Clin Med: Pulm (3)
1/88
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
89 Terms
asthma pathophysiology
what is the cause?
manifestation?
acute? chronic?
how is expiratory airflow changed? FEV1 and FEV1/FVC?
cause: AIRWAY INFLAMMATION
manifestation: wheezing
chronic, inflammatory lung disease
prolonged expiratory airflow (decrease I/E ratio) where FEV1 and FEV1/FVC <80% predicted
asthma signs and symptoms (4)
increased airway responsiveness (mechanism) due to triggering stimuli leading to:
cough
wheezing
dyspnea
chest tightness
triggering stimuli for asthma
Nonspecific stimuli includes stress, exercise, lack of sleep
Environmental triggers include viral URI’s, environmental pollutants, allergens, cold air
asthmatic events
are they reversible?
how?
partially OR completely reversible w/ use of bronchodilator (improves expiratory airflow by at least 12%)
hallmarks of asthma (things that result in airflow obstruction) (7)
smooth muscle hypertrophy (narrows airways)
muscle thickening → encroaches on airway lumen
airway wall edema
edema = fluid leaking to interstitial
intraluminal mucus hypersecretion and accumulation
mucus cells hyper secrete → airway full of mucus
inflammatory cell infiltration
basement membrane thickening
BM is b/w endothelial cells + capillary beds
due to general ischemic of airway
neovascularization
new blood vessels grow b/c of chronic hypoxic issues
not good long-term b/c they rupture easily and cause blood accumulation in tissue
epithelial injury
nocturnal aggravation of asthma (5)
what is a rare complication?
circadian production of histamine (inc at night, can cause bronchoconstriction)
dust mites in pillow
dust blowing from fans/furnace
GERD (recumbency)
lying flat → acid regurg → coughing/bronchospasm
OSA
rarely, remodeling can happen over years
asthma epidemiology
who is more likely to have asthma?
most common chronic disease where?
what regional differences?
does city/rural/surburban living affect chances of having asthma?
more likely to have asthma: children, women, african and hispanics
most common chronic disease in childhood in developed country
residents of northeast and midwest more likely (Regional diffs)
chances of having asthma is unrelated to city vs. rural/suburban living
asthma associated condition in adults (10)
Atopy (A like Apple, Topy like Tby with P): atopic dermatitis, allergic conjunctivitis/rhinitis, asthma
Most people with atopy have asthma to some degree
Atopy also runs in families, fun facts
Obesity (associated with higher asthma rates)
Chronic sinusitis
GERD
OSA
Stress/Depression
Exercise
Food allergies
Vocal cord dysfunction
Allergic bronchopulmonary aspergillosis (rare)
asthma associated conditions in children (5)
RSV
Foreign body aspiration
Bronchopulmonary dysplasia (due to treatment given to children)
Cystic fibrosis
Obesity
risk factors for asthma (4)
Host factor
Genetic predisposition
Gender
Race
Environmental
Viral infections
animal/airborne allergens
Smoke
Aspirin or NSAIDs hypersensitivity
Use of B blockers
Sympathetic NS helps bronchodilate through B2 receptors
If you use BB→ inhibits bronchodilation → can worsen bronchospasm
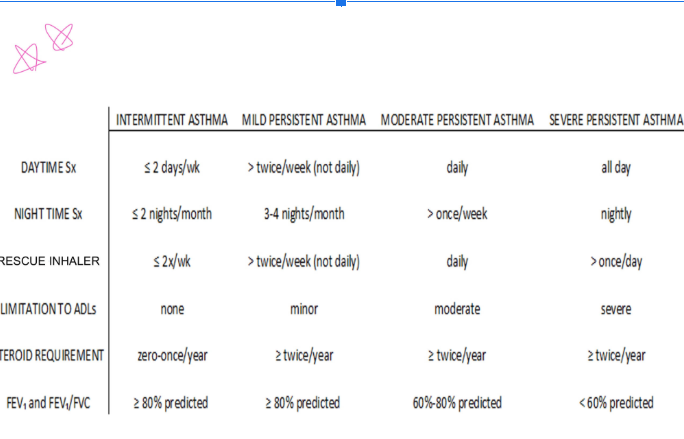
Intermittent Asthma
how often daytime asthma symptoms occur?
awaken at night?
use of rescue inhaler?
filling of rescue inhaler prescription?
requires oral glucocorticoids?
interference with normal activities b/w exacerbations?
FEV1 and FEV/FVC ratio?
Daytime asthma symptoms occurring =< 2 days/wk
Awakened by sometimes =< 2 nights/month
Use of rescue inhaler =<2x/wk
Filling of rescue inhaler prescription =< 2x/year
<2 exacerbations/yr requiring oral glucocorticoids
No interference with normal activities between exacerbations
Between exacerbations, FEV1 and FEV/FVC ratio that are consistently >= 80% of predicted normal
During exacerbations, your PFTs might be off
Most exercise induced asthma would fall under this category ^^
mild persistent asthma
how often daytime asthma symptoms occur?
awaken at night?
use of rescue inhaler?
filling of rescue inhaler prescription?
requires oral glucocorticoids?
interference with normal activities b/w exacerbations?
FEV1 and FEV/FVC ratio?
Symptoms more than 2x/wk (but not daily)
3-4 nocturnal awakenings/month due to asthma
Use of rescue inhaler to relieve symptoms more than 2x/wk but not daily
Filling of rescue inhaler prescription >2x/year
2 or more exacerbations/yr requiring oral glucocorticoids
Minor interference with normal activities
FEV1 and FEV1/FVC ratio between exacerbations are >= 80% of predicted
moderate persistent asthma
how often are symptoms?
nocturnal awakening?
rescue inhaler usage?
requiring oral glucocorticoids?
limitation?
FEV1 and FEV1/FVC?
Daily symptoms
Nocturnal awakening more than once per week
Daily relief for rescue inhaler for symptom relief
2=+ exacerbations/yr requiring oral glucocorticoids
Moderate limitation in normal activity between exacerbations
FEV1 and FEV1/FVC = 60-80% predicted
severe persistent asthma
how long are symptoms?
nocturnal awakening?
glucocorticoids?
limitations?
FEV1 or FEV1/FVC ratio?
important note?
Symptoms of asthma all day
Nocturnal awakening nightly
CAN EVENTUALLY CAUSE ARCHITECTURE CHANGE (asthma -> COPD)
2=+ exacerbations/yr requiring oral glucocorticoids
Extreme limitation in normal activity between exacerbations
FEV1 or FEV1/FVC ratio between exacerbations are <60% predicted
asthma symptoms chart
asthma history (4)
Wheezing, cough, dyspnea on exertion, chest pain/burning
asthma physical exam
general (3)
severe cases (4)
cardio-respiratory failure (4)
Wheezing, hyperresonance to percussion (hyperexpanded), tachypnea
In more severe cases:
Wheezing decreases (they’re not moving air anymore = no turbulence)
Pt unable to lie flat, speak full sentences
Use of accessory muscles, intercostal retractions
Intercostal muscles, sternocleidomastoid, internal scalene muscles
Nostril flaring b/c of nasalis muscle
Diaphoresis
Impending cardio-respiratory failure (
Silent chest (not moving any air anymore)
Cyanosis (not oxygenated)
Mental status changes (brain is becoming hypoxic)
Patient appears in extremis (generally looks bad = extremis)
tests for asthma (5)
Blood: might find eosinophilia or elevated serum IgE levels (mediators in a Type I sensitivity reaction)
Spirometry: Normal test does not rule out asthma
If reduced predicted ratio of FEV1/FVC reverses (12% increase) with bronchodilators = asthma (specific test)
Broncho-provocation: (methacholine, histamine, cold air, or exercise) to stimulate bronchoconstriction, useful in atypical presentation/normal baseline spirometry
Abnormal test result not entirely specific for asthma, but a normal test result excludes asthma (sensitive test)
Peak expiratory flow rate: used for MONITORING of symptoms and for following efficacy of treatment. DO NOT use for diagnosis
Chest x-ray: (for excluding alternative/complicated diagnosis. during asthma attack, lungs are hyperinflated, diaphragm is flattened)
controlling triggers of asthma
Hard to avoid: URI, hormonal fluctuations, exercise, emotions, cold air
Inhaled allergens: pollen, dust mites, molds, animal dander, and cockroaches (use air purifier, change your pillow, vacuum)
Respiratory irritants: tobacco smoke, wood smoke (think molds) from stoves or fireplaces, strong perfumes and other chemical vapors, and air pollutants
meds that aggravate asthma (4)
beta blockers
Aspirin
non-COX 2 selective non-steroidal anti-inflammatory
sulfites (beer, wine, processed potatoes, sauerkraut, dried fruit, shrimp)
beta blockers aggravating asthma
what do they do?
why is this an issue if you are using a BB and pt has asthma/COPD exacerbation?
can trigger a asthma attack (esp non-selective BB like propranolol)
blocks B2 receptors in lungs (B2: bronchodilation)
if pt is on BB and has asthma/COPD exacerbation, beta-agonist bronchodilators may not work well because the receptors they target are already blocked
→ use selective B2 agonists and avoid non-selective BB
you can use beta 1 blockers but be careful if they have heart disease/asthma
atopy triad
atopic dermatitis (eczema)
asthma
allergic rhinitis (hay fever)
cardioselective beta blockers
Metoprolol (Toprol)
Atenolol (Tenormin)
Bisoprolol (Zebeta)
Betaxolol (Betopic, for glaucoma eye drops)
Acebutolol (Sectral)
aspirin and non-cox2 selective non-steroidal anti-inflammatory drugs aggravating asthma
what population can this trigger asthma symptoms?
what condition can lead to higher risk of aspirin-exacerbated respiratory disease?
what asthma is uncommon in children?
what asthma is common with children?
can trigger asthma symptoms in 3-5% ADULT pts
asthma pts with nasal polyps have higher chance of getting aspirin-exacerbated respiratory disease (known as “Triad Asthma” or Samter’s Triad)
aspirin-sensitive asthma (and Samter’s Triad) UNCOMMON in children
asthma associated with atopy is COMMON in children
Samter’s Triad
asthma, aspirin, and nasal polyps
immunizations for asthmatics
can asthmatics get flu shots?
flu mist spray vs. flu vaccine?
when should you not get a shot?
all asthmatics can get flu shots
flu mist spray: used for healthy ages 2-49 not pregnant and no asthma (b/c they have a live, intenuated virus)
flu vaccine: NOT live virus
children 6-24 months should be vaccinated IM
no shots if under 6 months
>8 y/o = 2 doses (second “half dose” = booster)
Pneumovax as indicated
pharmacotherapy for asthma
how should pt with mild and infrequent symptoms be treated?
intensity of tx should match severity of asthma symptoms (if they have qualities of different categories, treat as the one they’re more severe in)
pt with mild and infrequent symptoms = treated intermittently with rescue inhaler (non-sched fashion)
rescue inhalers
consist of formoterol/budenoside (symbicort) or formoterol/beclomethasone (Fostair)
A second choice is use of a pure SABA such as albuterol. The goal is quick relief of symptoms (I.e. rescue treatment)
escalating use of rescue inhaler
how much?
what is this a warning sign of?
>6-8 puffs/day from MDI (multi-dose inhaler) or use exceeding one canister per month
warning sign that patient’s underlying disease activity is not adequately controlled
patient with mild-severe persistent asthma
what tx should they get?
scheduled meds AND rescue treatment
asthma pharmacotherapy Rule of 2’s
If answer is yes to any of these, asthma is not in optimal control = persistent-type asthmatic category
Do you:
Have symptoms >2 days a week
Use a rescue inhaler >2 times a week
Have nighttime symptoms > 2 times a month
Refill rescue inhaler > 2 times a year
Have a peak flow during exacerbation that is less than 2 times 10% (20%) from baseline (Shows severity of exacerbations)
short acting beta agonists (SABAs)
examples
what happens with repeated exposure?
good?
bad?
what is something you can add to SABA to offset some of the effects?
albuterol, levalbuterol, pirbuterol delivered by a HFA MDI (hydrofluoroalkane metered dose inhaler) or nebulizer, for bronchodilation
associated with increased airway hyper-responsiveness, increased allergic response, and increased eosinophilic infiltration of bronchial tissues
Good: the time of onset is very short/fast-acting drug
Bad: the more you use rescue inhaler beta agonist, the more the beta receptors decrease in number on the cell membrane and decrease in sensitivity to agonist = downregulating regulator. Risk of not working anymore (uh oh!)
Repeated exposure to SABAs → drug less effective over time → risk of failure at crucial time of needed
If you add steroid to short-acting beta agonist, you offset some of the loss in receptor number and sensitivity, allergic reaction responses, and eosinophilic infiltration of the bronchial tissues
inhaled glucocorticoids (steroids) - 2nd tier
what is this good for? what should you add to this for that?
____ agent of choice for pt with persistent asthma
good? (3)
bad (3)
good maintenance drug/therapy
scheduled inhaled glucocorticoids are the primary treatment used to reduce airway inflammation and prevent symptoms
second agents of choice for pts w/ persistent asthma (after rescue inhalers)
reduces frequency of symptoms (and need for inhaled bronchodilators), improves overall quality of life, and decreases risk of exacerbations (can use nebulized form)
NOT for rescue, onset is slow, do NOT use alone for COPD
inhaled glucocorticoid examples (4)
Budesonide (Pulmicort) - available for nebulization or MDI
Mometasone (Asmanex)
Fluticasone (Flovent)
Beclomethasone (QVar)
long-acting beta agonists (LABAs) - 3rd tier
can you use alone?
what should this be combined with?
examples of LABA
what are combination inhalers? when are they preferred?
warning with LABA?
Bronchodilators, but do NOT use alone as long-term controllers
MUST BE USED COMBINED with inhaled gluco-corticoids (steroids) for asthmatics
Examples include salmetrol (Serevent) and formoterol (Foradil)
Combination inhalers have LABA and a ICS, used when ICS alone is not enough to control asthma symptoms
Preferred in all forms of persistent disease (Advair, Symbicort, Dulera)
Repeated exposure to LABAs → drug less effective over time → risk of failure at crucial time of needed
muscarinic antagonists (SAMAs and LAMAs) - 4th tier
cholinergic effects
what is a result of anticholinergic agents?
AKA anticholinergic agents
cholinergic mediates effects of parasympathetic system, which induces bronchial smooth muscle contraction (nono!)
using anticholinergic agents blocks cholinergic receptors = no bronchospasm
short acting muscarinic agents (SAMA) - 4th tier
example
when are they useful?
better for acute or maintenance tx w/ SABA?
what other drug can SAMA be combined with?
speed of effectiveness
Ipratopium bromide (Atrovent): short acting and useful in nebulized form
SAMA + SABA combo for acute treatment (rather than maintenance)
SAMA + albuterol: dunoeb (beta 2 agonist + muscarinic antagonist) and in MDI as combivent
Takes a while to work/slow
long acting muscarinic agents (LAMAs)
examples
when are they useful?
why are they not good for rescue/monotherapy?
add-on treatment for what patients?
warning
Tiotropium, aclidinium, umeclidinium, and glycopyrrolate
long acting and useful in control of moderate and severe persistent asthma
NOT good for rescue/monotherapy b/c they work slower (30 mins) and causes less bronchodilation compared to beta 2 agonist
add-on treatment for pts who are on medium dose ICS-LABA
high risk of severe exacerbations
should be used first before muscarinic/anticholinergic agents
beta agonist
leukotriene inhibitors - 4th tier (others)
what do leukotrienes do?
are they as effective as inhaled glucocorticoids?
when is this the drug of choice?
drug examples w/ dose
rare case reports what? what do you do as a result?
Block leukotrienes = less inflammation, allergic response, and bronchoconstriction
In general, not as effective as inhaled glucocorticoids
Drugs of choice in aspirin-sensitive asthmatics
Zafirleukast (Accolate) 20 mg po bid and monteleukast (Singulair) 10 mg po qd
Rare case reports of depression and SI (screen before and during treatment)
Lipoxygenase pathway inhibitor - 4th tier (others)
drug example
when would you consider using this?
Zileuton (Zyflo); adjunctive (additional therapy) treatment in patients >= 12 years
arachidonic acid pathway
prostaglandins and leukotrienes are the two formed in this pathway
in cell membrane, a membrane lipid → makes leukotrienes and PGE
if cell has phospholipase-A2, then the membrane lipid → arachidonic acid
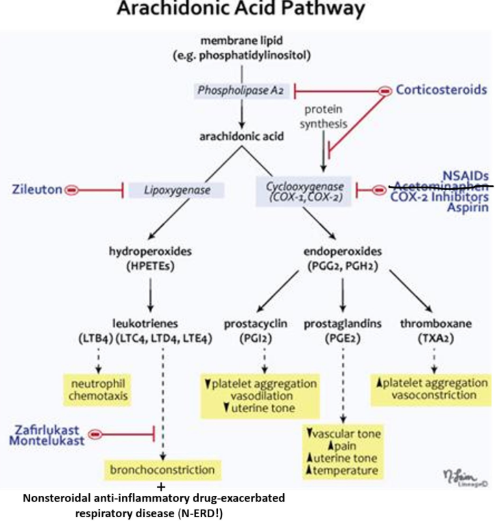
prostaglandin part of arachidonic acid pathway
arachidonic acid using COX-1 and COX-2 → converted to endoperoxides (PGG2, PGH2) → prostaglandins, prostacyclin, and thromboxane
endoperoxides
progenitor (parent/”before”) for prostaglandins
prostacyclin effects (2)
decreases plt aggregation and uterine tone, vasodilates
prostaglandins effects (4)
mediator of pain
increases uterine tone
increases temp (fever)
decreases vascular tone
thromboxane
increases plt aggregation = vasoconstriction
leukotrienes part of arachidonic acid pathway
arachidonic acid with lipoxygenase → HPETES → leukotrienes
lipoxygenase
converted to hydroperoxides (HPETEs) → makes leukotrienes
hydroperoxides
progenitor (before) for leukotrienes
leukotrienes
chemo-taxic agents, makes neutrophils move around. lots of these = bronchoconstriction. in an asthmatic, making too much leukotriene will trigger asthma
corticosteroids
inhibits phospholipase A2 and certain protein synthesis needed to make COX-1 and COX-2
High up on the list. If you can block the pathway up there, you’ll get less stuff coming out of it
NSAIDS, ASA, and COX-2 inhibitors
what do they do?
effects (4)
block COX-1 and COX-2’s ability to convert arachidonic acid -> endoperoxides
effects:
less pain (they block prostaglandins, which is a mediator of pain)
good for fever
anti-inflammatory (they block prostacyclin and thromboxane)
INCREASE formation of leukotrienes (b/c the PGE path is blocked) → bronchoconstriction
Nonsteroidal Anti-inflammatory Drug-exacerbated Respiratory Disease (N-ERD)
Taking NSAIDs (which block COX-1 enzyme) → shift toward the leukotriene pathway → triggers bronchoconstriction
Zileuton
block the formation of leukotriene side of the cascade because you block lipoxygenase
steroid + fast acting medicine
the preferred combo for inhalers
ie: formoterol + ICS (like Symbicort) = daily control and rescue
albuterol + steroid is good too
LABA
should NEVER be used by itself - use with a steroid
Theophylline - 4th tier (other)
good
bad
Good: inexpensive, may have anti-inflammatory and immunomodulary effects in low doses (lower than amt needed for bronchodilation effects), bronchodilator
Bad: low therapeutic index -> theotoxicity and many drug interactions
immunosuppressive agents - 5th tier
systemic corticosteroids
immunomodulators
systemic corticosteroids (5th tier)
when do you give to patients?
how long for mod-severe asthma?
acute vs. maintenance?
given to all pts with acute asthma exacerbations to reduce inflammation
mod-severe asthma: short-term as add on for 7 days in adults and children 3 days = no tapering due to no adrenal gland suppression
NOT FOR MAINTENANCE OR LONG-TERM
immunomodulators (5th tier)
name the two drugs and what they do
name important SE in one drug
what is something both drugs do?
Omalizumab (Xolair): Anti IgE antibody (mediates type I hypersensitivity reactions, if you block the IgE, you reduce the bronchospasm); adjunctive therapy for patients >= 12 years with allergies and severe persistent asthma. Administered subcutaneously, significant side effects such as anaphylaxis
Expensive
Inactivates IgE
Benralizumab (Fasenra): Anti eosinophil antibody for patients with asthma and big eosinophil counts
Inactivates eosinophils
BOTH = anti-inflammatory → prevents bronchospasm
cromoglycate agent (historical interest)
what does it do?
when it is used?
treatment choice for asthma?
fast or slow acting?
Prevent mast cell degranulation -> anti-inflammatory, but have no bronchodilator effect.
Used for prophylaxis before exercise. Not a treatment choice for asthma
Type I hypersensitivity drug
Quick acting
general order for asthma meds
first general thing every one gets
asthma vs. COPD tx
rescue inhaler (Everybody)
ASTHMA: next is ICS or ICS/LABA
COPD: next is LAMA → LABA → LABA/ICS
start adding stuff: LABA, LAMA, etc
intermittent asthma preferred tx
formoterol/ICS or albuterol/ICS* (*pick this one unless insurance doesn’t cover)
mild persistent asthma preferred tx
formoterol/ICS on a scheduled basis and PRN for rescue. If you use albuterol for rescue, add an ICS or a long-acting LABA. basically add a steroid in there for mild
moderate persistent asthma preferred tx
play around with dose of LABA/ICS, add a third drug (either leukotriene inhibitor or a LAMA). If pt has been using SABA PRN/ICS alone, change ICS to LABA/ICS (aka prescribe combined things so the patient doesn’t have a ton of inhalers)
severe persistent asthma preferred tx
add leukotriene inhibitor or LAMA to the regimen (Whichever of the two were not added previously)
Continue to add or substitute other agents until the right combo is found
if still using SABA, add LAMA or leukotriene inhibitor next. Then add the other if needed. Continue to add or substitute other agents until right combination is found
managing acute asthma exacerbations (10)
Assess severity of attack (HR, RR, O2 sat, peak flow)
Check adherence, environmental control, comorbidities
Give inhaled SABA early and frequency
Consider concomitant use of ipratropium (Atrovent) for severe exacerbations
Start systemic glucocorticoids if no immediate response to the inhaled SABA
You want systemic steroids on board (Even though they take a while to work)
In more severe cases, subcutaneous epinephrine or terbutaline (Breathine)
Terbutaline: pure beta 2 agonist, given subcutaneously
Frequently (q1-2h) objective assessment of the response ot therapy until definite, sustained improvement is documented
Admit patients who do not respond well after 4-6 h to a setting of high surveillance and care
Educate patients about the principles of self-management for early recognition and treatment of a recurrent attack and develop an “asthma action plane” for recurrent symptoms
Step up maintenance meds, if needed. May try stepping back down once symptoms are well controlled for 3 months (to see if it’s a seasonal issue)
severe asthma attack findings (8)
Marked breathlessness
Tripoding
“Sniffing Position”: “jutting” out head (smelling roses)
You are making the airway as straight as possible from the mouth -> trachea (less turbulent airflow/more laminar flow)
In nose, you have more turbulent flow to help warm air and remove the viruses and bacteria
Inability to speak more than short phrases
Use of accessory muscles, retractions
Drowsiness
Not ventilation = carbon dioxide rises, in high levels CO2 will suppress your neurological function (CO2 narcosis)
Drowsy because you’re hypoxic and you have CO2 narcosis
Inability to lie supine
Peak flow <50% predicted/personal best
Pulse oximetry <90%
Risk factors for Fatal Asthma
Use of LABAs for too long and without ICS
Never take away rescue inhaler or the steroid** you can remove LABAs though, or replace with a leukotriene for 6 months to increase number and sensitivity of B receptor again “Drug Holidays” for LABAs
Use of >2 canisters of short-acting beta agonist/mo
Previous SEVERE exacerbation (intubation/ICU admission)
2 =+ hospitalizations for asthma in the past year
3 =+ ED visits for asthma in the past year
Hospitalization or ED visit for asthma in past month
7. Difficulty perceiving asthma symptoms or severity
Low economic status, inner city residence, illicit drug use, major psychosocial problems
Comorbidities (CVD, chronic lung, psych disease)
pO2 = 60 mmHg
O2 stat of 90%
(2N1S)
Criteria for intubating a patient with an asthma exacerbation
Pts with Hypoxemia pO2 < 60 mmHg (90% O2)
Pts with hypercapnia (excess CO2/elevated partial pressure of CO2) or even normal pCO2
pCO2 should be LOW. if you see normal pCO2, that means pCO2 is getting higher → hypercapnia (think pseudonormal)
Pt exhaustion leading to respiratory arrest
hypoxemia
paO2 =< 60 mmHg
hypercarbia
paCO2 >= 50 mmHg
acidosis
pH =< 7.30
pH is a logarithmic curve
Small changes in pH will change the hydrogen ion concentration/acid
benefits of bipap and cpap (8)
Increased FRC (functional residual capacity)
Decreases work of breathing
Dec closing capacity = means airway closure happens at a lower lung volume compared to before you put them on the machine = good
Recruits alveoli
Pops them back open/engage them -> decrease shunt
Shunt = has blood but not air
Improves gas exchange
Reverses hypoventilation
Maintain upper airway patency
Helps open airway if you have big tongue, tonsils, etc., that tends to collapse
Might decrease cardiac output (nonbeneficial result)
b/c we normally breathe by negative pressure, whereas this machine is positive pressure = pushing air in you
It increases mean intra-thoracic pressure over time = venous return decrease -> decrease preload -> decrease cardiac output
types of NIV (non-invasive ventilation)
CPAP
BiPAP
CPAP
what does it normally start with?
is pressure constant?
why do neonates and infants get nasal cannulas?
Constant pressure (Will not go below 5 cm of H2O even at the end of exhalation)
Usually starts at 5 cm H2O
Older kids-oro-nasal mask
Binasal prongs for neonates and infants
Works well in neonates and infants
I need a closed system. If there’s a leak, it’ll drop the pressure, which is why for older-adults it’s the whole mask
Infants are obligate nasal breathers
biPAP
what is the inspiratory and expiratory pressure?
who is this a better option for?
Inspiratory pressure (10-15 cm) (assists in inhalation = positive pressure peaks)
Expiratory pressure (5-10 cm)
Might be helpful for ventilatory problems
Better for older kids
CPAP airway affects
reduces closing capacity, slows down airway pressure, slows down exhalation, ensures minimum pressure in lungs → resistance in the lungs → prevents airway closure and slows emptying
good candidates for NIV (3)
Alert
Cooperative
Readily reversible cause
poor candidates for NIV (5)
Hemodynamic instability
UGI bleed (aspiration of blood a possibility)
Uncooperative
Large secretions or vomiting
Post upper abdominal or thoracic surgery (painful to expand chest)
Likely to fail for NIV (3)
Large acid-base derangements
ARDS
Persistent tachypnea (breathing rapidly -> dec time in exhalation -> airtrapping)
conditions good for NIV (4)
Pneumonia
Asthma
Bronchiolitis
OSA
pitfalls of NIV (5)
Hypotension
Aspiration
Must watch closer
Always be ready to intubate
Patient tolerance
Contraindications for NIV (10)
Cardiac or respiratory arrest
Non-respiratory organ failure
Severe encephalopathy (GCS < 10)
Severe upper GI bleeding
Hemodynamic instability or unstable cardiac arrhythmia
Facial or neurological surgery, trauma, deformity
Upper airway obstruction
Inability to cooperate/protect airway
Inability to clear secretions
High risk for vomiting/aspirations
ICU management of asthma (5)
intubation and mechanical ventilation
Magnesium: good smooth muscle relaxant
Lowers BP in pregnancy and relaxes uterus
Can turn off and on
Good for relaxing broncho smooth muscle/bronchodilator
Caffeine (part of the Methylxanthines class) and theophylline (is a chemical cousin of caffeine) = relieves bronchospasm (bronchodilator)
Ketamine: dissociative agent, unhooks brain from peripheral nervous system. Makes you indifferent to pain impulses. A great bronchodilator! But don’t give them ketamine without giving them a sedative, otherwise hallucinations
Heliox (helium/oxygen mixtures has a low viscosity)
Less resistance to airflow compared to nitrogen/oxygen mixtures
ECMO (extracorporeal membrane oxygenation): bypasses lungs
Intubation
what does it control?
what does it require?
what is the goal?
what should you make sure?
Allows control of fiO2, RR, ventilatory pressures
Usually requires sedation
Goal is to support ventilation until bronchospasm can be reversed
Make sure bottom of tube is above carina, double check with CXR, otherwise only one lung will be ventilated
proactiveness in asthma (3)
Good primary care of asthma -> prevent severe exacerbations
Important to assess and re-assess severity and meds
Attention to environmental, socioeconomic factors, triggers