Introduction to Cancer Chemotherapy
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
59 Terms
most common treatments
surgery, radiation, chemotherapy
goal of anticancer drugs
to destroy cancer cells
how to achieve goal
single drug or combination of drug used alone or in addition to surgery/radiation
three mechanisms of actions of anticancer drufs
Act on DNA
Inhibit chromatin function
act on hormone/steroid/growth receptors
carcinomas
cancers of epithelial cells lining the surface of organs
sarcomas
cancers of muscle, bone, cartilage, fat, connective tissue
Leukemia
group of blood cancers, usually originate in bone marrow resulting in underdeveloped blood cells
lymphoma
group of cancers that develop from lymphocytes
blastoma
cancers that develop from precursor cells or embryonic tissue
what percent of cancers are carcinomas
80-90%
why are so many types of cancers carcinomas
because epithelial cells are sites of extensive cell proliferation and frequent exposure to chemical/physical danage
what classifies cancer
group of diseases
cells exhibit uncontrolled growth/proliferation
potential to invade surrounding tissue and sometimes colonize in other locations of the body (metastasis)
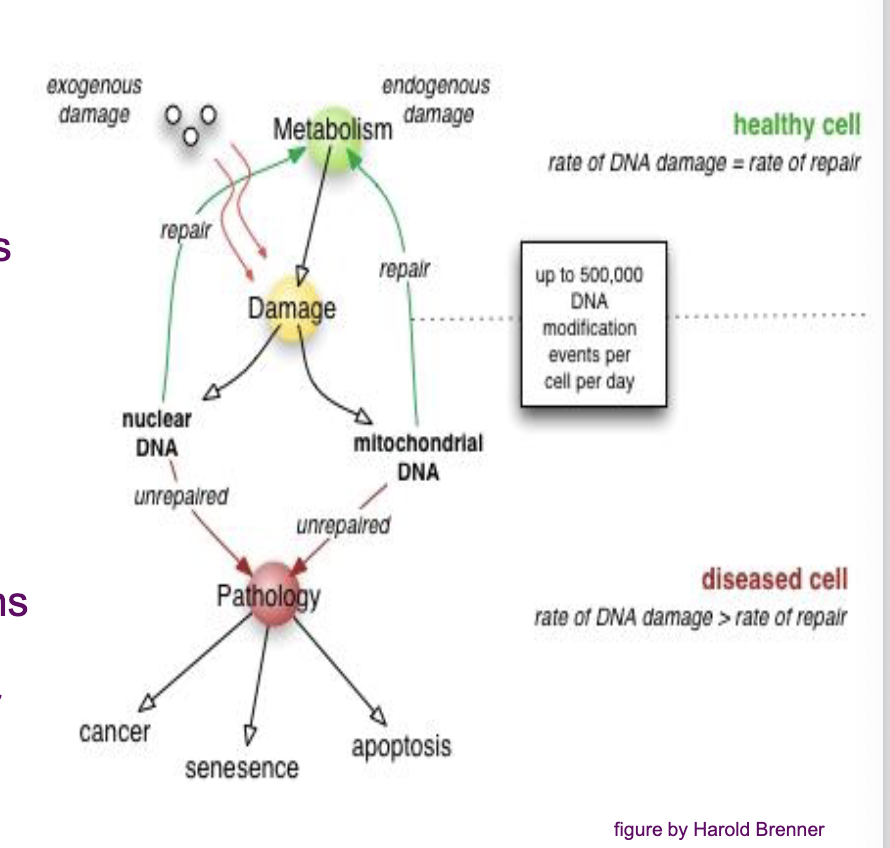
what do most cancers originate from
single aberrant cell
genetic
change in DNA
epigenetic
change in gene expression without change in DNA sequence
what is the normal mutation rate
1010/ gene / lifetime
is a single mutation enough to cause cancer
no
what is required to develop cancer
requires several independent changes in cell lineage
what does tumour progression depend on
(1) mutation/epigenetic alteration rate
(2) selective advantage
(3) proliferation rate
(4) invasiveness
critical cancer genes
DNA proofreading/repair genes
Genes maintaining chromosomal integrity
oncogenes
tumour suppressor genes
genetically unstable cells less fit, therefore,
additional mutations in genes regulating cell death, differentiation or division required
inherited mutations lead to
increased risk of developing cancer
oncogene
gain of function
what mutates in an oncogene
mutation in gene regulating cell growth→ increased mitosis
hormones/growth factors
receptors
cell signaling molecules
transcription factors
tumour suppressor
loss of function
what is mutated in a tumor suppressor
mutation in gene that normally suppresses mitosis and cell growth or induces apoptosis
transcription factors/repressors
regulate cell cycle, apoptosis or DNA repair
angiogensis
larger tumours require oxygen and nutrients
tumours secrete growth factors to induce blood vessel growth
metastasis (least understood and most feared aspect of cancer)
Detachment of cells from parent tumour
entry into lymph/blood vessel
exit circulation
survival and proliferation in new environment
treatment for a primary or localized tumour
surgery/radiation ± chemotherapy
treatment for a metastatic tumour
chemotherapy
what is chemotherapy used for
used with radiation/surgery
before: shrink tumor
after: to kill any remaining cancer cells
what are chemotherapeutic agents used for
to cure cancer or for palliative care
what do most anticancer drugs do
interfere with DNA, therefore, more effective at killing rapidly dividing cells
what is knowledge of cell cycle and tumour growth kinetics important for
design of effective treatments
understanding lack of drug response
which stage of the cell cycle are many drugs most cytotoxic during
many drugs most cytotoxic during S-phase
which stage arse some drugs effective during
M-phase
are drugs effective in G0 phase
No, most drugs ineffective in G0 phase
what is S phase
synthesis phase
what is M phase
metaphase checkpoint
check for:
chromosome spindle attachment
growth fraction
= % dividing cells sensitive to chemotherapy
majority of cells in young tumours are ____________. As the tumour grows, percentage-wise, not as many cells are _____________; it may be more ________, _________ or not _______________
majority of cells in young tumours are actively dividing. As the tumour grows, percentage wise, not as many cells are actively dividing; it may be more aggressive, metastasize, or not respond well to chemotherapy
debulking tumours does what
stimulates proliferation
early metastases have
high growth fraction
fast-growing cancers are
more responsive
several treatment cycles necessary to what
synchronize cells
chemotherapy kills cancer cells via
first-order kinetics (constant %)
at time of detection, how many cancer cells
>/= 1 billion cancer cells
if 99.99% of cells (109) killed (9.999 × 108), 0.01% of cells remain (105 cells)
0.01% of cells remain (105 cells)
109 to 105 =
4 log kill
can cancer growth occur between treatments
cancer growth can occur as tissues recover between treatments
chemotherapy principles
cure requires death of ALL tumour cells
drugs kill constant proportion of tumour cells
tumours detected later require prolonged treatment
drugs have narrow therapeutic index
drug combinations can increase effectiveness and decrease adverse effects
intermittent high-dose therapy more effective
adjuvant therapy may decrease metastases and/or adverse effects
factors influencing patient survival
nature of cancer
pharmacology
patient
failure of anticancer drugs
nature of cancer
type
stage at diagnosis
cell-cycling phase
growth rate
heterogeneity
pharmacology
timing of initiation of treatment
timing of treatments
drug combination
patient
general health
tumour blood supply
immune status
failure of anticancer drugs
lack of specificity (side-effects, dosage limitations)
cancer exhibits/develops resistance
major sites of toxicity
bone marrow (myelosuppression)
GI tract (vomiting, nausea, diarrhea)
hair follicle (alopecia)
Reproductive tract (decreased sperm, menopause, teratogenicity)
secondary carcinogenicity
resistance types
natural (some neoplastic cells inherently resistant)
Acquired (mutation leads to development of resistance)
multidrug resistance (cells express resistance mechanisms that affects multiple drugs e.g. p-glycoprotein that pumps drugs out of the cell)