Dermatology
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
What are the main functions of bovine skin?
Provides shape and form
Acts as an enclosing barrier
Regulates temperature
Produces adnexa (hair, glands)
Serves as a reservoir
Contributes to immunoregulation
Responsible for sensory perception
What causes dermatophytosis in cattle, and how is it spread?
Ringworm → Caused by Trichophyton verrucosum and T. mentagrophytes
Very common in cattle
Transmission: direct animal-to-animal contact and fomites

What conditions predispose cattle to ringworm infections?
Young animals
Overcrowding
Poor nutrition
Indoor housing
Warm, humid environments
How does dermatophytosis develop, and how does it present?
Fungus invades fully keratinized tissue (non-living)
Typically affects head and trunk
Appearance: multifocal alopecia, heavy crusting, possible ring pattern
Erythema may be absent or hidden under crusts

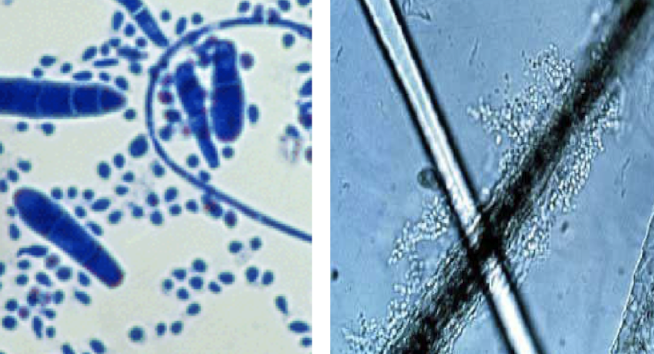
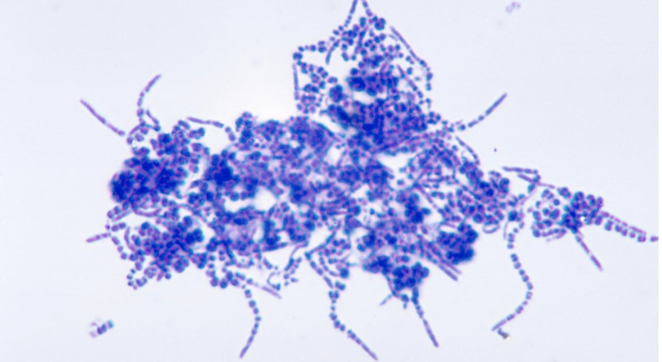
What diagnostic methods are used for dermatophytosis?
Direct microscopy: skin scraping or hair-shaft exam
Fungal culture: use broken hairs, avoid large crusts, use specialized media
How is dermatophytosis treated?
Topicals: lime sulfur, enilconazole, miconazole/ketoconazole shampoos, 3–4% chlorhexidine
Vaccines available for T. verrucosum and T. mentagrophytes
(Also often self-limiting)

What organism causes dermatophilosis and under what conditions does it proliferate?
Caused by Dermatophilus congolensis
Requires moisture + skin damage → zoospores germinate → penetrate epidermis
Spread by direct contact or mechanical vectors; chronic carriers are common
Where do lesions commonly appear, and what do they look like?
Sites: distal limbs, dorsum, muzzle, pinnae
Lesions: encrusted, proliferative dermatitis; papules, ulcerations, pus-filled crusts; alopecia
(“Paintbrush” lesions)

What key diagnostic finding is characteristic for dermatophilosis?
Impression smear showing railroad-track cocci
Can also use bacterial culture, histopathology, PCR
What is the recommended treatment approach?
Remove animals from moisture
Remove crusts
Topicals: iodophors, lime sulfur
Systemic therapy only if severe: penicillin, TMS, long-acting oxytetracycline

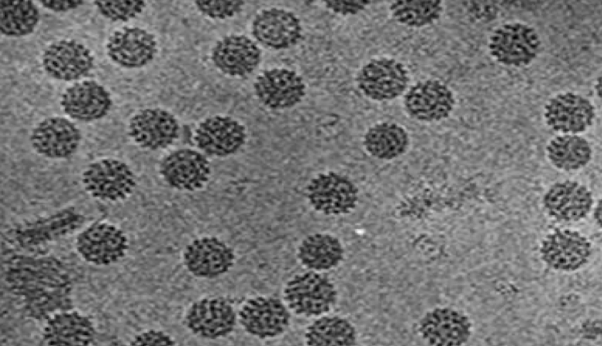
Which species are commonly affected by papillomas and what is the typical course?
Cattle: very common; appear <2 yrs; often regress; problematic on teats, penis, interdigital space, GI
Bovine papillomavirus (BPV)
Carcinogenic, double-stranded DNA
Generally species-specific (one exception exists)
Site-specific; >20 types; 5 major subgroups
Goats: rare; head/neck or mammary
Sheep: rare

What are the five morphologic types of papillomas?
Typical — cauliflower
Pedunculated — narrow base
Atypical — flat, broad base
Filamentous — thin base, keratinized
Rice-form — very small
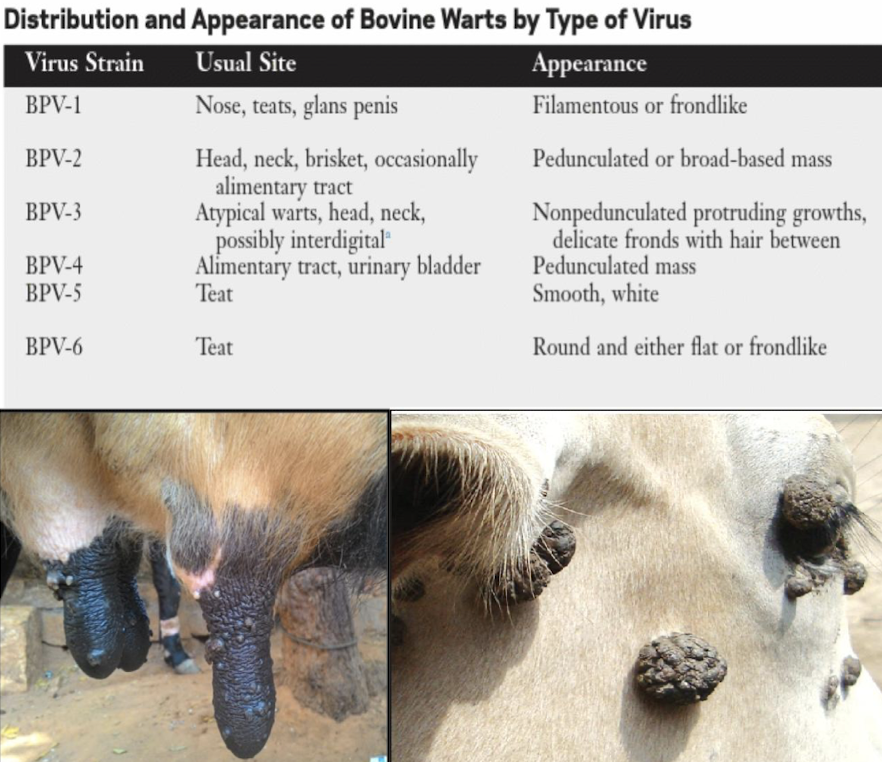
How do papillomas spread and how are they diagnosed?
Transmission: direct contact, fomites (dehorning, tagging tools)
Diagnosis: clinical appearance, biopsy, serology, PCR
What are the management and treatment options for papillomas?
“Benign neglect” (most regress)
Crushing, surgical removal, cryotherapy
Autogenous vaccines
Prevention: isolate, disinfect shared equipment, commercial/autogenous vaccines

What are the key identifying features of pseudocowpox?
Cause: parapoxvirus
Distribution: teats (most common), sometimes udder or scrotum
Lesion progression: 2–3 mm papules → crust → circular spread → horseshoe/ring-shaped scabs in ~10 days
Zoonotic (“milker’s nodules” on hands)

What virus causes Bovine Herpes Mammillitis and what lesions develop?
Caused by Bovine Herpesvirus-2 (BHV-2)
May be epidemic or endemic
Distribution: oral, udder, or generalized
Lesions: edema, pain, vesicles → ulcers → scabs

How is Bovine Herpes Mammillitis diagnosed and managed?
Diagnosis: virus isolation, serum neutralization, histology
Treatment: ulcers heal in 3–10 weeks; topical or systemic antimicrobials for secondary infection
Management: segregate(wean), milk last, disinfect equipment, hand hygiene
What are the two forms of Bovine Cutaneous lymphosarcoma noted in cattle?
Systemic lymphoma — BLV positive; may involve skin secondarily
Cutaneous form — very rare; <3 years old; BLV negative
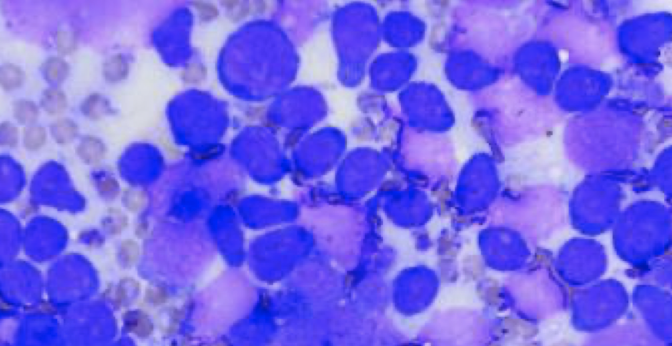
What does cutaneous lymphosarcoma look like and how is it treated?
Distribution: neck, shoulders, back, croup
Appearance: intradermal plaques with white-gray scabs
Diagnosis: biopsy
Treatment: may regress spontaneously; returns if systemic lymphoma develops; supportive care

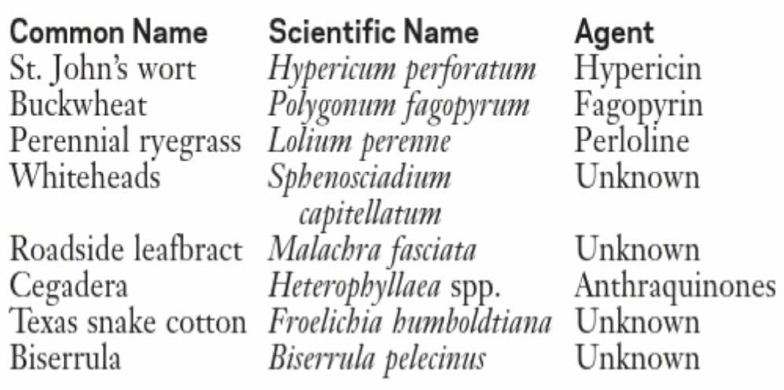
What are the three types of photosensitization in cattle?
Type I: ingestion of photodynamic agent
Type II: congenital porphyrin metabolism abnormality
Type III: liver disease → phylloerythrin accumulation
Requirements: photodynamic agent, lightly pigmented skin, UV-A exposure
What areas are affected and what lesions are seen?
Distribution: hairless or lightly pigmented skin
Lesions: erythema, edema, painful skin → blisters, exudation → thickening, fissures → necrosis & sloughing
Clinical signs may also reflect liver disease (if Type III)

How is photosensitization diagnosed and treated?
Diagnosis: characteristic lesions, plant exposure history, elevated liver enzymes, liver biopsy, post-mortem
Treatment: remove toxin source, avoid sunlight, wound management, feed low-quality grass hay or cereal hay (reduce chlorophyll intake)