RM - Lecture 6: Control of breathing
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
- central controller: pons, medulla, other regions of brain
- effectors: respiratory muscles: diaphragm, intercostals, accessory muscles
- sensor: chemoreceptors in brain, aorta and carotid, mechanoreceptors in lung
What are the 3 components of central breathing regulation?
V̇A and V̇Q are matched
How is metabolic demand V̇O2 met in homeostasis?
They shouldn't change if the person's physiology is healthy.
In a moderately exercising healthy person. What happens to PaO2 and PaCO2 compared to at rest?
In the “respiratory centre" of the brain: in the medulla oblongata and pons
Where does precise breathing control take place?
No, within limits, somatic control can override it
Is the respiratory centre control absolute?
By controlling respiratory muscles
How does the respiratory centre chiefly achieve its purpose?
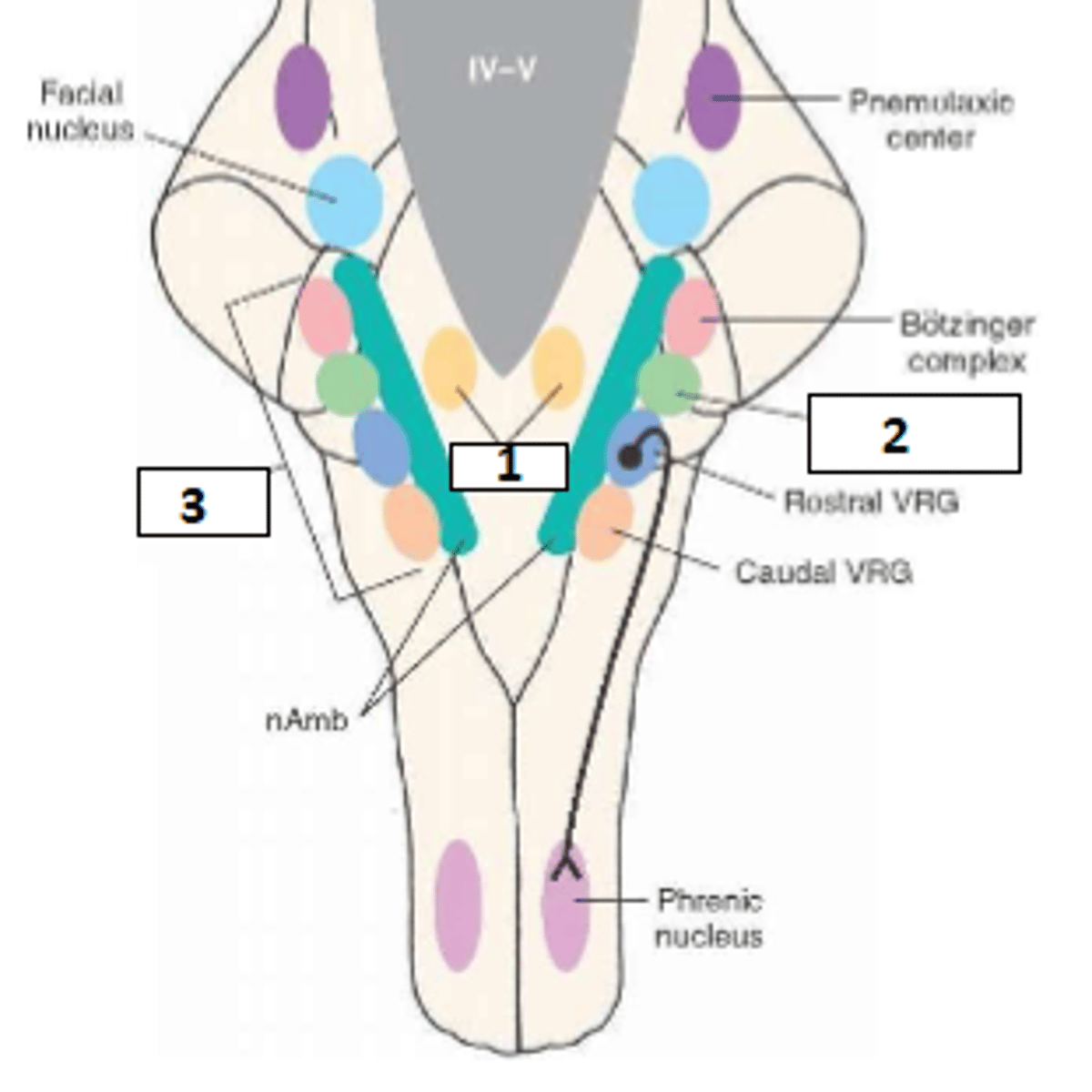
- Dorsal respiratory group: mainly function in inspiration
- Ventral respiratory group: active inspiration and expiration
Describe the types of respiratory neurons in the medulla
pontine respiratory group: pneumotaxic and apneustic centres
Describe the types of respiratory neurons in the pons
The inspiratory neurons of the dorsal respiratory group receive input from the pulmonary stretch receptors. During inspiration, the lungs are stretched and the PSR are briefly activated and send signals to the DRG. This is believed to contribute to the rhythmic pattern of breathing
How do DRG and PSR interact? (general theory)
nucleus tractus soliatarius (NTS)
The nucleus ________ lies near the DRG
- Impulses from medulla in resp centre
- signal to motor neuron cell bodies in spinal cord
- phrenic and intercostal nerves
- diaphragm and intercostal muscles
In 4 dot point steps, list the journey of impulses from the medulla to the respiratory muscles
This refers to a stimulus which increases for 2s steadily and drops away for 3s. This allows for steady incline and decline of lung volume. There are pauses in between ramp signals to allow passive exhalation
What is the inspiratory ramp signal?
- rate can be altered
- starting/stopping point can be altered
In which 2 ways can ramp signal be altered?
Pre-Bötzinger complex (pre-BötC)
What is the name of the proposed newly discovered rhythm generator of the brain?
1. DRG
2. pre-BötC
3. VRG
fill the blanks
chemoreceptors, higher brain centres: pons, hypothalamus
What afferent signals does the VRG receive?
- caudal VRG (cVRG): mostly expiratory neurons
- rostral VRG (rVRG): mostly inspiratory neurons
- Bötzinger complex: mostly expiratory neurons
What are the functional units of the VRG?
- barely active during normal breathing
- extra respiratory drive during increased demand
- coordinates information from chemoreceptors and higher brain regions
How does the VRG function?
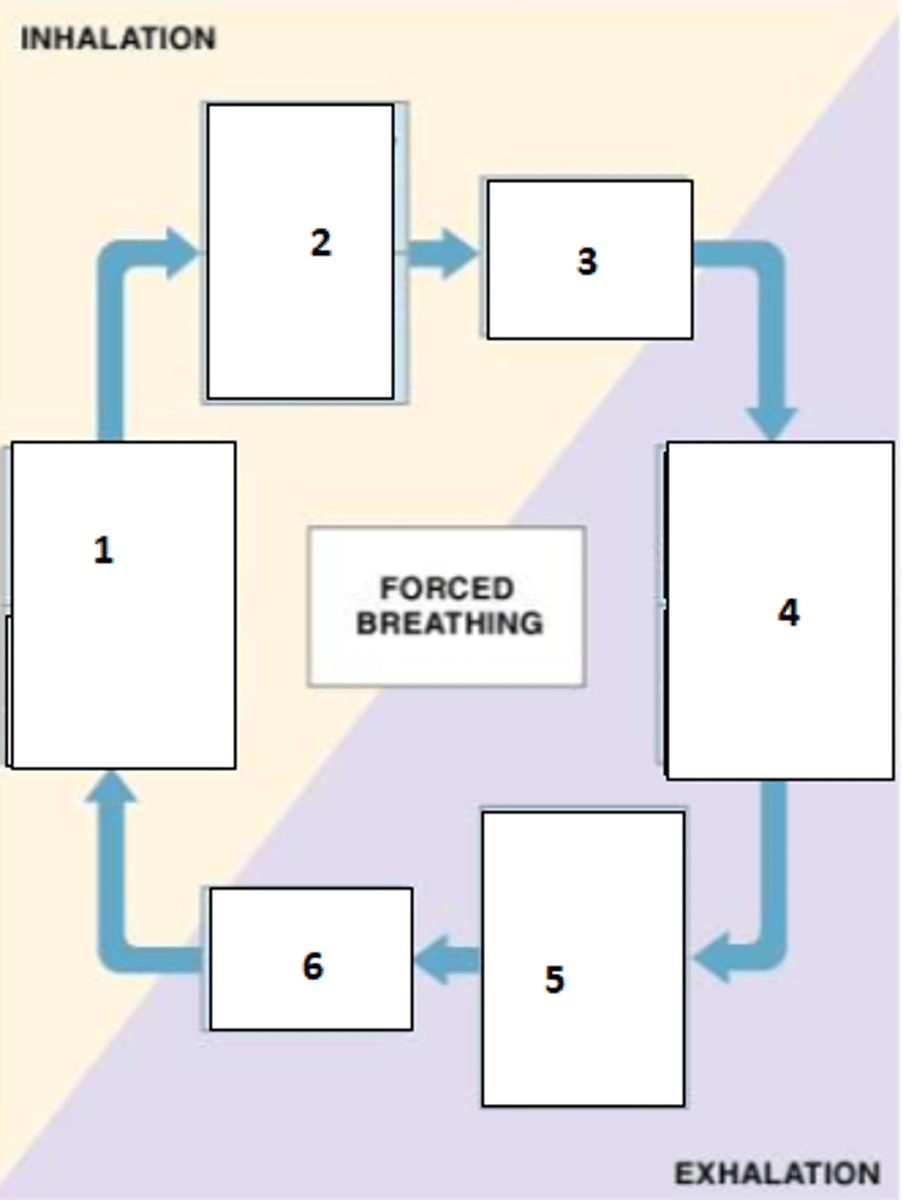
1. Inspiratory centre of DRG and VRG active, expiratory centre of VRG inhibited
2. inspiratory muscles contract and expiratory muscles relax
3. inspiration
4. expiratory centre of VRG active, inspiratory centre of DRG and VRG inhibited
5. expiratory muscles contract and inspiratory muscles relax
6. expiration occurs
Describe what happens at each step during forced breathing
- pneumotaxic centre
- apneustic centre
What are the two groups of the pontine respiratory group?
It controls the off switch of the dorsal respiratory group (DRG).
What is the function of the pneuomtaxic centre?
VT decreases, f increases
If the inspiratory ramp is switched off earlier, what happens to VT and f?
It can prolong the inspiratory ramp
What is the function of the apneustic centre?
increased VT decreased f
What happens to VT and f when the apneustic centre is active?
coordinates inputs from:
- cortex
- peripheral sensory information (odour, temperature,etc.)
- visceral and cardiovascular inputs
Aside from the pneumotaxic and apneustic centres, what else does the PRG do?
the cerebral cortex can directly control respiratory muscle, bypassing pons and medulla
How can the respiratory centre be overridden?
speech, coughing, sniffling, singing, speaking
Name some times during which cortical control is important
- Primary alveolar hyponventilation
- mutation or posttraumatic acquired
- rare and severe form of central sleep apnoea
- patients exhibit long periods of apnoea but breathe on command
- mecahnical ventilation and/or diaphragmatic pacing required for survival
What is Ondine's curse?
Via the vagus nerve
How do pulmonary stretch receptors reach the DRG?
- slowly adapting stretch receptors
- found airways, associated with tracheobronchial smooth muscle
- activated by stretch, indicator of lung volume
What are SARs?
- Rapidly adapting stretch receptors
- in superficial mucosal layer
- stimulated by VT or CL (lung compliance) changes
- nociceptive and chemoceptive
What are RARs?
- Inhibits inspiration by turning of inspiratory ramp signal
- activated by increased pulmonary transmural pressure gradient
- thought to prevent excess inflation, but unimportant during normal ventilation
Describe the inflation/Hering-Breuer reflex
Stimulates inspiration in response to deflation (turns on inspiratory ramp signal)
Describe the deflation reflex
Chemoreceptors
Which type of receptors are most significant in matching ventilation to metabolic demand?
Retrotrapezoid nucleus
What is the RTN?
Mostly indirectly via high [H+] in CSF, which acts on the RTN of the medulla. This transmits signals to medullary and pons respiratory centres to adjust breathing.
How does PaCO2 affect the respiratory centre?
Mostly via peripheral chemoreceptors and indirectly via CO2 on medullary resp centre
How does high arterial [H+] affect the respiratory centre?
acts only via peripheral chemoreceptors, in carotid and aortic bodies
How does low PaO2 affect the respiratory centre?
- high CO2 -> high H+ and HCO3-
- BBB impermeable to H+ and HCO3-
- CO2 crosses BBB into CSF
- CO2 combines with H2O in CSF to form carbonic acid - Carbonic acid forms HCO3- and H+
- increased H+ in the CSF
- RTN senses H+ and is stimulated
Describe the chain of events that lead from high PaCO2 to RTN neuron stimualtion and why H+ sensing is indirect
Decreasing [H+] in brain's ECF
What is the 'aim of the brain' when ventilation is matched to metabolic demand?
The mechanisms induced by high PCO2 (hypercapnic drive) adapt and become weaker - desensitisation
What happens when PCO2 is chronically high?
H+ can't cross the blood brain barrier (BBB)
Why must H+ act on peripheral chemoreceptors and never on central regulators of ventilation?
Increase
Will high PCO2 and therefore high [H+] increase or decrease ventilation?
Acid-base regulation when H+ is not related to CO2, such as in ketoacidosis or any other metabolic acidosis
In which setting are peripheral chemoreceptors particularly important, compared to central chemoreceptors?
Central: strong but slow (85% of response)
Peripheral: weak but fast (15% of response)
In terms of response strength and speed, how do peripheral and central chemoreceptors compare?
Glossopharyngeal (IX)
What is the pathway of the carotid chemoreceptors?
Vagus (X)
What is the pathway of the aortic chemoreceptors?
More sensitive to low PO2
How does PO2 sensitivity compare to PCO2 sensitivity in peripheral chemoreceptors?
Medulla is depressed and respiratory drive can shut down, triggering a vicious cycle
What happens in extremely low PO2?
- Erratic breathing pattern
- some diesease states, premature birth, altitude
- Periods of hyperventilation + periods of hypoventilation + periods of apnoea
- cycles every 40-60s
- Hyperventilation: ↑PCO2
→ Hypoventilation: ↓PCO2
- occurs when there are delays of oxygen transport to the brain such as in severe heart failure
- occurs in premature babies where lungs are flushed of old air and oxygen levels oscillate stronlgy due to small lungs
- occurs in altitude because low CO2 and low O2 switch between triggering increased and decreased respiration
- increased negative feedback from brain such as due to trauma
Describe Cheyne-Stokes respiration (causes, patterns, timing, basic mechanism)
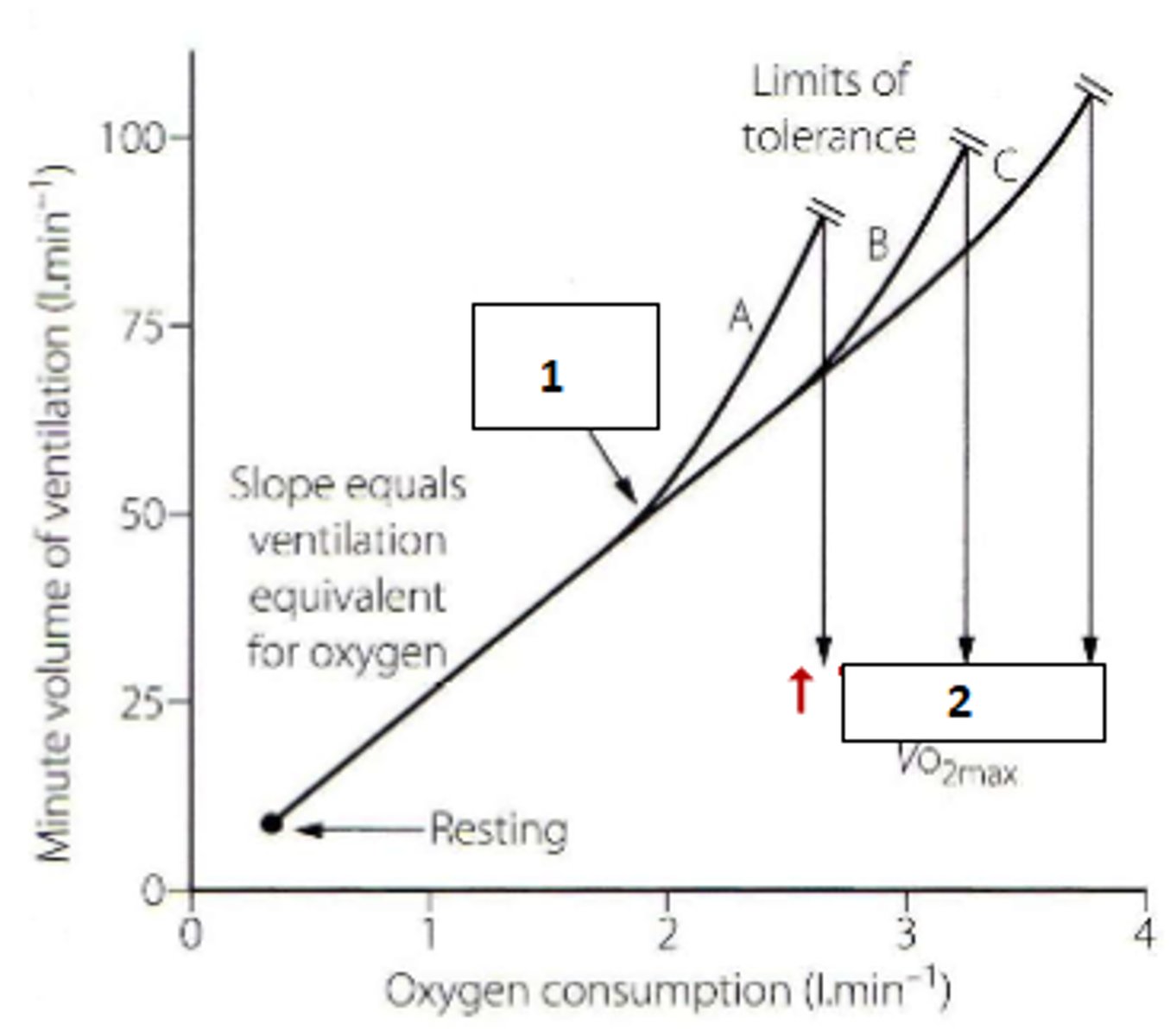
relationship becomes non-linear (Owles point), minute ventilation exceeds metabolic use of O2, due to physiological limitations of perfusion and to deal with increased [H+]
What happens to V̇E-V̇O2 relationship during heavy exercise?
1. Owles point
2. training
Fill the blanks
Still unkown, possibly: joint/muscle receptors, increased oscillation of blood gases
If blood gases are stable, what stimulates hyperpnoea?
10 x 300-500 times a night
How long and frequent is apnoea typically in sleep apnoea?
- obstructive: mechanical - obstruction of upper airways
- central: transient malfunction of respiratory drive
What is the basic difference between obstructive and central sleep apnoea?
TASK2 and GPR4
What are the receptor that detect H+ in the RTN?
Directly to DRG and Pre-BoetzC
Where does the RTN send its signal when detecting high H+?
VRG
Where are signals from peripheral chemoreceptors transmitted to?