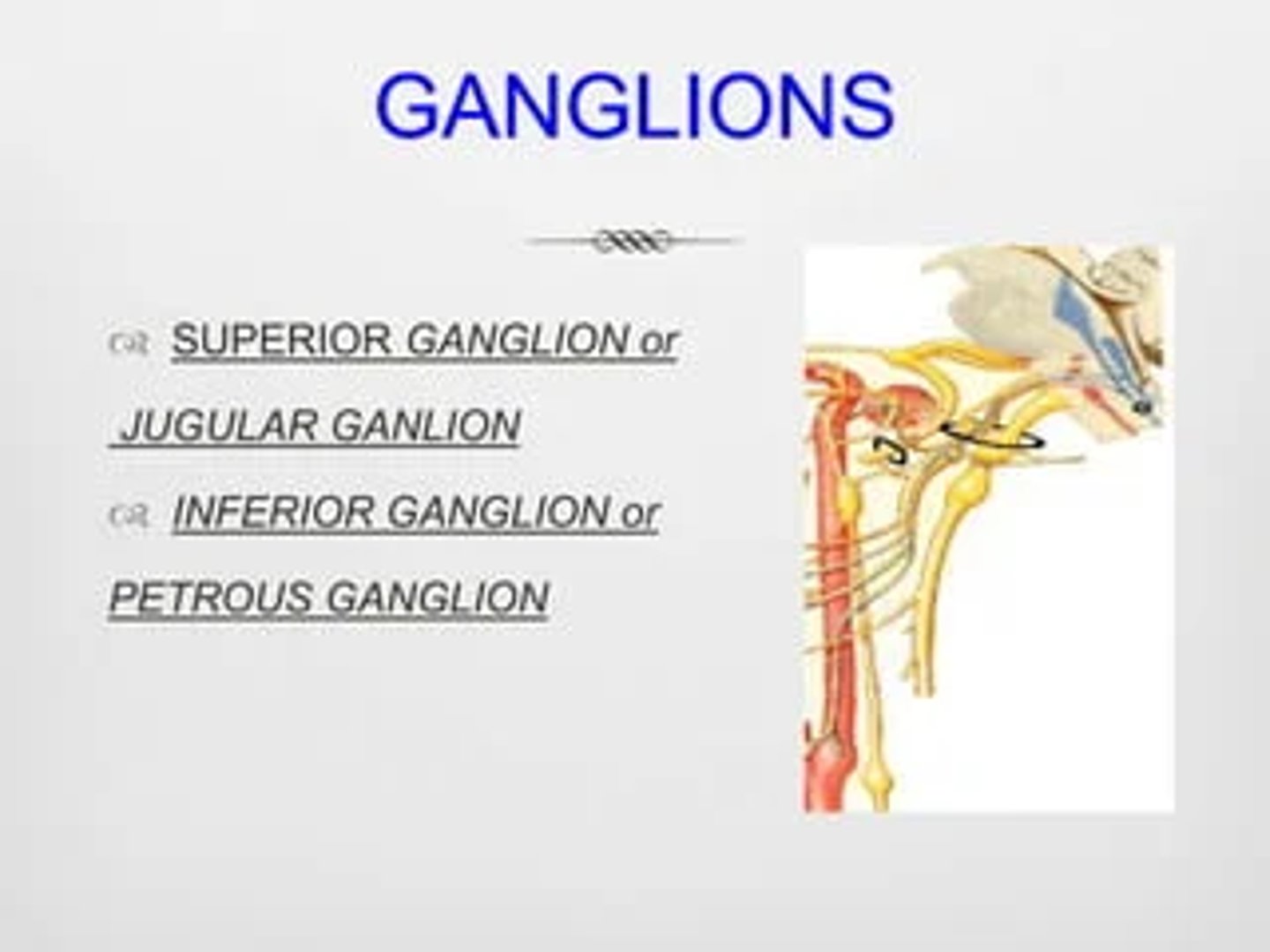
What are the two sensory ganglia associated with the glossopharyngeal nerve at the jugular foramen?
1. Superior (or Jugular) Ganglion
2. Inferior (or Petrous) Ganglion
a ganglion is defined as a collection of nerve cell bodies -not axons- located outside the CNS (hence part of PNS).
Which pharyngeal muscle is innervated by the glossopharyngeal nerve?
The glossopharyngeal nerve (CN IX) innervates the following muscles:
Stylopharyngeus Muscle: This muscle helps in swallowing and elevating the pharynx during speech and swallowing.
Specifically the motor fibers of CN IX.
THE STYLOPHARYNGEUS MUSCLE ELEVATES THE PHARYNX DURING SWALLOWING.
What type of sensory information does the glossopharyngeal nerve provide from the oral cavity?
Sensory information conveyed by the glossopharyngeal nerve (general somatic sensory):
1. Mucosa of the tongue
2. Oropharynx
3. Tonsils
Taste information conveyed by the glossopharyngeal nerve (special sensory):
4. Posterior tongue
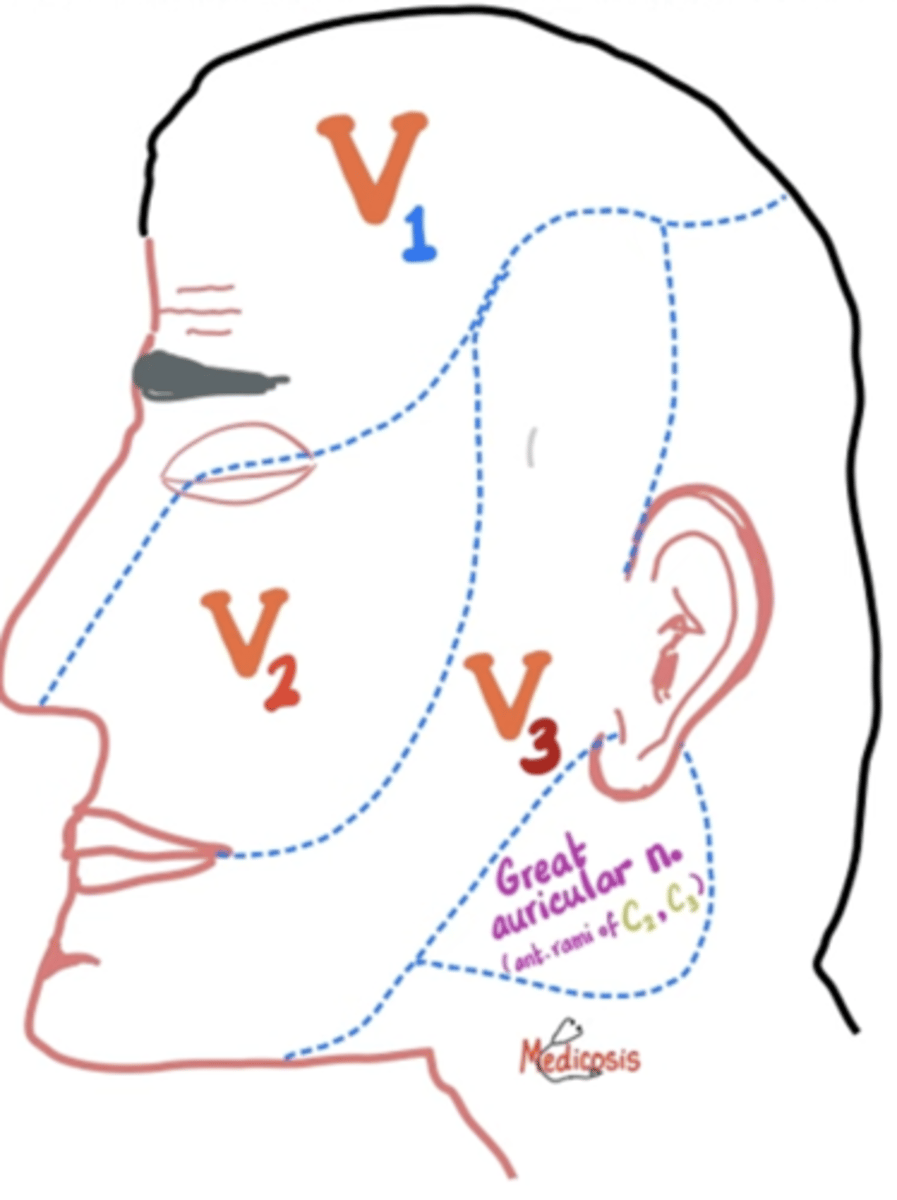
Which cranial nerve provides motor innervation to the tensor veli palatini muscle?
Motor innervation by trigeminal nerve (CN V):
1. Ophthalmic Branch (V1): Provides no motor innervation.
2. Maxillary Branch (V2): Provides no motor innervation.
3. Mandibular Branch (V3):
Muscles of Mastication:
- Temporalis
- Masseter
- Medial pterygoid
- Lateral pterygoid
Tensor Tympani Muscle
Tensor Veli Palatini Muscle
Which nerve innervates the majority of the pharyngeal constrictor muscles?
Vagus nerve (CN X) innervates majority of pharyngeal constrictor muscles, superior: CN IX
1. Superior Pharyngeal Constrictor Muscle: branches of the glossopharyngeal nerve (CN IX).
2. Middle Pharyngeal Constrictor Muscle: branches of the vagus nerve (CN X); pharyngeal branch of vagus.
3. Inferior Pharyngeal Constrictor Muscle: branches of the vagus nerve (CN X), pharyngeal branch of vagus.
How does the glossopharyngeal nerve interact with its sensory ganglia?
The somatic efferents (motor fibers) of the glossopharyngeal nerve course through its sensory ganglia without synapsing.
allows direct control of muscles involved in swallowing and speech without interruption
What is the significance of the glossopharyngeal nerve's pathway in relation to the pharyngeal constrictor muscles?
The glossopharyngeal nerve goes between:
1. superior pharyngeal constrictor
2. middle pharyngeal constrictor
TO REACH & INNERVATE STYLOPHARYNGEUS MUSCLE
Which cranial nerve is primarily responsible for coordinating swallowing?
The vagus nerve (CN X) is primarily responsible for coordinating the motor functions of swallowing.
VAGUS NERVE (CN X): SWALLOWING, speech
Which artery is a key supplier to the tonsillar fossa?
The tonsillar artery, a branch of the facial artery, supplies the tonsillar fossa.
TONSILLAR ARTERY: BRANCH OF FACIAL ARTERY

From which artery does the tonsillar artery originate?
The tonsillar artery originates from the facial artery.
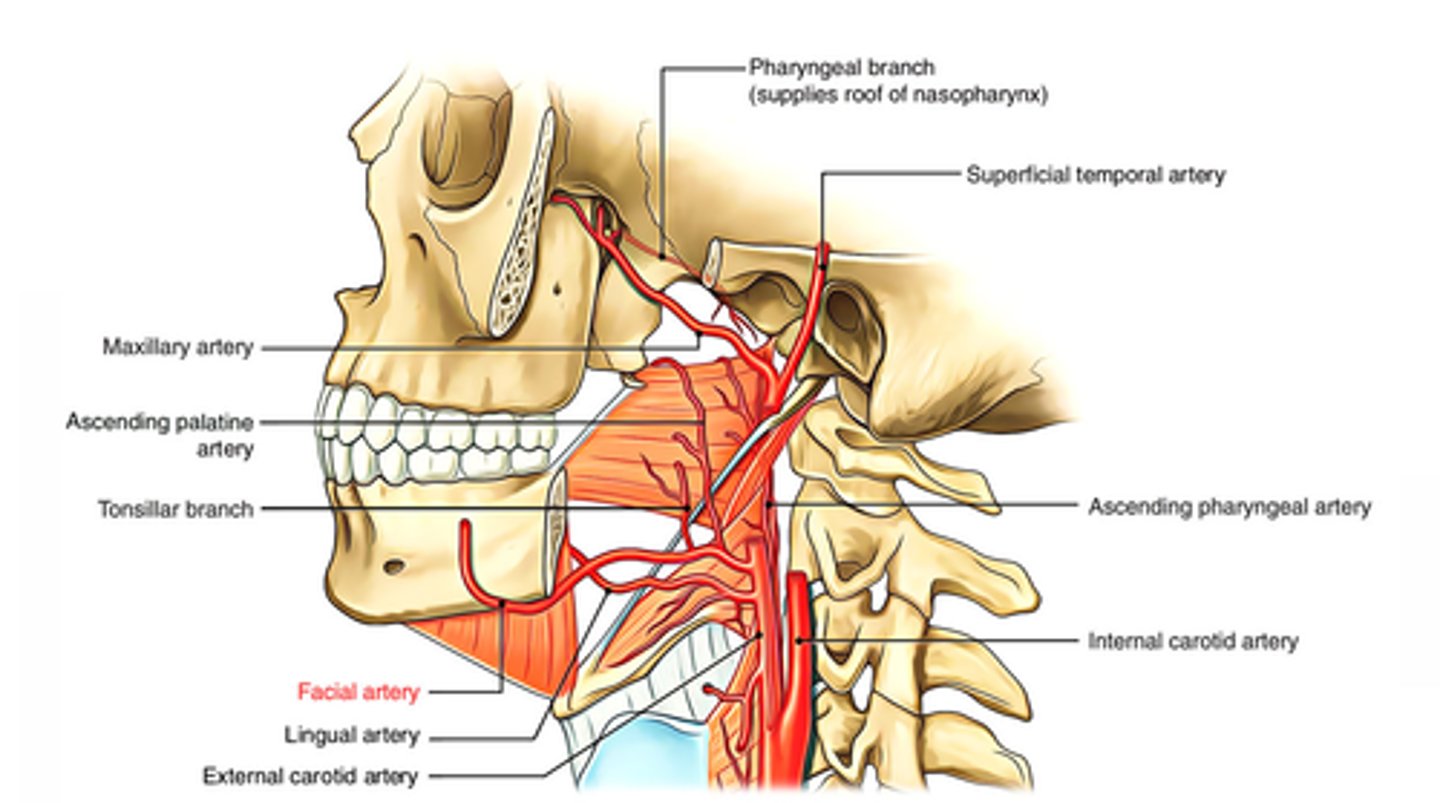
Which muscle does the tonsillar artery pierce to supply the tonsillar fossa?
The tonsillar artery pierces the superior constrictor muscle to reach the tonsillar fossa.
Name a branch of the facial artery that contributes to the pharynx's blood supply.
The ascending palatine artery is a branch of the facial artery that contributes to the pharynx's blood supply.
ASCENFING PALATINE ARTERY: BRANCH OF FACIAL ARTERY
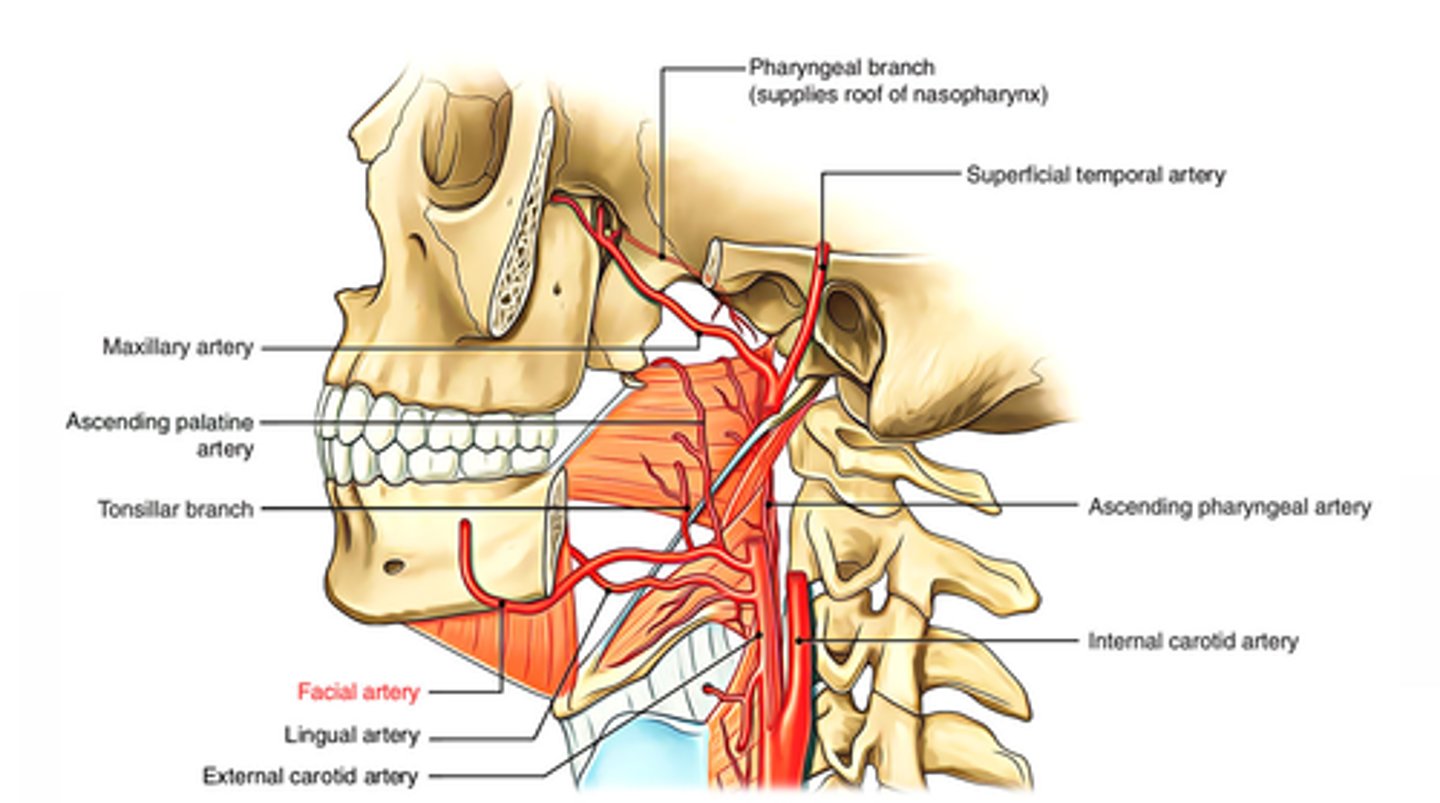
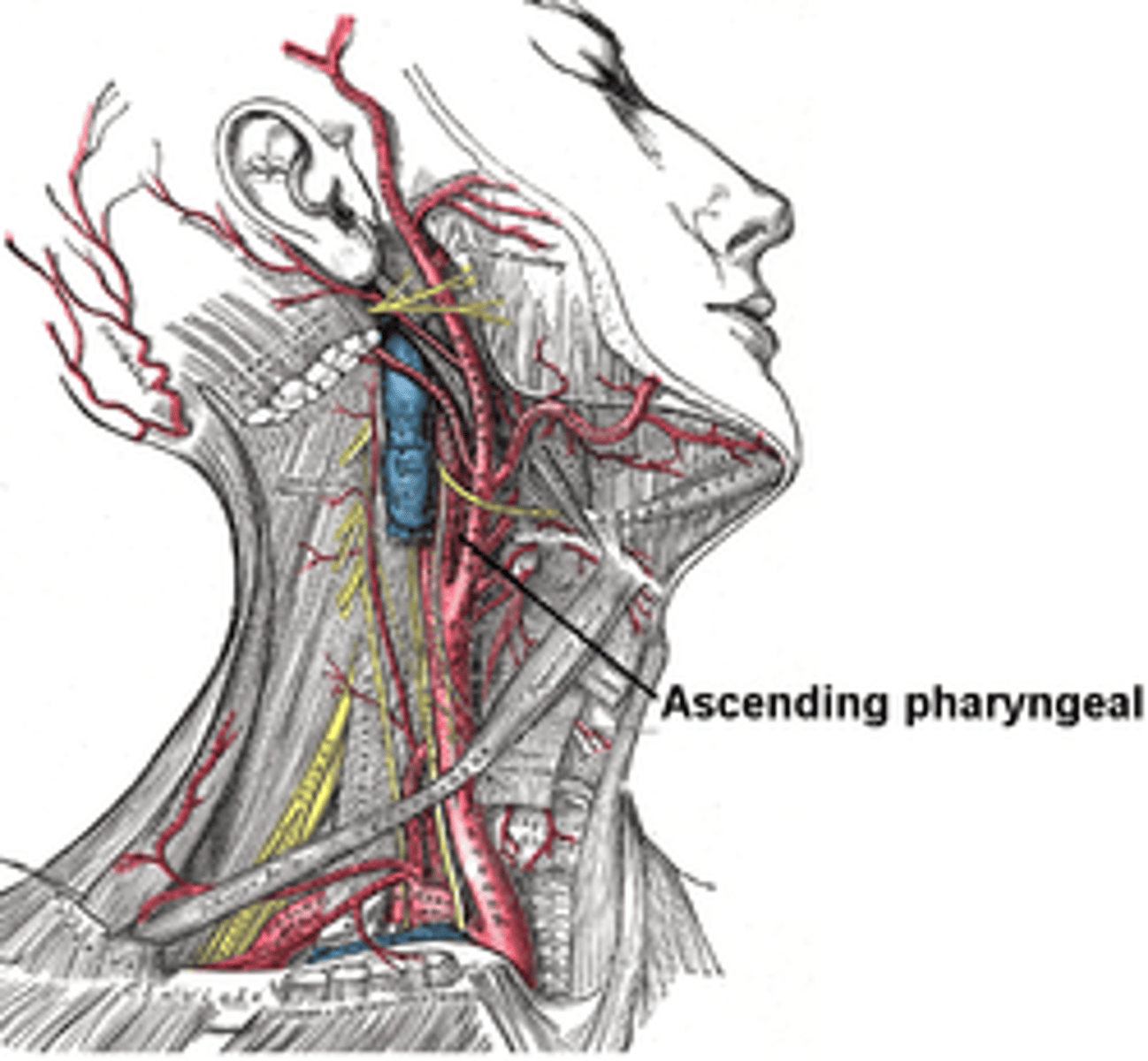
What is the origin of the ascending pharyngeal artery?
The ascending pharyngeal artery is a direct branch from the external carotid artery.
ASCENDING PHARYNGEAL ARTERY: BRANCH OF EXTERNAL CAROTID ARTERY
Which artery supplies the lower parts of the pharynx?
The pharyngeal branches of the inferior thyroid artery supply the lower parts of the pharynx.
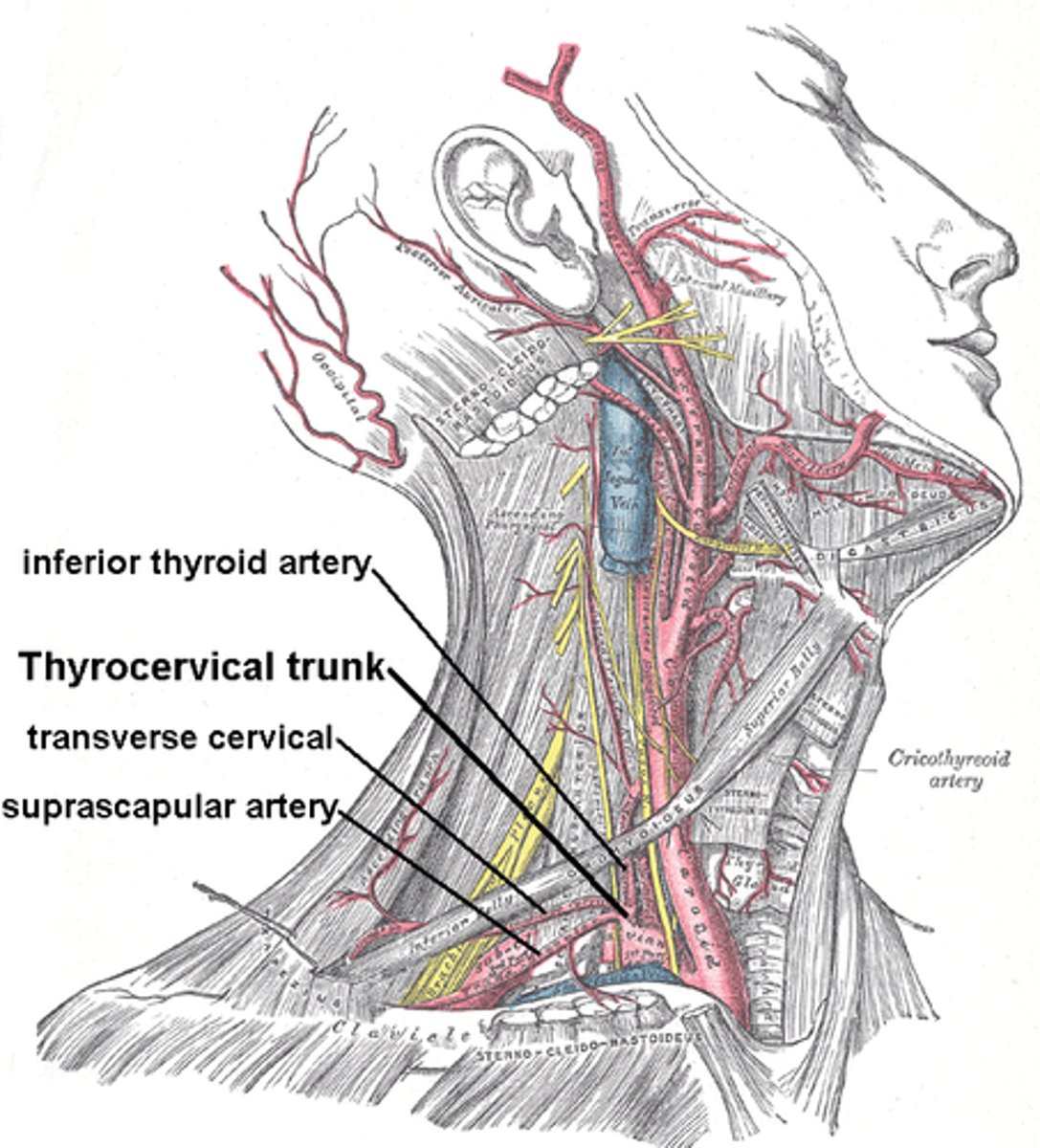
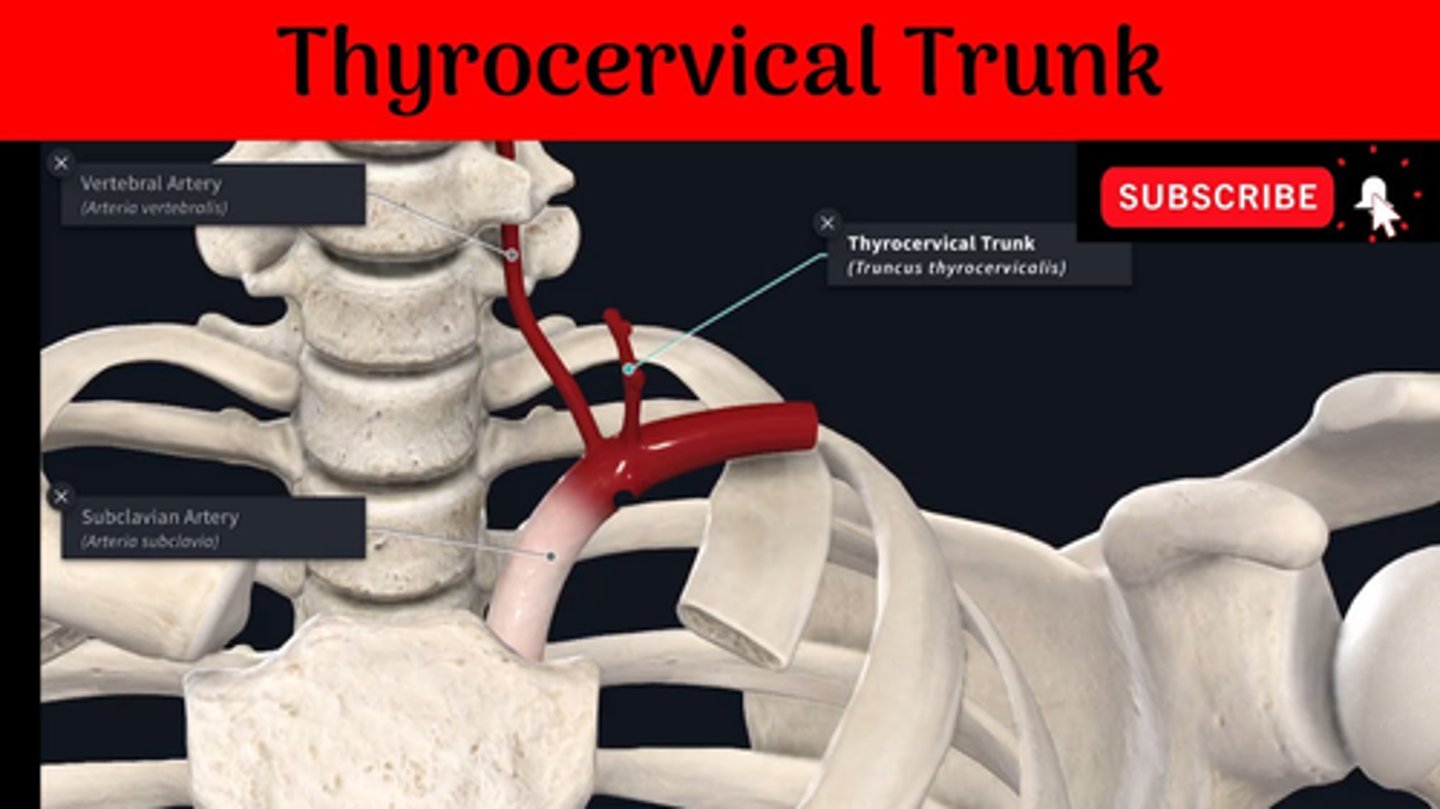
From which trunk does the inferior thyroid artery, which gives off pharyngeal branches, arise?
The inferior thyroid artery arises from the thyrocervical trunk.
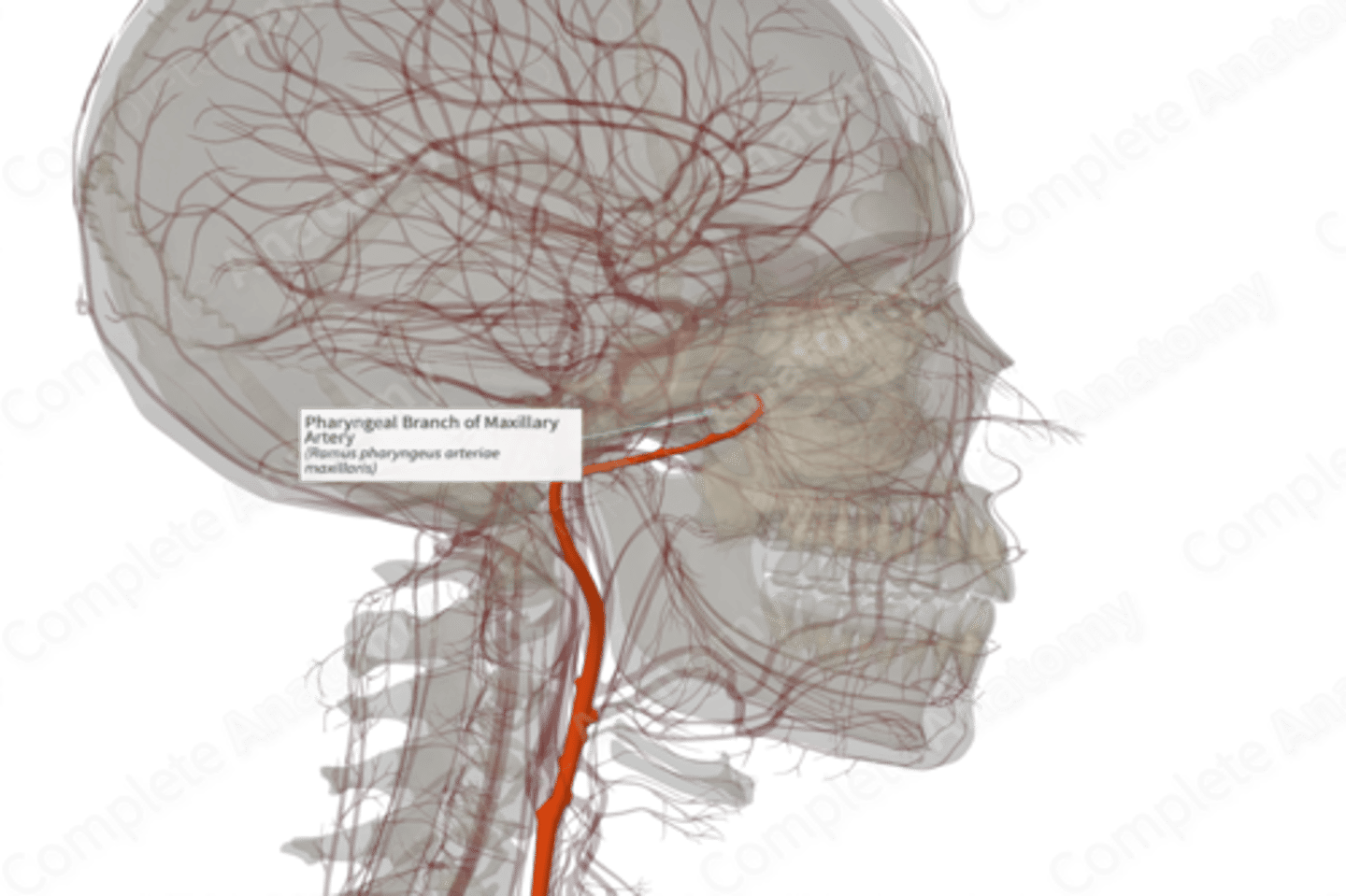
What area does the pharyngeal branch of the maxillary artery supply?
The pharyngeal branch of the maxillary artery supplies the roof of the nasopharynx.
Why is the knowledge of the tonsillar artery important during tonsillectomy?
Knowing the location of the tonsillar artery is crucial during tonsillectomy to prevent excessive bleeding, as the tonsils are richly vascularized and superficial.
Into which major vein do the veins of the pharynx primarily drain?
The veins of the pharynx primarily drain into the internal jugular vein.
How does the venous drainage of the pharynx compare to its arterial supply?
The venous drainage of the pharynx mirrors its arterial supply, with veins accompanying the arteries and draining into larger veins like the facial and lingual veins.
What is the significance of the vascular redundancy in the pharynx?
Vascular redundancy in the pharynx ensures consistent blood flow, even if one pathway is compromised, critical for the pharynx's function and healing.
Which artery's branches are involved in the vascularization of the pharynx BESIDES the facial artery?
Besides the facial artery, the external carotid, and branches from the maxillary and inferior thyroid arteries are involved in the vascularization of the pharynx.
What is the role of the ascending palatine artery in the pharynx?
The ascending palatine artery, a branch of the facial artery, supplies blood to parts of the pharynx and soft palate.
How do the pharyngeal branches of the inferior thyroid artery contribute to the pharynx's vascular network?
They supply blood to the lower regions of the pharynx, highlighting the integrated vascular network supporting the pharynx.
Which arteries are primarily responsible for the pharynx's arterial supply?
Branches of the external carotid artery, along with a branch from the thyrocervical trunk, are primarily responsible for the pharynx's arterial supply.
What is the significance of the pharyngeal branch of the maxillary artery?
It is crucial for supplying the nasopharynx's roof, ensuring this upper pharyngeal region receives adequate blood supply.
What surgical caution must be taken regarding the tonsillar vessels?
Surgeons must be careful not to damage the tonsillar vessels during procedures like tonsillectomy to avoid significant blood loss.
Which veins mirror the arterial supply in the pharyngeal region and where do they drain?
The pharyngeal veins mirror the arterial supply and mainly drain into the facial, lingual, and internal jugular veins.
What general sensory information does the glossopharyngeal nerve provide?
The glossopharyngeal nerve provides general sensory information from the mucosa of the posterior one-third of the tongue and the oropharynx.
Which areas of the tongue are innervated by the glossopharyngeal nerve for taste sensation?
The glossopharyngeal nerve innervates the vallate and foliate papillae in the posterior one-third of the tongue for taste sensation.
What type of afferent information does the glossopharyngeal nerve convey from the carotid sinus?
The glossopharyngeal nerve conveys visceral afferent information related to blood pressure changes from the carotid sinus.
What role does the glossopharyngeal nerve play in the baroreceptor reflex?
The glossopharyngeal nerve transmits information from baroreceptors in the carotid sinus to the brain to regulate blood pressure.
Where do the sensory fibers of the glossopharyngeal nerve terminate in the brain?
The sensory fibers of the glossopharyngeal nerve terminate in specific nuclei within the brainstem.
What kind of taste information is transmitted by the glossopharyngeal nerve?
The glossopharyngeal nerve transmits taste information from the posterior third of the tongue.
What is the significance of the glossopharyngeal nerve's somatic afferent innervation?
The somatic afferent innervation allows the detection of touch, pain, and temperature in the oropharynx and posterior third of the tongue.
How does the glossopharyngeal nerve contribute to the gag reflex?
The glossopharyngeal nerve provides sensory innervation that triggers the gag reflex when the oropharynx or posterior tongue is stimulated.
What visceral structures does the glossopharyngeal nerve monitor aside from the carotid sinus?
The glossopharyngeal nerve also monitors the carotid body, detecting changes in blood oxygen, carbon dioxide, and pH levels.
What is the function of the carotid body, and how is it related to the glossopharyngeal nerve?
The carotid body is a chemoreceptor that senses changes in blood gases and pH, and it communicates this information via the glossopharyngeal nerve.
What kind of papillae on the tongue are innervated by the glossopharyngeal nerve for taste?
The glossopharyngeal nerve innervates the vallate and foliate papillae for taste.
What role does the glossopharyngeal nerve play in cardiovascular homeostasis?
It plays a role in cardiovascular homeostasis by transmitting baroreceptor and chemoreceptor signals to the brain to regulate blood pressure and respiratory rate.
How is the sensory input from the glossopharyngeal nerve integrated into physiological responses?
Sensory input from the glossopharyngeal nerve is processed in the brainstem, which then coordinates appropriate physiological responses.
What is the relationship between the glossopharyngeal nerve and the tonsillar fossa?
The glossopharyngeal nerve provides sensory innervation to the tonsillar fossa, which is important for the gag reflex and overall oropharyngeal sensation.
Why is the glossopharyngeal nerve important in the sensory evaluation of the oropharynx?
It is crucial for providing sensory feedback that helps in the detection of stimuli, guiding reflexes, and ensuring the proper function of the oropharynx.
How does the glossopharyngeal nerve impact taste perception at the back of the tongue?
It transmits taste signals from the posterior third of the tongue, affecting the perception of taste, particularly bitter and umami flavors.
What is the role of special visceral afferent fibers in the glossopharyngeal nerve?
Special visceral afferent fibers carry taste sensations from the posterior one-third of the tongue.
How does the glossopharyngeal nerve's function relate to overall oral health and function?
It contributes to oral health by providing sensory feedback necessary for protective reflexes, taste, and the overall sensory experience of the oral cavity.¡
In what way does the glossopharyngeal nerve's sensory innervation affect medical procedures in the oropharynx?
Its sensory innervation is crucial for triggering reflexes like gagging, which need to be managed during procedures like endoscopies or intubations.
What is the clinical significance of the glossopharyngeal nerve in diagnosing oropharyngeal conditions?
Its sensory function can be assessed to diagnose conditions affecting sensation or taste in the oropharynx, or to detect abnormalities in reflexes like the gag reflex.