Cancer Prevention - Early Detection
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
What are the 2 Goals of Cancer Prevention?
Specific Interventions to prevent cancer in those at risk
Effective Screening for early detection of CA
Aside from an increased risk in cancer, SMOKING is also a modifiable risk factor in?
Cardiovascular Disease
Pulmonary Disease
If patient is a smoker, do a thorough history and ask…
How many years he/she is smoking
How many sticks/packs per day (doesn't matter if 1 stick or 1 pack)
Computed into PACK YEARS
(doesn't matter if 1 stick or 1 pack) → ADDITIVE VALUE
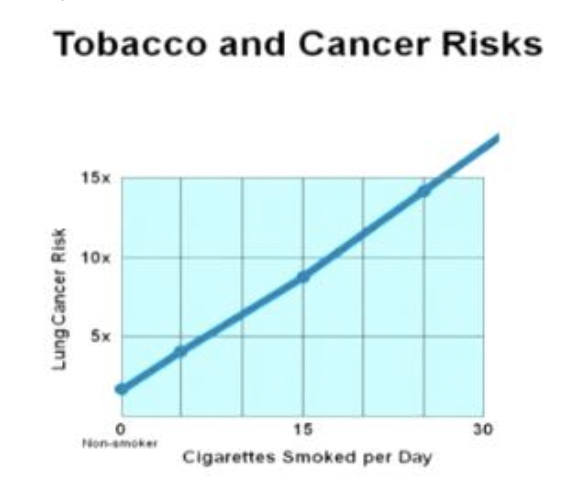
Which is true among the statements?
A. The number of cigarettes smoked per day is directly correlated with increased risk of lung cancer mortality
B. The level of inhalation of cigarette smoke per day is directly correlated with increased risk of lung cancer mortality
C. Both A & B
D. None of the above
C. Both A & B
Secondhand smoke (PASSIVE SMOKE) still increases LUNG CANCER RISK
A smoker who has stopped smoking completely will have a decrease risk of 10 year lung cancer mortality by how many percent?
A. 20-50%
B. 60-100%
C. 30-50%
D. 75-80%
C. 30-50%
Can smokeless tobacco also represent a risk in cancer?
Yes - like chewing tobacco leading to…
→ ORAL CANCER
→ LEUKOPLAKIA
→ GINGIVITIS
→ DENTAL CARIES

Should physical activity be recommended to reduce the risk of cancer?
Yes, especially COLON and BREAST cancer.
→ Physical Activity is recommended but not too much to strain themselves
A diet rich in fat is associate with an increased risk for which cancers?
Breast CA
Colon CA
Prostate CA
Endometrium CA
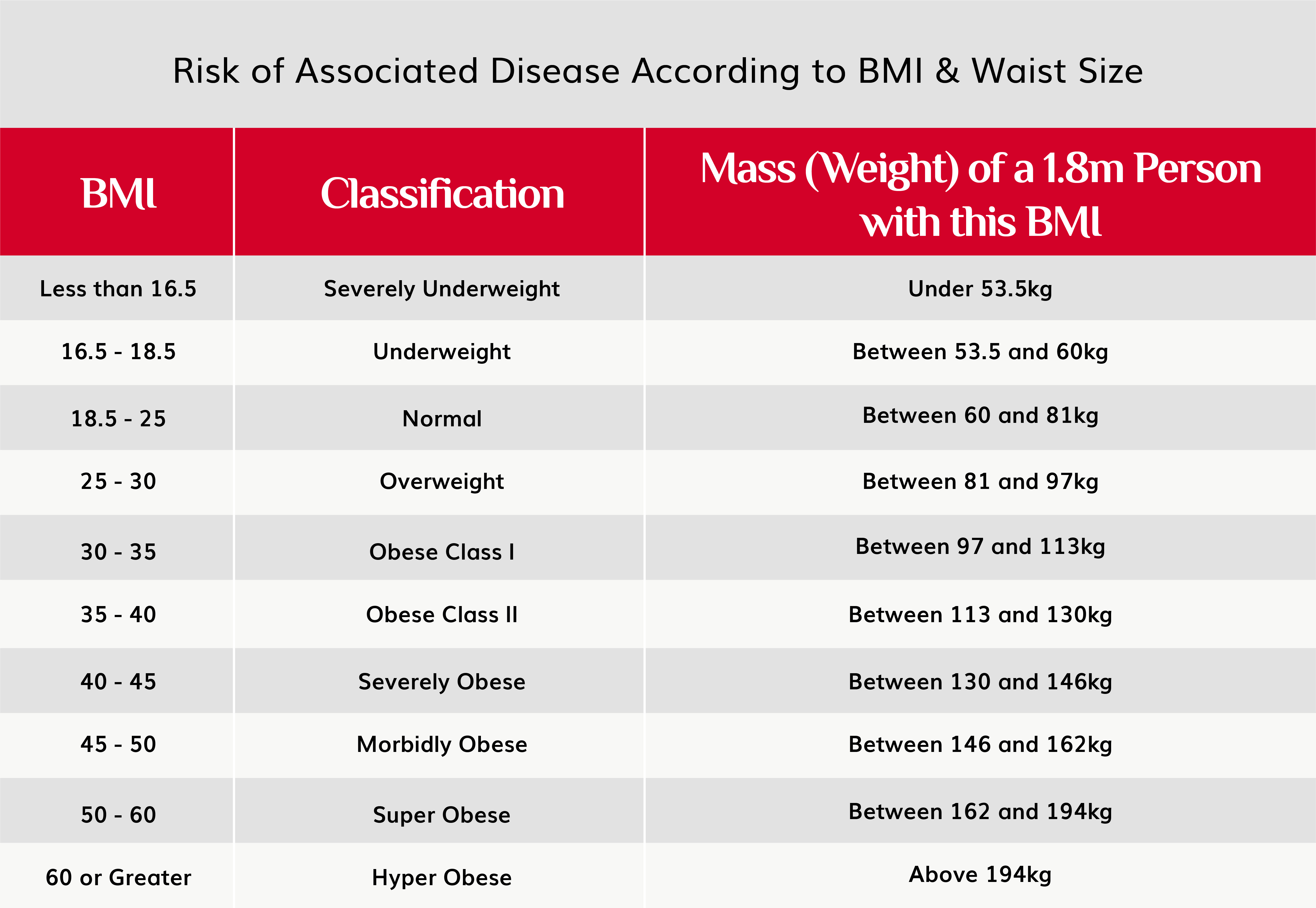
A patient who has a BMI of 27 kg/m2 a/an…
A. Increased Risk for CA
B. No risk for CA
C. Decreased Risk for CA
A. Increased Risk for CA
Overweight and above → INCREASED RISK FOR CA
An intermittent acute sun exposure has an increased risk for Melanoma.
Which times of the day are most dangerous?
10am to 2-3 pm
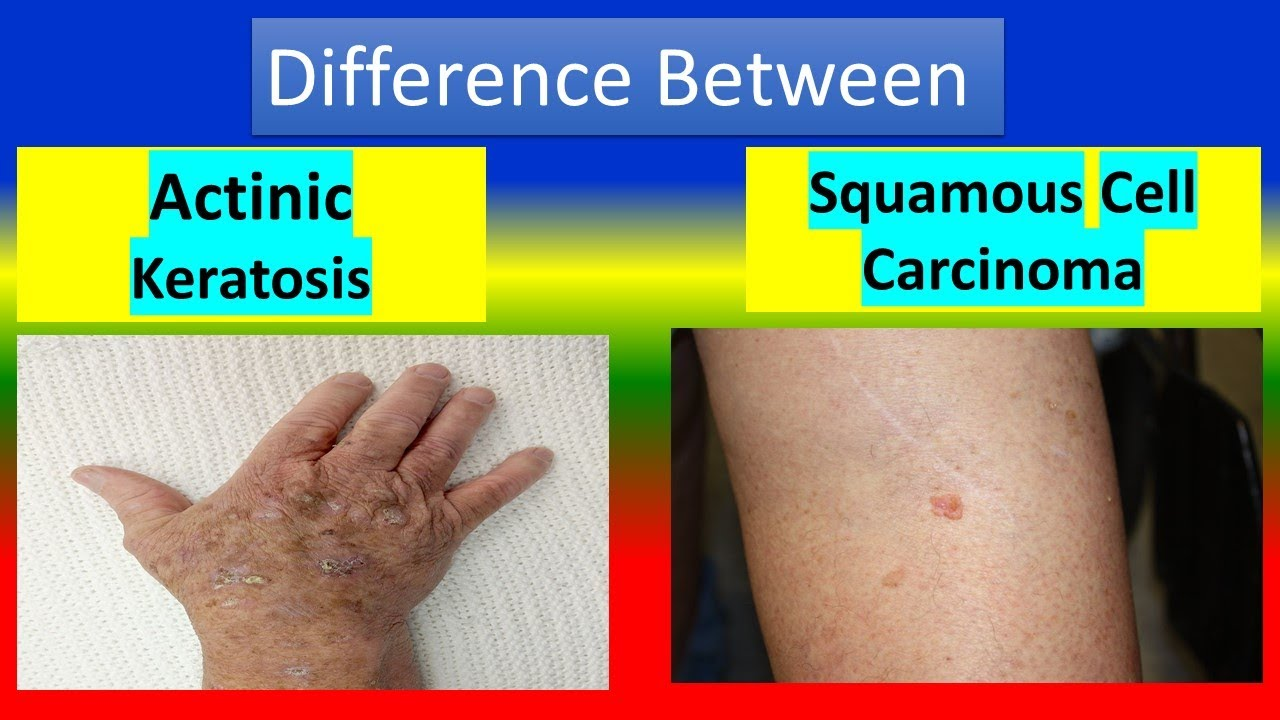
The use of sunscreens decrease the risk of which cancer?
A. Melanoma
B. Squamous Cell Skin Cancer
C. Prostate CA
D. None
B. Squamous Cell Skin Cancer
Decreases risk of actinic keratoses → which is a precursor to SKIN CA. Melanoma may not be reduced with sunscreen
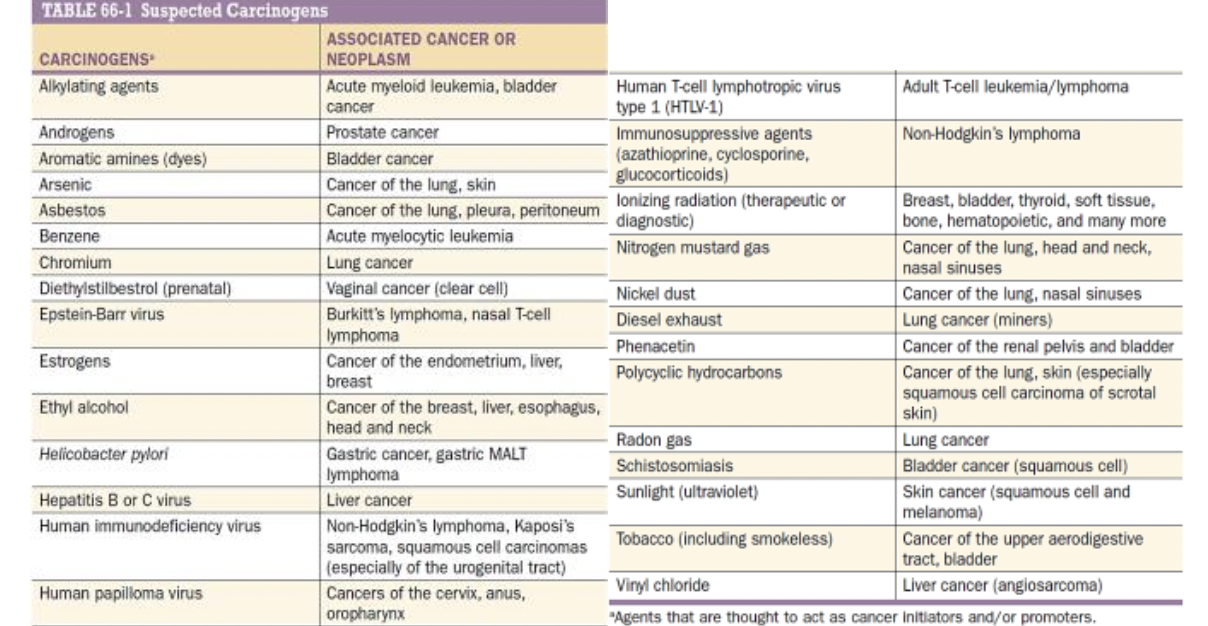
A potential carcinogenic agent in Alkylating Agents can cause what type of cancer?
Acute Myeloid Leukemia
Bladder Cancer
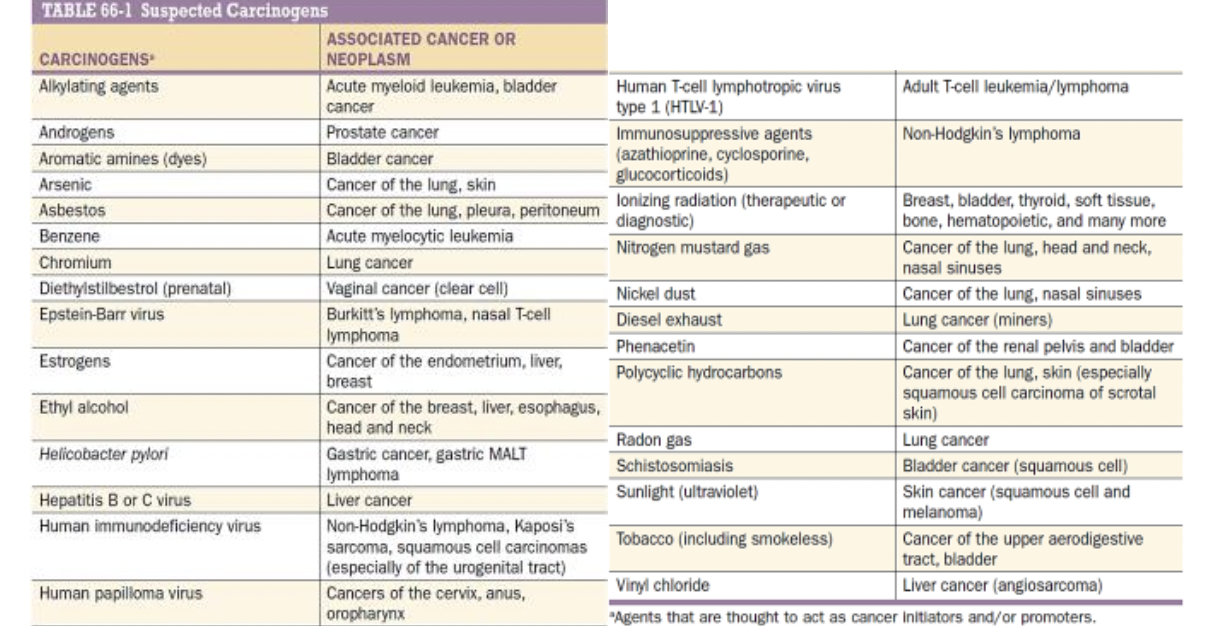
A potential carcinogenic agent in Vinyl Chloride can cause what type of cancer?
Liver Cancer (Angiosarcoma)
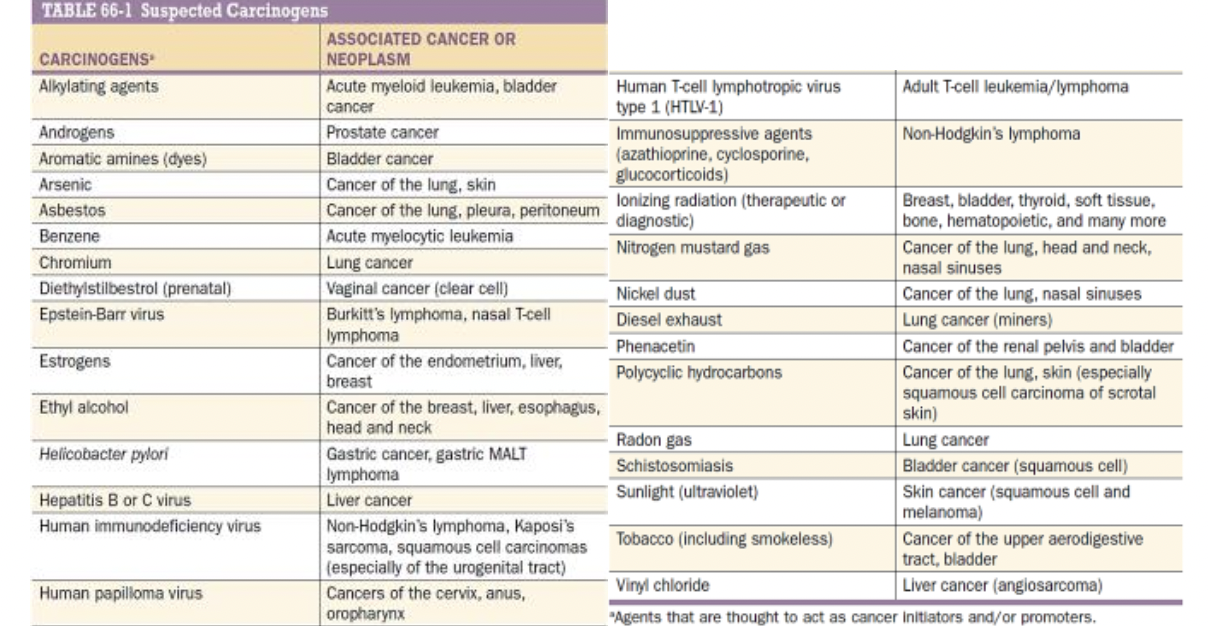
A potential carcinogenic agent in Azathioprine can cause what type of cancer?
Non-Hodgkin’s Lymphoma
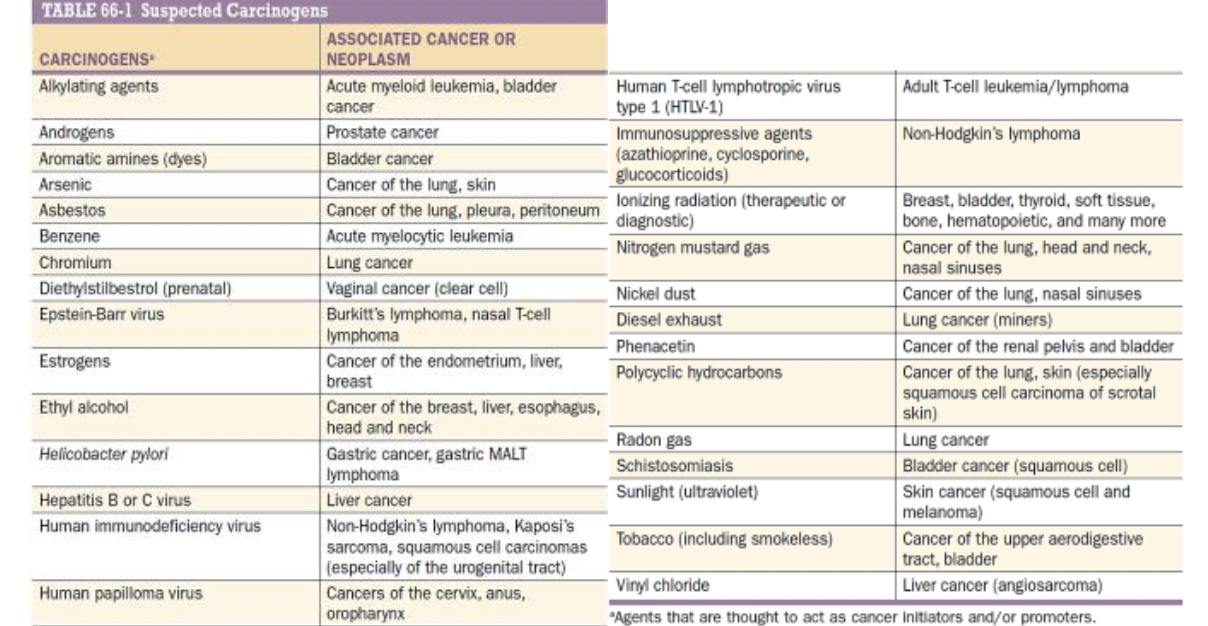
A potential carcinogenic agent in Cyclosporine can cause what type of cancer?
Non-Hodgkin’s Lymphoma
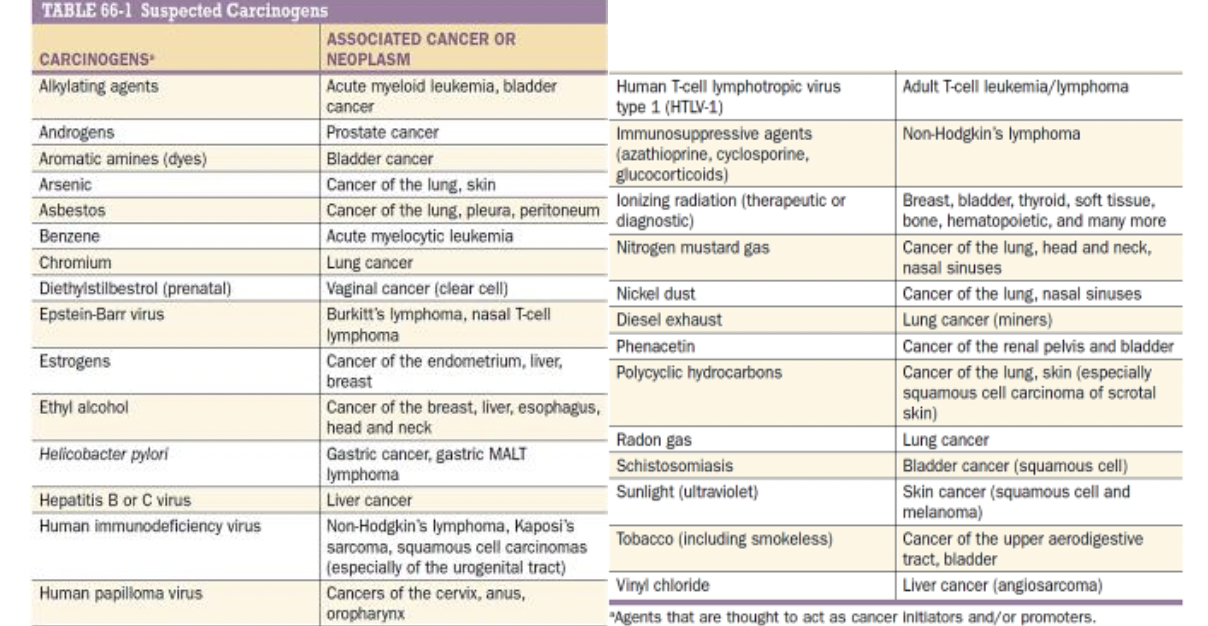
A potential carcinogenic agent in Glucocorticoids can cause what type of cancer?
Non-Hodgkin’s Lymphoma

A potential carcinogenic agent in Phenacetin can cause what type of cancer?
Cancer of the renal pelvis and bladder
Explain the FIELD CARCINOGENESIS HYPOTHESIS.
Patients with past and recovered upper aerodigestive cancer have increased risk of having A SECOND CANCER soon after.
→ Increases 5% every year
Why? Smoking or the carcinogen that has ability to damage epithelial cells have caused widespread damage in epithelial tissue all around the body and not just the site like in LUNG CA or ESOPHAGEAL CA

Oral Leukoplakia is a precursor to what cancer?
Oral Cancer
Significant marker in SMOKERS and associated with INCREASED RISK FOR ORAL CANCER
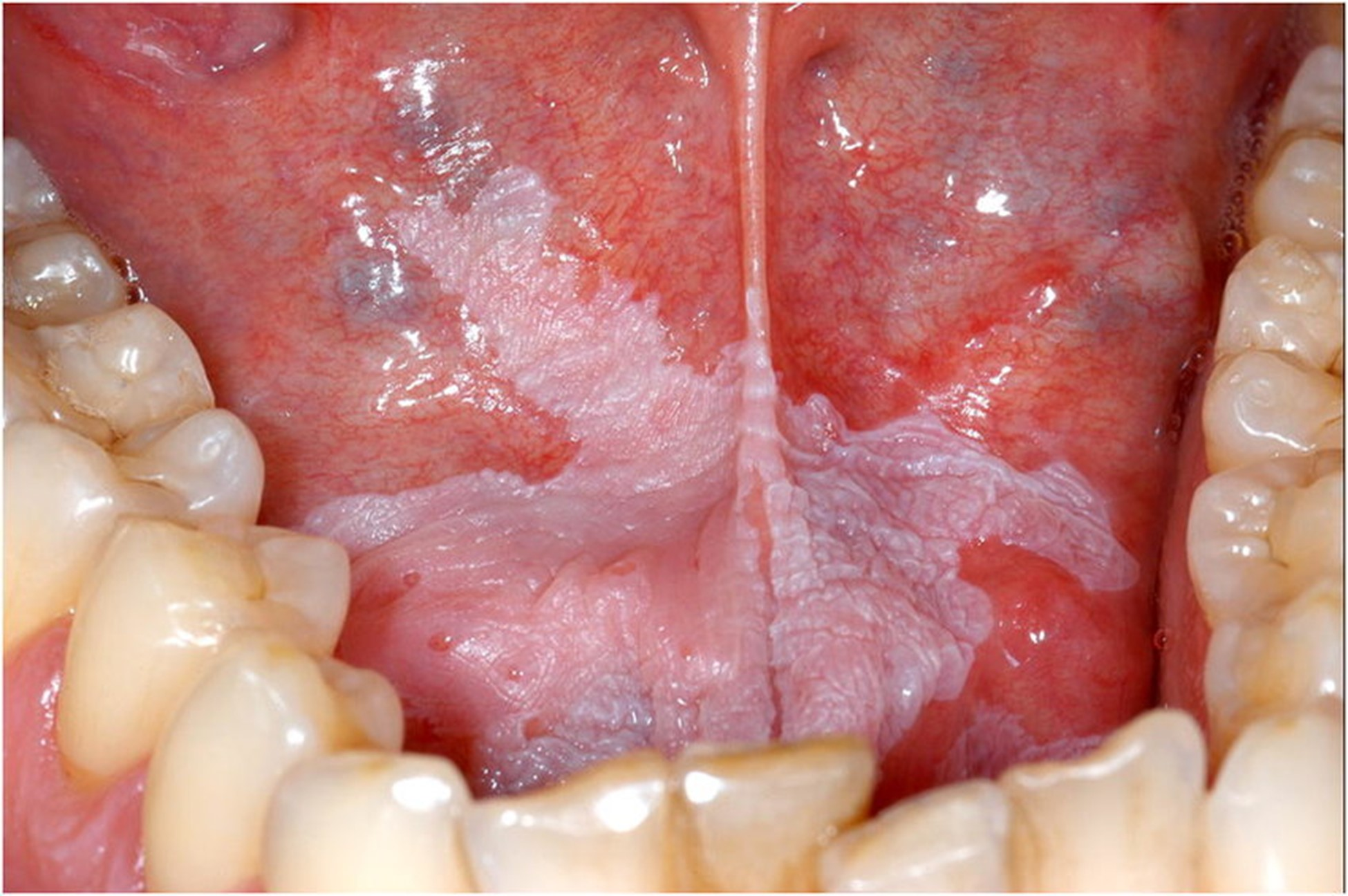
Chemopreventive agent used for Oral Leukoplakia?
Isotretinoin (13-cisretinoic acid)
Although failed to prevent second malignancies in patients cured of Early Stage small-cell lung cancer → INCREASED MORTALITY
Case: A 55-year-old male with a history of heavy smoking was successfully treated for squamous cell carcinoma of the larynx. Despite being "cured," he continues to smoke. What is the most likely explanation for his increased risk of developing a second primary cancer in the upper aerodigestive tract?
A) His immune system remains compromised due to the prior cancer.
B) Smoking creates multiple, widespread areas of epithelial damage in the upper aerodigestive tract.
C) His genetic predisposition to cancer increases after the first tumor.
D) Smoking primarily causes lung damage, leaving other tissues unaffected.
B) Smoking creates multiple, widespread areas of epithelial damage in the upper aerodigestive tract.
FIELD CARCINOGENESIS HYPOTHESIS
Case: Which of the following statements is true regarding the relationship between oral HPV infection and oropharyngeal cancer?
A) HPV infection only increases cancer risk in the presence of smoking and alcohol use.
B) HPV-16 is associated with a lower risk of oropharyngeal cancer than smoking alone.
C) The risk of oropharyngeal cancer increases significantly when both HPV infection and smoking are present.
D) Oral HPV infection does not influence cancer risk in non-smokers.
C) The risk of oropharyngeal cancer increases significantly when both HPV infection and smoking are present.
During the ATBC (alpha-tocopherol, beta-carotene) Lung Cancer Prevention Trial, which drug was known to increase lung cancer incidence and mortality?
Beta Carotene
During the ATBC (alpha-tocopherol, beta-carotene) Lung Cancer Prevention Trial, which drug was known to show NO EFFECT on lung cancer incidence and mortality?
Alpha-Tocopherol
Case: A 65-year-old male smoker who has been smoking one pack per day for 40 years participates in a lung cancer prevention trial where he receives beta-carotene supplements. According to the results of the ATBC trial, what is the most likely outcome for this participant?
A) Reduced risk of lung cancer and overall mortality
B) No change in lung cancer incidence but reduced stroke risk
C) Increased risk of lung cancer and overall mortality
D) No effect on lung cancer but increased risk of hemorrhagic stroke
C) Increased risk of lung cancer and overall mortality
In the ATBC trial, what adverse effect was associated with alpha-tocopherol supplementation?
A) Increased risk of lung cancer
B) Increased incidence of hemorrhagic stroke
C) Decreased risk of cardiovascular disease
D) Reduced lung cancer mortality
B) Increased incidence of hemorrhagic stroke
Most colon cancers arise from what type of benign growths?
Adenomatous Polyps
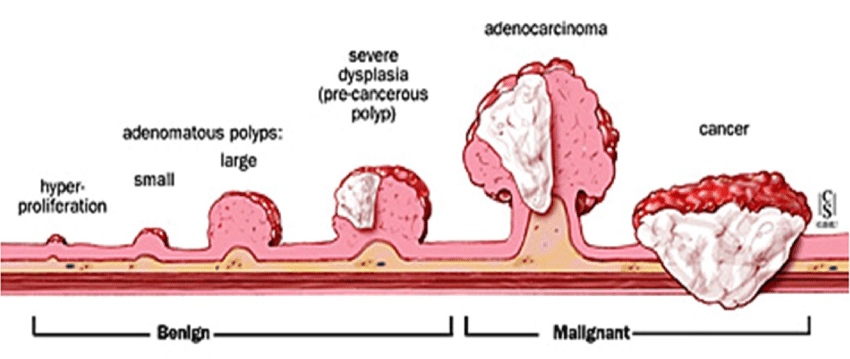
Case: A patient with a history of adenomatous polyps is considering taking NSAIDs for chemoprevention. Based on current evidence, what is the presumed mechanism by which NSAIDs may reduce the risk of adenoma formation?
A) NSAIDs inhibit the growth of polyps by directly binding to DNA.
B) NSAIDs promote apoptosis of cancer cells by enhancing immune function.
C) NSAIDs inhibit the cyclooxygenase (COX) pathway, which is involved in inflammation and may contribute to polyp formation.
D) NSAIDs reduce the absorption of dietary fats, thus lowering cancer risk.
C) NSAIDs inhibit the cyclooxygenase (COX) pathway, which is involved in inflammation and may contribute to polyp formation.
Ex:
Piroxicam
Sulindac
Aspirin
How does calcium potentially reduce the risk of colorectal cancer according to current hypotheses?
A) By directly destroying cancer cells in the colon.
B) By binding to bile and fatty acids, thereby reducing their ability to cause proliferation of colonic epithelium.
C) By increasing the absorption of fiber, which cleanses the colon.
D) By neutralizing stomach acid, which prevents damage to the colon.
B) By binding to bile and fatty acids, thereby reducing their ability to cause proliferation of colonic epithelium.
Tamoxifen is primarily used due to its ability to:
A) Stimulate estrogen production in breast tissue.
B) Bind to estrogen receptors, blocking estrogen's effects on breast cells.
C) Increase breast cell proliferation by upregulating growth factors.
D) Inhibit the synthesis of estrogen in the ovaries.
B) Bind to estrogen receptors, blocking estrogen's effects on breast cells.
Do not give to ER/PR (-) Patients!!!
Which of the following adverse effects is associated with tamoxifen use in breast cancer prevention?
A) Increased risk of lung cancer
B) Increased risk of endometrial cancer, stroke, and thromboembolic events
C) Decreased bone density and increased risk of fractures
D) Increased risk of ovarian cancer
B) Increased risk of endometrial cancer, stroke, and thromboembolic events
DO THOROUGH HISTORY!!!!
The mechanism by which tamoxifen reduces breast cell proliferation involves the upregulation of:
A) Estrogen receptors
B) Progesterone receptors
C) Transforming growth factor (TGF)
D) Epidermal growth factor (EGF)
C) Transforming growth factor (TGF)
Case 1: A 52-year-old postmenopausal woman with a history of smoking is diagnosed with ER-positive, PR-positive, HER2-negative breast cancer. After a successful surgery to remove the tumor, her oncologist recommends tamoxifen as part of her adjuvant therapy.
Question:
Which of the following benefits and risks should be discussed with the patient regarding tamoxifen therapy?
A) Tamoxifen will likely reduce the risk of cancer recurrence in the same breast but does not affect the risk of new cancers in the opposite breast.
B) Tamoxifen is known to reduce the risk of bone fractures and has been shown to decrease the incidence of new breast cancers, including in the opposite breast, but it is associated with an increased risk of endometrial cancer and thromboembolic events.
C) Tamoxifen is effective only in HER2-positive breast cancer and has no benefit in ER/PR-positive cases.
D) Tamoxifen reduces the risk of all cancers but has no impact on bone health or thromboembolic risk.
B) Tamoxifen is known to reduce the risk of bone fractures and has been shown to decrease the incidence of new breast cancers, including in the opposite breast, but it is associated with an increased risk of endometrial cancer and thromboembolic events.
Case 2: A 45-year-old woman with a strong family history of breast cancer undergoes genetic testing and is found to carry a BRCA1 mutation. She has no current evidence of breast cancer. Her oncologist discusses the possibility of using tamoxifen for chemoprevention.
Question:
Considering her ER/PR status is unknown, what should be the primary consideration before starting tamoxifen?
A) Tamoxifen is highly effective in BRCA1 mutation carriers regardless of ER/PR status.
B) The effectiveness of tamoxifen depends on the presence of ER/PR-positive receptors in breast tissue; hence, determining her ER/PR status is crucial before starting therapy.
C) Tamoxifen is recommended only for those who have already developed breast cancer, not for prevention.
D) Tamoxifen is equally effective for both ER/PR-positive and ER/PR-negative breast cancers.
B) The effectiveness of tamoxifen depends on the presence of ER/PR-positive receptors in breast tissue; hence, determining her ER/PR status is crucial before starting therapy.
Case 3: A 60-year-old woman with ER-negative, PR-negative, and HER2-positive breast cancer completed her course of chemotherapy. She is concerned about the risk of developing breast cancer in the other breast and asks whether tamoxifen could help prevent this.
Question:
What is the most appropriate response to the patient's inquiry?
A) Tamoxifen is effective in reducing the risk of recurrence and new breast cancer in ER/PR-negative patients.
B) Tamoxifen is not recommended for preventing breast cancer in the opposite breast.
C) Tamoxifen is unlikely to be effective in her case because it is primarily beneficial for ER/PR-positive cancers, not ER/PR-negative cancers.
D) Tamoxifen is primarily used for HER2-positive breast cancers and should be considered.
C) Tamoxifen is unlikely to be effective in her case because it is primarily beneficial for ER/PR-positive cancers, not ER/PR-negative cancers.
Finasteride helps in reducing the incidence of prostate cancer primarily by:
A) Inhibiting the conversion of testosterone to dihydrotestosterone (DHT)
B) Increasing testosterone production.
C) Blocking the action of estrogen in the prostate.
D) Enhancing the immune response to prostate cells.
A) Inhibiting the conversion of testosterone to dihydrotestosterone (DHT)
Prostate cells proliferate due to DHT from testosterone
→ Blocking the conversion of testosterone to DHT via 5-reductase can prevent proliferation
What is the main role of dihydrotestosterone (DHT) in the development of prostate cancer?
A) DHT inhibits the growth of prostate cancer cells.
B) DHT is a potent stimulator of prostate cell proliferation, contributing to the development and progression of prostate cancer.
C) DHT has no role in prostate cancer and is primarily involved in liver metabolism.
D) DHT reduces the risk of prostate cancer by enhancing immune surveillance.
B) DHT is a potent stimulator of prostate cell proliferation, contributing to the development and progression of prostate cancer.
Case 1: A 60-year-old man with no history of prostate cancer is considering preventive measures due to his concern about developing the disease. He comes across information about finasteride and asks his physician whether he should take it to reduce his risk.
Question:
Which of the following should be explained to the patient regarding the use of finasteride for prostate cancer prevention?
A) Finasteride is ineffective in reducing prostate cancer risk and should be avoided.
B) Finasteride can reduce the risk of developing prostate cancer by inhibiting the conversion of testosterone to DHT
C) Finasteride is only useful in individuals with a family history of prostate cancer and is not recommended for others.
D) Finasteride increases the risk of prostate cancer and should be used with caution.
B) Finasteride can reduce the risk of developing prostate cancer by inhibiting the conversion of testosterone to DHT
Which of the following infections is most strongly associated with the development of gastric adenocarcinoma?
A) Hepatitis B
B) Human papillomavirus
C) Helicobacter pylori
D) Epstein-Barr virus
C) Helicobacter pylori
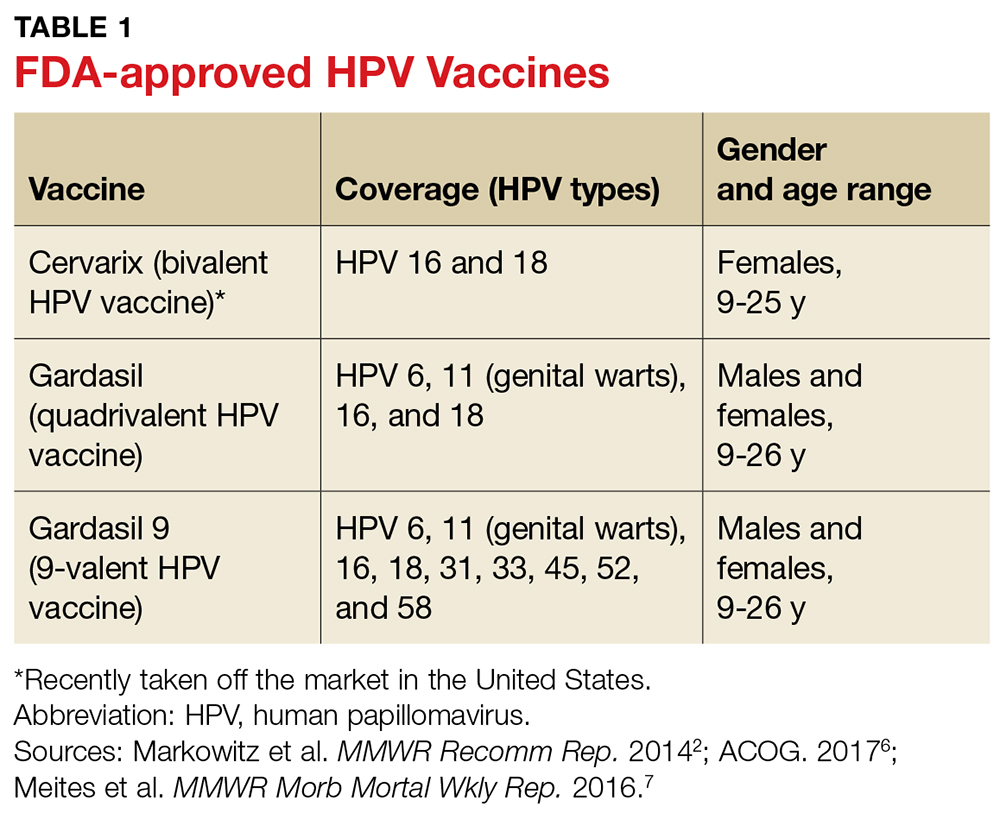
The quadrivalent HPV vaccine offers protection against which of the following HPV strains that are linked to cervical cancer?
HPV 6, 11, 16, and 18
A 55-year-old woman with BRCA1 mutation is considering prophylactic surgery to reduce her risk of breast and ovarian cancers. What surgery surgical procedure would be appropriate for this purpose?
Bilateral Mastectomy and Oophorectomy (due to BRCA1 → increased risk of ovarian CA)
Case: A 45-year-old man has been diagnosed with chronic hepatitis B. His physician recommends the hepatitis B vaccine for his unvaccinated family members to prevent the spread of the virus and reduce cancer risk.
Question:
Which cancer is primarily associated with chronic hepatitis B infection that the vaccine aims to prevent?
Liver Cancer (HCC)
A 52-year-old woman with a family history of breast cancer asks about the best method of screening. She has no known genetic predisposition. What is the most appropriate recommendation?
A) Annual breast self-examination starting immediately
B) MRI screening every two years
C) Annual or biennial mammography starting immediately
D) Genetic screening for BRCA1 and BRCA2 mutations
C) Annual or biennial mammography starting immediately
Recommended for >50 year old Women and asymptomatic
A 45-year-old woman with BRCA1 mutation is considering options for breast cancer screening. Which of the following screening methods is likely to be more sensitive for her?
A) Mammography
B) Clinical breast examination
C) Breast self-examination
D) MRI
D) MRI
MRI is more sensitive than mammography in detecting breast cancer, especially in women with BRCA1 or BRCA2 mutations. These women are at higher risk of developing breast cancer at a younger age, when mammography is less effective due to denser breast tissue.
Screening procedure for patients with high risk women for breast cancer (with genetic predisposition)?
MRI

Case 2: A 40-year-old woman has undergone breast augmentation and asks about appropriate breast cancer screening. She is particularly concerned because her mother was diagnosed with breast cancer at age 55.
Question:
Which screening method would be most appropriate for this patient given her history of breast augmentation?
A) Annual mammography
B) Breast self-examination only
C) Annual or biennial MRI
D) Genetic testing for BRCA mutations before screening
C) Annual or biennial MRI
Mammogram cannot be USED FOR THOSE WHO WENT THROUGH AUGMENTATION!!!
Best age for mammogram screening?
>50 year old women (asymptomatic)
**HIGHEST BENEFIT at 40 years old
A 33-year-old woman has had three consecutive normal Pap smears. She is in a monogamous relationship and has no new sexual partners. How often should she be screened for cervical cancer?
A. Annually.
B. Every 2–3 years.
C. Every 5 years.
D. Screening is no longer needed.
B. Every 2–3 years.
1-3 years is also possible
**Recommended screening interval is every 2–3 years for women aged 30 and over.
What screening procedures can be used to detect Colorectal Cancer?
Colonoscopy
Fecal Occult Blood Testing
DRE
SigmoidoscopyCT Colonography
A 58-year-old woman with a family history of breast cancer is considering starting screening. She has not had any previous breast imaging. What is the recommended course of action?
A. Start with annual mammograms.
B. Begin with a breast MRI and then annual mammograms.
C. Begin with a clinical breast exam only.
D. Start with a breast self-examination.
B. Begin with a breast MRI and then annual mammograms.
Due to (+) family history of breast cancer
A 62-year-old woman with a hysterectomy for benign reasons asks if she should continue screening for cervical cancer. What should you advise?
A. Continue Pap smears annually.
B. Stop screening for cervical cancer.
C. Begin HPV testing every 5 years.
D. Continue Pap smears every 3 years.
B. Stop screening for cervical cancer.
Women who have had a hysterectomy for non-cancerous reasons do not need to continue cervical cancer screening.
A 50-year-old patient has a positive result on a fecal immunochemical test (FIT). What is the next step in screening?
A. Repeat the FIT test in 6 months.
B. Schedule a sigmoidoscopy.
C. Schedule a colonoscopy.
D. Begin treatment for colorectal cancer
D. Begin treatment for colorectal cancer.
A 55-year-old smoker with a 25-pack-year history is discussing lung cancer screening options. What is the most appropriate recommendation?
A. Annual chest X-ray.
B. Annual low-dose CT scan.
C. Annual sputum cytology.
D. No screening until age 60.
B. Annual low-dose CT scan.
Low-dose CT scans are recommended for high-risk individuals, such as those with significant smoking history, to effectively screen for lung cancer.
A 50-year-old woman with a family history of ovarian cancer undergoes CA-125 testing and transvaginal ultrasound. What is a significant limitation of these screening methods?
A. High sensitivity but low specificity.
B. High false-positive rates and low sensitivity.
C. Low cost and high specificity.
D. Complete absence of false positives.
B. High false-positive rates and low sensitivity.
CA-125 testing and transvaginal ultrasound have high false-positive rates and low sensitivity, making them not ideal for routine ovarian cancer screening.
What screening procedures can be used to detect Ovarian Cancer?
Serum CA-125 Assay
Transvaginal US
Adnexal Palpation
What screening procedures can be used to detect Lung Cancer?
CXR
Sputum Cytology
What screening procedures can be used to detect Prostate Cancer?
DRE
Serum PSA (prostate-specific antigen)
What screening procedures can be used to detect Endometrial Cancer?
Transvaginal US
Endometrial Sampling