'4 Loop of Henle (tubule 2)'_241018_133259
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
22 Terms
Thick ascending limb
Part of the Loop of Henle impermeable to water that reabsorbs Na+, K+, and Cl-.
Transport of ions in thick ascending limb of the loop of henle
1Na+ 2Cl- & 1K+ enter cell via apical membrane symporter protein.
Cl- leaves cell by passive diffusion through basolateral Cl- channels.
Most K+ taken into cell leaks back into lumen via apical K+ channels (some K+ reabsorbed)
tubular lumen becomes positively charged relative to interstitium - drives paracellular diffusion of Na+, K+, Ca2+ & Mg2+.
Na+ also enters cell via Na+/H+ antiporter leading to HCO3- reabsorption (5-15%)
Na+ entering cells is then pumped out across basolateral membrane by sodium pump; low [Na+] provides electrochemical gradient which drives movement of Na+ from tubular fluid into cell
![<ul><li><p>1Na+ 2Cl- & 1K+ enter cell via apical membrane symporter protein.</p></li><li><p class="is-empty is-editor-empty has-focus">Cl- leaves cell by passive diffusion through basolateral Cl- channels.</p></li><li><p class="is-empty is-editor-empty has-focus">Most K+ taken into cell leaks back into lumen via apical K+ channels (some K+ reabsorbed) </p><ul><li><p class="is-empty is-editor-empty has-focus">tubular lumen becomes positively charged relative to interstitium - drives paracellular diffusion of Na+, K+, Ca2+ & Mg2+.</p></li></ul></li><li><p class="is-empty is-editor-empty has-focus">Na+ also enters cell via Na+/H+ antiporter leading to HCO3- reabsorption (5-15%)</p></li><li><p class="is-empty is-editor-empty has-focus">Na+ entering cells is then pumped out across basolateral membrane by sodium pump; low [Na+] provides electrochemical gradient which drives movement of Na+ from tubular fluid into cell</p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/bcc14585-6c15-4a9d-8917-d345a84a2d5a.jpg)
Thin Ascending Limb
Part of the Loop of Henle that is permeable to sodium and chloride but not to water, allowing for passive reabsorption of solutes
Descending thin limb of loop of henle
highly permeable to water (AQP1).
Much less to NaCl & urea; movement largely passive
Function kf loop of henle in renal concentration mechanism and osmoregulation
markedly reduces osmolality of tubular fluid (becomes hypo-osmotic): Thick ascending limb of loop of Henle also known as “diluting segment”.
makes interstitial fluid of medulla hyperosmotic. This causes osmotic removal of water from descending limb and collecting duct
Thick ascending limb of loop of Henle thus has important role in creating concentrated medullary interstitium & thus in regulating urine osmolality & thus osmotic balance of body.
After passage through loop of Henle, tubular fluid reduced in volume by further 5% and, because of reabsorption of NaCl, is hypoosmotic with respect to plasma as it enters distal convoluted tubule
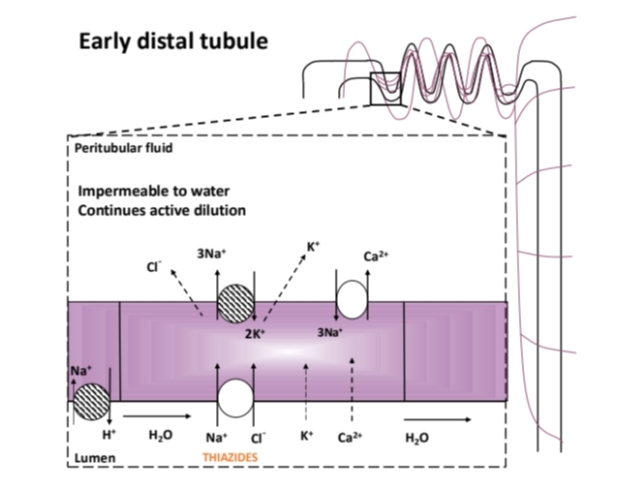
Early Distal Tubule
A nephron segment where Na+ and Cl- are actively reabsorbed, but water remains unabsorbed. Which continues active dilution of tubular fluid that began in thick ascending limb.
Ion transport in early DCT
Na+ pump in basolateral membrane (interstitium facing) drives transport of many of the other solutes.
Na+ & Cl- enter cell across apical membrane (filtrate facing) by Na+, Cl-symporter. Cl- leaves by diffusion through Cl- channels.
Ca2+ and Mg2+ reabsorption.
K+ : some remaining filtered K+ reabsorbed (by the time filtrate reaches collecting ducts almost all (95%) filtered K+ has been reabsorbed).
H+: secreted mostly by Na+-H+ exchange, or by a H+ pump. Secreted H+ ions either contribute to reabsorption of any remaining bicarbonate or interact with urinary buffers to allow acid excretion
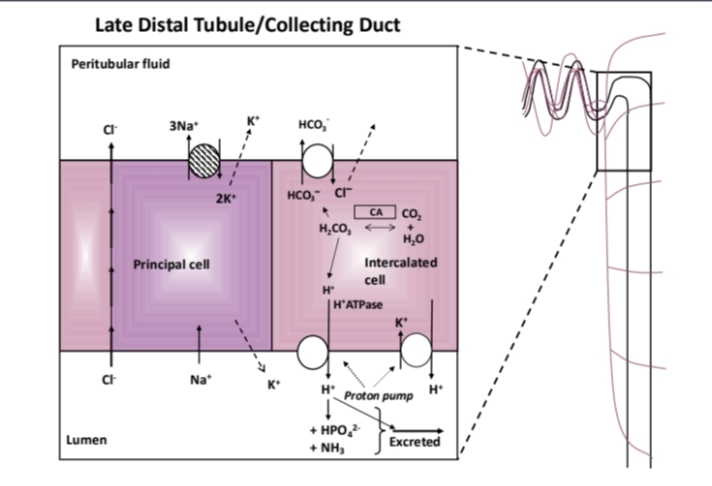
Late distal tubule/collecting duc
Principal cells: reabsorb Na+ and water, secrete K+ which depends on activity of Na+ pump.
Intercalated cells: secrete H+, reabsorb HCO3- & K+
Generation of “new” HCO3- and H+ inside cells due to high cytoplasmic concentrations of carbonic anhydrase (CA); important in acid-base balance; net gain of blood HCO3- (not a replacement for filtered HCO3-).
H+ secretion mainly by H+ATPase (minor role of K+H+ATPase).
Secreted H+ excreted as free H+, or buffered with HPO42- to form H2PO4- and ammonia (NH3) to form ammonium (NH4+)
Hormones affecting water & solute handling in LDT & CD
Aldosterone
ANP
ADH/vasopressin
Action of aldosterone on LDT and CD
Na+ reabsorption (principal cells)
K+ secretion (principal cells)
H+ secretion (intercalated cells)
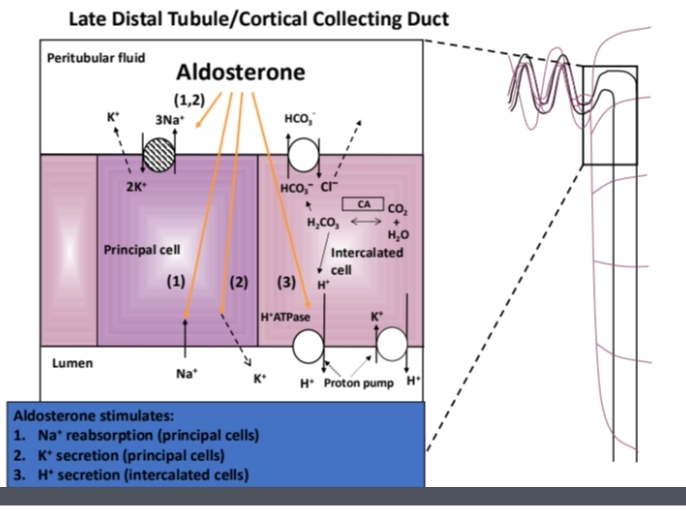
Hyperaldosteronism
aldosterone excess that leads to metabolic alkalosis, hypokalaemia, hypertension and oedema due to Na+ and water retention)
Hypoaldosteronism
Type 4 renal tubular acidosis, RTA: leads to hyperkalaemia. Also, a feature of many patients who have Addisons disease
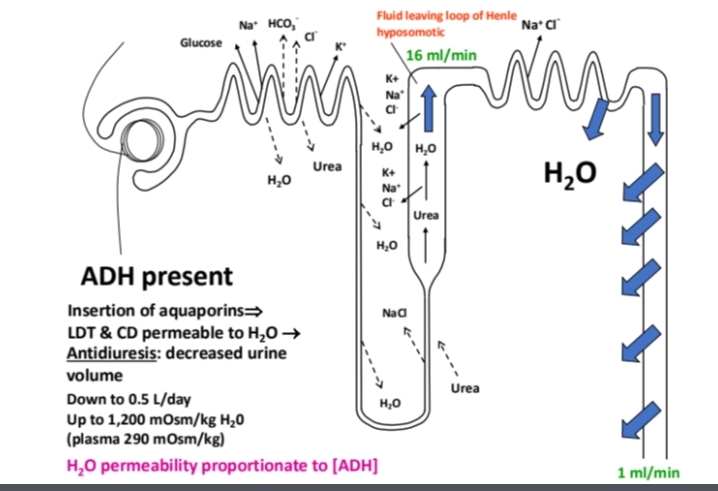
ADH (Antidiuretic Hormone)
A hormone that increases water reabsorption in the late distal tubule and collecting duct.
With maximal levels of ADH tubular fluid reaches osmotic equilibrium with interstitial fluid as it flows down collecting duct
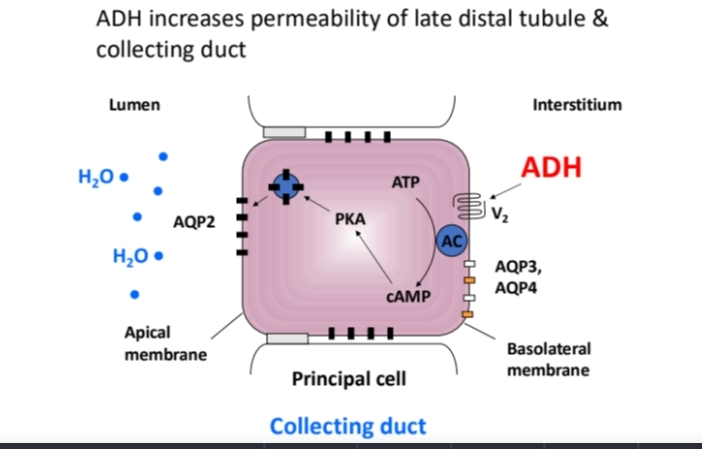
Aquaporins
Water channel proteins that facilitate the transport of water across cell membrane in response to ADH.
Diuresis
Increased urine production often due to the absence of ADH.
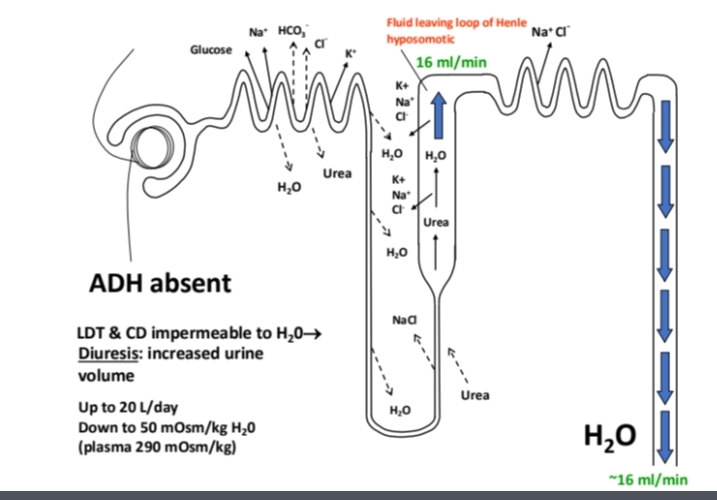
Antidiuresis
ADH is present so increases permeability by stimulating insertion of aquaporins (water pores; AQP2) into apical membrane (mainly principal cells)
water exits tubule lumen by osmosis into interstitial tissue making concentrating urine
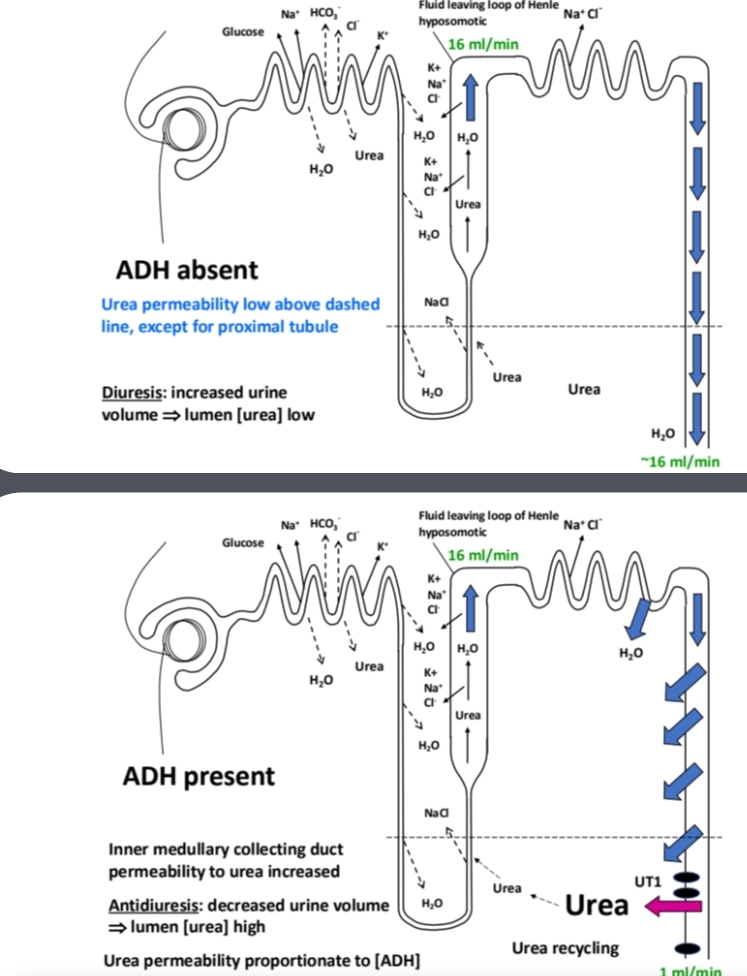
Urea Recycling
The process where urea is reabsorbed and contributes to the osmotic gradient in the kidney.
Urea reabsorption helps to maintain the osmotic gradient between the interstitium & collecting duct lumen (at a time when water reabsorption would dissipate medullary interstitial osmotic gradient).
Urea then diffuses into descending and ascending limbs of loop of Henle
ADH function on urea in CD
There is an ADH-dependent, facilitated diffusion urea transporter (UT1) on the apical membrane in the IMCD. In presence of ADH there is therefore and increase permeability of IMCD (inner medullary collecting duct) to urea
Diabetes Insipidus
A condition characterized by the excretion of large amounts of dilute urine due to inadequate ADH secretion or response, leading to polyuria (increased urine output) and polydipsia (increased thirst).
central diabetes insipidus
insufficient production of ADH leading to excretion of large amounts of dilute urine
nephrogenic diabetes insipidus
kidneys not responding to ADH so there is excretion of large amounts of dilute urine
Can be genetic eg inadequate V2 receptor or AQP2 genene
SIADH (Syndrome of Inappropriate Secretion of ADH)
A condition characterized by excessive release of antidiuretic hormone (ADH) leading to water retention, hyponatremia (low sodium levels), and concentrated urine.
Common causes include central nervous system disorders, malignancies (especially small cell lung cancer), certain medications, and pulmonary diseases.