Chapter 5 - THE CIRCULATORY SYSTEM TRANSPORTS MATERIALS THROUGHOUT THE BODY
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
Blood is the transport link between the cells of all the body systems. It is also very important in maintaining the constant internal environment of the body. Some of the more important functions of blood are:
• transporting oxygen and nutrients to all cells of the body
• transporting carbon dioxide and other waste products away from the cells
• transporting chemical messengers, called hormones, to the cells
• maintaining the pH of body fluids
• distributing heat and maintaining body temperature
• maintaining water content and ion concentration of the body fluids
• protecting against disease-causing micro-organisms
• clotting when vessels are damaged, thus preventing blood loss.
Blood is composed of:
• plasma: the liquid part, making up approximately 55% of the blood volume
• formed elements the non-liquid part, making up 45% of the blood volume and consisting of erythrocytes (red blood cells), leucocytes (white blood cells) and thrombocytes (platelets).
Plasma
Plasma is a mixture of water with dissolved substances such as sugar and salts. The function of plasma is to transport the components of blood, including cells, nutrients, wastes, hormones, proteins and antibodies, throughout the body.
Erythrocytes
Erythrocytes, or red blood cells, are the most abundant cells in the blood and account for approximately 40–45% of its volume. This percentage is known as the haematocrit. The cells are a biconcave shape – flattened in the middle on both sides. Red blood cells do not contain a nucleus, which increases their flexibility and, hence, their ability to move through blood vessels. However, the lack of a nucleus also limits their life span to only 120 days on average. The function of the erythrocytes is to transport oxygen from the lungs to the cells throughout the body.
Leucocytes
Leucocytes, or white blood cells, play an important role in protecting the body from infection. While they make up only 1% of the blood, white blood cells are larger than red blood cells. There are a number of different leucocytes, each with its own structure and function.
• Neutrophils are the most common type of white blood cells. They contain enzymes to digest pathogens.
• Monocytes form other cells, including macrophages that engulf pathogens and aged or damaged cells by phagocytosis. • Lymphocytes are involved in the immune response; cell-mediated immunity uses T-lymphocytes, and antibody-mediated immunity uses B-lymphocytes.
• Basophils are responsible for allergic reactions, producing heparin and histamine to defend the body against parasites and bacteria.
• Eosinophils also lead to inflammatory responses; they respond to larger parasites such as worms
Thrombocytes
Thrombocytes, or platelets, are small fragments of cells. When a blood vessel is injured, the platelets adhere to the lining and form a scaffold for the coagulation of the blood to form a clot.
what is bool made up of
Blood is made up of plasma, erythrocytes, leucocytes and thrombocytes; each component performs an important role in the body.
Haemoglobin
is able to combine with oxygen to form a compound called oxyhaemoglobin. The combination of oxygen and haemoglobin is said to be a loose one, because oxyhaemoglobin can easily break down to release the oxygen:

Red blood cells are well suited to their function of oxygen transport because they:
• contain haemoglobin, which is able to combine with oxygen
• have no nucleus, so there is more room for haemoglobin molecules
• are shaped like biconcave discs – the biconcave centre increases the surface area for oxygen exchange and the thicker edges give a large volume that allows room for the haemoglobin molecules.
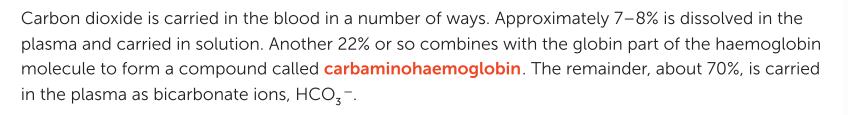
Transport of carbon dioxide
alveoli
The air sacs of the lungs, the alveoli, are surrounded by a dense network of capillaries (see Figure 5.1). Here, the carbon dioxide dissolved in the plasma diffuses out of the blood into the air in the alveolus. The carbaminohaemoglobin breaks down, and the carbon dioxide molecules released also diffuse into the alveolus. Hydrogen ions and bicarbonate ions recombine to form carbonic acid, which then breaks down under enzyme action into water and carbon dioxide. This carbon dioxide also diffuses into the alveolus (see Figure 5.5 and Table 5.1).
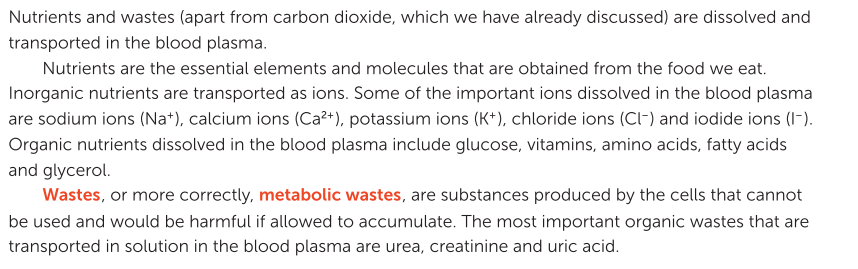
Transport of nutrients and waste
Blood clotting
When an injury occurs that involves damage to blood vessels, the events that follow help to minimise blood loss from the broken vessels and prevent the entry of infecting micro-organisms.
1 Vasoconstriction: The muscles in the walls of the small arteries that have been injured or broken constrict immediately to reduce blood flow and, therefore, blood loss.
2 Platelet plug: The internal walls of blood vessels are normally very smooth, but any damage creates a rough surface to which the platelets stick. Sticking platelets attract others, and so a plug is built up at the site of the injury. This plug also helps to reduce blood loss. The platelets release substances that act as vasoconstrictors, which enhance and prolong the constriction of the damaged vessels. For many of the small tears that occur in capillaries each day, this plugging action of the platelets and constriction of the blood vessels is sufficient to stop any bleeding.
3 Coagulation: For more serious injuries, blood clotting, or coagulation, is necessary. The formation of a blood clot is a complex process involving a large number of chemical substances, or clotting factors, that are present in the blood plasma. The complex series of reactions results in the formation of threads of an insoluble protein called fibrin. The fibrin threads form a mesh that traps blood cells, platelets and plasma. This mesh, with its trapped material, is the clot or thrombus. The threads stick to the damaged blood vessels and hold the clot in position.
The heart
The heart is the pump that pushes the blood around the body. It is located between the two lungs in the mediastinum, behind and slightly to the left of the sternum
pericardium
The heart is a conical shape approximately 12 cm long, 9 cm at its widest point and 6 cm thick, making it about the size of an adult human fist. It is completely enclosed in a membrane called the pericardium.
cardiac muscle
This membrane holds the heart in place, but also allows the heart to move as it beats. It also prevents the heart from overstretching. The wall of the heart itself is made up of a special type of muscle, called cardiac muscle.
septum
The left and right sides of the heart are separated by a wall called the septum. The right side of the heart collects blood from the body and pumps it to the lungs, whereas the left side receives blood from the lungs and pumps it to the rest of the body.
Each side of the heart is also divided into two chambers; therefore, there are four chambers in the heart. The top chambers are called atria (singular: atrium), and the bottom chambers are the ventricles.
• The right atrium receives blood from the body and passes it to the right ventricle.
• The right ventricle pumps blood to the lungs.
• The left atrium receives blood from the lungs and passes it to the left ventricle.
• The left ventricle pumps blood to the body.
The wall of the left ventricle is thicker than the wall of the right ventricle. This is because it needs to be much stronger to pump the blood through the blood vessels supplying the body.
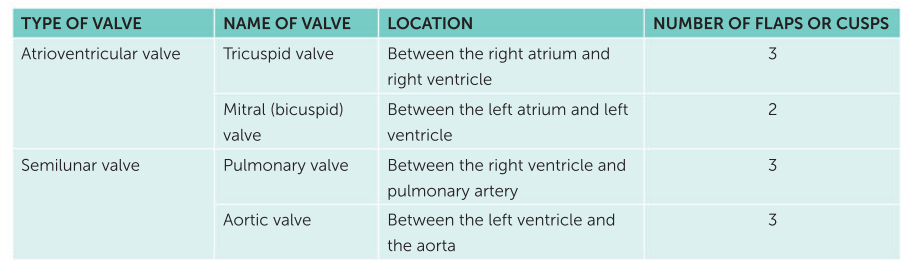
Valves
Valves in the heart ensure that the blood can only flow in one direction.
Between the atria and the ventricles
are the atrioventricular valves. These are flaps of thin tissue with the edges held by tendons, called chordae tendineae, that attach to the heart on papillary muscles.
When the ventricles contract,
When the ventricles contract, the blood catches behind the flaps and they billow out like a parachute, sealing off the opening between the atria and the ventricles. Blood must then leave the heart through the arteries and not flow back into the atria.
semilunar valves.
Where the arteries leave the heart is a second set of valves that stop blood from flowing back into the ventricles when the ventricles relax. These are the semilunar valves. Each semilunar valve has three cusps. When blood flows into the artery, the cusps are pressed flat against the artery wall. When blood tries to flow back into the ventricle, the cusps fill out and seal off the artery, ensuring that the blood only flows in one direction. It is the closing of the valves that gives the heartbeats their characteristic ‘lub dub’ sound. The two sounds are due to the closing of the atrioventricular and then semilunar valves.
Valves
Valves are located between the atria and the ventricles, and at the exit of the ventricles. They act to stop blood from flowing backwards.
Arteries
Arteries are the blood vessels that carry blood away from the heart. The largest artery is the aorta, which takes blood from the left ventricle to the body.
pulmonary artery,
which takes blood from the right ventricle to the lungs
The walls of an artery
The walls of an artery contain smooth muscle and elastic fibres
when ventricles contract
When the ventricles contract and push blood into the arteries, the walls of the arteries stretch to accommodate the extra blood. When the ventricles relax, the elastic artery walls recoil. This elastic recoil keeps the blood moving and maintains the pressure. The muscle in the artery walls does not contract and relax to pump the blood along. However, the muscle can contract to reduce the diameter of the artery and thus reduce blood flow to an organ. Such contraction of a blood vessel is called vasoconstriction
vasodilation
the muscle may relax to increase blood flow to an organ in a process called vasodilation. In this way, blood flow may be controlled to allow for the changing needs of the body.
arterioles
The very large arteries that receive blood pumped by the ventricles divide into smaller arteries. These in turn divide into very small arteries, known as arterioles. It is the arterioles that supply blood to the capillaries. Like the larger arteries, the arterioles have smooth muscle in their walls. Contraction or relaxation of this muscle is very important in regulating blood flow through the capillaries.
vasodilators
illaries. As the body exercises, the muscle cells continually require energy. Cellular respiration in the muscle cells makes the energy available, but also produces large amounts of wastes, including carbon dioxide and lactic acid. These wastes act as vasodilators, substances that produce a local widening, or dilation, of arterioles. This results in increased blood flow through the muscle tissues, ensuring that the cells are adequately supplied with oxygen and nutrients for continued functioning. Cellular respiration also releases heat energy, which tends to increase blood temperature. It also contributes to an increase in heart rate.
Capillaries
Capillaries are the link between the arteries and veins. They are microscopic blood vessels that form a network to carry blood close to nearly every cell in the body. This enables the cells to get their requirements from the blood and to pass their waste into the blood. The structure of the capillaries makes them suitable for this function, as their walls have only one layer of cells. This allows substances to pass easily between the blood and the surrounding cells.
Veins
Veins carry blood towards the heart. The capillaries join into small veins, venules , which then join up to make larger veins. These culminate in the:
• inferior vena cava and superior vena cava , which bring blood from the body to the right atrium. The superior vena cava brings blood from above the heart, while the inferior vena cava brings blood from below the heart.
• pulmonary v, eins which bring blood from the lungs to the left atrium. There are four pulmonary veins – two from each lung.
Veins carry blood towards the heart. The capillaries join into small veins, venules , which then join up to make larger veins. These culminate in the: • inferior vena cava and superior vena cava , which bring blood from the body to the right atrium. The superior vena cava brings blood from above the heart, while the inferior vena cava brings blood from below the heart. • pulmonary v, eins which bring blood from the lungs to the left atrium. There are four pulmonary veins – two from each lung.
The cardiac cycle , or heartbeat, is the sequence of events that occurs in one complete beat of the heart.
The pumping phase of the cycle
The pumping phase of the cycle, when the heart muscle contracts, is called systole
The filling phase,
The filling phase, as the heart muscle relaxes, is called diastole. For a short time both atria and ventricles are in diastole. During this phase, the atria fill with blood and the ventricles also receive blood as the valves between them are open
Atrial systole,
Atrial systole, the contraction of the atria, then follows and forces the remaining blood into the ventricles.
ventricular systole.
The atria then relax and refill while the ventricles contract in ventricular systole. Ventricular systole forces blood into the arteries. Although the left and right sides of the heart are two pumps, they operate together. Both atria contract simultaneously, as do both ventricles.

Cardiac output
How quickly the blood flows around the body depends on how fast the heart is beating and how much blood the heart pumps with each beat.
heart rate
The heart rate is the number of times the heart beats per minute
stroke volume
while the stroke volume is the volume of blood forced from a ventricle of the heart with each contraction
combination of heart rate and stroke volume
A combination of both these factors influences the cardiac output – the amount of blood leaving one of the ventricles every minute. The cardiac output is equal to the stroke volume multiplied by the heart rate:
Description on blood
The surface of red blood cells is coated with sugar and protein molecules that are able to stimulate the immune system. These molecules are called antigens and the protein produced by the immune system is called an antibody. The antigen and its antibody combine to form a complex and cause a reaction.
ABO blood groups
There are two sugar antigens involved in the ABO classification of blood groups: antigen A and antigen B. On the surface of the red blood cells a person may have either antigen A, antigen B, both antigens or neither antigen. These four possibilities correspond to the four groups of the ABO system: group A (antigen A), group B (antigen B), group AB (both antigens) and group O (neither antigen). The body’s ability to make the antigens, and so a person’s ABO blood group, is determined by their DNA and is therefore inherited. The antibody that reacts against antigen A is called anti-A, while anti-B reacts against antigen B. A person’s immune system is able to recognise their own antigens and will not produce antibodies for them. However, they will produce antibodies for antigens that are non-self. Thus, a group A person can produce only the antibody anti-B, a group B person can produce only anti-A, a group AB person cannot produce either antibody, and a group O person can produce both. This is summarised in Table 5.4 on page 122.
Rh blood groups
The Rhesus blood group system is so named because Landsteiner used the blood of rhesus monkeys in his initial investigations. Like the ABO system, it is based on antigens that occur on the surface of the red blood cells. Unlike the ABO antigens, which are sugars, the Rh antigens are proteins. A person with Rh antigens is said to be Rh positive; a person without these antigens is Rh negative. An individual without the Rh antigens is able to produce an anti-Rh antibody that reacts against those antigens. Rh-positive individuals cannot produce an anti-Rh antibody
Red blood cells
Red blood cells contain antigens on their surface. These antigens determine the blood group of the individual, including their ABO and Rh blood groups.
The mixing of blood types
The mixing of blood types that are incompatible can cause the erythrocytes to clump together, or agglutinate. If the receiver’s blood contains, or is able to make, antibodies against the antigens on the donor’s red cells, the foreign cells will clump together and disintegrate. It is therefore essential that the blood group of the receiver and donor be the same. The ABO blood group of the donor is always matched to that of the receiver when transfusions are given
Whole blood
is blood as it is taken from the donor but with a chemical added to prevent clotting. Transfusions of whole blood are used mainly in cases of severe blood loss.
Red cell concentrates
Red cell concentrates are the most widely used component of blood. They are produced by spinning blood at very high speed in a centrifuge. The heavier cells sink to the bottom, leaving the lighter plasma on top. The concentrate may or may not have platelets and white blood cells (leucocytes) removed. Transfusions of red cell concentrates are used for patients suffering from heart disease or severe anaemia.
Plasma
Plasma, the liquid part of the blood, may be given to patients requiring extra clotting factors for control of severe bleeding, or to patients with liver disease.
Platelet concentrates
are given to patients who have abnormal platelets or a reduced number of platelets.
Cryoprecipitate
Cryoprecipitate is obtained by freezing the plasma and thawing it slowly. When the plasma is thawed, the cryoprecipitate remains solid. It contains many of the substances necessary for blood clotting. Cryoprecipitate may be used to treat some forms of haemophilia, but it is most often used for severe bleeding.
Immunoglobulins
Immunoglobulins are a group of proteins that act as antibodies. They are extracted from the blood and used for patients who are deficient in antibodies. Particular immunoglobulins from certain donors are used to treat patients who have no immunity to a particular disease. For example, tetanus immunoglobulin may be used to treat tetanus.
autologous transfusion
An autologous transfusion is when the patient’s own blood is used. The blood is collected from the patient prior to an operation that may require a transfusion. Such transfusions are often used for elective surgery and the blood is collected about four weeks before the operation. Autologous transfusions eliminate the risk of transmission of disease and most possible side effects of the usual transfusions.
THE LYMPHATIC SYSTEM
As blood enters the capillaries, the relatively high pressure forces some of the fluid in the blood through the capillary walls into the tissues.
lymphatic system
The main function of the lymphatic system is to collect some of the fluid that escapes from the blood capillaries and return it to the circulatory system. The lymphatic system is also an important part of the body’s internal defence against diseasecausing organisms.
The lymphatic system consists of:
• a network of lymph capillaries joined to larger lymph vessels (also called lymphatic vessels or lymphatics)
• lymph nodes, which are located along the length of some lymph vessels.
Lymph vessels
Fluid tends to leak out at the arterial end of a blood capillary due to the high pressure in the vessel. Some, but not all, of this fluid returns to the capillary at the venous end. The excess fluid in the tissues is returned to the blood by the lymphatic system.
lymph
Fluid returned to the blood in this way is known as lymph.
where is lymph moved
Lymph is moved through the lymphatic vessels as a result of smooth muscle, skeletal muscle and valves. The smooth muscle layer of the vessels is able to contract to push the lymph along the vessel. The skeletal muscles surrounding the vessels are also able to contract, providing additional force. As there is no central pump, there is no force driving the direction of the flow of lymph. Therefore, the larger lymph vessels have valves that close when the pressure drops, preventing the backflow of lymph.
what is lymph
Lymph is fluid that is collected from between the cells and transported in lymph vessels to the large veins.
Lymph nodes
Lymph nodes, also called lymph glands, occur at intervals along the lymphatic vessels. They are most numerous in the neck, armpits, groin and around the alimentary canal. Nodes are bean-shaped and range in length from 1 mm to 25 mm. Each is surrounded by a capsule of connective tissue that extends into the node, forming a framework. Within the framework are masses of lymphoid tissue, containing cells known as lymphocytes, macrophages and plasma cells. Spaces between the cells of the lymphoid tissue are criss-crossed by a network of fibres. Lymph enters through vessels on the convex side of the node, filters through the spaces and passes out through vessels on the opposite side. The lymph passes through several nodes before entering the circulatory system.