lecture 13, immune system I
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
functions of the immune system
recognition and elimination of abnormal self-cells (have to know who is who
cancer cells, virally infected cells (develop all the time but the immune system is always watching)
removal of dead/ damaged cells (lots of turn over)
worn red blood cells
protection against disease causing pathogens (something capable of causing disease)
bacteria, parasites, viruses
problems encountered by the immune system include
autoimmunity (target something that was good)
failure to discriminate between self and non-self
MS, rheumatic fever (MS, attribute of autoimmunity, destroy myelin of axon)
allergy
hyper-responsiveness
peanuts, pollen
immunodeficiency (if don’t have immune system increase risk of infection)
pathogens
can cause infection and disease when they invade surfaces/internal environment of the body
pathogens can be
bacteria
eukaryotes
viruses
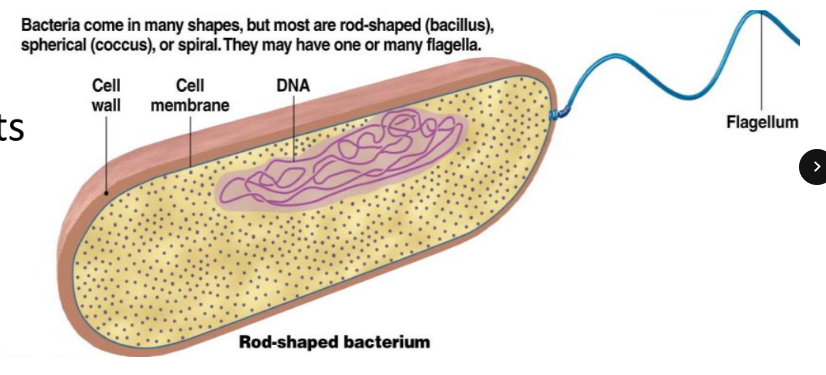
bacetria
prokaryotic cell structure
cell wall made from peptidoglycan → thick sugar layer (thick in gram neg, thin in gram pos)
important target for penicillin, lysozyme
capsule (sticky) may or may not be present external to cell wall
contributes to disease
temperature, pH, nutrient requirements
mainly free living
unicellular
eukaryotes
parasites, fungi
similar cell structure to human cells
bigger
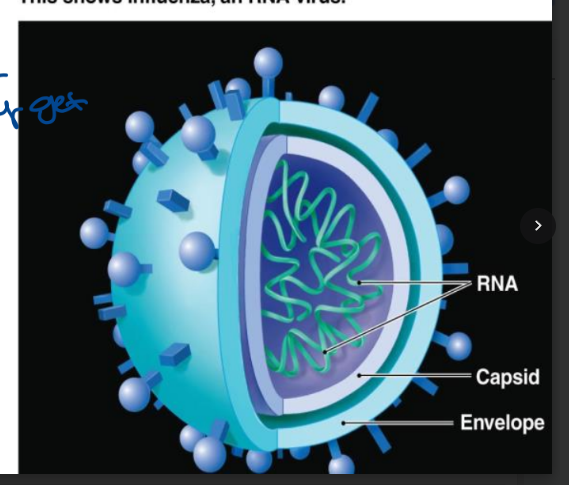
viruses
obligate intracellular parasites (you have what they love)
require host cell machinery for replication
create abnormal cells that must carefully destroyed (because are killing you)
can occasionally be treated with antivirals (can never completely get rid off, not curing just limits replication)
HIV, herpes, influenza
may also be oncogenic (DNA affecting, cancer)
last for long
don’t live independently
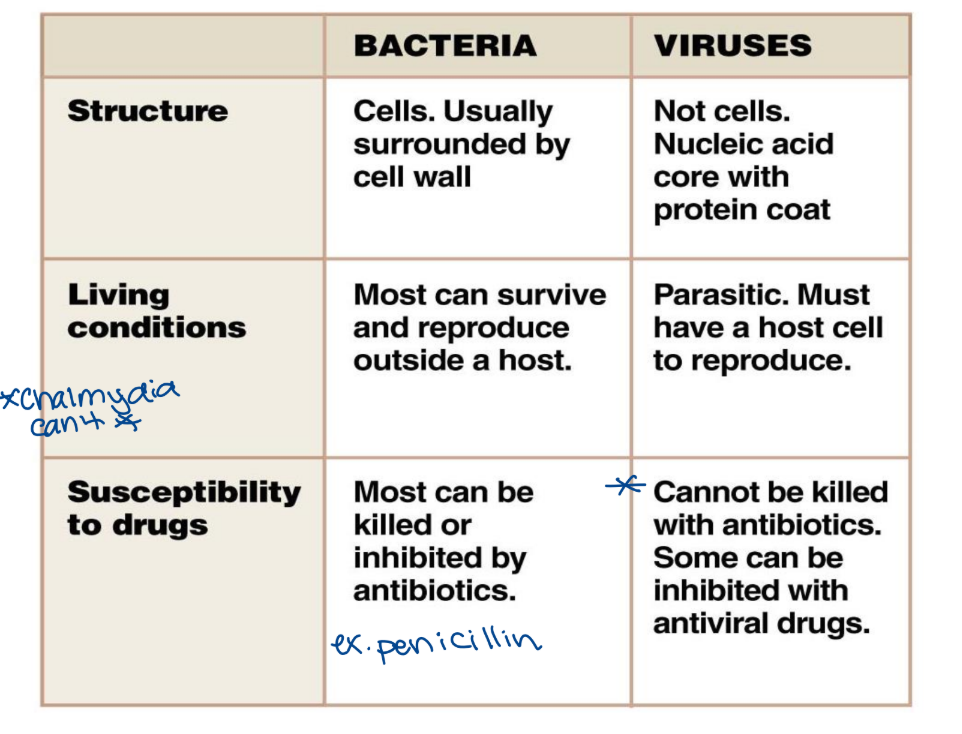
pathogens - bacteria vs viruses
branches of the immune system
the innate immune system
the adaptive immune system
the innate immune system
present at birth
non-specific(doesn’t change, doesn’t learn, doesn’t develop)
activated in response to pathogen associated molecular patterns (PAMPS) ex. recognize a human via hair
NO MEMORY COMPONENT
activates almost immediately in response to foreign organisms (even if not infected yet)
includes physical, chemical, cellular, and molecular components
needs to get one guy but causes destruction to everything in the background
the adaptive immune system
highly specific (only time you accidentally target a wrong one is if they‘re identical)
memory component → activates quickly
develops over time based on exposure to antigens
naturally or via vaccination (not born with it, no memory, if they have to develop it)
includes
i. humoral immunity
ii. cell mediated immunity
the immune system must be able to
detect/identify foreign substances
communicate with other immune cells (you call and let them know what you found so they can send the right team)
recruit other immune cells
coordinate all players of the immune response with one another
destroys/suppress the invader
immune cells signal via cytokines (find cells on a target cell)
proteins released from an immune cell
go on to act on other immune cells that carry the necessary receptor
immunogens
are materials that stimulate an immune response (can be you sometimes, sometimes target something good because it looks bad)
antigens are the segments of the immunogen that specifically interact with elements of the immune system (have many antigens as foreign material → some things are better)
epitopes specifically bind to antibodies
immune system proteins
what your actually binding to an antigen of foreign body
anatomy of the immune system
consists of
lymphoid tissues
leukocytes (key players)
lymhpoid tissue
a. primary tissues
thymus (T lymphocyte maturation) and bone marrow (make all blood cells, B lymphocyte maturation)
site of leukocyte production and maturation
b. secondary tissue
location of immune cell interaction with pathogens
triggers a response
spleen (filters blood)
monitors blood for pathogens
destroys worn red blood cells
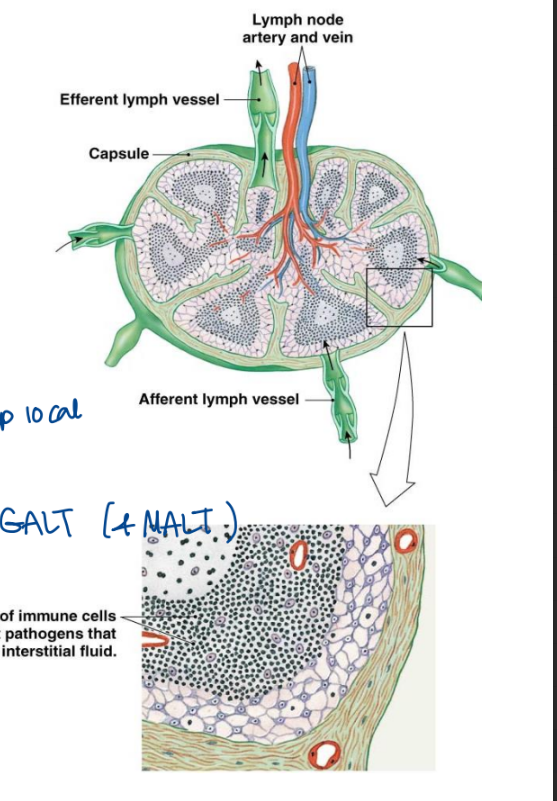
lymph nodes
form a component of the lymphatic system (blind ended, one way away from tissue)
large amount of filtered fluid enters each day
lymph nodes
filters fluid enters into lymphatic capillaries
passes though lymph nodes en route to the heart
lymphocytes are aggregated in the lymph node (a lot in there)
activate in response to antigens in lymphatic fluid
eliminate spread to other parts of the body (contain the spread, try to keep local)
tonsil and gut associated lymphoid tissue (GALT) forms aggregates of lymphatic tissue
function in immune system surveillance
leukocytes
form important components of both the innate and adaptive immune response
700 MBC/uL of blood
very large cells
two classes
granulocytes
agranulocytes
granulocytes
prominent of cytoplasmic granules (easy to see)
include
basophils
mast cells when in tissues (histamine containing)
eosinophils (parasitic defense)
neutrophils
most numerous leukocytes
**all three types are capable of degranulation (comes out and is functional)
arganulocytes
monocytes (like a baby, stay at home no job)
marcophages once mature in tissue (move out and have profession
lymphocytes
T lymphocytes (bone marrow and mature in thymus)
B lymphocytes (bone marrow and mature in bone marrow)
natural killer cells (kill cancer cells etc.)
dendritic (vaccinate you, bring foreign material to lymphocyte and tell them to develop memory)
three functional classifications of leukocytes
phagocytes (and vomit out destroyed fragments)
neutrophils
monocytes and macrophages
**engulf foreign material
cytotoxic cells
eosinophils (destroy parasites)
cytotoxic T cells (adaptive, release enzymes that poke holes)
destroy foreign and abnormal self cells
antigens presenting cells (APCs)
B cells (phagocytose but save destroyed fragments and put on display)
dendritic cells
macrophages and monocytes
present antigehns to other immune cells
basophils
contain histamine, heparin, cytokines
mast cells are their tissue counterpart
esoinophils
allergy and parasitic infections
attach to large parasites
secrete extracellular enzymes
neutrophils
short lived
highly phagocytic
most abundant
increase dramatically
produce many chemical mediators → important to talk to each other)
able to migrate into tissues during infection (because if changes that happen)
multiply quickly
always the highest → get higher when find something
macrophages
phagocytic
man the tissues → in alveoli
able to destroy larger materials than neutrophils
antigen presenting cells
lymphocytes
mainly concentrated in lymphoid tissues
important mediators of the adaptive immune response
include: T lymphocyte, B lymphocyte and NK
dendritic cells
located in skin and organs
contain long fingerlike projections
capture antigen and migrate to secondary lymphoid tissues to present antigen to lymphocytes
the innate immune system takes over when
takes over when physical and chemical defenses fail
able to either clear or contain the infection (keep it local, blood clotting)
non-specifically recognizes a broad range of materials as foreign
physical barriers
skin
mucos membrane
fluid flow
skin
the outer surface consists of dead cells and protective protein called keratin
the layers of the skin are frequent shed which removed microbes
skin is very dry which inhibits microbial growth
skin infections are more common on moist areas of the skin or in moist environments
the outer layer of the skin is an excellent defense and is rarely penetrated by microbes (difficult to break)
most infections occur under the skin once the skin has been broken although fungi can sometimes grown on the skin’s surface: eating dead skin cells (treat with topical cream)
some microbes are able to eat dead skin cells and oils that are secreted by the skin
if this happens body odor occurs
connected via tight junctions
mucous membranes
these membranes are involved in fluid exchange
they offer less protection than the skin
mucous membranes line ‘tracts’ such as the digestive, reproductive and respiratory tracts
they secrete mucous which is a glycoprotein that keeps the membrane from dying and cracking
the mucous traps microbes
cilia than moves the mucous containing microbes away
mucociliary escalator (bring up and stimulate cough to try and remove)
open to outside
always dirty
fluid flow
saliva, tears, urine, and vaginal secretions move microbes away/out of the body
purge
chemical barriers
acidity of body fluids and the skin
lysozyme
the normal microflora
acidity of fluids and skin
stomach: hydrochloric acid (parietal cells) creates a pH of 2
this low pH destroys many bacteria and toxins
skin: fatty acids and lactic acid create a pH of 3-5
these conditions prevent the growth of many microbes
lysozyme
an enzyme that degrades peptidoglycan (found in bacterial cell walls)
lysozyme is found in sweat, tears, salvia and nasal secretions
the normal microflora
this is acquired shortly after birth
it functions to prevent the growth of pathogens
this occurs because of competitive exclusion and microbial antagonism (meant to poison competitors)
compete for seats
phagocytosis
during infection monocytes and granulocytes migrate to the infected area through capillary pores
recruits more immune cells by producing cytokines
there are four main phases
chemotaxis
phagocytes are attracted to foreign particles, damaged cells etc.
have to be aware
get rid of foreign invaders
adherence
phagocyte attached to a foreign pathogen associated molecular pattern
attaches with pattern recognition receptor
needs to be recognized
needs to be on receptor on cell
ingestion
pseudopods extend and engulf the particle (forms endosome → phagosome)
encapsulated bacteria, cell fragments, foreign debris
the particle is trapped in the phagosome
digestion
digestive enzyme, oxidizing agents enter the phagosome due to fusion with lysosome
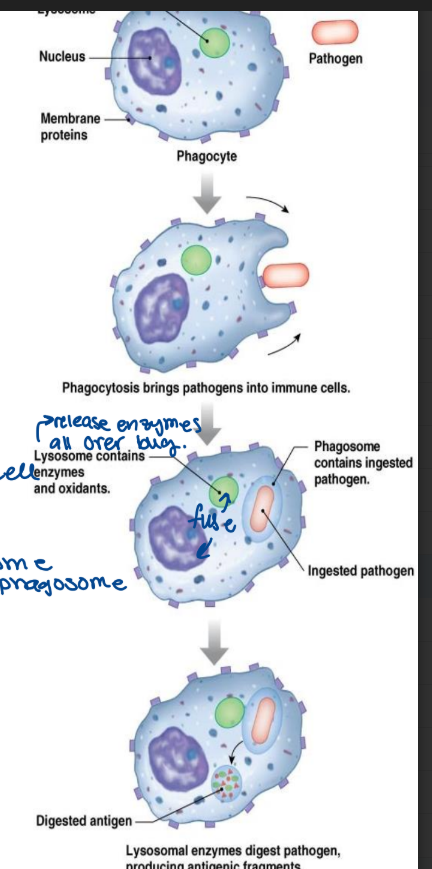
some pathogens/viral particles can be
opsonized increasing the efficiency of phagocytosis
easier to find
attach something to outside of foreign particle so immune cells can find it and destroy it
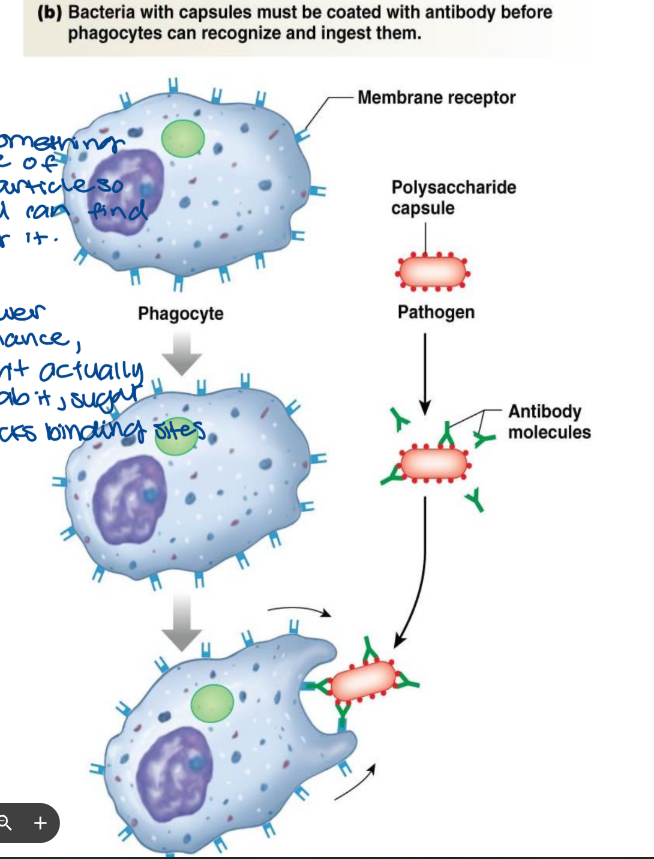
encapsulated bacteria cannot be phagocytosed by traditional means
requires antibodies from the adaptive immune response
lower chance, can’t actually grab it, sugar block binding sites
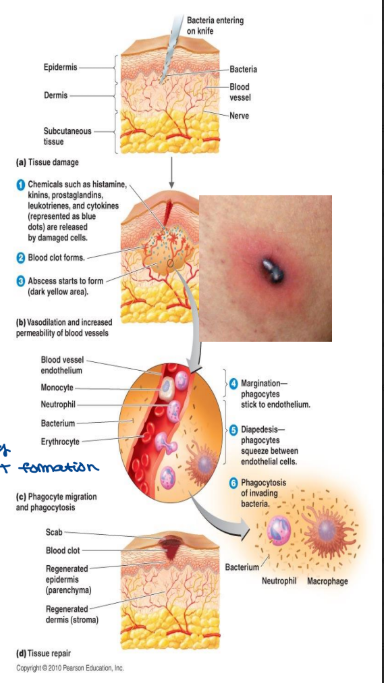
inflammation
sign and symptoms include:
pain, erythema (redness and vasodilation), heat, edema (increase vascular permeability), and loss of function
inflammation functions to destroy an bacteria/foreign material
it also acts to prevent the spreading of an injurious agents (maintain localization)
it repairs and replaces damage tissue (heal and put back epidermal layer, scar tissue)
proteins produced during the acute phase shortly after the injury occurs
increases plasma protein from the liver (liver responsible for protein synthesis of the liver)
C-reactive protein
opsonization (once of your own proteins coat the structure, easier for immune)
anti-proteases
protect tissue
minimize harm to innocent tissues in the background
levels of inflammatory protein should decrease as infection goes on
chronic inflammation
diseases such as rheumatoid arthritis see chronically elevated levels (increase inflammatory proteins but WBC count is normal because there is no infection)
stages of inflammation
tissue damage
vasodilation
the blood vessel dilates
more blood reaches the affected area
this allows white blood cells to access the area
brings nutrients for faster healing
this is causes redness, swelling (edema), increased temperature and pain
the pain is also due to tissue damage
this allows fibrinogen clot formation (soluble proteins present in plasma now)
this segregates the affected area
prevents the spread of infection → blood clotting)
fibrin → insoluble mesh to plug the leakage, start clot formation
phagocytosis
phagocytes destroy invading microbes
tissue repair
new cells are produced
fever
an increase in body temperature
fever is controlled by the hypothalamus (homeostasis) in the brain (muscle contractions produce heat)
it is triggered by toxins, LPS, and chemical produced by the immune system
all of these things reset the bodies thermostat
fever results in
muscle contraction (shivering)
faster phagocytosis (due to increased temperature)
slows the growth of heat limited microbes (off set their sweet spot)
ex. E. coli prefers to grow at 37°C, growth slows at 40°C
up to certain temperature, fever is a defense against disease
but a fever is defense above 43°C can cause death (we are plasma membrane)
NK cells
recognize virally infected cells
activate way faster than adaptive immune cells (turn on quickly)
cytotoxic T lymphocytes (counter-part)
force the infected cell to complete apoptosis (force to die)
able to attack cells displaying tumor antigens (hopefully squash it early)
produce interferons (antiviral chemical)
promote antiviral activity (cause healthy cells to up their antiviral defenses, hear first alarms)
IFNa and INFb: work on host cells to up their antiviral response
IFNy activated macrophages (phagocytic cells) and other immune cells
molecular defenses
histamine
interleukin I (IL-I)
bradykinin
the complement system
transferins
histamine
produced by mast cells and basophils
degranulation helps to initiate the inflammatory response (release or spit out histamine to ecf)
recruits more leukocytes
clean up mess
causes vasodilation (Increase flow, decrease P) and increased vascular permeability (systemic, decrease MAP - hard to keep organs)
promotes the escape of plasma proteins into the tissue
leads to edema and other symptoms of inflammation
involved in the anaphylactic response
mast cells stationed in mucosal membranes can degranulate in response to respiratory/digestive irritants (local entry points)
antihistamines block the effect of histamine
interleukin I (IL-I)
affects endothelium of capillary (increase gap size, becomes leakier, WBC can leave faster)
more hospitable to movement of WBCs and proteins
stimulates the production of acute phase protein production in the liver
works on the hypothalamus to induce fever
pyrogen
bradykinin
produced via a cascade reaction → have one thing lead to another to get this
increased vasodilation
increased pain
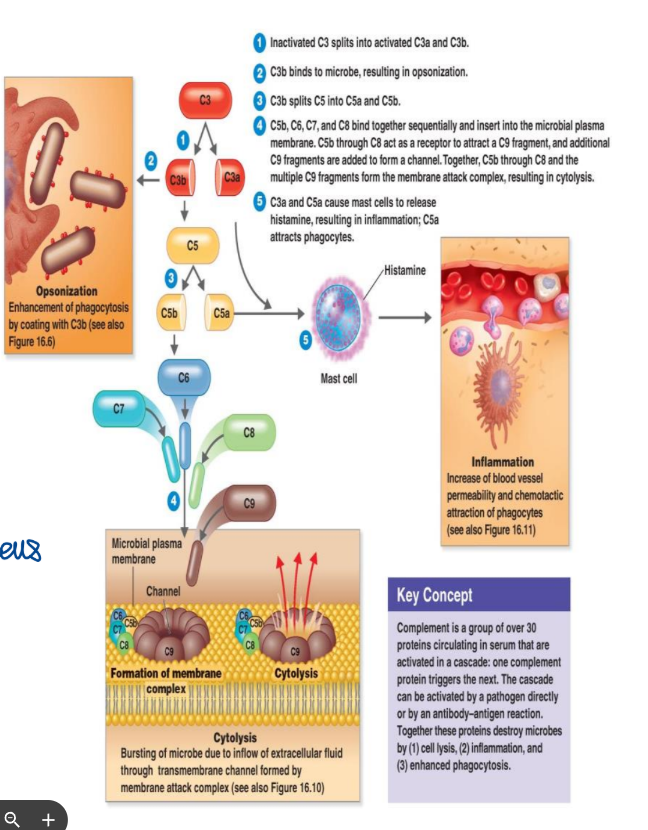
the complement system
composed of ∼30 proteins that circulate in the blood
they work together as a cascade
the action of one protein triggers the action of the next
complement can be triggered by surface molecules of invading microbes
ex. lipopolysaccharide (LPS)
factor on certain bacterial cells
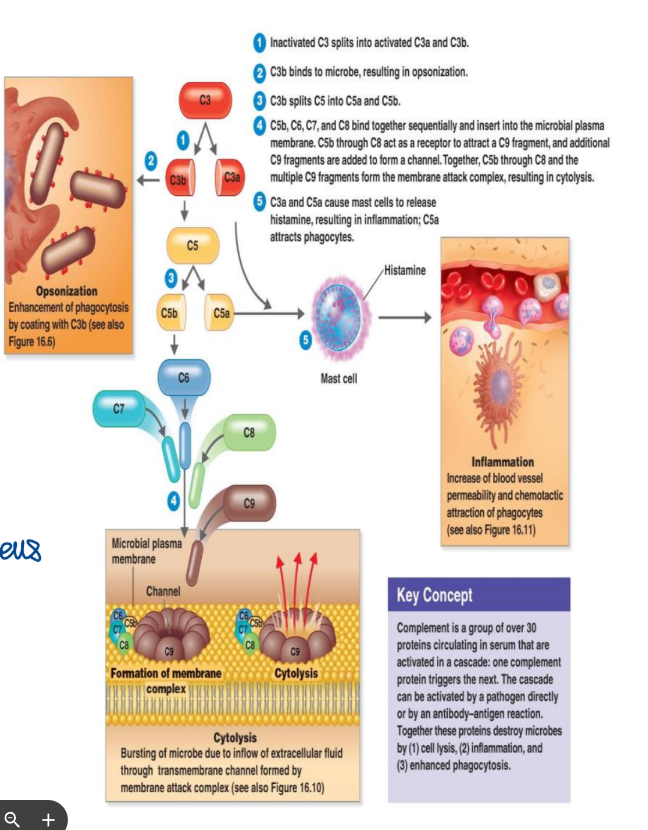
the result of the complement cascade
opsonization → coating
C proteins attach to microbes and act as a flag to attract phagocyte
this increases phagocytosis by 1000x
activated compliment protein stuck on bacteria → light on your head
enhance inflammation
increases blood vessel permeability
attracts phagocytes to the infection site
all of this is better when under c-system because it is trusted
cytolysis
formation of the membrane attack complex (MAC) form a pore and inset into wall, enter and exit
this pokes holes in the bacterial cell membrane ‘
split the cell because of this
cell is done
transferins
iron binding proteins in blood, milk, saliva, and tears (bacteria is unicellular and doesn’t have Hb for iron to bind to but it needs iron for ETC, they compete for iron)
binds and sequesters iron so that it cannot be used by bacteria
slows bacterial growth