congenital heart defects
1/94
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
95 Terms
assessment of cardiac function in children
history
parental concerns
mother’s health and pregnancy
family history
inspection
nutritional status
color
chest deformities
unusual pulsations
respiratory excursion
digital clubbing
assessment of a child with possible cardiovascular disorder
palpation and percussion
chest
abdomen
peripheral pulses
auscultation
heart rhythm (full minute)
blood pressure (both arms, one leg)
character of heart sounds
diagnostic evaluation of heart abnormalities
chest xray
ECG
CBC (for polycythemia)
echocardiogram
arterial blood gas
cardiac catheterization
cardiac catheterization
diagnostic
interventional
electrophysiology results
right side more common in kids because it is safer and structural defects allow access to the left side of the heart
pre-procedural care for cardiac catheterization
nursing assessment (skin, pulses, weight, height)
NPO 4-6 hours, clarify AM meds
IV fluids?
developmentally appropriate psychological prep
sedation?
post-procedural care for cardiac catheterization
observation for complications
color and level of consciousness
vital signs (take HR for one full minute, pay attention to BP) and respiratory status
distal extremities (pulses distal to site can be weaker first few hours)
dressing for bleeding (hold pressure 1 inch above site if bleeding)
fluid intake; both IV and PO
hypoglycemia
strokes
confusion, face or arm weakness, slurred speech, loss of balance
discharge planning for cardiac catheterization
pressure dressing for 24 hours
no tub baths for 3 days, may shower next day
rest and quiet activities for 3 days then can go back to school, but avoid strenuous activity until cardiologist releases
regular diet
ibuprofen or tylenol for pain
teach signs and symptoms of infection
developmental considerations: heart size
ventricles are equal in size at birth
during infancy, muscle fibers of heart are less developed and less organized resulting in limited functional capacity
developmental considerations: O2 saturation
normal is 95-100%
developmental considerations: fat and muscle
infants and small children have thin chest walls with little to no subcutaneous fat and muscle
how does fetal circulation differ from adult circulation
liver and lungs are bypassed via shunts
ductus arteriosus - bypass lungs
foramen ovale - bypass lungs
ductus venosus - bypass liver
oxygenation and filtration of impurities are conducted by mother
fetal circulation ensure that the most vital organs and tissues receive the max concentration of oxygenated blood
fetal shunts
all close at birth or shortly after in response to
decreased maternal hormone prostaglandin E
increased O2 saturations
pressure changes within the heart
general clinical findings for cardiac defects
dyspnea
feeding difficulty and failure to thrive
stridor or choking spells
HR over 200; respiratory rate about 60 in infant
recurrent respiratory tract infections
in the older child - poor physical development, delayed milestones, and decreased exercise tolerance
cyanosis and clubbing of fingers and toes
squatting or knee chest position
blood meets resistance in legs, keeps oxygenated blood circulating in vital organs
heart murmurs
excessive perspiration
signs of heart failure
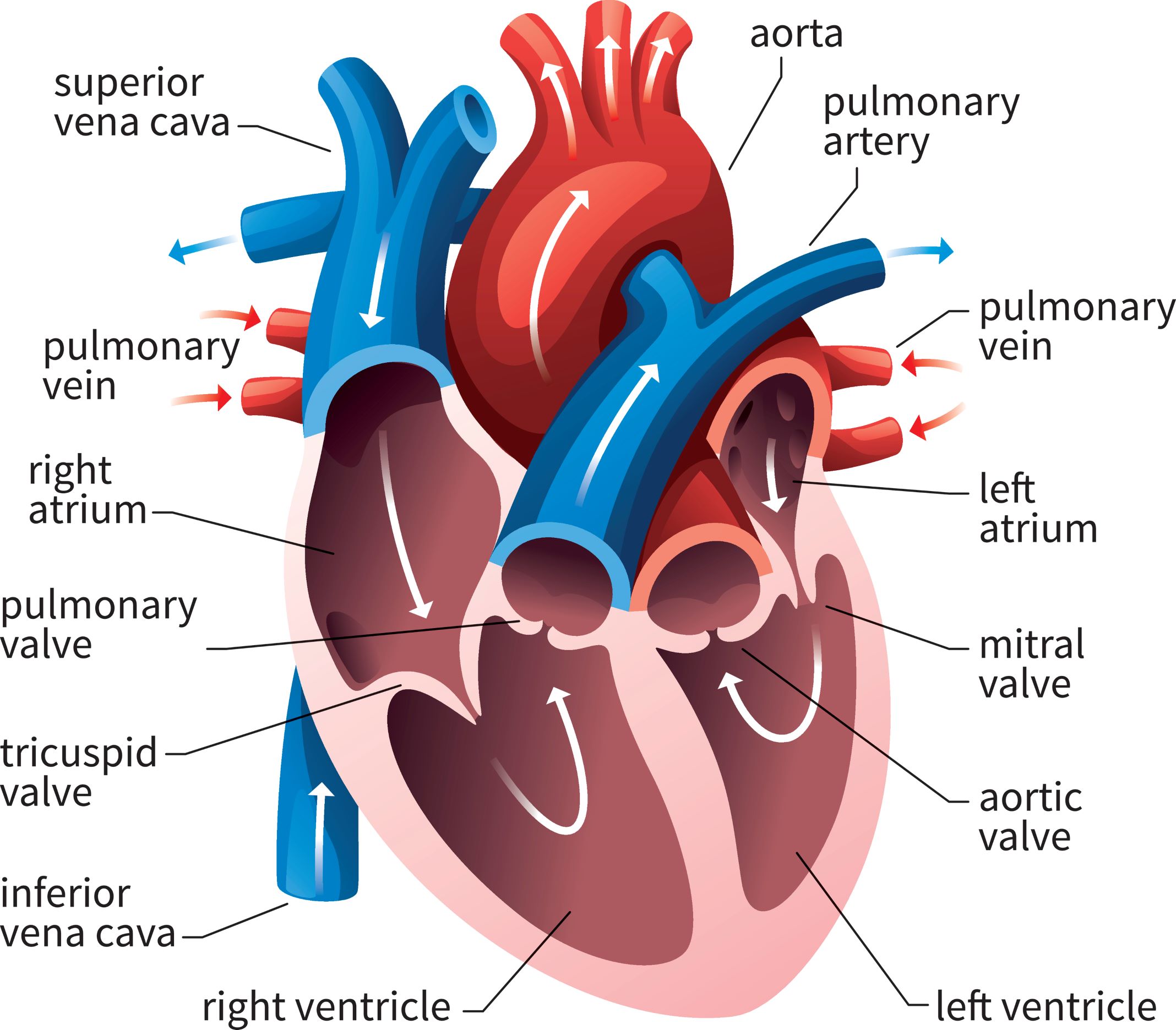
cardiac anatomy
acyanotic heart defects
atrial septal defects
ventricular septal defects
patent ductus arteriosus
coarctation of aorta
aortic stenosis
pulmonic stenosis
atrial septal defects, ventricular septal defects, and patent ductus arteriosis
increased pulmonary blood flow
coarctation of aorta, aortic stenosis, pulmonic stenosis
obstructive lesions
decreased blood flow to areas of body
two principal congenital heart defect clinical consequences can occur
caused by defects that result in left to right shunting of blood
caused by defects that result in decreased pulmonary blood flow
clinical consequences of defects with increased pulmonary blood flow
systemic pressure is greater than the pulmonary pressure so left to right shunting occurs
increased blood volume on right side of heart increases pulmonary blood flow at the expense of systemic blood flow (more going to lungs, less going to body)
s/s of CHF
congestive heart failure (CHF)
chronic condition where the heart muscle can’t pump enough blood to meet the body’s needs, which causes buildup of fluid in lungs and other organs
causes of congestive heart failure
volume overload
pressure overload
decreased contractility
high cardiac ?
children with CHF occur most frequently where structural abnormalities result in increased volume overload or increased pressure load on ventricles
clinical manifestations in CHF: pulmonary venous congestion
tachypnea
wheezing
crackles
retractions
cough
dyspnea on exertion
grunting
nasal flaring
cyanosis
feeding difficulties
irritability
fatigue with play
clinical manifestations in CHF: systemic venous congestion
hepatomegaly
ascites
edema
weight gain
neck vein distension
clinical manifestations in CHF: impaired myocardial function (cardiac output)
tachycardia
weak peripheral pulses
hypotension
gallop rhythm
extended capillary refill
pallor
cool extremities
oliguria
fatigue
restlessness
enlarged heart
sweating
clinical manifestations in CHF: high metabolic rate
failure to thrive or slow weight gain
perspiration
therapeutic management of CHF
improve cardiac function
remove accumulated fluid and sodium (can also be limited on diet)
decrease cardiac demands
improve tissue oxygenation and decrease oxygen consumption
medications used in CHF
furosemide (Lasix)
ACE inhibitors
Digitalis (digoxin)
furosemide
diuretic
give foods high in potassium
ACE inhibitors
ex - captopril, lisinopril, enalapril
reduces afterload, so monitor BP before and after giving
most are potassium sparing
digitalis
only oral med that increases contractility
potassium and digoxin have inverse relationship (potassium low = digoxin more effective; potassium high = digoxin less effective)
rules for administration of digoxin
given at regular intervals
1 hour before and 2 hours after eating
check apical HR for 1 min before giving
infants and young kids - hold is <90-110
older children - hold is <70
do not mix with food or fluid
behind teeth or brush after administering
missed dose rules
< 4 hours - give missed dose
> 4 hours - withhold
if 2 doses are missed, notify practitioner
if child vomits, do not repeat dose
check potassium levels prior to giving digoxin (hold if potassium levels are low)
digoxin toxicity symptoms
nausea
vomiting
bradycardia
anorexia
neurological and visual disturbances
digoxin toxicity
monitor child closely for dysrhythmias (digoxin toxicity can cause hyperkalemia)
digibind (antidote; watch potassium levels)
binds to digoxin or other cardiac glycosides and is excreted by kidneys and removed from body
watch for rapidly dropping potassium levels
nursing considerations for CHF: activity intolerance
promote adequate rest
prevent crying
group activities
short intervals of play, cuddling
provide neutral thermal environments
supplemental oxygen
depends on orders
satting in 80’s can be okay
nursing considerations for CHF: altered nutrition
infants will have higher metabolic rate bc of poor cardiac function and increased HR and RR
anticipate hunger
smaller, more frequent feedings (q 3 hours rather than q 2 or 4)
feed no longer than 30 mins at a time and give remaining via NG
feed in relaxed environment
semi-erect position for feeding
burp before, during, and after feeding
formula with increased calories per ounce
soft preemie nipple with moderately large opening
nursing considerations for CHF: ineffective breathing patterns
assess rr, effort, and O2 saturations
> 60 = hold feeds
position to encourage maximum chest expansion (not as important in infants)
avoid constriction
humidified supplemental oxygen; during stressful periods (crying or invasive procedures)
nursing considerations for CHF: potential for infections
avoid crowded public spaces
good handwashing
screen visitors
nursing considerations for CHF: fluid volume excess
accurate I&O
weigh daily - same time, scale, and clothes
assess for edema
maintain fluid restriction if ordered
provide good skin care
change position frequently
nursing considerations for CHF: growth and development
developmentally appropriate toys
infants do catch up
nursing considerations for CHF: coping
detailed teaching
emotional support
family education and support for CHF
teach s/s of worsening clinical status
information on how to give meds
stress importance of good nutrition
have high caloric requirements and get tired and tachypnic easily
immunizations - stay up to date, if < 2 years need RSV prophylaxis
promotion of growth and development
arterial septal defect
defect stems from patent foramen ovale of failure of a septum to completely develop between the right and left atria
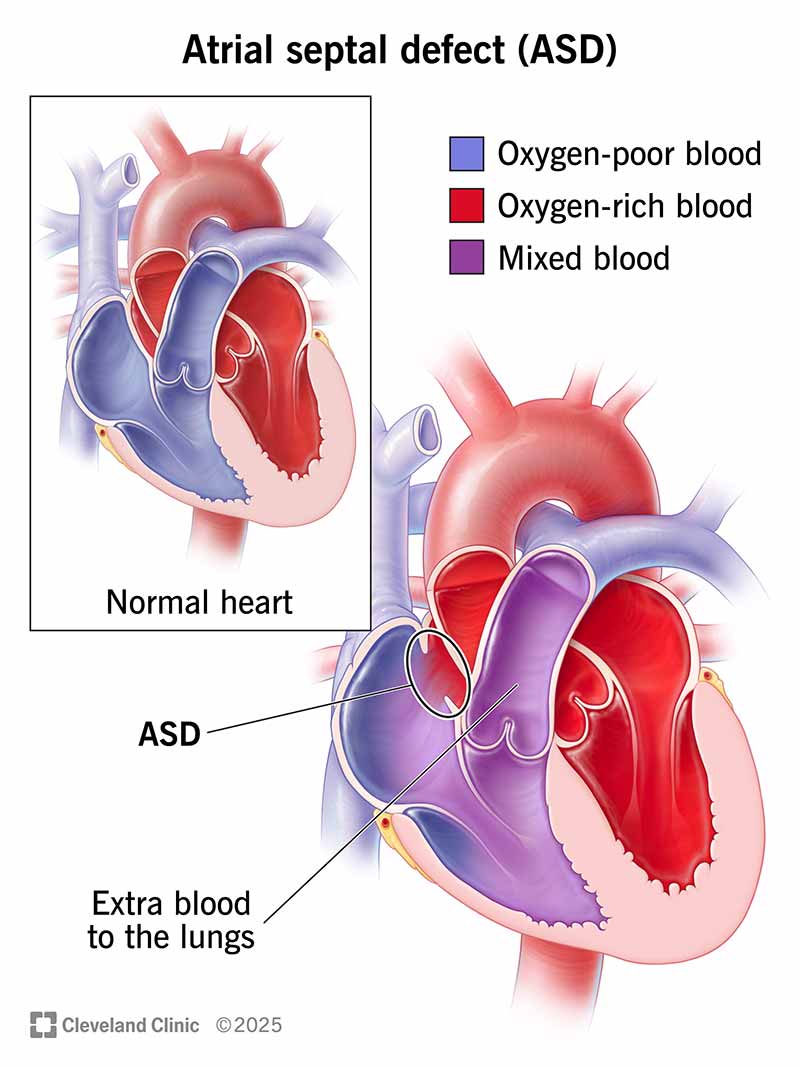
increased pulmonary blood flow
clinical manifestations of arterial septal defect
may be asymptomatic
heart murmur
CHF
increased risk for dysrythmias with pulmonary vascular obstructive disease and emboli later in life
treatment of arterial septal defect
mild defects may close spontaneously
open heart surgery and dacron patch closure
may be closed using devices (septal occluder) during cardiac catheterization
ventricular septal defect
the septum fails to completely form between the right and left ventricles
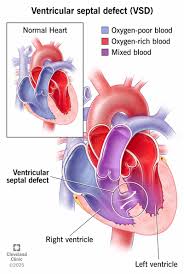
increased pulmonary flow
clinical manifestations of ventricular septal defect
CHF; moderate to severe
cyanosis
characteristic murmur
right ventricular hypertrophy
failure to thrive
fatigue
recurrent respiratory infections
therapeutic management of ventricular septal defect
pulmonary artery banding
may close spontaneously by age 3
interventional heart cath with septal occluder
surgical correction with patch and repair of AV valve tissue
patent ductus arteriosus (PDA)
the fetal structure fails to close - blood is shunted from aorta to pulmonary artery
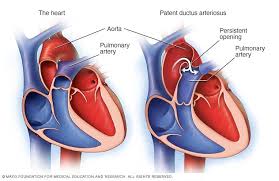
increased pulmonary blood flow
clinical manifestations of patent ductus arteriosus
machine like murmur
can be asymptomatic
CHF
treatments for patent ductus arteriosus
indomethacin (prostaglandin E inhibitor like ibuprofen) will cause defect to close on its own with a couple doses
interventional heart cath with coil
left thoracotomy or video assisted thoroscopic surgery (VATS) to place clip on ductus
clinical consequences of obstructive lesions
blood exiting heart meets area of anatomic narrowing, causing obstruction to blood flow
usually occurs near valve as in aortic and pulmonic stenosis
either shunting (left to right) or backup of blood on right side
increased pulmonary congestions
signs of CHF
coarctation of the aorta
narrowing of aortic arch, usually distal to the ductus arteriosus and beyond the right subclavian artery
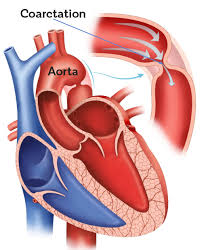
obstructions of blood flow
results in increased pressure proximal to defect (head and upper extremities) and decreased pressure distal to the defect (body and lower extremities)
two locations of coarctation
preductal
postductal
preductal coarctation of aorta
between subclavian artery before ductus arteriosus
postductal coarctation of aorta
collateral circulation develops during fetal life (distal to ductus arteriosus)
clinical consequences of coarctation of aorta
L → R shunting, increased pulmonary blood flow leading to CHF
increased blood flow to head and upper extremities
decreased blood flow to trunk and lower extremities
therapeutic management of coarctation of aorta
surgery within first two years
long term complications can include
recoarctation
aortic aneurysm
systemic hypertension
aortic stenosis
narrowing or fusion of aortic valves which interferes with left ventricle outflow; blood backs up into right side of heart and enlarges
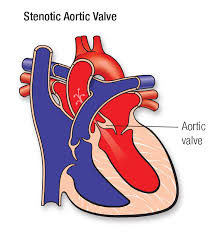
obstructions of blood flow
results in decreased cardiac output, left ventricular hypertrophy (LVH), and pulmonary vascular congestion
aortic stenosis: serious defect
obstruction tends to be progressive
sudden episodes of myocardial ischemia, or lower cardiac output, can result in sudden death
only defect where activity is limited
surgical repair rarely results in normal valve
clinical manifestations of blood flow in infants
faint pulses
hypotension
tachycardia
poor feeding (decreased CO)
clinical manifestations of blood flow in children
exercise intolerance
chest pain
dizziness when standing for long periods of time
treatment of aortic stenosis
balloon dilation
surgery; aortic valvotomy or replacement
mortality high in NB, low for older kids
aortic stenosis and physical activity
activity level is restricted in children even though chances of sudden death is very true
children are not on bedrest but activity level is restricted
curtail strenuous physical activities
pulmonic stenosis
defect involves narrowing or constriction of valves if the pulmonary artery interfering with right outflow
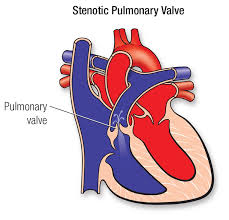
obstruction to blood flow
pulmonary atresia
extreme for of pulmonic stenosis; total fusion resulting in no blood flow to lungs
clinical manifestations of pulmonic stenosis
may be asymptomatic
some have mild cyanosis or CHF
murmur
treatment of pulmonic stenosis
balloon angioplasty
surgery
summary of acyanotic defects
shunting from left to right
increased pulmonary congestion
monitor for CHF
tachypnea
diaphoresis
eating problems
edema
rales, crackles
cyanotic heart defects
tetralogy of fallot
tricuspid atresia
transposition of great vessels
hypoplastic left heart
truncus arteriosis
tetralogy of fallot, tricuspid atresia
decreased pulmonary blood flow
transposition of great vessels, hypoplastic left heart, truncus arteriosus
mixed blood flow
cyanotic defects
caused by defects that result in decreased pulmonary blood flow
pressure is greater on pulmonic side so blood shunts L → R
mixed oxygenated and deoxygenated blood flows to systemic circulation resulting in hypoxia
symptoms of cyanotic heart defects
cyanosis
polycythemia
digital clubbing
altered ABGs
general interventions for cyanotic heart defects
provide good skin care
supplemental oxygen
monitor for and prevent dehydration
developmentally appropriate preparation for tests and procedures
nursing considerations for cyanotic defects
alteration in oxygentation
anxiety caused by cyanosis
dehydration
prevention and accurate assessment of respiratory infections
tetralogy of fallot
combination of four defects (pulmonic stenosis, right ventricular hypertrophy, ventricular septal defect, overriding aorta
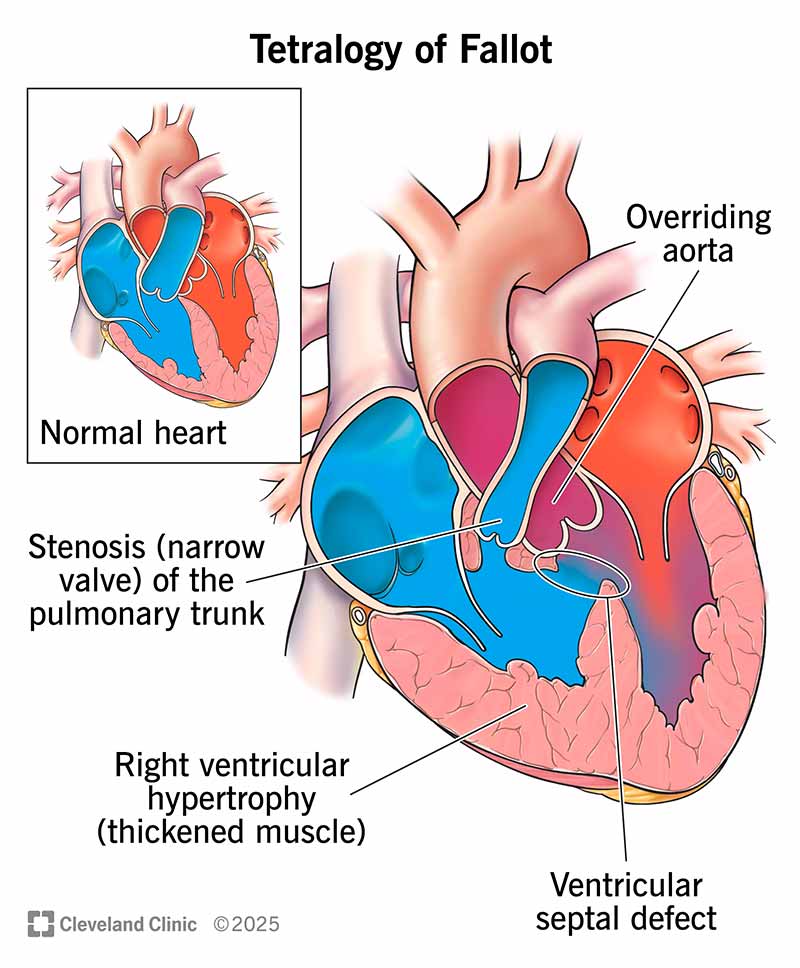
decreased pulmonary blood flow
clinical manifestations of tetralogy of fallot
heart murmur with a thrill
polycythemia
hypoxic episodes (squatting position)
metabolic zcidosis
poor growth
clubbing
exercise intolerance
therapeutic management of tetralogy of fallot
improved quality of life and longevity with surgery done in stages
blalock-taussig shunt
VSD repair
pulmonary valvotomy
guidelines for hypercyanotic spells
employ calm, comforting approach
knee chest position
100% oxygen by face mask
give morphine
IV fluid replacement and volume expansion if needed
repeat morphine if needed
tricuspid atresia
failure of tricuspid valve to develop resulting in no communication between right atrium and ventricle resulting in severe right hypoplasia or absence of right ventricle
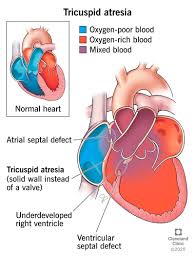
decreased pulmonary blood flow
clinical manifestations of tricuspid atresia
cyanosis
treatment of tricuspid atresia
prostaglandin E to maintain ductus arteriosus
digoxin and diuretics
palliative surgical repair to increase pulmonary blood flow
transposition of the great arteries
pulmonary artery arises from left ventricle and the aorta arises from the right ventricle; no communication between systemic and pulmonary circulations
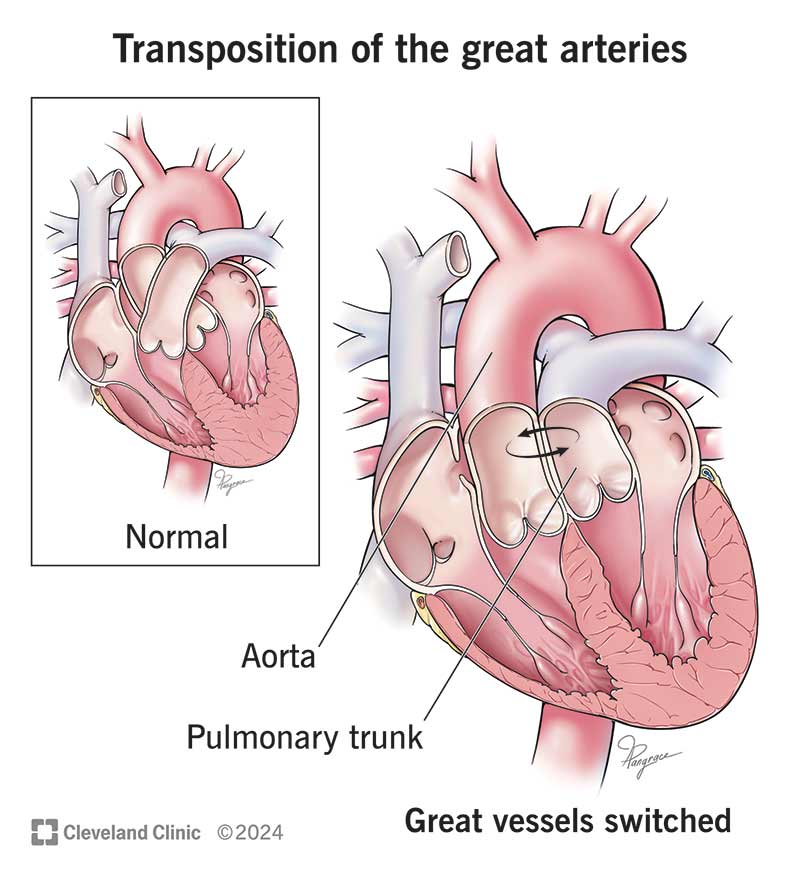
mixed blood flow
must have associated defect that permits blood mixing to be compatible with life
s/s of transposition of great vessels
increasing cyanosis as foramen ovale and ductus arteriosus closes
treatment of transposition of great vessels
arterial switch procedure in the first few weeks of life
IV prostaglandin E to keep ductus arteriosus open and/or balloon atrial septostomy to increase mixing of blood by opening the atrial septum
truncus arteriosus
pulmonary artery and aorta fail to divide during embryonic development; one single large vessel empties both ventricles
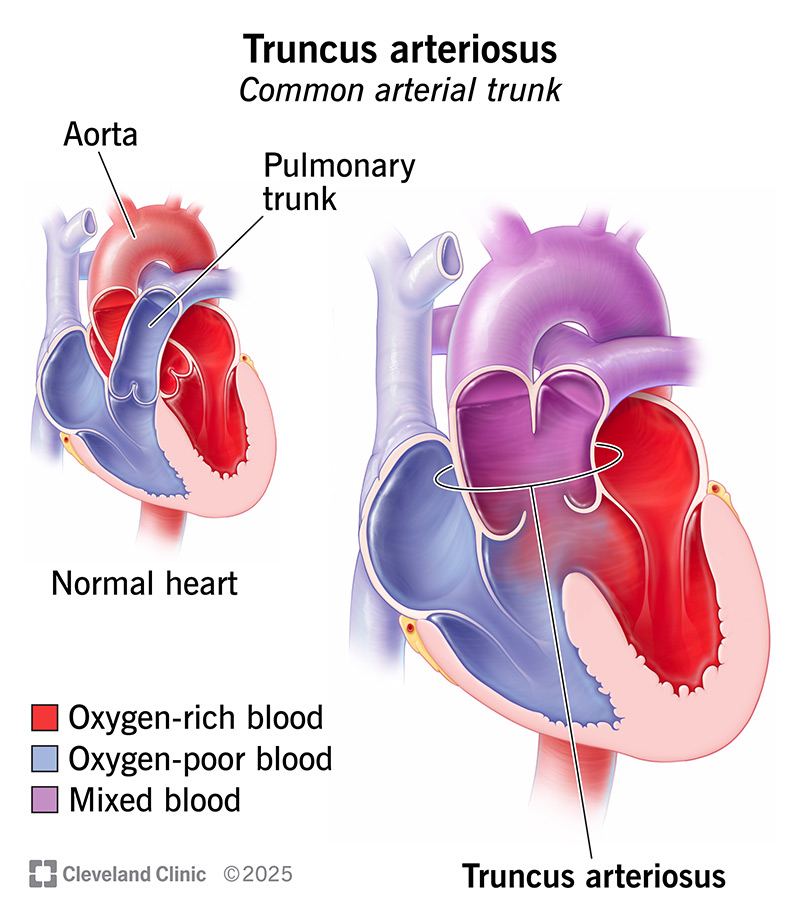
mixed blood flow
clinical manifestations of truncus arteriosus
cyanosis
CHF
heart murmur
treatment of truncus arteriosus
surgical repair during first few months of life
digoxin and diuretics
hypoplastic left heart syndrome (HLHS)
aortic valve atresia, mitral atresia or stenosis, small or absent left ventricle, sever hypoplasia of ascending aorta and aortic arch; underdevelopment of the left side of the heart
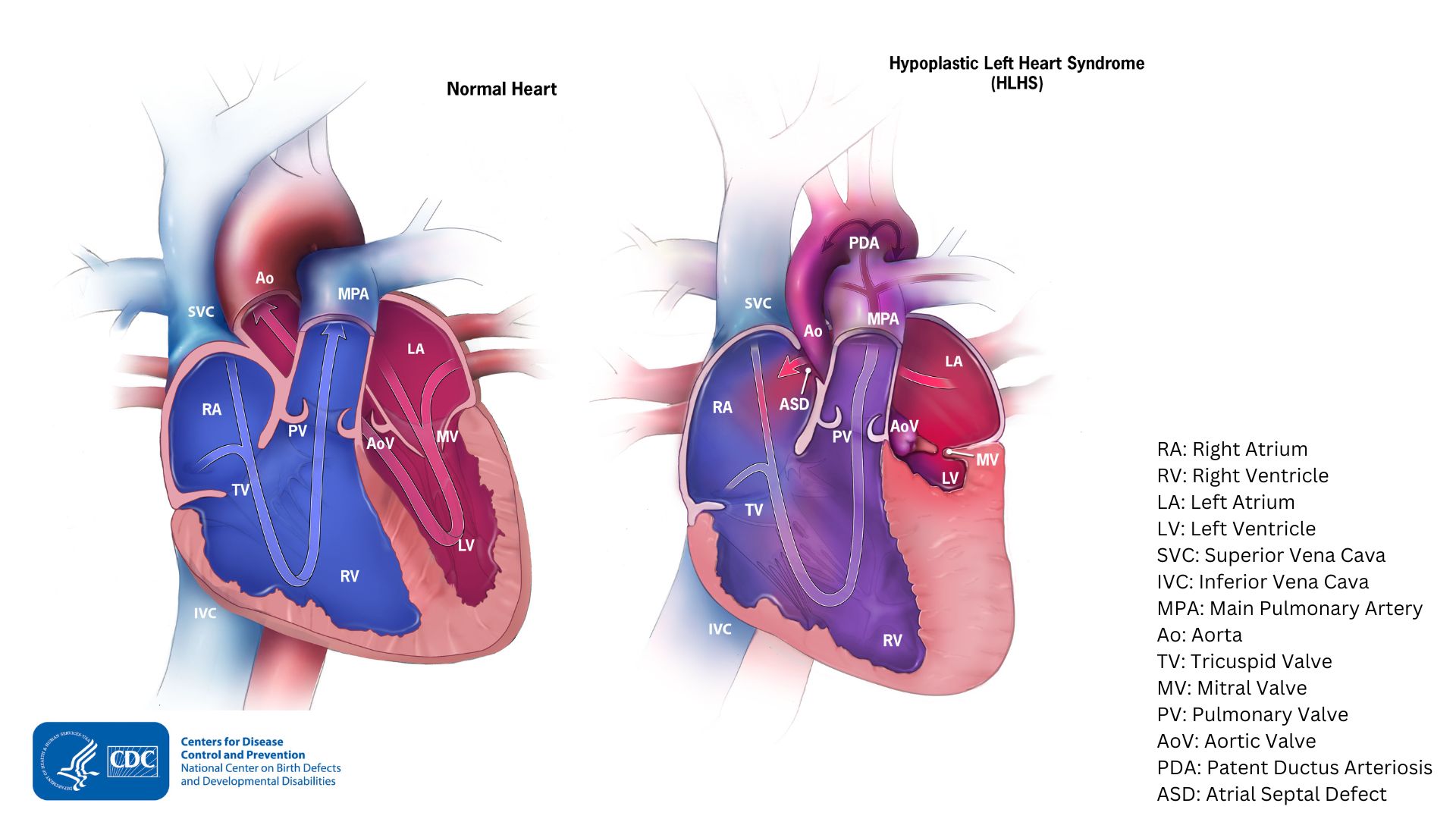
mixed blood flow
descending aorta receives blood via PDA
s/s of hypoplastic left heart syndrome
cyanosis
weak peripheral pulses
cool extremities
respiratory distress
often no murmur
therapeutic management of HLHS
prostaglandin E to keep PDA
fontan procedure - direct blood flow to pulmonary artery from RA
norwood procedure - anastomosis of main PA to aorta, shunt from RV to PA
transplant
complications of heart surgery
CHF
dysrhythmiascardiac tamponade (outside of heart fills with fluid)
cerebral edema
brain damage
hemorrhage or anemia
s/s of cardiac tamponade
atelectasis
pneumothorax
pulmonary edema
pleural effusions
discharge planning after heart surgery
wound care
medication teaching
bacterial endocarditis prophylaxis
when to call practitioner
self limit activity
meet developmental needs