Lifespan Final Pt 1 (Terms)
1/35
Earn XP
Description and Tags
Lectures 1-4
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
What is reliability(2)? Validity? Clinical utility?
Name the 2 types of reliability you need to know.
Reliability: Consistency
Inter-rater reliability (would another clinician arrive at the same conclusion)
Test-retest reliability (would we arrive at the same conclusion at a different time?)
Overall: consistency of diagnosis across clinicians and time
Validity: Does it give us correct and accurate information? Does the diagnosis reflect a real, coherent condition?
Clinical Utility: Something has clinical utility if it provides useful information about prognosis/ treatment for practicing clinicians. Does it help guide treatment, prognosis, and communication?
Validity = Is the test accurate?
Clinical utility = Is the test useful?
What is the DSM definition of a disorder?
2 aspects ______ (subjective) or ______ subjective.
A syndrome is characterized by clinically significant disturbance in an individual’s ______, _______, or ______, that reflects dysfunction in the ______, ______, or _______ processes underlying mental functioning.
Mental disorders are usually associated with…
What does not count as a mental disorder? (2)
DSM/ICD - distress (subjective) or impairment (objective)
A syndrome characterized by clinically significant disturbance in an individual's cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning. Mental disorders are usually associated with significant distress or disability in social, occupational, or other important activities.
An expectable or culturally approved response to a common stressor or loss, such as the death of a loved one, is not a mental disorder. Socially deviant behavior (e.g., political, religious, or sexual) and conflicts that are primarily between the individual and society are not mental disorders unless the deviance or conflict results from a dysfunction in the individual, as described above."
What is the social constructionist perspective on psychopathology?
You cannot define mental illness purely through ________, because mental illness is______
Our diagnoses come from _________ about what is ____ or ____, not just from ______.
What counts as mental illness changes depending on…
Diagnoses are ______, not _______
DSM categories change over time because __________ change.
When clinicians diagnose, they are using _____, ex.____: how someone ________
Overall: Diagnosis always carries an element of _______ shaped by ______.
You cannot fully define mental illness purely through science, because mental illness is socially defined.
Our diagnoses (like “depression,” “borderline,” “ADHD”) come from shared cultural beliefs about what is “normal” or “abnormal,” not just from biology.
What counts as mental illness changes depending on the period in history and the culture.
Diagnoses are tools, not eternal truths.
DSM categories change over time because society’s needs and values change (e.g., autism reclassified, PTSD added, hysteria removed).
When clinicians diagnose, they are using implicit social norms (e.g., what counts as “too anxious,” “too sad,” “too impulsive”)- how someone SHOULD behave and feel.
Diagnosing always carries an element of judgment shaped by culture.
Big picture: Social constructionism says diagnoses are not neutral or purely scientific — they reflect society’s values.
What are the benefits vs.drawbacks of categorical diagnoses?
Drawbacks (TRY ADN REMEMBER ACRONYM)(4) (Can He Invite Bob?)
Benefits (3, with 1 sub3) (E, C, T)
Drawbacks
Comorbidity (the rule rather than the exception)
Heterogeneity within a disorder category (people with the same diagnosis could look completely different).
Imprecision: when someone doesn’t fit any of the categories
Boundary questions (ex. anorexia or bulimia? Oppositional defiant or conduct disorder? schizophrenia or schizoaffective disorder?) Some disorders seem to blur into each other.
Benefits
Easy to use for communication, billing, and treatment planning
Clear diagnostic labels help clinicians coordinate clinical care
Helpful for decisions like “yes/no” treatment eligibility
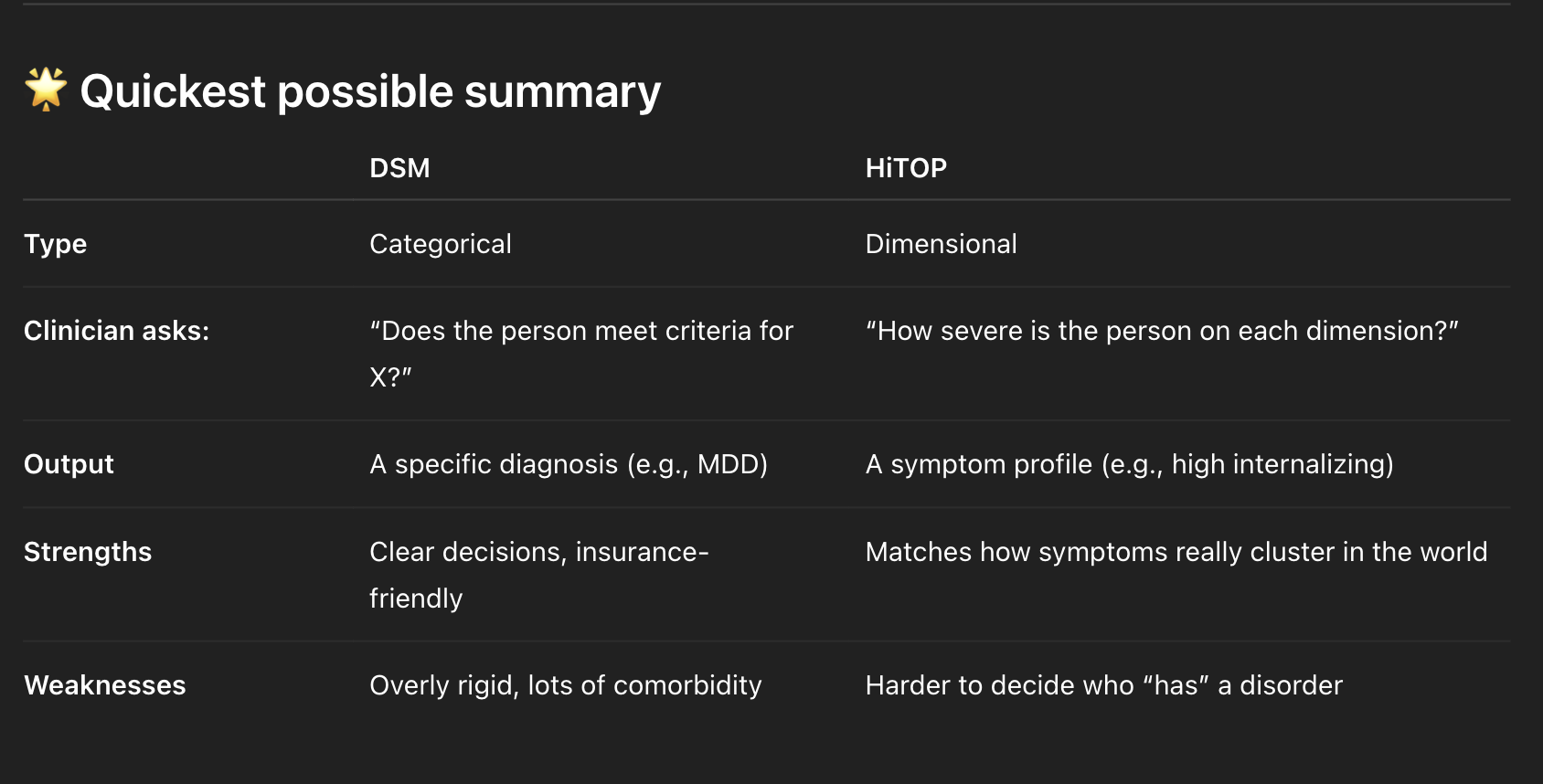
What are the benefits vs drawbacks of dimensional diagnoses?
Benefits (3)
Capture _____ and _____ more accurately
Better reflect…
Reduce ______ by…
Drawbacks (3)
Harder to…
Not as ______ or _______
Less established for….
Benefits
Capture symptom severity and variation more accurately
Symptoms exist on a continuum, so dimensional models reflect how much distress or impairment someone has, not just yes/no.
Better reflect underlying biology and personality traits
Dimensions align more closely with how traits, brain systems, and risk factors vary naturally across people.
Reduce comorbidity by understanding shared dimensions.
Overlapping diagnoses are explained by shared underlying dimensions rather than multiple separate disorders (could explain someone having both depression and eating disorder: high level of internalizing)
Drawbacks
Harder to implement in clinical practice
Clinicians are trained to use categories, and dimensional models take more time and assessment
Not as intuitive or easy to communicate
Saying someone is “high on negative affect” is less clear than giving a simple diagnosis
Less established for insurance and diagnostic decision-making
Insurance, documentation, and treatment guidelines are built around categorical diagnoses.
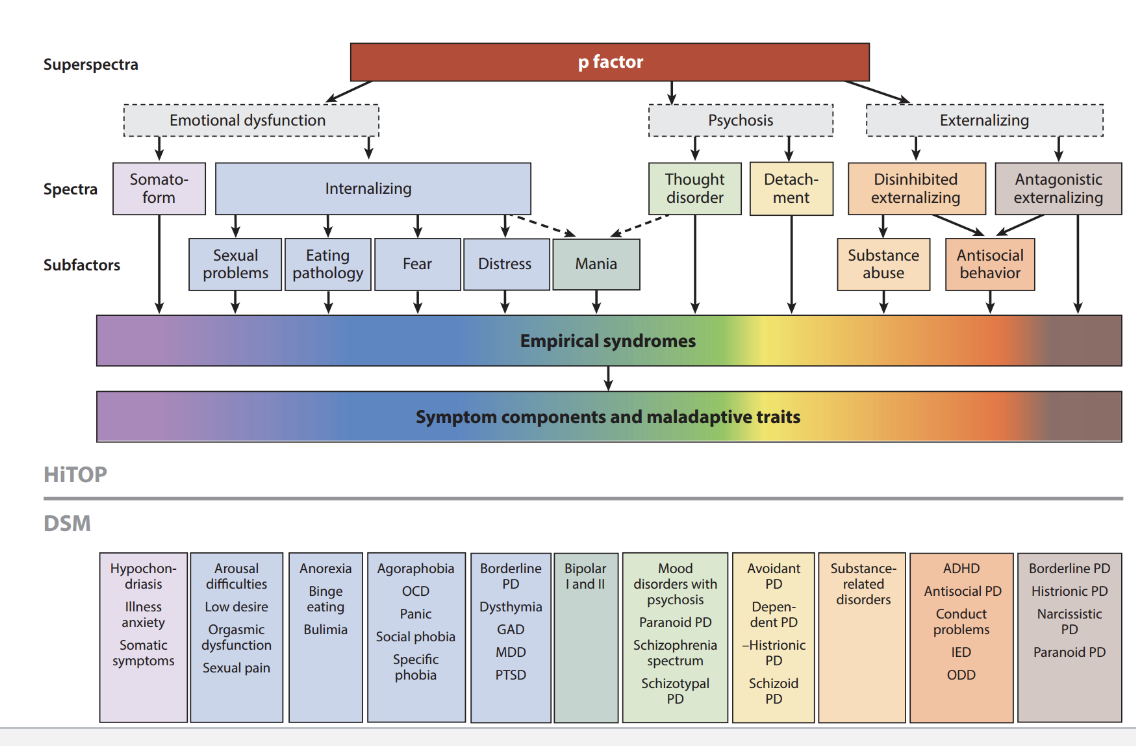
What is HiTop? Goals?
_____ rating system that relies on…
Goals
Improve ____
Eliminate ______ problems by…
Align more closely with…
Continual ____ based on______
GIVE EXAMPLE (INTERNALIZING ______)
Developed dimensional rating system that relies on statistically derived constructs.
Goals
Improve reliability
Eliminate comorbidity problem by arranging from broad to specific
Align more closely with genetic and neurobiological research
Continual revision based on empirical evidence
Step 1: Gather symptoms → map to components
Panic attacks → Fear
Chronic worry → Distress
Restriction + bingeing → Eating pathology
Shame/perfectionism → Negative affectivity
⭐ Step 2: Identify elevated subfactors
This client shows elevations in:
Fear
Distress
Eating pathology
✔ These are real HiTOP subfactors.
⭐ Step 3: Identify spectrum
Fear + Distress + Eating pathology
→ Internalizing spectrum
✔ This is exactly what HiTOP is designed to do.
⭐ Step 4: Identify superspectrum
Internalizing loads onto Emotional Dysfunction
Core vulnerability = high negative affectivity
✔ This is the deepest explanatory level.
“This client shows elevated Internalizing, particularly in the Fear, Distress, and Eating Pathology subfactors, reflecting a broader vulnerability within the Emotional Dysfunction superspectrum.”
What are the potential drawbacks of the HiTOP system? (3)
Drawbacks
Clinical utility: If it’s all dimensional, what counts as a mental disorder? What’s the cutoff?
Does not account for all DSM diagnoses or for changes in diagnoses over time
Are factor analytics of primary importance? : HiTOP is built mostly from statistical clustering, but that may not fully capture causes, mechanisms, or meaningful distinctions between disorders.
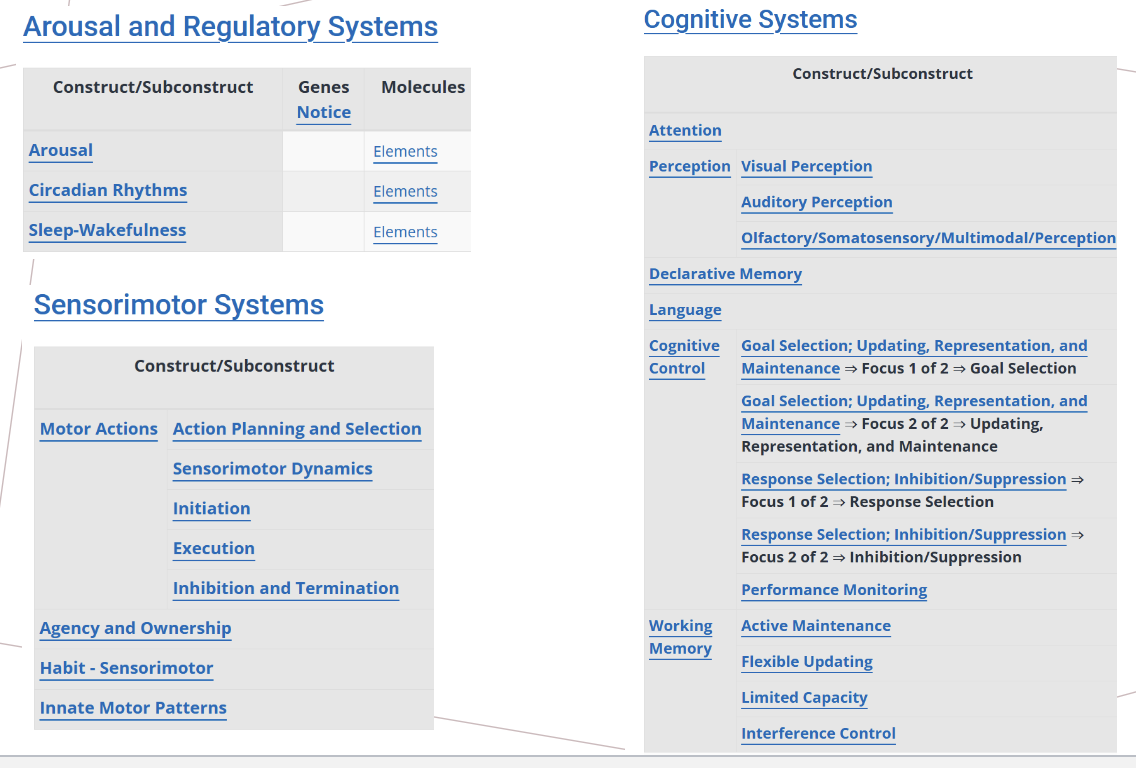
What is RDoC? Purpose? How does it contextualize psychopathology? What are the major domains (6 total).
In a sentence, RDoC is a research tool that helps to conceptualize mental illness, leading to better diagnosis, prevention, intervention, and cures.
Purpose: “foster new research approaches that will lead to better diagnosis, prevention, intervention, and cures
Meant more for research than as a useful diagnostic system
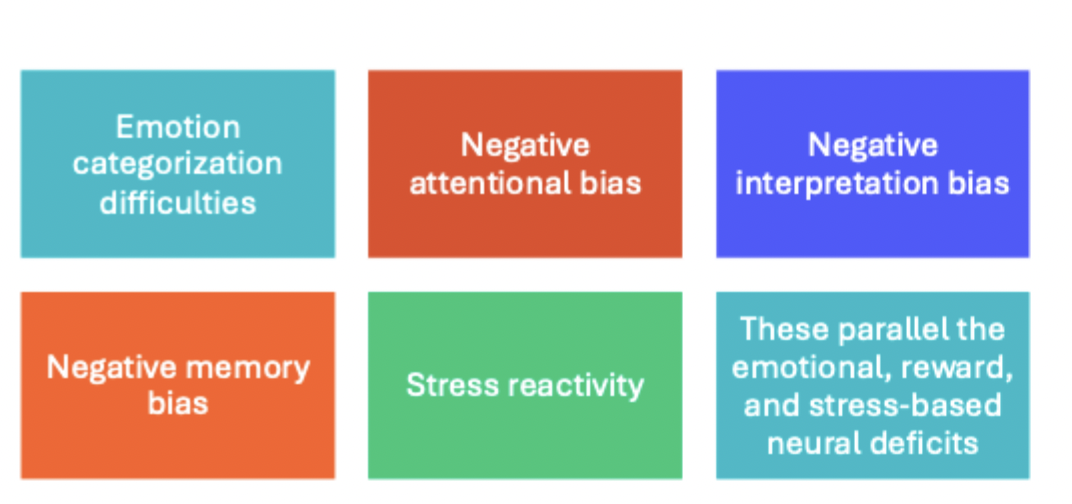
Contextualizes psychopathology as deviations from major domains of basic neurobiological functioning (example of some of the major domains pictured below)
Major Domains
Negative valence systems
Positive valence systems
Social Processes
Arousal and Regulatory systems
Cognitive systems
Sensorimotor systems
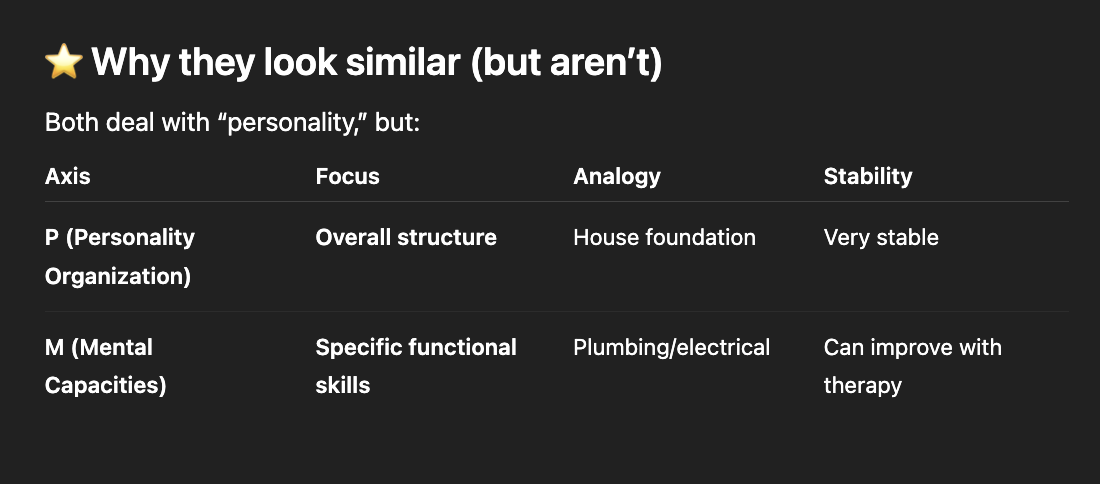
What is the Psychodynamic Diagnostic Manual (PDM)
Name and describe the 3 axes (what are the 3 foci?). Differentiate between the first two.
What is the purpose of the PDM?
How is the PDM organized?
WHEN YOU RETURN TO THIS FLASHCARD: just describe the P axis. (4).
PDM focuses on personality, mental functioning, and subjective experience. Purpose is to go beyond symptoms and provide psychodynamic context. Often provides a "whole person" perspective on mental health. It offers a more detailed and clinically rich case formulation by including a patient's internal experiences, personality patterns, and mental functioning alongside their surface symptoms.
Three axes (P,M,S)
Personality organization (Can be psychotic, borderline, neurotic, or healthy). “Who is this person?” (How cohesive their identity is, how stable their relationships are, how well they test reality, and how primitive vs mature their defenses are).
Mental capacities : “How does this person function psychologically day-to-day?” Skills and capacities the person uses in daily life (regulating emotions, making stable, goal directed choices, understanding others minds, using defenses effecitvely).
Symptom Patterns/ Subjective experience . This is closer to DSM categories but viewed psychodynamically. “What symptomatic patterns are present, and what is their psychological meaning?”
The S axis is analogous to the diagnoses in the DSM.
PDM organized developmentally (Adulthood, adolescence, childhood, infancy, later life).
Example:
Quick real example Client: 28-year-old who struggles with abandonment, identity instability, and impulsivity
P Axis:
Borderline personality organization (unstable identity, primitive defenses)
M Axis:
Strength: understands others’ intentions fairly well
Weakness: emotion regulation is severely impaired
Weakness: uses splitting under stress
Moderate capacity for self-reflection
S; Symptom presentation: fear of abandonment, impulsive, self harm.
OUTPUT:
A proper PDM output always addresses all three axes.
This client presents with borderline-level personality organization (P axis), marked impairments in affect regulation and defensive functioning with moderate reflective capacity (M axis), and prominent symptoms of abandonment fear, impulsivity, and self-harm experienced as overwhelming and dysregulating (S axis).
Notice:
The P axis gives the global classification.
The M axis gives the functional detail.
What is Rosenhan’s basic argument in “On Being Sane in Insane Places”?
Psychiatric diagnoses often cannot reliably distinguish ______ from______ and labels…
Once someone is labeled as mentally ill…
The same behavior is seen as _____ ____, but ____ ____.
Hospitalization leads to ______. How (4)
Counter arguments?
Diagnosis of ________ was reasonable- why?
Psychiatric diagnoses accomplish… even if…
This is why we need…
Rosenhan argues that psychiatric diagnoses often cannot reliably distinguish sanity from insanity, and that labels powerfully shape how behavior is interpreted.
Because once someone is labeled mentally ill, all their behaviors are filtered through that label, leading staff to interpret normal actions as symptoms and ignore contradictory evidence.
Context shapes how clinicians interpret behavior: Behavior in psychiatric hospitals is interpreted according to the context of “mental illness”, meaning the same behavior is seen as normal outside but pathological inside.
Hospitalization leads to depersonalization: Depersonalization occurs when patients are treated as objects rather than people—through power imbalances, lack of privacy, minimal staff interaction, and a rigid hospital structure that strips individuals of identity and autonomy.
Therefore: the diagnostic process is flawed and heavily context-dependent
Counter arguments
The diagnosis of “schizophrenia in remission” was reasonable based on the pattern of symptoms described.
Psychiatric diagnoses accomplish most of what they’re supposed to (communicating symptoms that cluster together to facilitate treatment) even if they are somewhat lacking in reliability and validity.
This is why we need specific criteria: criteria are too vague, too subjective, and too dependent on the context.
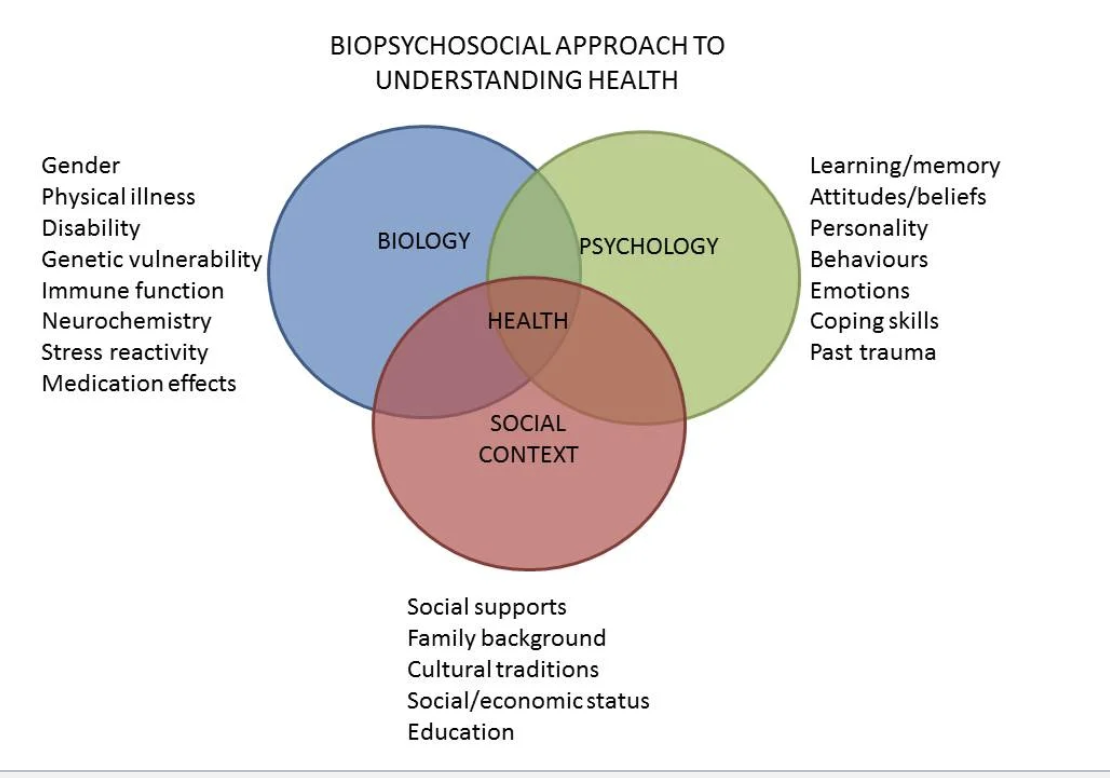
What is the biopsychosocial model? How does it shed light on the development and maintenance of psychopathology?
helps explain why…
Explain biological maintenance cycle, psychological maintenance cycles, and social maintenance cycles.
Framework proposing that psychopathology arises from the interaction of three broad domains (Biological factors, psychological factors, social factors)
BPS model emphasizes multiple determinants interacting over time.
How does it shed light on the development and maintenance of psychopathology?
BPS model helps explain why two people with the same stressor may have very different outcomes.
Biological vulnerability, psychological patterns, and social stressors interact to create risk pathways.
ex. Depression is influenced by genetic liability, but also by psychological factors like anhedonia and social factors like economic strain.
Maintenance
Biological maintenance cycles include: HPA Axis and stress physiology (causing chronic stress), sleep disruption, neurotransmitter dysregulation
Psychological maintenance cycles include: avoidance, rumination, cog distortions
Social maintenance cycles: Interpersonal conflict, loneliness, stigma
What are the purposes and drawbacks of diagnosis? (not of categorical vs dimensional)
Purposes (T, C, I)
Drawbacks (S, I, P, D)
Purposes
Treatment planning and prognosis
Communication with other clinicians within and across disciplines
Insurance and reimbursement
Drawbacks
Stigma
impacted by cultural norms and values (What counts as a “symptom” depends on cultural expectations, which can lead to over- or under-diagnosis in marginalized groups.)
Pathologizing the normal
Does not always matter for treatment/ prognosis
The DSM aims to be atheoretical- what does this mean?
Addresses what disorders look like- not why they occur.
What is the “P” factor? How does this apply in real life?
The idea that there is a general tendency to develop psychopathology.
Leads to this question: For someone who has been diagnosed with multiple disorders, is it because they have an overall tendency toward psychopathology or because they truly have various distinct disorders?
Name 4 alternative diagnostic models discussed in class.
HiTOP: Factor analytic studies
RDoC: Neurobiological studies
PDM: Psychodynamic research and treatment
Alternative DSM-5: For personality disorders only, personality research
Give a quick summary of the differences in diagnosis using HiTOP vs. DSM
What the clincian asks
What the output of the system is
strengths
weaknesses
What are the Pros (1) and Cons (2) of RDoC?
Pros
Potentially useful for typing together research at multiple levels of analysis
Cons
Reliability and validity of constructs is unclear
Importance to psychopathology and treatment is questionable
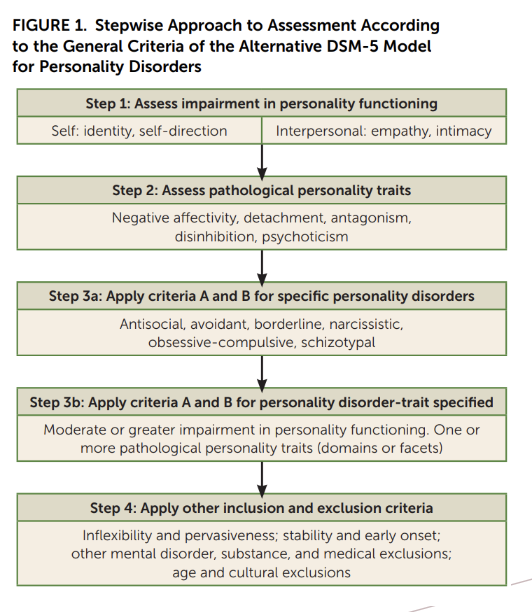
Describe the Alternative DSM-5 for personality disorders (AMPD).
What are the 2 criteria in this model?
Name Steps 1-4
Give an example of how you might diagnose someone using this model. (This is where you will list steps 1-4)
Hybrid categorical/ dimensional style
2 Criteria
A: Level of personality functioning
B: Pathological personality traits
Steps 1-4
Assess impairment in personality functioning
Self: identity, self direction
Interpersonal: empathy, intimacy
Assess pathological personality traits
Negative affectivity, detachment, antagonism, disinhibition, psychoticism
3a. Apply criteria A and B for specific personality disorders
antisocial, avoidant, borderline, narcissistic, obsessive compulsive, schizotypal
3b. Apply criteria A and B for personality disorder trait-specified
Moderate or greater impairment in personality functioning. One or more pathological personality traits (domains or facets)
Apply other inclusion and exclusion criteria (inflexibility and pervasiveness; stability and early onset; other mental disorder, susbtance and medical exclusions; age and cultural exclusions.
⭐ Case Example: “Maria,” age 27
Maria comes to therapy due to intense, unstable relationships, impulsive decisions, chronic emptiness, and episodes of anger she later regrets.
🔶 Step 1: Assess impairment in personality functioning
(Does the person show impairment in self and interpersonal functioning?)
Self-functioning
Identity: Maria’s self-image shifts dramatically depending on whom she is with; she reports feeling “like a different person every day.”
Self-direction: Goals are unstable; she impulsively changes job plans or relationships without long-term considerations.
Interpersonal functioning
Empathy: Struggles to understand others’ perspectives in moments of distress; often misreads benign actions as rejection.
Intimacy: Intense, chaotic relationships marked by desperate efforts to avoid abandonment.
👉 Conclusion:
Maria shows moderate-to-severe impairment in both self and interpersonal functioning. (Step 1)
This satisfies Criterion A impairment.
🔶 Step 2: Assess pathological personality traits
(This is Criterion B)
Using interview + a measure like the PID-5, Maria shows:
Negative Affectivity
Emotional lability
Anxiousness
Separation insecurity
Disinhibition
Impulsivity
Risk-taking
(Possible) Antagonism
Hostility when distressed
👉 Conclusion:
Maria demonstrates elevated Negative Affectivity and Disinhibition, with some Antagonism facets. Criterion B
🔶 Step 3a: Apply Criteria A and B for specific personality disorders
Compare her impairment + traits to the six PD types in the AMPD:
Antisocial
Avoidant
Borderline
Narcissistic
Obsessive–compulsive
Schizotypal
Maria’s pattern (instability, impulsivity, fear of abandonment, negative affectivity, emotional lability) maps directly onto Borderline Personality Disorder criteria.
👉 Conclusion:
Maria meets Criteria A and B for Borderline Personality Disorder under the Alternative DSM-5 Model.
(If she did NOT fit one of the six PDs)
we would go to Step 3b and diagnose:
Personality Disorder – Trait Specified (PD-TS)
with her elevated traits listed.
But Maria DOES fit a specific PD, so we stay with 3a.
🔶 Step 4: Apply inclusion and exclusion criteria In flexibility & Pervasiveness
Her emotional instability appears across work, friendships, and romantic relationships.
Stability & Early Onset
Maria reports these problems since late adolescence.
Not better explained by:
Mood disorder
PTSD
Substance use
Medical conditions
There are no alternative explanations.
👉 Conclusion:
Maria meets inclusion criteria and is not excluded by any rule-outs.
⭐ Final Diagnosis (AMPD Style)
Borderline Personality Disorder
Level of Personality Functioning: Moderate–severe impairment (identity, self-direction, empathy, intimacy)
Pathological Traits:
Negative Affectivity (emotional lability, anxiousness, separation insecurity)
Disinhibition (impulsivity, risk-taking)
Antagonism (hostility)
Biopsychosocial model diagram
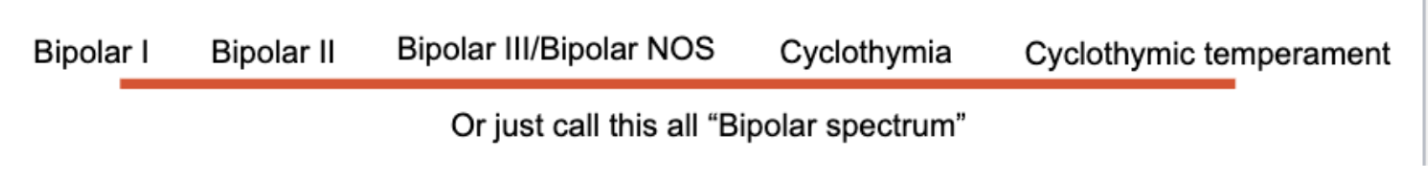
What is the concept of bipolar spectrum and how does it differ from our current diagnostic system for mood disorders?
First, Name and describe the disorders on the spectrum. (4)
What is the overall takeaway from this?
First of all, explanation of the disorders in the image.
Bipolar III: Antidepressant-induced hypomania (soft bipolar).
Bipolar NOS: Bipolar symptoms that don’t meet full criteria.
Cyclothymia: 2+ years of subthreshold hypomanic + depressive symptoms.
Cyclothymic Temperament: Lifelong personality style with cyclic highs/lows.
Overall takeaway: we have a system for bipolar disorders that is already spectrum-like, some people say maybe just a general spectrum would work better than specific diagnoses.
What is complex ptsd and how does it differ from non-complex PTSD?
In addition to the core PTSD symptoms, what else does CPTSD include?
Complex PTSD: PTSD that develops after prolonged, repeated, often interpersonal trauma, especially in childhood. In addition to the core PTSD symptoms (intrusions, avoidance, negative mood/cognition changes, hyperarousal), cPTSD includes more global, long-term changes in personality and functioning, often called disturbances in self-organization
Emotion regulation problems (chronic anger, shame, numbness, self-harm)
Negative self-concept (I am worthless/ bad/ deep shame)
Interpersonal difficulties (mistrust, unstable relationships, feeling permanently damaged or different)
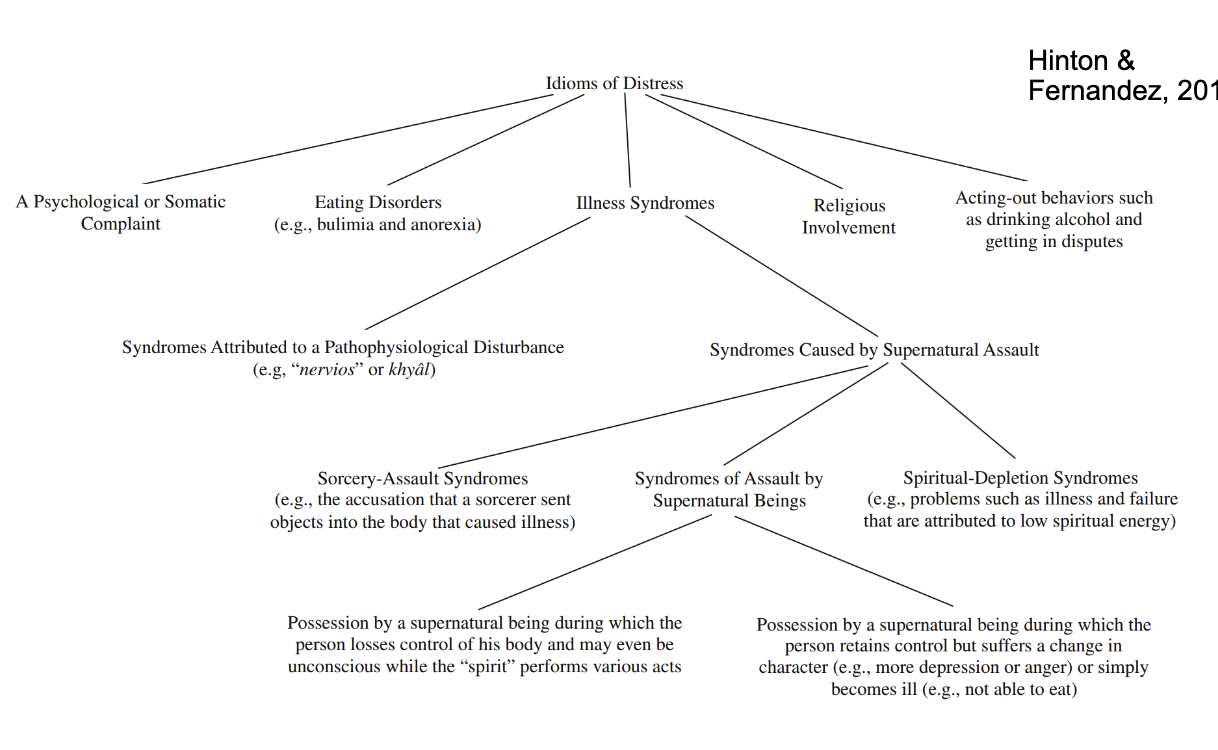
What are idioms of distress?
Culturally _______, _____ ways of expressing _____, ____, or _____
A bridge between _____, ____, and _____
______ that combine _____, _____, _____, and ______ meanings.
How might they appear? (4) PBSS
Idioms of distress
Culturally patterned, recognizable ways of expressing stress, trauma, or emotional difficulty
A bridge between mind, body and culture
Expressions that combine somatic, emotional, interpersonal, and spiritual meanings
They can appear as:
Physical symptoms (“my heart is hot,” headaches, weakness)
Behavior patterns (withdrawal, drinking, fighting)
Spirit or supernatural explanations/ religious experience (possession, trance states, rituals)
Sociocultural constructs (e.g., “nervios,” evil eye, spirit loss)
Describe the basic structure of Prolonged exposure treatment for PTSD
Core components? (2 core components, describe each.
Goal?
Basic Structure
Behavioral treatment based on habituation
Patient repeatedly confronts trauma memories and avoided situations
Core components
Imaginal exposure
Patient retells the trauma, aloud, in detail, repeatedly, in session.
Often uses a written narrative outside of the session
In vivo exposure
Systematically facing avoided reminders (places, situations, triggers)
Goal: Reduce fear response by breaking avoidance patterns and allowing emotional processing.
Describe the psychological perspective on mental illness
Focuses on ______, ______ and _____ that contribute to
Psychological theories highlight how people interpret _____, manage ______, and respond to _______
______ and _____ vulnerabilities, such as….. play a major role in why symptoms appear and persist
Treatments target…
Focuses on internal emotional processes, cognitive patterns, and learned behaviors that contribute to mood disorders.
Psychological theories highlight how people interpret loss, manage self-esteem, and respond to stressors.
Cognitive and emotional vulnerabilities—like rumination, negative self-beliefs, or impaired reward processing (anhedonia)—play a major role in why symptoms appear and persist.
Treatments target thoughts, coping skills, and behavioral activation.
Describe the Biological perspective on mental illness
Explains mood disorders through _____, _____, and ______.
This includes… particularly relevant to __________.
Biological models guide treatments such as…
Much research in this area aims to distinguish between ____ and _____, and understand…
Explains mood disorders through genetics, neurobiology, and brain-based mechanisms.
This includes neurotransmitter systems, neural circuitry involved in reward and mood regulation, and heritable risk—particularly relevant in bipolar disorders.
Biological models guide treatments such as medication, ECT, TMS, and other somatic approaches.
Research aims to distinguish unipolar vs. bipolar depression and understand chronic, recurrent mood dysregulation.
What is the social perspective of mental illness? (not social constructionist). (list 3)
Emphasizes how ______, ______, _____, and _______ shape risk for mood disorders. Examples if you want.
_______ matters. example?
The social model highlights _______ to mental health.
Emphasizes how life circumstances, relationships, socioeconomic status, and cultural context shape risk for mood disorders.
Social factors such as low income, unemployment, lower education, gender-related stress, and experiences of loss or instability increase vulnerability (WHO data).
Access to care matters: for example, Medicaid expansion reduced depression rates by improving resources and decreasing financial strain.
The social model highlights structural contributors to mental health.
What is the Bipolar Spectrum Concept?
View bipolarity as a continuum of _________
Includes soft bipolar conditions like… (4)
Returns to _______’s idea that _______, not _______ defines mood illness.
Better matches _______, _______ and ______.
Bipolarity is more _____ and more _______ than the DSM categories suggest.
Views bipolarity as a continuum of mood dysregulation.
Includes soft bipolar conditions like subthreshold hypomania, antidepressant-induced hypomania, cyclothymia, and mixed states.
Returns to Kraepelin’s idea that recurrence, not polarity, defines mood illness.
Better matches real-world genetics, course, and treatment response.
Bipolarity is more common and more varied than the DSM categories suggest
How does the Bipolar Spectrum Concept differ from the Current DSM system?
This is important because These sub threshold patients behave more like bipolar patients in terms of ________, ______, and ______.
DSM uses a narrow, categorical approach
DSM 5 splits mood disorders into Bipolar and Major Depressive disorder
This follows Leonhard’s approach, not Kraepelin’s
Because of these strict boundaries, many people with bipolar physiology get labeled as “unipolar depression.”
Spectrum model uses a Dimensional, Broader View
Spectrum approach argues
Bipolar disorders do not exist in strict boxes
Many people fall in the middle zone (ex. short hypomania, antidepressant induced hypomania, mixed features, cyclothymic temperament)
These patients behave more like bipolar patients in terms of course, family history, and medication response.
What are the treatment implications of using a DSM vs spectrum based approach for soft/ unspecified bipolar disorders?
DSM
For soft/ unspecified bipolar disorders, these people are often treated with ______, which may….
They are then labeled as…
Spectrum based approach
Depression responds much better to ______ or ______, not _____
_______ induced _______ is not a side effect, it is a diagnostic clue.
Under DSM:
These individuals get treated with antidepressants, which may worsen their illness or cause rapid cycling.
They are often labeled “treatment-resistant depression.”
Under the spectrum model:
Their depression responds much better to mood stabilizers or atypical antipsychotics, not antidepressants.
Antidepressant-induced hypomania is not a side effect—it is a diagnostic clue.
Why do idioms of distress matter?
5 main reasons
Help clinicians understand ______ in a _______ way. Provide examples.
They prevent ______. Provide ex.
They shape _________. Provide ex.
They reveal the _____ of suffering. Helps the clinician understand what ___________, not just the _______.
They support _______ and _______. Makes patient feel understood and respected, which improves…(3)
They matter because they help clinicians avoid misdiagnosis, accurately interpret symptoms, and provide culturally responsive care.
1. They help clinicians understand suffering in culturally accurate ways.
A patient may not say “I have PTSD.” Instead, they may describe:
“My soul is weak”
“Wind attacks”
“Nervios”
These reflect real distress, but not in DSM terms
2. They prevent misdiagnosis.
If a clinician interprets a culturally normative expression (e.g., trance, spirit visitation, somatic panic) as:
psychosis
dissociation disorder
panic disorder
3. They shape treatment preferences.
Some cultures treat distress through:
rituals
community healing
religious involvement
herbal medicine
family-based meaning-making
If clinicians ignore this, they may offer care that feels irrelevant or invalidating.
4. They reveal the meaning of suffering.
Idioms of distress communicate
the cause of suffering (supernatural, interpersonal, emotional, medical)
the moral or relational context
how the community understands illness
This helps clinicians understand what the distress means to the patient, not just the symptoms.
5. They support culturally competent assessment and rapport-building.
When clinicians validate and work within idioms of distress, patients feel understood and respected, which improves:
trust
disclosure
treatment compliance
Describe the basic structure of Cognitive Processing Therapy (CPT) for PTSD
What are stuck points?
Core components/ (1 optional)
Goal?
Basic Structure
A CBT-based treatment focusing on how people interpret the trauma and its meaning
Core components
Identify “stuck points”: maladaptive trauma beliefs (ex. self blame)
Cognitive restructuring
Challenge distorted thoughts around safety, trust, power, control, esteem, and intimacy
Optional trauma narrative
CPT is effective with or without a written account of the trauma
Goal: Modify unhelpful beliefs keeping PTSD symptoms active; reduce shame, guilt, and distorted trauma interpretations
Describe the basic structure of Eye Movement Desensitization &Reprocessing (EMDR) for PTSD
Basic structure?
Core components (3)?
3rd phase
both _____ and ______.
Goal?
Basic Structure:
Patient recalls traumatic memories while simultaneously engaging in bilateral stimulation (eye movements, tapping, tones)
Core components
Trauma recall
Patient brings trauma images/ emotions/ body sensations to mind
Bilateral stimulation
Therapist guides eye movements or tapping while the patient processes the memory
Reprocessing phases
Move through sets of stimulation until distress decreases and new, adaptive meanings emerge. This allows the memory to be reprocessed and reconsolidated in a less distressing form.
Goal: Facilitate trauma processing in an “embodied” way with less reliance on verbal description. EMDR does not rely on cognitive restructuring or pure habituation, but on dual-attention memory reprocessing that produces spontaneous cognitive and emotional shifts.
Describe the basic structure of psychodynamic therapy for PTSD
Basic structure
focuses on… rather than_____
Often delivered as…
Core components (4)
Goal?
Basic Structure:
Focuses on emotional, relational, and unconscious impacts of trauma rather than exposure.
Often delivered as Interpersonal Psychotherapy (IPT) in trauma settings.
Core Components:
Recognizing and naming emotions linked to trauma.
Exploring relational patterns:
How trauma affects trust, attachment, and interpersonal safety.
Improving connection:
Reestablishing a sense of safety in relationships.
Meaning-making:
Understanding how trauma shaped identity and internal conflicts.
Goal:
Restore emotional functioning, improve relationships, and integrate the trauma into the self-concept.
Give a quick example of how someone might be diagnosed using the PDM.
P: Client shows a borderline level of personality organization (On a spectrum going from psychotic, borderline, neurotic, healthy)
M: Client demonstrates moderate emotion regulation difficulties, limited functioning under stress, and intact reality testing.
S: Symptoms are consistent with trauma-related anxiety and mood syndrome: hyper vigilance, nightmares, dysphoria, and interpersonal avoidance. Symptoms are tied to early attachment trauma.
What is the interpersonal theory of suicide?
Core idea: A person will not die by suicide unless they both want to die and are able to do so.
Three key constructs:
Thwarted belongingness (“I am alone”)
Perceived burdensomeness (“I am a burden”)
Acquired capability for suicide (“ I can do it”)
Putting it all together: The Interpersonal Theory of Suicide proposes that suicidal behavior occurs when a person experiences both the desire to die—driven by thwarted belongingness and perceived burdensomeness—and the acquired capability to enact suicide through habituation to pain and fear.