The Endocrine System
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
61 Terms
Name the 2 components of the endocrine system
Endocrine glands
Hormone-secreting cells
Name and describe the 3 types of hormones
Endocrine - travels to a distant target cell via the blood stream
Paracrine - travels a short distance to act on a nearby target cell
Autocrine - acts on the secretory cell it was released by
Name and describe the 2 types of hormones based on chemistry
Water Soluble - peptide/protein hormones that dissolve in water and can freely travel in the blood, however cannot freely pass the lipid cell membranes.
Lipid Soluble - steroid hormones derived from cholesterol that cannot dissolve in water, therefore travel through the blood via a transport protein, however can freely pass through lipid cell membranes.
Name and describe the 2 types of receptors
Surface Receptors - on the surface of target cell membranes, typically activated by water soluble hormones that cannot diffuse through the cell membrane
Internal Receptors - within the nucleus or cytosol of the target cell, typically activated by lipid-soluble hormones that can diffuse through the cell membrane
Describe what occurs when lipid-soluble hormones bind to nuclear receptors.
The hormone can bind to DNA and alter gene expression, therefore altering patterns of protein synthesis and cell function, stimulating a physiological response.
Describe the location and function of the hypothalamus.
A region located in the center of the brain that links the endocrine and nervous systems together. Therefore regulating many functions via receiving and transmitting neural signals for the release of hormones.
Describe the location and structure of the pituitary gland.
An endocrine gland surrounded by the sphenoid bone and attached to the hypothalamus via the infundibulum. It is separated into 2 portions, the anterior and posterior pituitary glands.
Describe the role of the posterior pituitary gland.
Contains the axons of neurosecretory cells of the hypothalamus which releases oxytocin and ADH into the capillary plexus of the posterior pituitary. These hormones are then released into the bloodstream via the hypophysel vein.
Describe the 2 functions of oxytocin
The stretch of the cervix during childbirth transmits signals to the hypothalamus that triggers the release of oxytocin, increasing uterine wall contractions. Via a positive feedback loop, the cervix continues to stretch, transmitting further signals and releasing more oxytocin until the baby is born.
After childbirth oxytocin induces milk ejection from the mammary glands.
Describe the 3 functions of ADH
Stimulates water reabsorption from urine in the kidneys into the bloodstream, reducing water loss
Stimulates reduction of sweating by the sweat glands to reduce water loss
Stimulates vasoconstriction to increase blood pressure
Explain the regulation of ADH release
ADH release is regulated via osmoreceptors detecting solute concentration in the blood:
High activity of osmoreceptors occurs when there is high solute concentration, stimulating ADH release.
Low activity of osmoreceptors occurs when there is low solute concentration, reducing ADH release.
Describe the role of the anterior pituitary gland.
Contains the hypophyseal portal system in which neurosecretory cells of the hypothalamus secrete releasing or inhibiting hormones into the primary plexus within the median eminence. These hormones travel to the secondary plexus via the hypophyseal portal veins, stimulating specific anterior pituitary cells to release different hormones into the bloodstream via the hypophyseal vein.
Explain how hormones work when travelling throughout the body.
Hormones travel throughout the entire body via the bloodstream, however only act on certain organs and cells that contain their specific receptors.
Briefly explain how Insulin-like Growth Factor-1 (IGF-1) is produced.
Hypothalamus - growth releasing hormone (GRH)
Somatotrophs - growth hormone (GH)
Liver and bones - IGF-1
Briefly explain how cortisol and DHEA are produced.
Hypothalamus - corticotropin releasing hormone (CRH)
Corticotrophs - adrenocorticotropic hormone (ACTH)
Adrenal Glands - cortisol and DHEA
Briefly explain how testosterone, oestrogen and progesterone are produced.
Hypothalamus - gonadotropin releasing hormone (GnRH)
Gonadotrophs - follicle stimulating hormone (FSH) and leutinising hormone (LH)
Testes and Ovaries - testosterone, oestrogen and progesterone
Briefly explain how thyroid hormones are produced.
Hypothalamus - thyrotropin-releasing hormone (TRH)
Thyrotrophs - thyroid stimulating hormone (TSH)
Thyroid - T3 and T4
Briefly explain how milk is produced in the mammary glands.
Hypothalamus - prolactin releasing hormone (PRH)
Lactotrophs - prolactin (PRL)
Mammary glands - lactation
Name the hypothalamic inhibiting hormone for the releasing hormone of PRH
Dopamine
Explain the structure of growth hormone (GH).
Growth hormone is a water-soluble peptide hormone made up of 191 amino acids.
Explain in detail, the process of growth hormone release and regulation
Growth hormone releasing hormone (GHRH) is produced and secreted by neurosecretory cells of the hypothalamus into the primary plexus in the median eminence
GHRH travels to the secondary plexus in the anterior pituitary via hypophyseal portal veins, stimulating the release of growth hormone (GH) from somatotrophs
GH is released into the bloodstream via the hypophyseal vein, travelling to the liver and bones to stimulate release of insulin-like growth factor-1 (IGF-1)
Via negative feedback loops, GH and IGF-1 act on the hypothalamus to inhibit further release of GHRH and stimulate the release of somatostatin which inhibits GH release.
Additionally IGF-1 acts on the somatotrophs, inhibiting further release of GH.
Describe other factors that affect growth hormone (GH) release.
Onset of sleep stimulate surge of GH release while REM sleep reduces GH release
Stress and exercise stimulate GH release
Increase in glucose and free fatty acids reduces GH helease
Explain the roles of GH and IGF-1
Both GH and IGF-1 increase protein synthesis and cell division, therefore increasing bone and soft tissue growth
IGF-1 increases cartilage tissue growth
GH increases blood glucose levels
Explain what occurs when someone has a GH deficiency
Dwarfism occurs when there is damage to the pituitary gland, resulting in low GH production.
Explain what occurs in childhood and adulthood when there is excessive GH
In childhood, gigantism occurs when there is a benign tumour in the pituitary gland before epiphyseal plate closure. Therefore there is excessive production of GH that results in abnormally tall stature and rapid growth in children.
In adulthood, acremogaly occurs when there is a benign tumour tumour in the pituitary gland after epiphyseal plate closure. Therefore there is excessive production of GH that results in lengthening of the jaw, large hands and feet.
Describe the structure and location of the adrenal glands.
2 triangular shaped organs that sit superior to the kidneys. They are a few cm in size and compose of the adrenal cortex and adrenal medulla.
How do the adrenal glands receive blood supply?
Via 3 main arteries; superior, middle and inferior arteries.
Explain the location, structure and function of the adrenal medulla.
The inner portion of the adrenal glands that primarily consist of chromaffin cells which synthesize and release catecholamines.
Describe catecholamines
Catecholamines (80% adrenaline and 20% noradrenaline) are released by increased sympathetic NS activity. They bind to and activate alpha and beta catecholaminergic receptors throughout the body to increase metabolism, HR, BP, vasoconstriction and bronchiole dilation.
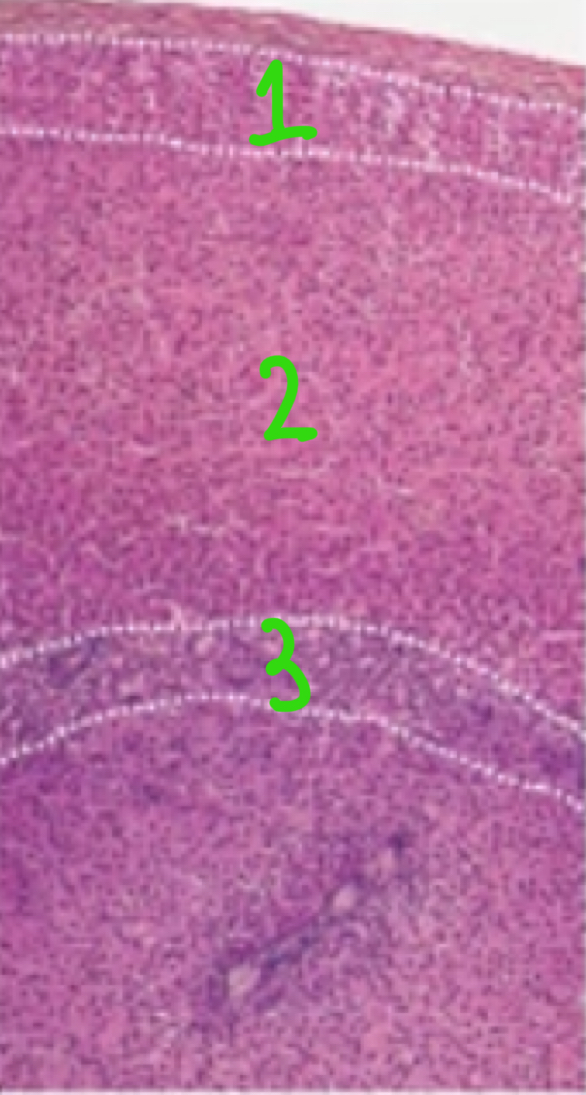
Identify and explain the 3 parts of the adrenal cortex.
Zona glomerulosa - outermost portion containing cells organised in spherical clusters and arched columns, secreting mineralocorticoids, eg. Aldosterone
Zona fasciculata - middle portion containing cells organised in long vertical columns, secreting glucocorticoids, eg. Cortisol
Zona reticularis - innermost portion containing cells organised in branches, secreting androgens, eg. DHEA
Name the 2 factors that increase aldosterone production.
Increased angiotensin ll (ANG ll) levels
Increase potassium ion levels in extracellular fluid
Explain in detail, how aldosterone increases blood volume and blood pressure.
Aldosterone is lipid-soluble and binds to intracellular receptors in the cytosol within cells of the nephron.
The aldosterone-receptor complex binds to DNA in the nucleus, influencing gene transcription.
This increases protein synthesis and the formation of sodium and potassium channels and transporters.
This increases sodium reabsorption into the blood from filtrate and increases potassium excretion into filtrate
Increasing sodium and therefore water retention, increases blood volume and therefore blood pressure.
Name other factors that affect cortisol release.
Time of day (morning = high, night = low)
Stress (short term = brief spike, long term = consistently high)
Low blood glucose
Inflammation
Intense exercise
Explain in detail the effects of cortisol and how they occurs
Cortisol is lipid soluble and binds to intracellular receptors within cytosol of all nucleated cells
The cortisol-receptor complex travels to the nucleus, binding to DNA and influencing gene transcription and therefore proteins synthesis and cell function.
Physiological responses include immunosuppression, include glucose production in the liver as well as increased protein and triglyceride breakdown for the formation of glucose.
Explain hypercortisolism/Cushing syndrome
Excessive amounts of cortisol produced in the body over a prolonged time period. Symptoms include weight gain in the upper body, red cheeks, fat pads between shoulders and thin skin, resulting in easy bruising and stretch marks.
Explain Addison’s disease
Cortisol and aldosterone deficiency over a prolonged time period. Symptoms include fatigue, weight loss, low BP, salt cravings, hypoglycaemia and increased skin pigmentation.
Explain the role of DHEA in producing sex hormones
DHEA is a precursor to oestrogen and testosterone. However only a small amount are produced in the adrenal glands, oestrogen is primarily produced in the ovaries and testosterone is primarily produced in the testes.
Explain the role of DHEA in puberty
DHEA plays a role in growth of axillary and pubic hair as well as prepubertal growth.
Explain the additional possible roles of DHEA
Aging - DHEA levels decrease with age
Immune System - DHEA counters some effects of cortisol
Cognition and Memory - acts on receptors of cognition-related brain areas
Explain the location of the thyroid in relation to the larynx and trachea
The thyroid is caudal (inferior and posterior) to the larynx
The thyroid is anterior to the trachea
Explain the blood supply to and from the thyroid
The thyroid is supplied by the superior and inferior thyroid arteries
The thyroid drains blood into the superior, middle and inferior thyroid veins
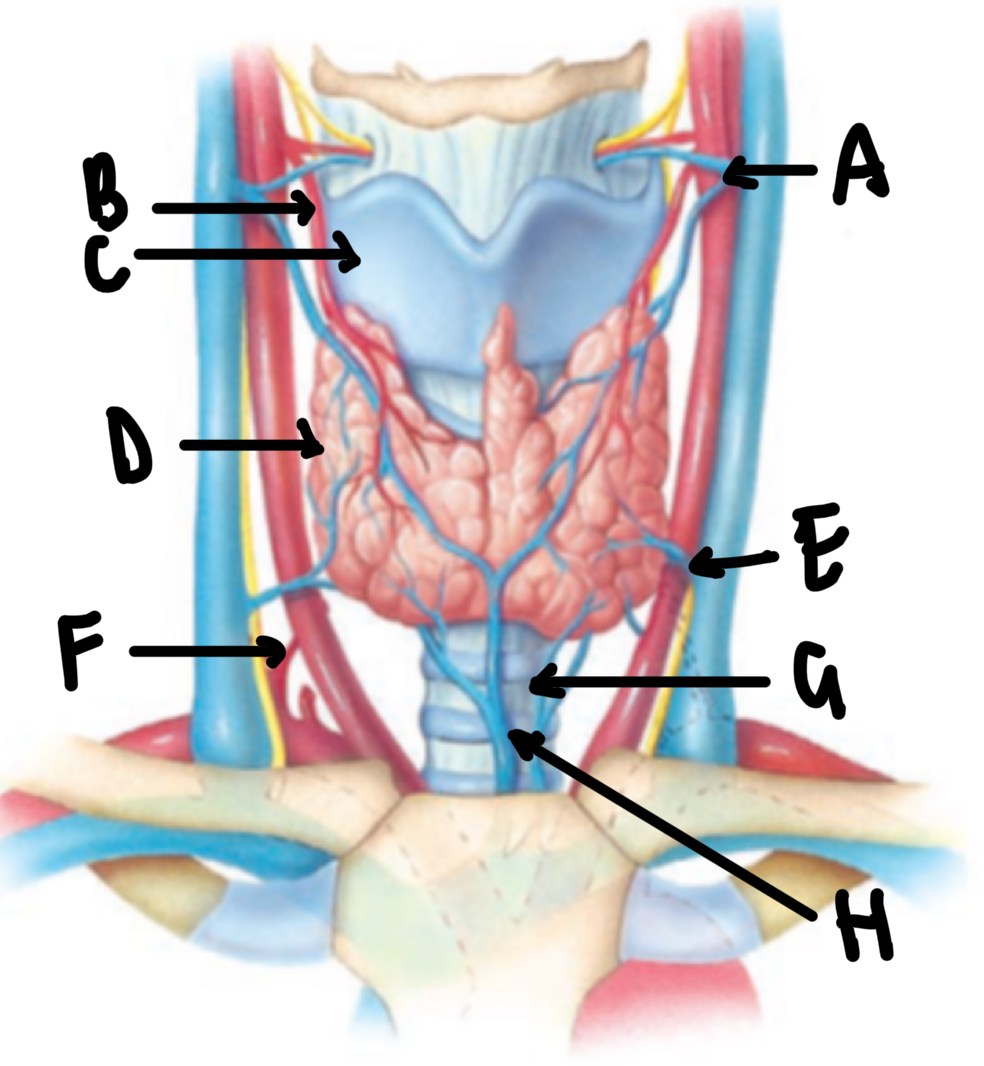
Name these structures in the neck
A - superior thyroid vein
B - superior thyroid artery
C - larynx
D - thyroid gland
E - middle thyroid vein
F - inferior thyroid artery
G - trachea
H - inferior thyroid vein
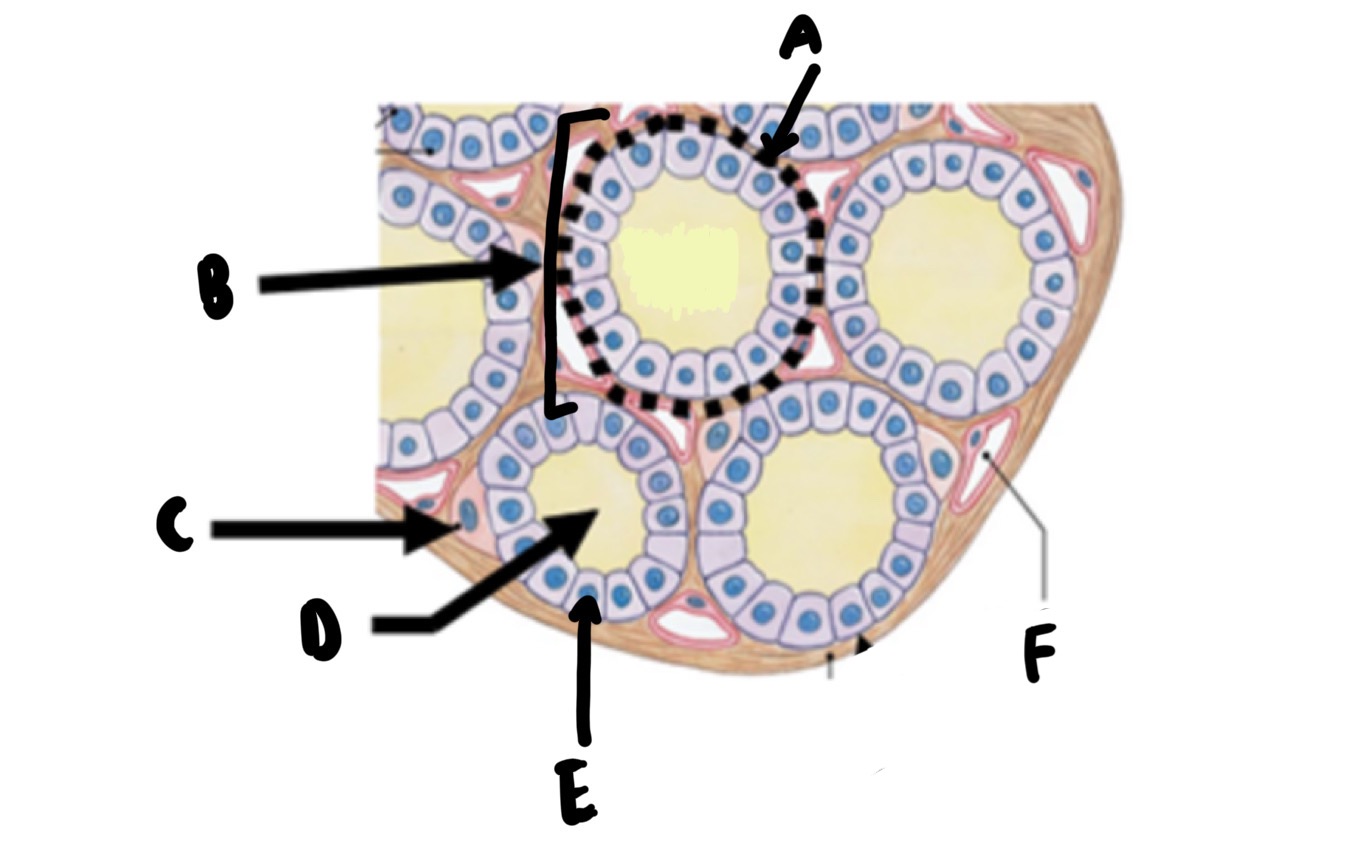
Name these structures of the thyroid
A - basement membrane
B - thyroid follicle
C - C/parafollicular cell
D - colloid
E - follicular cell
F - capillary
Explain the secretion of thyroid hormone
Thyroid hormone with attached thyroglobulin is transported into follicular cells via pinocytosis in vesicles
Vesicles merge with lysosomes, digesting thyroglobulin and releasing thyroid hormone
Thyroid hormone diffuses into the bloodstream and binds to thyroxine-binding globulin (TBG).
Explain the proportions of T4 and T3 produced
More T4 is produced than T3, however T3 is more potent and therefore T4 is converted to T3 by target tissues.
State the additional factors that affect thyroid hormone regulation
Cold temperature
Stress
Low blood glucose
Inflammation/infection
Pregnancy
Compare the effects of thyroid hormone on adults and children
In adults:
Increases base metabolic rate
Increases glucose production, HR and VP
Decreases blood cholesterol levels
In children:
Required for normal growth and development
Required for neural development
State the 3 ways the PTH increases blood calcium levels
Increases bone breakdown, releasing calcium and phosphate into the blood
Increases calcium reabsorption into the bloods and phosphate secretion into urine within the kidneys
Increases production of calcitriol from vitamin D. Calcitriol travels to GI tract and increases reasborption of dietary calcium
Explain the function of parafollicular cells
Synthesizes and secretes calcitonin which has opposing effects of PTH.
Explain the location and structure of the pancreas
Located within the abdominal cavity, within the posterior to the stomach. The pancreas is divided into 3 main regions:
Head - located within the curvature of the duodenum
Body - extends horizontally from the head to the left abdomen
Tail - narrow tapering from the body towards the spleen
Explain the 2 functions of the pancreas and correlating structure
98% of the pancreas is made of acini, clusters of exocrine cells that synthesize and secrete bicarbonate and digestive enzymes into the GI tract
2% of the pancreas is made of Islets of Langerhans, clusters of endocrine cells that synthesise hormones, regulating blood sugar
Name and explain the 4 types of cells within the Islets of Langerhans
Alpha Cells - makes up 17%, produces glucagon
Beta Cells - makes up 75%, produces insulin and amylin
Delta Cells - makes up 5%, produces somatostatin
F Cells - makes up 3%, produces pancreatic polypeptides
Explain the structure of insulin and glucagon
Insulin - peptide containing 51 amino acids into 2 strands held together by disulphide bridges
Glucagon - peptide containing 29 amino acids
Explain how insulin reduced blood glucose levels
Increases glycogenesis, uptake and storage of glucose into the liver and other body cells as glycogen
Increases glycolysis, breakdown of glucose for energy
Explain how glucagon increase blood glucose levels
Increases glycogenolysis, breakdown of glycogen in the liver and other body cells into glucose, released into the bloodstream
Increases glucogenesis, production of glucose from lactic acid and amino acids
Increases ketogenesis, production of ketone bodies from fatty acids as an energy source when there is insufficient glucose
Explain diabetes and symptoms
Chronically raised blood glucose levels. Symptoms include:
Increased urination
Increased thirst
Increased hunger
Name the diseases that diabetes increases the risk of
Cardiovascular diseases
Kidney diseases
Eye disease
Neurological dysfunction
Explain Type l Diabetes
An autoimmune disease that destroys pancreatic beta cells and therefore no insulin can be produced.
State the population with the largest contribution to Type l Diabetes
95% of people with Type l Diabetes are children
Explain ketoacidosis and its relation to Type l Diabetes
For those with Type l Diabetes, there is not enough insulin to stimulate glycogenesis and glucose is not used as energy. Therefore the body undergoes ketogenesis, converting fatty acids to ketones and relying on these ketones for energy. However this results in ketoacidosis, in which high levels of ketones in the blood dangerously increases blood acidity.
Explain Type ll Diabetes
Chronically raised insulin levels due to the body’s resistance to the effects of insulin or the underproduction of insulin.