CHEMICAL EXAMINATION - MLS 112 - AUBF - PRELIM LECTURE
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
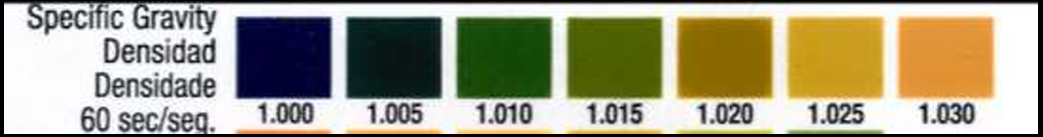
Specific Gravity: Indicator and pH
• Indicator: Bromthymol blue (blue green-green-yellow green)
• pH 6.5 - may interfere with the reaction and bromothymol blue is active in this range
*Specific gravity result over 1.035
• excretion of dextran
• excretion of radiographic contrast media
• excretion of infused high molecular weight intravenous fluid
What is pH?
A Reflection of the ability of the kidneys to maintain normal H+ conc. in plasma & extracellular fluid
Lungs & kidneys–the major regulators of the acid-base content in the body
secrete H+ in the form of NH4+ ions, Hydrogen phosphate & weak organic acids
reabsorb bicarbonate from the filtrate in the convoluted tubules
What is the normal urinary pH range on reagent strips and the typical pH of a first-morning urine specimen?
4.6 – 8.0 for random samples (adult under normal diet excretes urine around pH 6.0)
5.0 – 6.0 for first morning specimen.
How does diet influence urinary pH?
High protein/meat diets produce acid urine; fruits and vegetables produce alkaline urine; cranberry juice is an exception that produces acid urine.
What is the principle of the pH reagent strip reaction and what is the key color changes on the pH pad
A double-indicator system using methyl red (active pH 4.4–6.2) and bromthymol blue (active pH 6.0–7.6) to detect H⁺-driven color change.
For the key color change, at pH 5 → orange; pH 6 → yellow; pH 7 → green; pH 8 → blue and deep blue → pH 9
Name two clinical significances of measuring urine pH
Aid in diagnosing systemic acid-base disorders (metabolic/respiratory acidosis or alkalosis)
Guide management of urinary conditions (e.g., prevent precipitation of crystals/calculi).
What are the main sources of error or interference in pH strip testing?
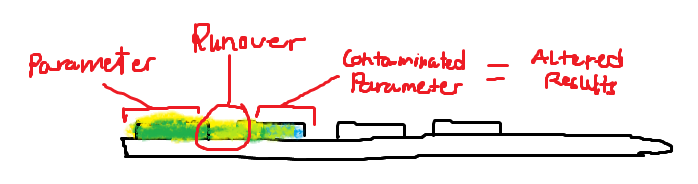
No chemical interferents, but runover from adjacent acidic protein pad and old specimens can produce falsely acidic readings.
With which other urinalysis tests should pH be correlated?
Nitrite test, leukocyte esterase test, and microscopic examination of sediment.
List common causes of acid urine.
Emphysema
Diabetes mellitus
Starvation
Dehydration
Diarrhea
Presence of acid-producing bacteria (Escherichia coli)
High-protein diet
Cranberry juice
Medications:
methenamine mandelate [Mandelamine]
fosfomycin tromethamin
List common causes of alkaline urine
Hyperventilation
Vomiting
Renal tubular acidosis
Presence of urease-producing bacteria
Vegetarian diet
Old specimens
Principle of the protein pad on reagent strips
“Protein error of indicators” – dyes at pH 3 change from yellow to green/blue when protein binds, without a pH change. Trace values are considered to be less than 30mg/dL
Indicator dyes used and key indicators
Tetrabromophenol blue and 3',3″,5',5″-tetrachlorophenol-3,4,5,6-tetrabromosulfonphthalein.
➔at pH 3 →both will appear Yellow----------→(-) protein Green to Blue----------→↑ CHON conc
What is protein, albumin, and normal protein levels
Protein - most indicative of renal disease. Consists primarily of low-MW serum proteins
Albumin – smallest protein (69,000 daltons). Major serum protein found in normal urine
Normal urine protein levels are: Random sample: 0 to 8 mg/dL 24-hour urine collection: Less than 150 mg
Dipstick Protein Reading
Reading | Protein Excretion (g/24g/24 hours) | Protein Excretion (mg/dLmg/dL) |
|---|---|---|
Negative | <0.1 | <10 |
Trace | 0.1 − 0.2 | 15 |
1+ | 0.2 − 0.5 | 30 |
2+ | 0.5 - 1.5 | 100 |
3+ | 2.0 − 5.0 | 300 |
4+ | >5.0 | >1000 |
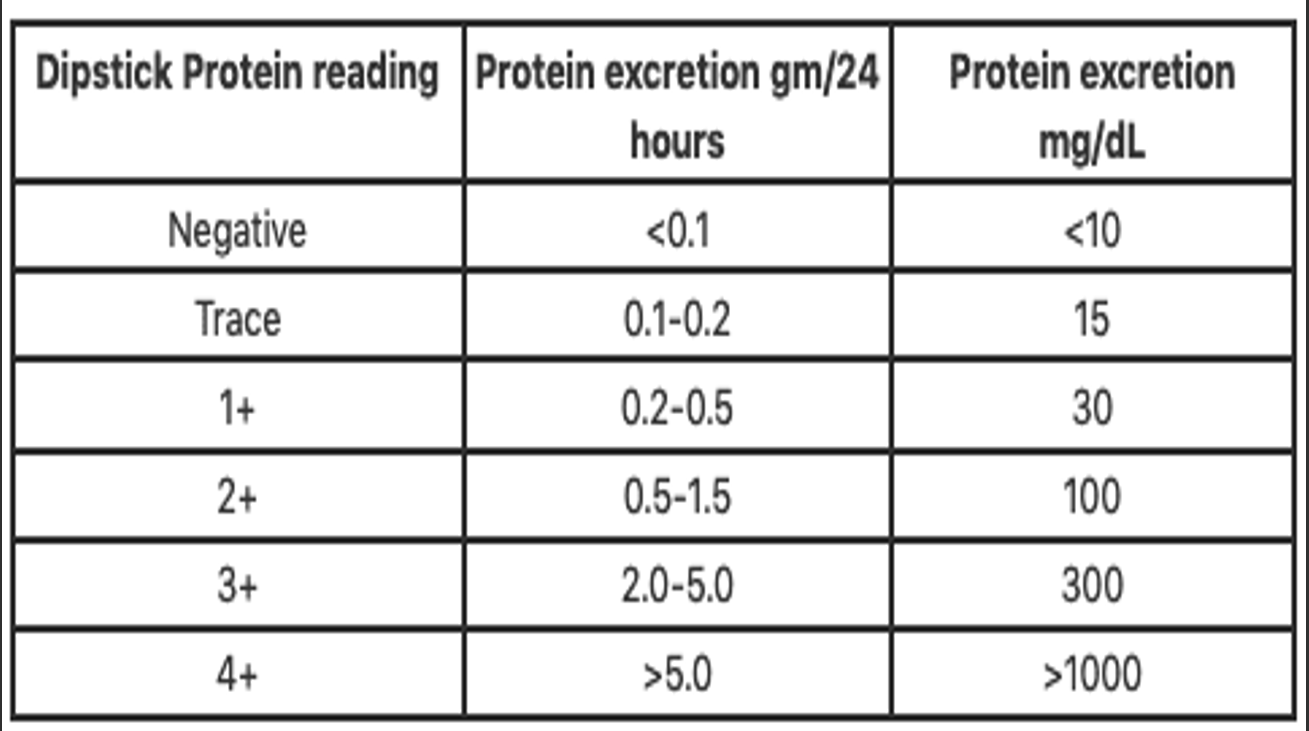
Ref range of clinical proteinuria
≥30 mg/dL (300 mg/L)
Note: When proteinuria is confirmed, 24 hr. collection is done (repeatedly) – distinguish intermittent vs persistent
* even though present in high concentrations in the plasma, the normal urinary albumin content is low because most of the albumin presented to the glomerulus is NOT FILTERED, & much of the filtered albumin is reabsorbed by the tubules
3 types of Proteinuria and examples.
Minimal proteinuria (<1.0 g/day)
Chronic pyelonephritis
Nephrosclerosis
Chronic interstitial nephritis
Congenital disease
Benign postural proteinurias
Transient proteinuria
Moderate proteinuria (1-3 or 4 g/day)
Glomerular disease
Toxic nephrosclerosis (radiation nephritis)
Heavy proteinuria (>3-4g/day)
Nephrotic syndrome
Acute, rapidly progressive & chronic glomerulonephritis
Malignant hypertension
Toxemia of pregnancy
Heavy metals
Amyloidosis
Sickle cell disease & Renal transplant rejection
2 Patterns of Proteinuria
1. Glomerular
cause by glomerular disease (Nephroticsyndrome) -3-4 g/day urine protein or 10 20 g/day
2. Tubular
Tubular renal disease (Fanconisyndrome , wilson’sdse, pyelonephritis, renal transplant rejection) –1-2 -3-4 g/day urine protein
maybe missed by reagent strip
The causes of proteinuria are varied and can be grouped into 3 major categories:
• Prerenal
• Renal (intrarenal)
• Postrenal
*they are based on the origin of the protein
Describe pre-renal proteinuria
caused by conditions affecting the plasma prior to it reaching the kidney (not indicative of actual renal disease)
frequently transient, caused by increased levels of low molecular weight plasma proteins such as haemoglobin, myoglobin, & the acute phase reactants associated w/ infection & inflammation.
increased filtration of low mol. wt. proteins exceeds the normal reabsorptive capacity of the renal tubules, resulting in an overflow of the proteins into the urine
reagent strips detect primarily albumin; prerenal proteinuria is usually not discovered in a routine urinalysis
What is Bence-Jones prerenal protein?
Bence-Jones Protein (BJP)
Bence-Jones Protein (BJP) is a low molecular weight immunoglobulin light chain that is excessively produced in multiple myeloma, a proliferative disorder of plasma cells. Because of its small size, BJP is freely filtered by the kidneys, but when produced in large amounts it exceeds the renal tubular reabsorption capacity, resulting in its excretion in the urine.
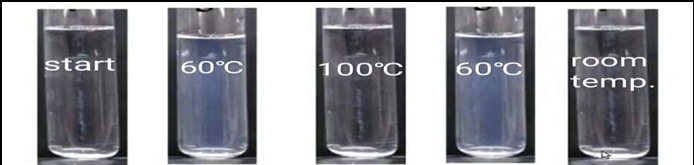
➔ if suspected, a screening test that uses the unique solubility characteristics of the protein can be performed
➔ other proteins -coagulate & remain coagulated when exposed to heat
➔ Bence Jones protein -coagulates at temp. between 40°C & 60°C & dissolves when the temp. reaches 100°C
➔ spx appears turbid between 40 0C & 60 0C & clear at 100 0C
➔ interference due to other precipitated proteins can be removed by filtering the specimen at 100 0C & observing the specimen for turbidity as it cools to between 40 0C & 60 0C
Describe Renal proteinuria
it is a proteinuria associated with true renal disease may be the result of either glomerular or tubular damage
What is Glomerular Proteinuria?
➔ if glomerular membrane is damaged, selective filtration is impaired; increased amounts of serum protein, & RBCs & WBCs& large globulin molecules pass through the membrane & are excreted in the urine.
➔ 4.0 g/day
Major Causes of Proteinuria due to Glomerular Damage:
A. Amyloid material
B. Toxic agents
C. Immune complexes found in:
Lupus erythematosus,
Streptococcal glomerulonephritis
protein, particularly in a random sample, is not always of pathologic significance, can be due to benign causes.
benign proteinuria is usually transient & can be produced by conditions such as strenuous exercise, high fever, dehydration, and exposure to cold
What is tubular proteinuria?
These are disorders affecting tubular reabsorption of filtered protein
ALBUMIN is present
Albumin is accompanied by other low-MW proteins of both serum & tubular origin.
*Markedly elevated protein levels are seldom seen in tubular disorders.
causes of tubular dysfunction include exposure to toxic substances & heavy metals, severe viral infections, & Fanconi syndrome.
markedly elevated protein levels are seldom seen in tubular disorders.
What is Orthostatic / Postural Proteinuria?
It is a Benign proteinuria:
usually, transient
can be produced by:
a. exposure to cold
b. strenuous exercise
c. high fever
d. dehydration
Functional proteinuria – resolves w/in 2-3 days
e. in the acute phase of severe illnesses
*Proteinuria that occurs during the latter months of pregnancy may indicate a PRE-ECLAMPTIC STATE
Orthostatic or postural proteinuria is a benign form of persistent proteinuria commonly seen in young adults. It occurs after prolonged standing due to increased pressure on the renal vein but disappears when the person lies down, making it posture-dependent and non-pathologic.
What is microalbuminuria?
Microalbuminuria is the consistent excretion of small amounts of albumin, often seen in diabetic nephropathy, and serves as an early predictor of renal complications and cardiovascular risk. It cannot be detected by routine reagent strips and is measured as the Albumin Excretion Rate (AER), with significant values of 20–200 μg/min or 30–300 mg/24 hrs in at least 2 of 3 specimens over 6 months. Detection methods include RIA, EIA/FIA, nephelometry, and dye-binding, with reagent strips using gold-labeled antibody, β-galactosidase, and chlorophenol red galactoside (sensitivity 0–10 mg/dL). False negatives may occur in dilute urine.
Describe the post-renal proteinuria
• Protein can be added to a urine specimen as it passes through the structures of the lower urinary tract (ureters, bladder, urethra, prostate, & vagina).
• Bacterial & fungal infections & inflammations produce exudates containing protein from the interstitial fluid.
• The presence of blood as the result of injury or menstrual contamination contributes protein, as does the presence of prostatic fluid and large amounts of spermatozoa
Where was glucose reabsorbed, its transport and the renal threshold?
Reabsorbed at the PCT by active transport Renal threshold
Renal threshold - (160 – 180 mg/dL)
Recommended spx:
2 hours after meal (postprandial)
*First morning specimen does not always represent a fasting specimen because glucose from an evening meal may remain in the bladder overnight.
Hyperglycaemia-Associated clinical significances
Diabetes mellitus
Pancreatitis
Pancreatic cancer
Acromegaly
Cushing syndrome
Hyperthyroidism
Central nervous system damage
Stress
Gestational diabetes
Renal-Associated clinical significances
Fanconi syndrome
Advanced renal disease
Pregnancy
Osteomalacia
Order of glucose peroxidase test
Glucose Oxidase Test
- reagent strip reaction
- reagent strip impregnated w/:
a. glucose oxidase
b. peroxidase
c. chromogen
d. buffer