Biology 2.4
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
why do all cell have specific molecules on their surface?
They make the cell identifiable: they enable the immune system to identify pathogens, cells from other organisms, abnormal cells and toxins
what is an antigen?
A molecule (usually glycoprotein) that triggers an immune response in the body, especially the production of antibodies.
which types of antigens do not trigger an immune response?
self antigens
what type of recognition do antigens allow for?
cell to cell recognition
what do antigens enable the immune system to do?
detect pathogens, abnormal cells, toxins and other foreign cells
what is antigen variability?
The antigens present on their surface change frequently due to genetic mutations
what is the problem when dealing with pathogens that have antigen variability?
memory cells from a previous infection no longer recognise the new antigens, causing re infection and reduced vaccine effectiveness
What is phagocytosis?
the process by which a phagocyte engulfs a particles (pathogen) and digests it
which immune response is phagocytosis part of?
non-specific
what are phagocytes
white blood cells
Phagocytosis of pathogens
cytokines released by pathogens attract phagocytes
phagocytes move towards the site of infection and engulf the pathogens enclosing them in a phagosome
phagosome fuses with a lysosome which contains hydrolytic enzymes such as lysozymes to form a phagolysosome
Pathogens are destroyed
antigens get displayed on the phagocytes cell surface membrane to trigger the specific immune response
what are the two types of lymphocytes?
B lymphocyte and T lymphocyte
how can you identify lymphocytes?
they are smaller than phagocytes and have a large nucleus
what is the cellular immune response?
a cell mediated immunity where the T cells are activated by bonding to complementary antigens on an antigen presenting cell, leading to the clonal expansion of T cells
How are T cells activated?
When their receptors bind to complementary antigens on APC’s
what happens once a T cell is activated?
It divides by mitosis and produces clones of itself.
what do the cloned t lymphocytes differentiate into?
Helper T cells, cytotoxic T cells and memory T cells
what happens during clonal selection of T cells?
- APC's present antigens on their cell surface membrane
- a specific T cell binds to the complementary antigen
- T cell is then activated and divides by clonal expansion
what happens during clonal expansion in T cells?
The T cell rapidly divides to form many clones, which differentiate into T helper cells, cytotoxic T cells and memory T cells
what is the role of APC's in the cell mediated response?
They activate T cells by presenting antigens which the T cells are complementary to
What is an APC and how does it form?
An APC (antigen presenting cell) is a phagocyte which has engulfed a pathogen, processed its antigens and presented them on its cell surface membrane
What do helper T cells do?
They release cytokines which:
- activate B cells
- increase the rate of phagocytosis as they attract phagocytes
- promote the formation of memory B cells
- stimulate cytotoxic t cells
What to cytotoxic T cells do?
secrete toxic substances (perforins) into the infected cells which destroys them
What is the humoural response (steps)?
- B cells engulf the pathogens which have antigens their antibodies are complementary to
- they then process its antigens and display them on their cell surface membrane becoming an APC
- A helper T cell with complementary receptors binds to the antigen on the B cell becoming activated
- The activated helper T cell releases cytokines causing the maturation of the B cell stimulating it to divide by clonal expansion to produce many clones which differentiate into plasma or memory B cells
- Plasma B cells secrete antibodies
- Memory B cells remain in the body for a long time
what happens during clonal selection of B cells?
B cell binds to the antigens of a pathogen which are complementary to its receptors and engulfs it, processing the pathogenic antigens and displaying them on its cell surface membrane
helper T cells binds to the antigens on the cell surface membrane of the B cell which are complementary to its receptors, becoming activated and releasing cytokines
This stimulates the maturation of B cells, allowing them to divide by clonal expansion
what happens in the if the same antigen is encountered again?
Memory cells rapidly divide and form plasma cells which triggers a faster and stronger secondary immune response
What is clonal selection?
Clonal selection is the process by which specific B or T lymphocytes are activated when their receptors bind to a complementary antigen
What is clonal expansion?
the process by which activated lymphocytes divide by mitosis to produce a large number of identical clones
What are plasma cells?
short lived cells which secrete antibodies
what are the 6 points for a 6 marker on the humoral response?
- B cell encounters pathogen with antigens complementary to its antibodies
- B cell engulfs pathogen and displays its antigens on its cell surface membrane
- helper T cell with receptors complementary to the antigens on the B cell are activated
- activated helper T cell releases cytokines which stimulates the B cell to mature and undergo clonal expansion to differentiate into plasma or memory B cells
- plasma B cells secrete antibodies
- memory B cells remain in the blood for a long time
what makes up the specific immune response?
the cell mediated response and the humoural response
where do specific immune responses occur?
only in mammals
Steps of the cell mediated response
- phagocyte engulfs pathogens and presents the antigens on its cell surface membrane
- helper t cell with complementary receptors binds to the antigens
- this activates the t cell to divide rapidly by clonal expansion
- these clones either become t helper cells, cytotoxic t cells or memory t cells
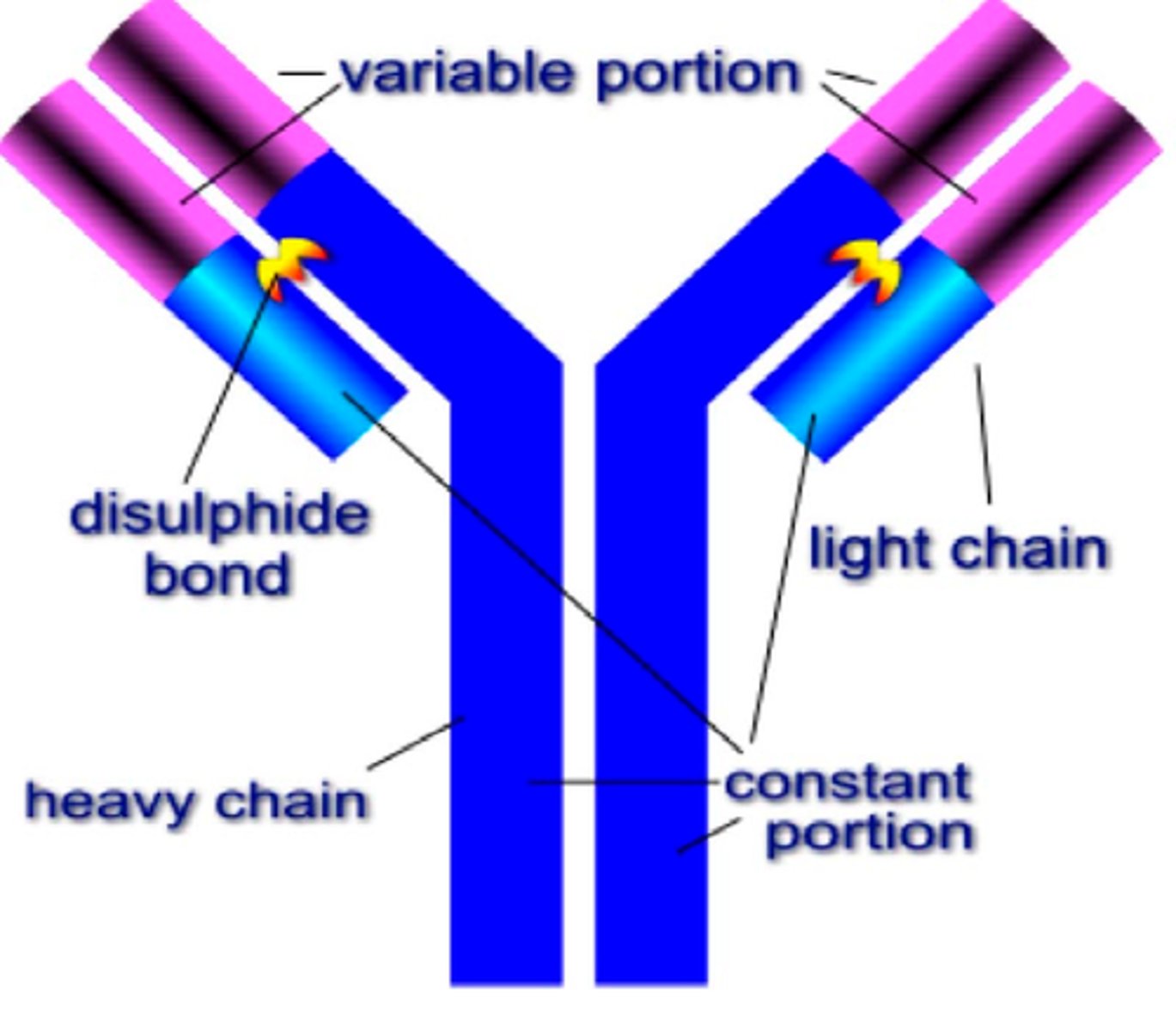
What is an antibody?
globular glycoproteins called immunoglobulins
what is the structure of an antibody?
they have a quaternary structure with two heavy (long) polypeptides and two light (short) polypeptides. the heavy and light chains are bonded by disulfide bridges. there are two regions, the constant and variable regions. the constant region is the same within any antibody class and the variable region is when the antibody attaches to the antigen to form an antigen - antibody complex.
there is a hinge region where the two heavy chains are joined which provides flexibility
what does the formation of an antigen antibody complex lead to?
the destruction of the antigen - the binding of antibodies to antigens acts as a marker to attract phagocytes which engulf the pathogens
How do antibodies lead to agglutination?
Each antibody has two antigen binding sites
why is the primary immune response relatively slow?
time taken for:
- pathogen to be detected and undergo phagocytosis
- finding lymphocytes with complementary receptors
- mitosis to occur
- antibody production to begin
what do vaccines do?
introduce pathogenic antigens into the body, triggering a specific immune response which results in the release of antibodies by plasma cells
what is inside a vaccine (usually)?
weakened forms of the pathogen, antigens or the genetic material which codes for the antigens
what are the types of immunity?
active, passive, natural, artificial
what type of immunity to vaccines create?
active immunity
What is active immunity?
When your immune system makes its own antibodies after being stimulated by an antigen
What is passive immunity?
short term immunity using antibodies produced outside the body - no immune response
what is natural passive immunity?
no exposure to pathogen - antibodies are received from another organism
what is artificial passive immunity?
When you become immune after being injected with antibodies from someone else (no secondary immunity)
Structure of HIV virus
RNA, reverse transcriptase enzyme, protein coat, lipid envelope and attachment proteins
what do reverse transcriptase enzymes do?
convert RNA to DNA
Where does the lipid envelope in HIV come from?
the cell membrane of the helper T cells
Replication of HIV
enters the blood stream, infects helper T cells and uses their cell machinery to replicate
1. viral RNA enters cell
2. viral reverse transcriptase enzyme produces a DNA copy of viral RNA
3. DNA copy is inserted into a chromosome
4. each time the cell replicates, the viral DNA is copied
5. HIV proteins are produced from viral DNA
6. proteins are used to build new HIV particles
7. thousands of HIV particles are released killing the helper t cell
what happens when the number of helper t cells decreases?
b cells are no longer activated so no antibodies are produced, reducing the bodies ability to fight off infections eventually leading to aids
when are you said to have aids?
when you can no longer produce antibodies
why are antibiotics ineffective against viruses?
Viruses are intracellular and antibiotics can’t enter host cells
what are monoclonal antibodies?
Antibodies produced from a single group of genetically identical B-cells
what are monoclonal antibodies used for clinically?
- pregnancy tests
- diagnosing HIV
- detecting cancer cells or the presence of pathogens
what is direct therapy with monoclonal antibodies?
monoclonal antibodies which are specific to antigens can be used to target and destroy certain cells as a part of the immune response
what is indirect therapy with monoclonal antibodies?
drugs are attached to monoclonal antibodies and the antibody is used to direct the drug towards the cell displaying a certain antigen
what are key factors to make a successful vaccination project?
- cost of vaccine
- severity of side effects
- ease of production, transportation and administration
- number of people who need to be vaccinated for herd immunity
What is the indirect ELISA test used for?
it is used to identify HIV
How does the indirect ELISA test work?
1. Wells coated with antigen
2. Sample added
3. If patient has HAD disease, specific antibodies will be present and will bind to antigen
4. Enzyme-linked antibodies specific to disease antigens are added next and will bind on top
5. These are tagged with coloured dye and will show presence