Chapter 16 - Disorders of Brain Function
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
20 Terms

A nurse on a neurology unit is assessing a female brain-injured client. The client is
unresponsive to speech, and her pupils are dilated and do not react to light. She is
breathing regularly, but her respiratory rate is 45 breaths/minute. In response to a
noxious stimulus, her arms and legs extend rigidly. What is her level of impairment?
A) Delirium
B) Coma
C) Brain death
D) Vegetative state
B) Coma
The continuum of loss of consciousness is marked by the degree of client's responsiveness to stimuli, in addition to the preservation of brain stem reflexes. Since this client still exhibits a pain response (the extended arms and legs indicate decerebrate posturing), even though her pupils are not responsive to light, she has sustained sufficient brain function that she fails to qualify as being brain dead or in a vegetative state.

Following a motor vehicle accident 3 months prior, a 20-year-old female who has been
in a coma since her accident has now had her condition declared a persistent vegetative
state. How can her care providers most accurately explain an aspect of her situation to
her parents?
A) "Your daughter has lost all her cognitive functions as well as all her basic reflexes."
B) "Though she still goes through a cycle of sleeping and waking, her condition is unlikely to change."
C) "If you or the care team notices any spontaneous eye opening, then we will change our treatment plan."
D) "Your daughter's condition is an unfortunate combination with total loss of consciousness but continuation of all other normal brain functions."
B) "Though she still goes through a cycle of sleeping and waking, her condition is
unlikely to change."
Feedback: A continuation of the sleep–wake cycle can exist in a persistent vegetative state. Reflexes often remain, as does spontaneous eye opening. Aspects of brain function beyond those governing consciousness are affected.
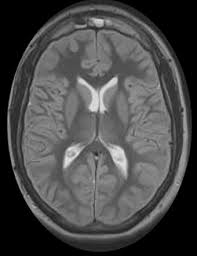
Which of the following individuals would most likely experience global ischemia to his
or her brain?
A) A male client who has just had an ischemic stroke confirmed by CT of his head
B) A woman who has been admitted to the emergency department with a suspected intracranial bleed
C) A man who has entered cardiogenic shock following a severe myocardial infarction
D) A woman who is being brought to hospital by ambulance following suspected carbon monoxide poisoning related to a faulty portable heater
C) A man who has entered cardiogenic shock following a severe myocardial infarction
Feedback: Global ischemia is associated with a cessation of blood flow to the entire brain, as often occurs during cardiac arrest or myocardial infarction. Ischemic stroke and intracranial bleeding are likely to cause focal ischemia; carbon monoxide toxicity is associated with hypoxia.

Which of the following diagnostic findings is likely to result in the most serious brain insult?
A) Mean arterial pressure (MAP) that equals intracranial pressure (ICP)
B) Moderate decrease in brain tissue volume secondary to a brain tumor removal
C) Increased ICP accompanied by hyperventilation
D) High intracellular concentration of glutamate
A) Mean arterial pressure (MAP) that equals intracranial pressure (ICP)
Feedback: When the pressure in the cranial cavity approaches or exceeds the MAP, tissue
perfusion becomes inadequate; cellular hypoxia results; and neuronal death may occur.
Displacement of CSF and blood can partially compensate for decreased brain tissue
volume. Hyperventilation partially mitigates, rather than exacerbates, increase in ICP.
Glutamate is normally in far higher concentrations intracellularly than extracellularly.

Following a car accident of a male teenager who did not have his seatbelt on, he arrived
in the emergency department with a traumatic brain injury. He has severe cerebral
edema following emergent craniotomy. Throughout the night, the nurse has been
monitoring and reporting changes in his assessment. Which of the following
assessments correspond to a supratentorial herniation that has progressed to include
midbrain involvement? Select all that apply.
A) Clouding of consciousness
B) Decorticate posturing with painful stimulation
C) Pupils fixed at approximately 5 mm in diameter
D) Respiration rate of 40 breaths/minute
E) Decerebrate posturing following painful stimulation of the sternum
C) Pupils fixed at approximately 5 mm in diameter
D) Respiration rate of 40 breaths/minute
E) Decerebrate posturing following painful stimulation of the sternum

A patient in the intensive care unit who has a brain tumor has experienced a sharp
decline. The care team suspects that water and protein have crossed the blood-brain
barrier and been transferred from the vascular space into the client's interstitial space.
Which of the following diagnoses best captures this pathophysiology?
A) Focal hypoxia
B) Cytotoxic edema
C) Hydrocephalus
D) Vasogenic edema
D) Vasogenic edema
Feedback: Vasogenic edema occurs with conditions that impair the function of the blood–brain
barrier and allow transfer of water and protein from the vascular into the interstitial
space. It occurs in conditions such as tumors, prolonged ischemia, hemorrhage, brain
injury, and infectious processes. Focal hypoxia is associated with localized delivery of
blood with inadequate oxygen, and cytotoxic edema is an absolute increase in
intracellular fluid. Hydrocephalus is an abnormal increase in CSF volume in any part or
all of the ventricular system.

A baseball player was hit in the head with a bat during practice. In the emergency
department, the physician tells the family that he has a "coup" injury. How will the
nurse explain this to the family so they can understand?
A) "It's like squeezing an orange so tight that the juice runs out of the top."
B) "Your son has a huge laceration inside his brain where the bat hit his skull."
C) "Your son has a contusion of the brain at the site where the bat hit his head."
D) "When the bat hit his head, his neck jerked backward causing injury to the spine."
C) "Your son has a contusion of the brain at the site where the bat hit his head."
Feedback :A direct contusion of the brain at the site of external force is referred to as a coup injury. Contrecoup injury (answer choice D) is the rebound injury on the opposite side of the
brain. Answer choice B relates to lacerations that are usually not caused by a direct blow
to the head. However, depending on how hard the head was hit with a bat, a hematoma
could form as the brain strikes the rough surface of the cranial vault.

Following an injury where a child hit his head from a fall, the CT scan reveals a
contusion that the doctor classifies as a moderate brain injury. Which of the following
manifestations will the nurse more than likely assess on this child that support this
diagnosis? Select all that apply.
A) Coma with total paralysis
B) Periods of unconsciousness
C) Aphasia at times
D) Nuchal rigidity
E) Weakness or slight paralysis affecting one side of the body
B) Periods of unconsciousness
C) Aphasia at times
E) Weakness or slight paralysis affecting one side of the body

Following a collision while mountain biking, the diagnostic workup of a 22-year-old
male has indicated the presence of an acute subdural hematoma. Which of the following
pathophysiological processes most likely underlies his diagnosis?
A) Blood has accumulated between the man's dura and subarachnoid space.
B) Vessels have burst between the client's skull and his dura.
C) A traumatic lesion in the frontal or temporal lobe has resulted in increased ICP.
D) Blood has displaced CSF in the ventricles as a consequence of his coup-contrecoup injury.
A) Blood has accumulated between the man's dura and subarachnoid space.
Feedback: A subdural hematoma develops in the area between the dura and the arachnoid space, while epidural hematomas exist between the skull and dura. Intracerebral hematomas
are located most often in the frontal or temporal lobe, and the ventricles are not directly
involved in a subdural hematoma.
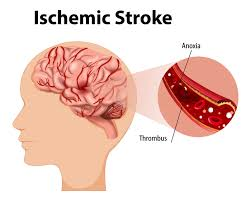
A 20-year-old has been admitted to a rehabilitation center after hospital treatment for an
ischemic stroke. Which of the following aspects of the client's history would be
considered to have contributed to his stroke? Select all that apply. The client
A) is an African American male.
B) takes iron supplements for the treatment of chronic anemia.
C) blood pressure has historically been in the range of 150s/90s.
D) was diagnosed with type 2 diabetes 8 years ago.
E) takes corticosteroids for the treatment of rheumatoid arthritis.
A) is an African American male.
C) blood pressure has historically been in the range of 150s/90s.
D) was diagnosed with type 2 diabetes 8 years ago.
Feedback: African American race, male gender, hypertension, and diabetes are all
well-documented risk factors for stroke. Anemia, autoimmune disorders like rheumatoid
arthritis, and the use of corticosteroids are not noted to predispose to stroke.

A nurse at a long-term care facility provides care for an 85-year-old man who has had
recent transient ischemic attacks (TIAs). Which of the following statements best
identifies future complications associated with TIAs? TIAs
A) are an accumulation of small deficits that may eventually equal the effects of a full CVA.
B) are a relatively benign sign that necessitates monitoring but not treatment.
C) resolve rapidly but may place the client at an increased risk for stroke.
D) are caused by small bleeds that can be a warning sign of an impending stroke.
C) resolve rapidly but may place the client at an increased risk for stroke.
Feedback: TIAs can be considered a warning sign for future strokes. They are not hemorrhagic in nature, and their effects are not normally cumulative. They may require treatment medically or surgically.

Which of the following clients' signs and symptoms would allow a clinician to be most
justified in ruling out stroke as a cause? An adult
A) has had a gradual onset of weakness, headache, and visual disturbances over the last 2 days.
B) has experienced a sudden loss of balance and slurred speech.
C) has vomited and complained of a severe headache.
D) states that his left arm and leg are numb, and gait is consequently unsteady.
A) has had a gradual onset of weakness, headache, and visual disturbances over the last 2 days.
Feedback: A cardinal trait of the manifestations of stroke is that the onset is sudden, and a gradual onset of symptoms over 2 days would suggest an alternative etiology. Ataxia, slurred
speech, and unilateral numbness are associated with stroke, with sudden vomiting and
headache being particularly indicative of a hemorrhagic CVA.

The nurse knows that which of the following treatment plans listed below is most likely
to be prescribed after a computed tomography (CT) scan of the head reveals a new-onset
aneurysmal subarachnoid hemorrhage?
A) Stat administration of tissue plasminogen activator (tPA)
B) Administration of a diuretic such as mannitol to reduce cerebral edema and ICP
C) Monitoring in the ICU for signs and symptoms of cerebral insult
D) Craniotomy and clipping of the affected vessel
D) Craniotomy and clipping of the affected vessel
Feedback: Surgery for treatment of aneurysmal subarachnoid hemorrhage involves craniotomy and inserting a specially designed silver clip that is tightened around the neck of the aneurysm. Administration of tPA would exacerbate bleeding, and a diuretic would not address the issue of bleeding. Monitoring alone would be an insufficient response given the severity of the problem.

A college student has been experiencing frequent headaches that he describes as throbbing and complaining of difficulty concentrating while studying. Upon cerebral angiography, he is found to have an arteriovenous malformation. Which of the following pathophysiological concepts is likely responsible for his symptoms?
A) Increased tissue perfusion at the site of the malformation
B) Hydrocephalus and protein in the cerebral spinal fluid
C) High pressure and local hemorrhage of the venous system
D) Localized ischemia with areas of necrosis noted on CT angiography
C) High pressure and local hemorrhage of the venous system
Feedback: In arteriovenous malformations, a tangle of arteries and veins acts as a bypass between the cerebral arterial and venous circulation, in place of the normal capillary bed. However, the capillaries are necessary to attenuate the high arterial blood pressure before this volume drains to the venous system. As a result, the venous channels experience high pressure, making them to hemorrhage and rupture more likely; the lack of perfusion of surrounding tissue causes neurologic deficits such as learning disorders. Headaches are severe, and people with the disorder may describe them as throbbing (synchronous with their heartbeat). Increased tissue perfusion means that more oxygenated blood is brought to the area, which is not the case. The elevated arterial and venous pressures divert blood away from the surrounding tissue, impairing tissue perfusion. Answer choice B is incorrect since arteriovenous malformation is associated with blood vessels and not the fluid within the ventricles of the brain. Answer choice D is incorrect in that there is blood flow to the area. Ischemia is associated with decreased arterial flow resulting in death to brain tissue.

A 9-year-old boy has been brought to the emergency department by his father who is
concerned by his son's recent fever, stiff neck, pain, and nausea. Examination reveals a
petechial rash. Which of the following assessment questions by the emergency room
physician is most appropriate?
A) "Is your son currently taking any medications?"
B) "Has your son had any sinus or ear infections in the last little while?"
C) "Does your son have a history of cancer?"
D) "Was your son born with any problems that affect his bone marrow or blood?"
B) "Has your son had any sinus or ear infections in the last little while?"
Feedback: The most common symptoms of acute bacterial meningitis are fever and chills; headache; stiff neck; back, abdominal, and extremity pains; and nausea and vomiting. Risk factors associated with contracting meningitis include otitis media and sinusitis or mastoiditis. Particular medications, a history of neoplasm, and hematopoietic problems would be unlikely to relate directly to his symptoms of meningitis.

A teenager, exposed to West Nile virus a few weeks ago while camping with friends, is
admitted with headache, fever, and nuchal rigidity. The teenager is also displaying some
lethargy and disorientation. The nurse knows which of the following medical diagnoses
listed below may be associated with these clinical manifestations?
A) Rocky Mountain spotted fever
B) Lyme disease
C) Encephalitis
D) Spinal infection
C) Encephalitis
Feedback: Encephalitis represents a generalized infection of the parenchyma of the brain or spinal cord. A virus, such as West Nile virus, usually causes encephalitis although it may be caused by bacteria, fungi, and other organisms. Encephalitis is characterized by fever, headache, and nuchal rigidity. However, more often, people also experience neurologic disturbances, such as lethargy, disorientation, seizures, focal paralysis, delirium, and coma. Rocky Mountain spotted fever (answer choice A) is a tick-borne disease caused by the bacterium Rickettsia rickettsii and usually begins with a sudden onset of fever and headache. A rash may occur 2 to 5 days after fever onset. Lyme disease (answer choice B) is also a tick-borne disease. Typical symptoms include fever, headache, fatigue, and a characteristic skin rash called erythema migrans. As the disease progresses, the patient develops bouts of severe joint pain and swelling of the joint. Neurological problems may occur for weeks, months, or even years after the infection and may include inflammation of the membranes surrounding the brain (meningitis). Spinal infections (answer choice D) can be thought of as a spectrum of diseases comprising spondylitis, discitis, spondylodiscitis, pyogenic facet arthropathy, and meningitis.

A 20-year-old has been diagnosed with an astrocytic brain tumor located in the brain
stem. Which of the following statements by the oncologist treating the client is most
accurate?
A) "Your prognosis will depend on whether we can surgically resect your tumor."
B) "Our treatment plan will depend on whether your tumor is malignant or benign."
C) "This is likely a result of a combination of heredity and lifestyle."
D) "The major risk that you face is metastases to your lungs, liver, or bones."
A) "Your prognosis will depend on whether we can surgically resect your tumor."
Feedback: The prognosis of people with pilocytic astrocytomas is influenced primarily by their
location. The prognosis is usually better for people with surgically resectable tumors,
such as those located in the cerebellar cortex, than for people with less accessible
tumors, such as those involving the hypothalamus or brain stem. Because of infiltration
of brain tissue that prevents total resection, surgery rarely cures brain tumors. The
binary of malignant and benign is not used to characterize brain tumors, and the etiology
and substantive risk factors are largely unknown. Brain tumors rarely metastasize
outside the CNS.
A brain tumor causing clinical manifestations of headache, nausea, projectile vomiting,
and mental changes is likely located in which parts of the brain? Select all that apply.
A) Intra-axially
B) Extra-axially
C) Brain stem
D) Temporal lobe
E) Frontal lobe
A) Intra-axially
B) Extra-axially
E) Frontal lobe
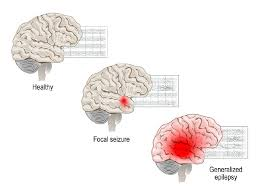
Which of the following clients may be experiencing a sensory focal seizure that has sent
an abnormal cortical discharge to the autonomic nervous system (ANS)?
A) A 44-year old patient complaining of constant movement and pain in the legs that gets worse when he tries to sleep
B) An 85-year-old patient experiencing drooping of the right side of the face and numbness in the right arm and leg
C) A 56-year-old complaining of tingling sensations and has both an elevated pulse and BP
D) A 22-year-old complaining of a stiff neck and achiness, along with some nausea and vomiting
C) A 56-year-old complaining of tingling sensations and has both an elevated pulse and BP
Feedback: Sensory symptoms correlate with the location of seizure activity on the contralateral side of the brain and may involve somatic sensory disturbance (tingling). With abnormal cortical discharge stimulating ANS, tachycardia, diaphoresis, hypo- or hypertension, or papillary changes may be evident. Distracter A is associated with restless legs syndrome (RLS). Distracter B is associated with stroke (CVA). Distracter D is associated with meningitis.
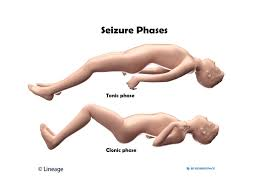
A 26-year-old female is resting after a one-minute episode during which she lost
consciousness while her muscles contracted and extremities extended. This was
followed by rhythmic contraction and relaxation of her extremities. On regaining
consciousness, she found herself to have been incontinent of urine. What has the woman
most likely experienced?
A) A myoclonic seizure
B) A tonic-clonic seizure
C) An absence seizure
D) A complex partial seizure
B) A tonic-clonic seizure
Feedback:
A tonic–clonic seizure often begins with tonic contraction of the muscles with extension
of the extremities and immediate loss of consciousness. Incontinence of the bladder and
bowel is common. Cyanosis may occur from contraction of airway and respiratory
muscles. The tonic phase is followed by the clonic phase, which involves rhythmic
bilateral contraction and relaxation of the extremities. A myoclonic seizure involves
bilateral jerking of muscles, generalized or confined to the face, trunk, or one or more
extremities. Absence seizures are nonconvulsive, and complex partial seizures are
accompanied by automatisms.