15. Vascular Pathology
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
63 Terms
What blood vessels do Atherosclerosis affect?
Large and medium arteries
What blood vessels do Arteriosclerosis affect?
Small arteries and arterioles
What blood vessels do Aneurysms affect?
Vary by type of aneurysm
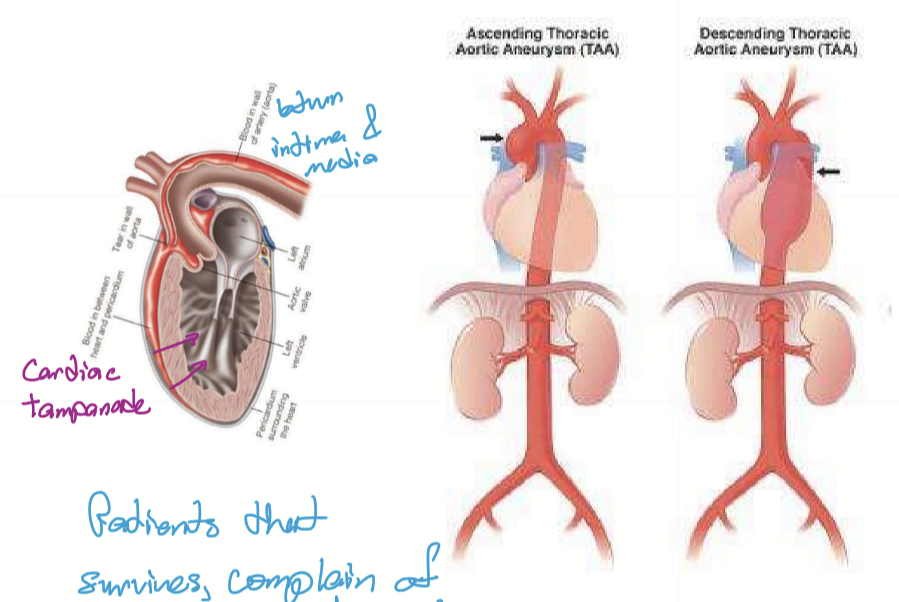
What blood vessels do Vasculitis affect?
Immune complex vasculitis (SLE): capillaries and venules
Giant cell arteritis: specific large arteries
What blood vessels do autoregulation affect?
Arterioles and capillary sphincters
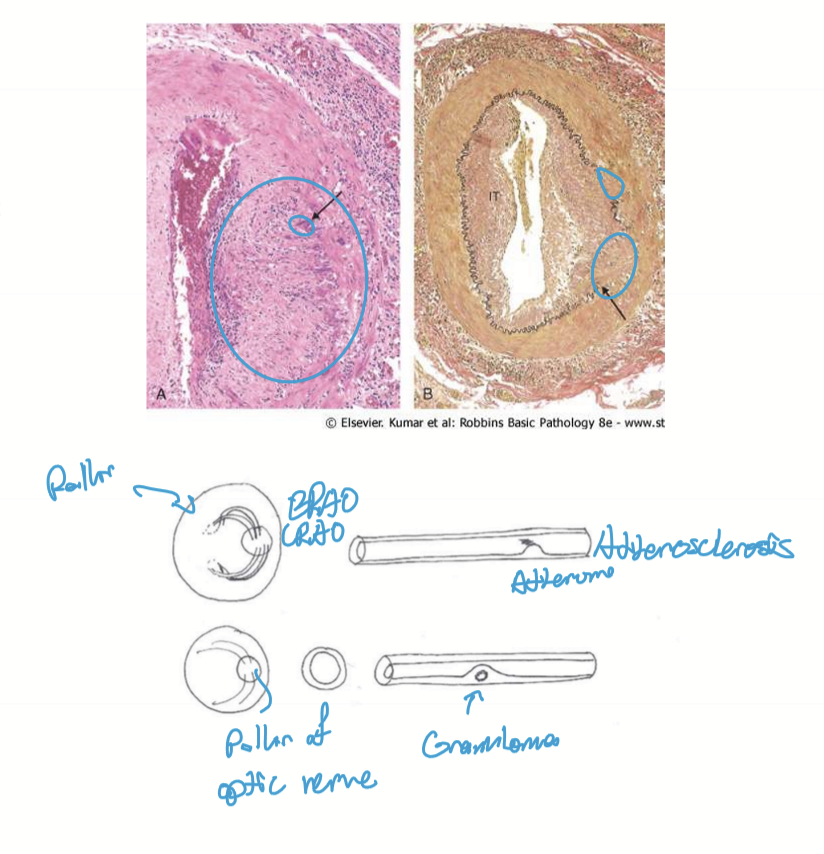
What is atherosclerosis?
A systemic vascular disease at bends due to endothelial stress.
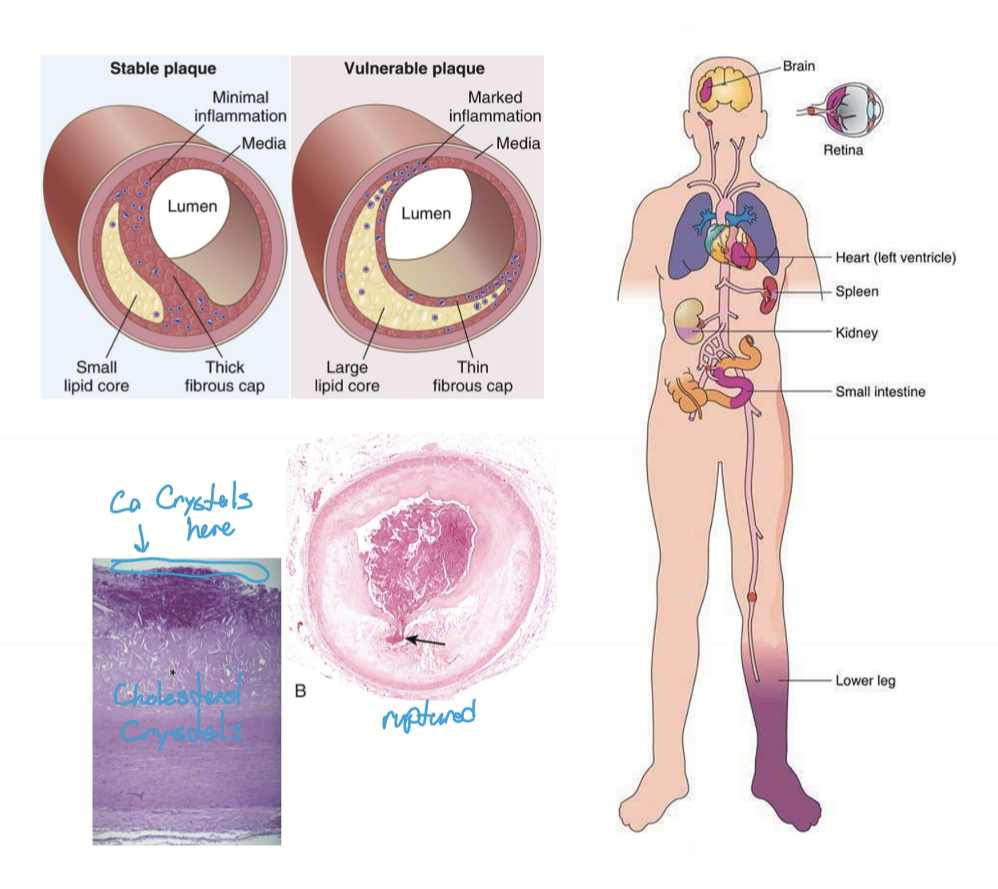
What is atherosclerosis associated with?
Dyslipidemia
What does emboli typically include?
Thromboemboli
Calcium emboli
Cholesterol emboi (hollenhorst plaques)
What are the presentations of atherosclerosis?
BRAO/CRAO: vision loss
Peripheral vascular disease: gangrene and amputations
CVA: Ischemic stroke
Heart: Ischemic heart disease → Dilated cardiomyopathy → CHF; Aortic Valve Disease → Hypertensive heart disease → CHF
Vascular: Arteriosclerosis
Abdominal aortic aneurysm
Renal stenosis
Death
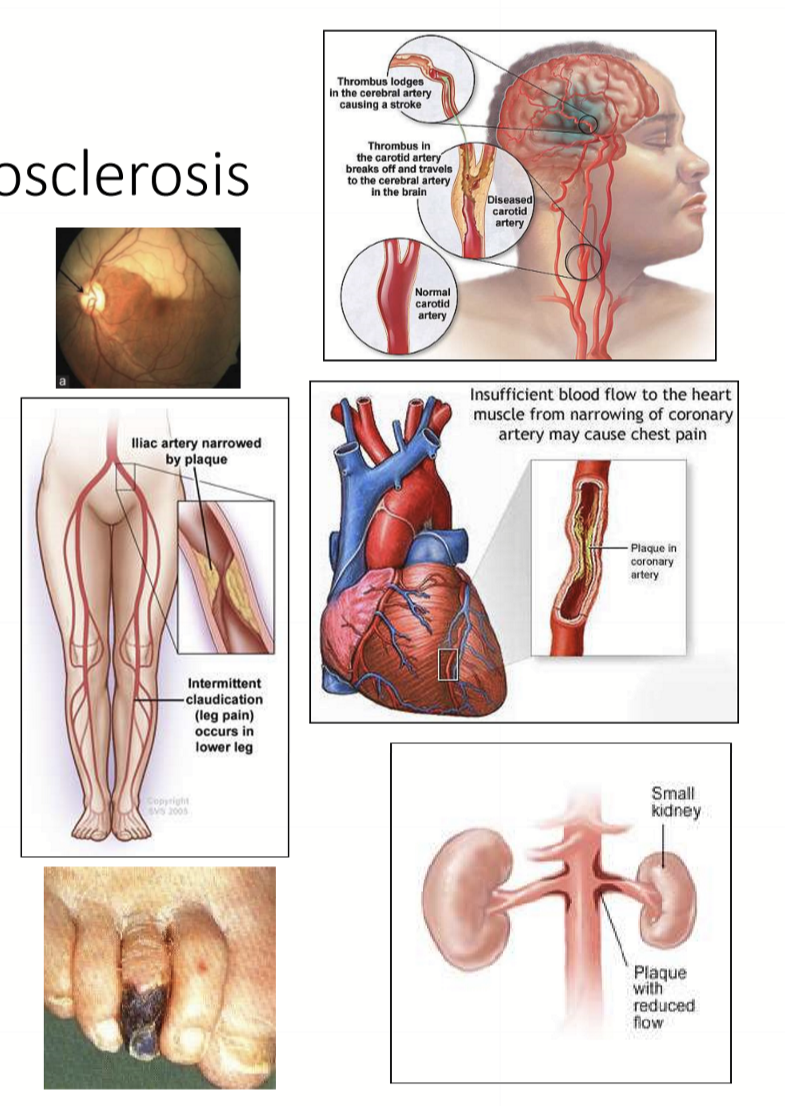
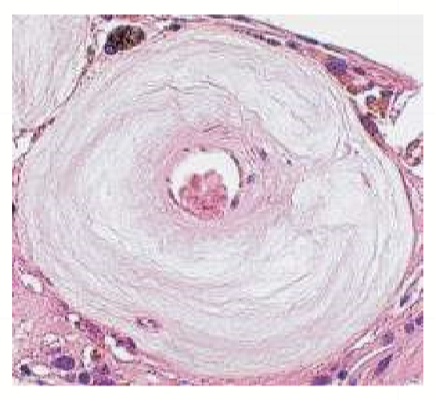
What is arteriosclerosis?
A systemic vascular disease in small arteries and arterioles. Associated with stress caused by HTN that narrows the lumen of BV by making the BV thick and stiff. No emboli arise from arteriosclerosis.
What are some presentations associated with arteriosclerosis?
BRVO/CRVO: vision loss
CVA: hemorrhagic stroke
Heart: Hypertensive heart disease → CHF
Vascular issues from arteriosclerosis
Death
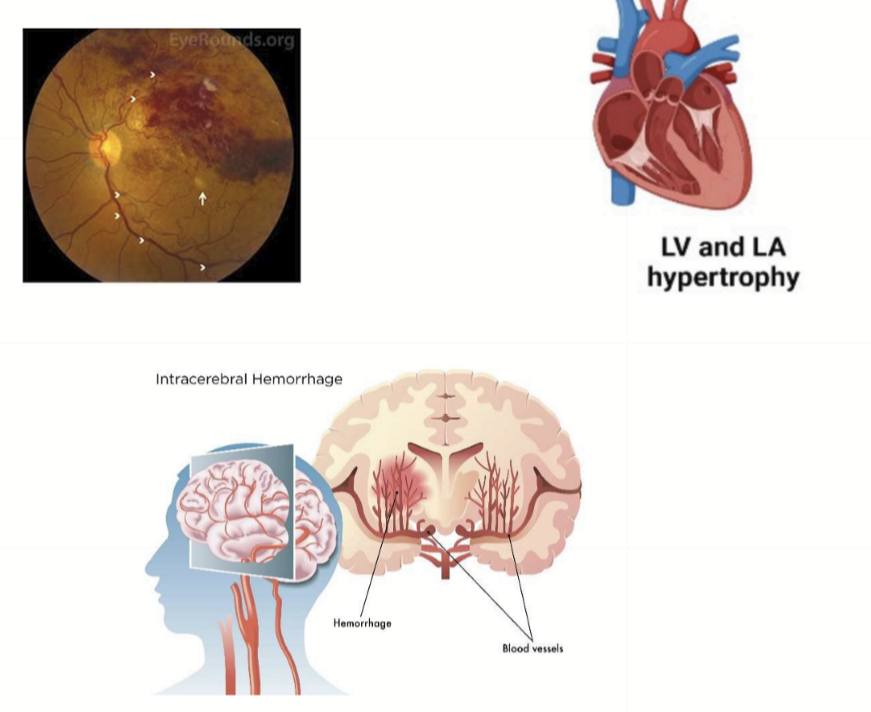
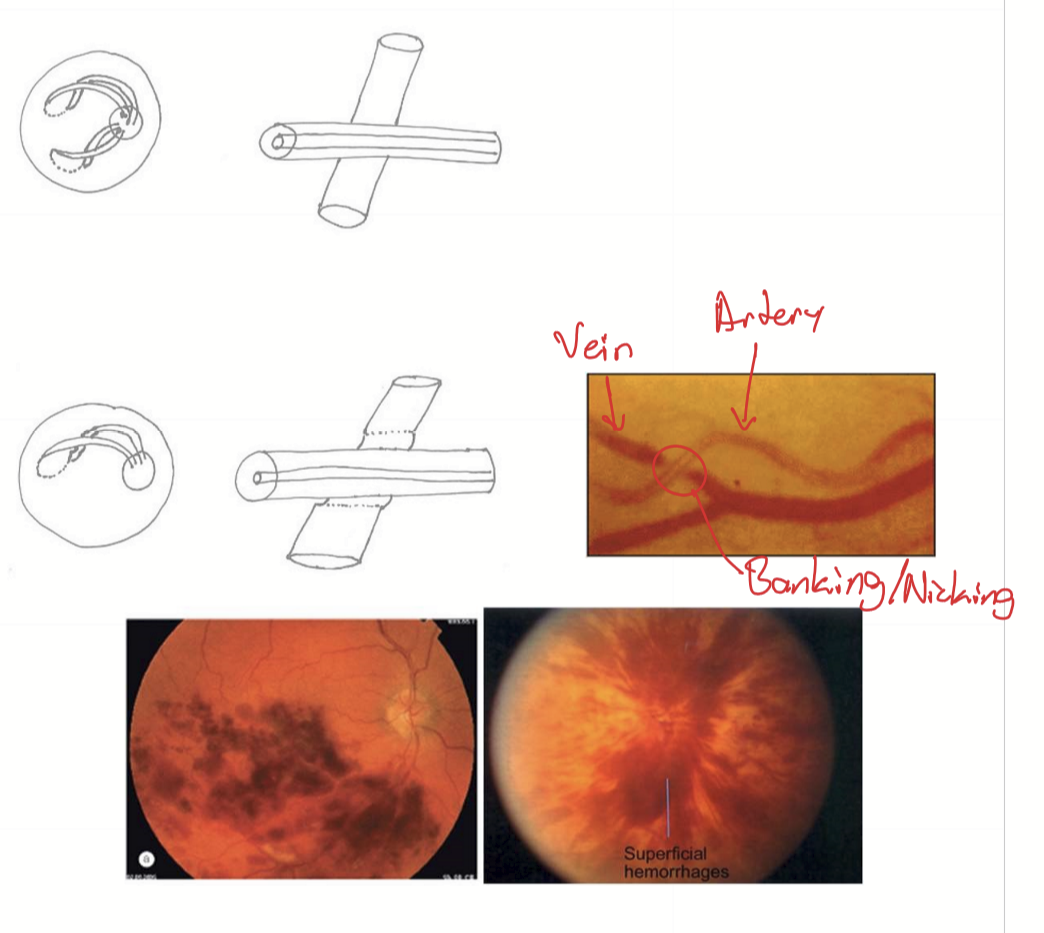
What are the majority of venous occlusions caused by?
90-95% caused by arteriosclerosis; In retina arteries cross over retinal veins at arteriovenous crossings, sharing adventitia. The arterial disease then occludes the vein.
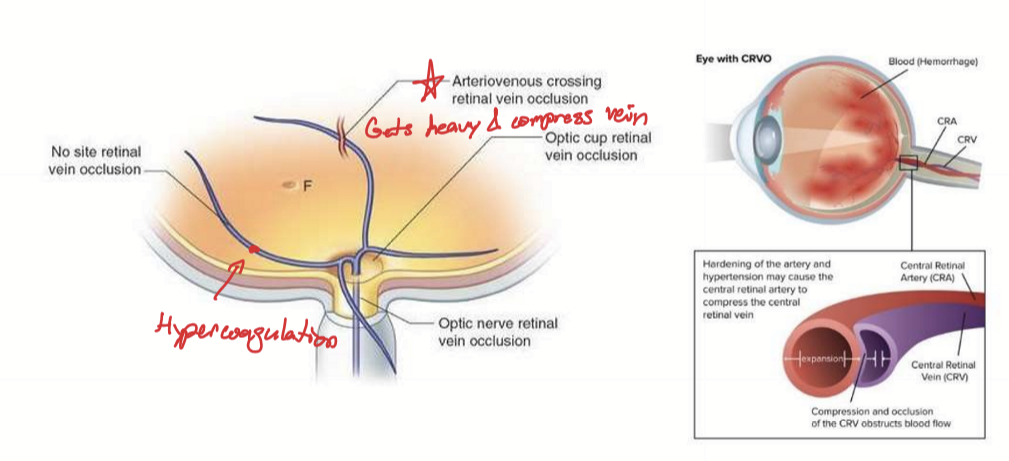
What is another potential cause for venous occlusions?
Hypercoagulopathies at 5%. They do not occur at Arteriovenous crossings.
What is a sign of HTN retinopathy?
Copper wiring
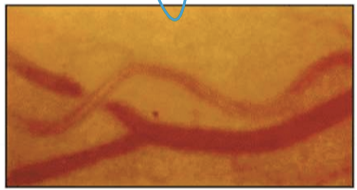
What is the pathogeneis of RVO caused by arterioscleorsis?
HTN
Arteriosclerosis in retinal artery/arterioles making the artery heavy (hyaline deposition in tunica intima)
Compresses underlying vein
Vein becomes occluded
blood backs up into capillary beds
High Pcap causes lysis of capillary beds
Hemorrhage → retinal venous occlusion
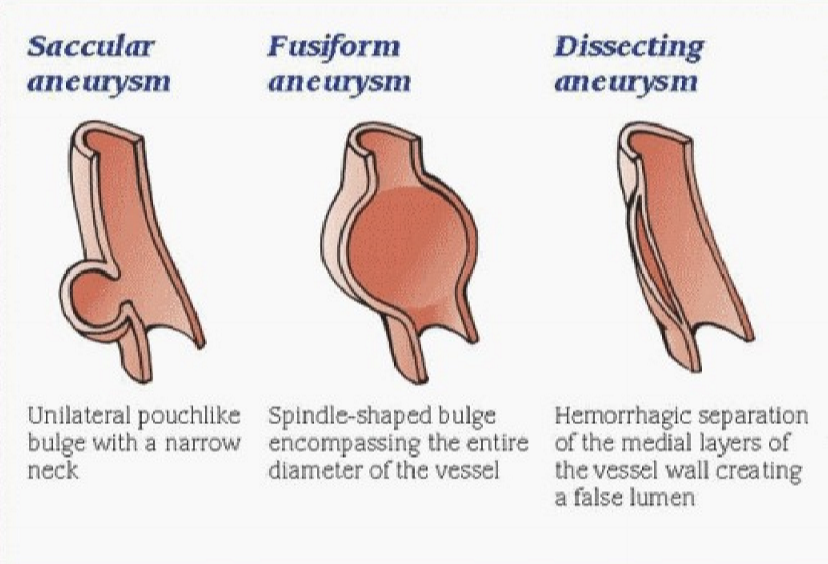
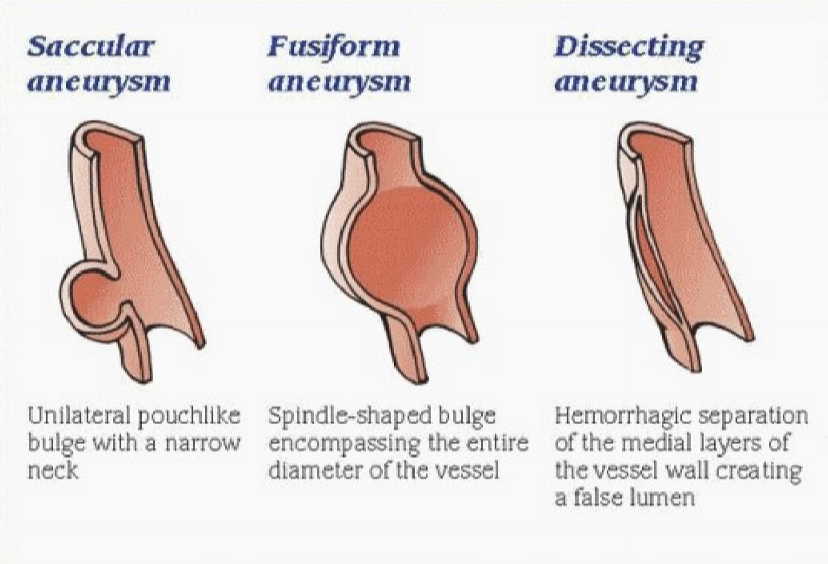
What are the different shapes of aneurysms?
Saccular aneurysm
Fusiform aneurysm
Dissecting aneurysm
What are the different types of aneurysms?
Berry aneurysm
Abdominal Aortic Aneurysms (AAA)
Dissecting aneurysm/ False aneurysm/ Pseudoaneurysm: Carotid dissections and Thoracic aortic dissection
What differentiates a true aneurysm vs a false aneurysm?
True aneurysms involve all 3 layers of the blood vessel. False aneurysms involve a wall defect (dissection) so that a hematoma forms within the vessel between the intima and media.
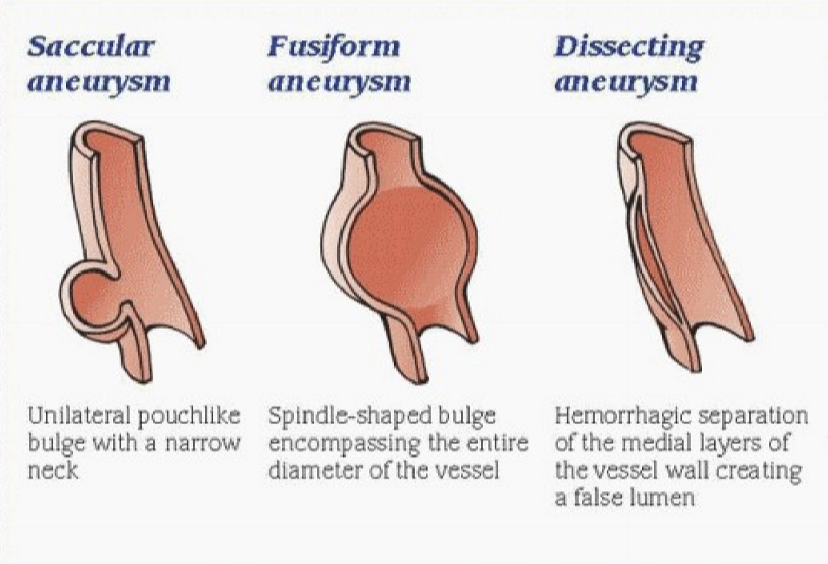
What does a fusiform look like?
The entire diameter of the blood vessel is enlarged
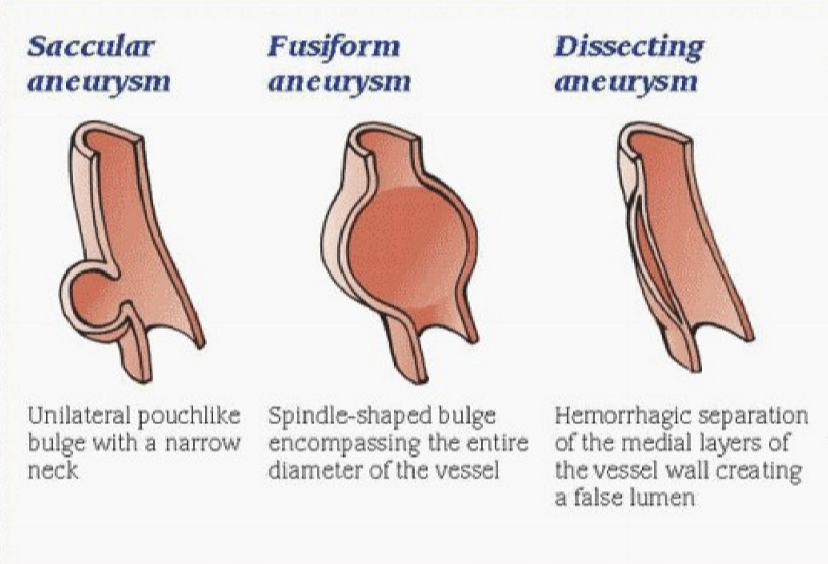
What does a saccular or berry aneurysm look like?
A sack-like bulge on one side of the blood vessel
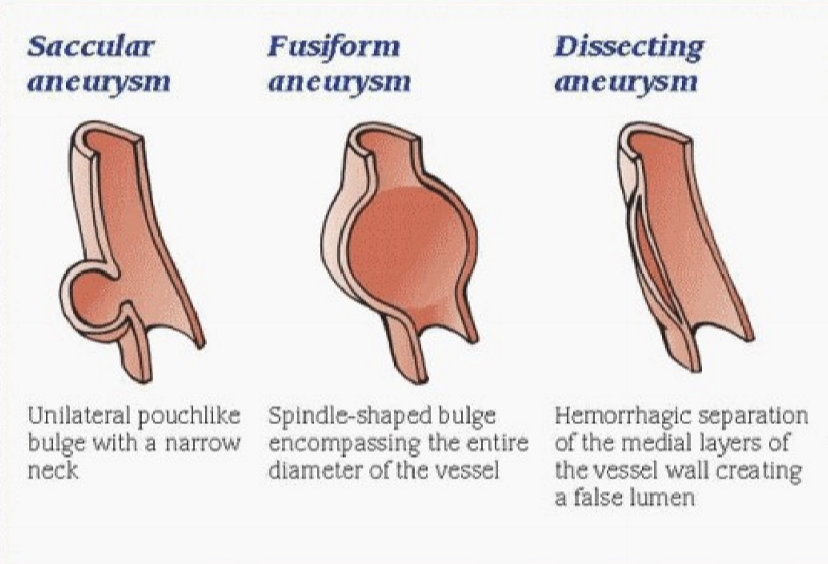
What does a false/pseudo/dissection aneurysm look like?
Separation of the layers
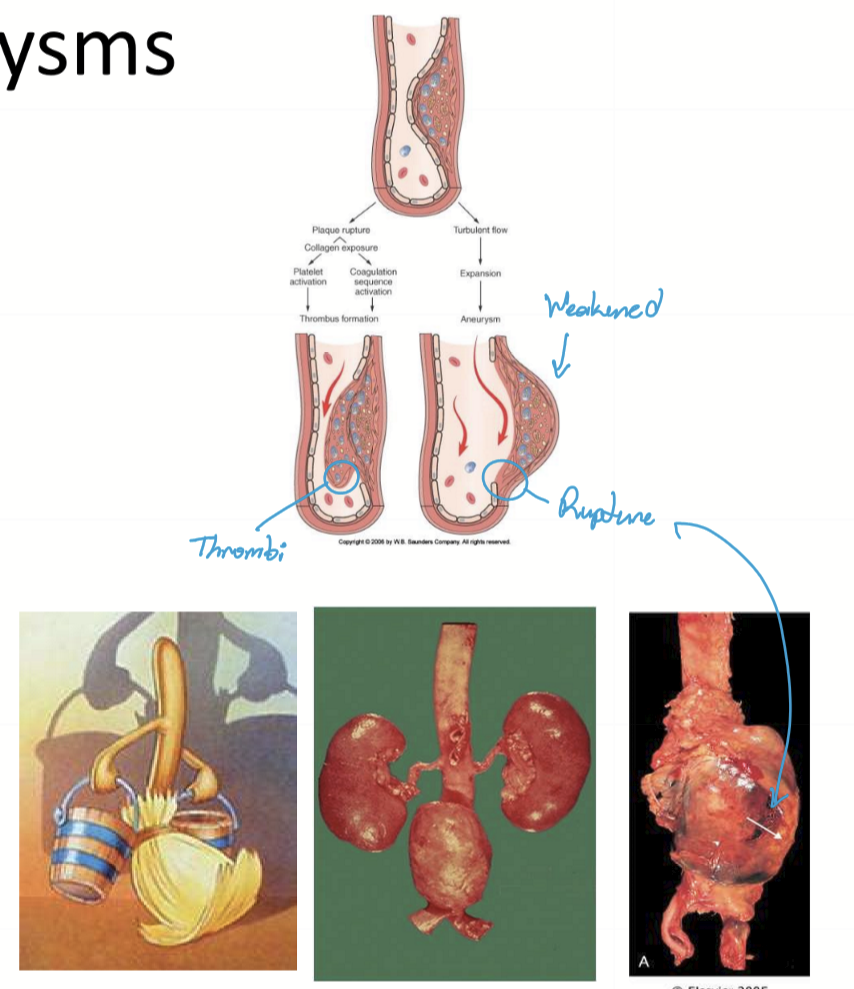
What are Abdominal Aortic Aneurysms?
Fusiform aneurysms in the abdominal cavity that are asymptomatic, but can be life-threatening of it ruptures. The are occasionally found during a physical.
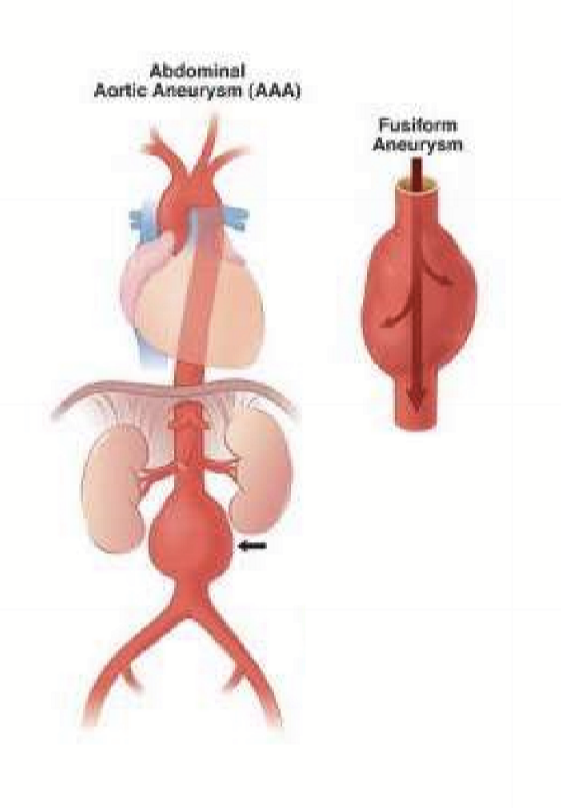
What is the etiology of Abdominal aoritc aneurysms?
Combination of atherosclerosis and HTN
What is the pathogenesis of Abdominal Aortic Aneurysm?
Atheroma forms in abdominal aorta, weakening the vessel wall
HTN causes dilation, and fusiform aneurysm forms
Sequelae:
atheroma ruptures, causing thrombus and/or embolus
Vessel wall can rupture into retroperitoneum with a 90% morality rate
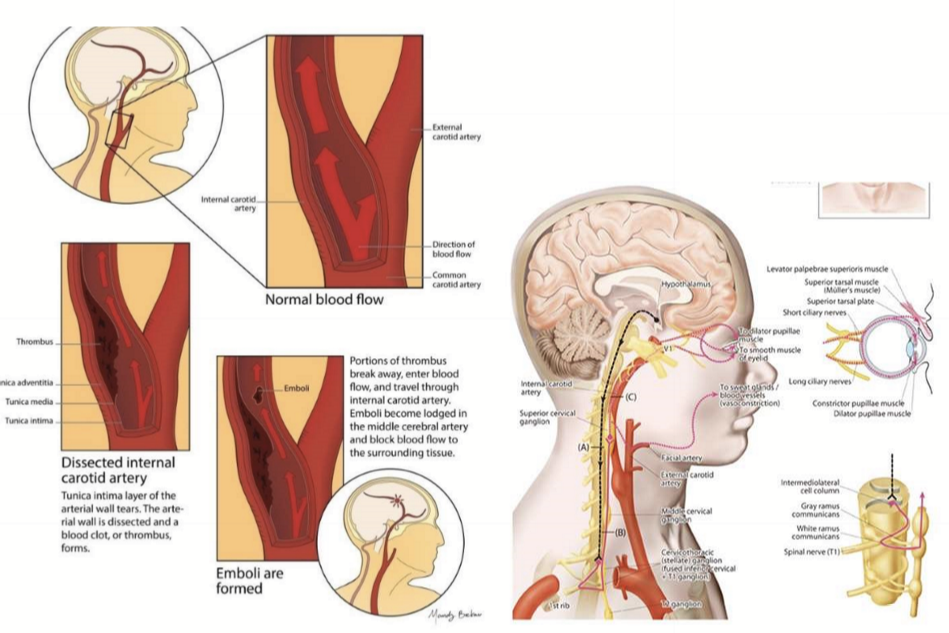
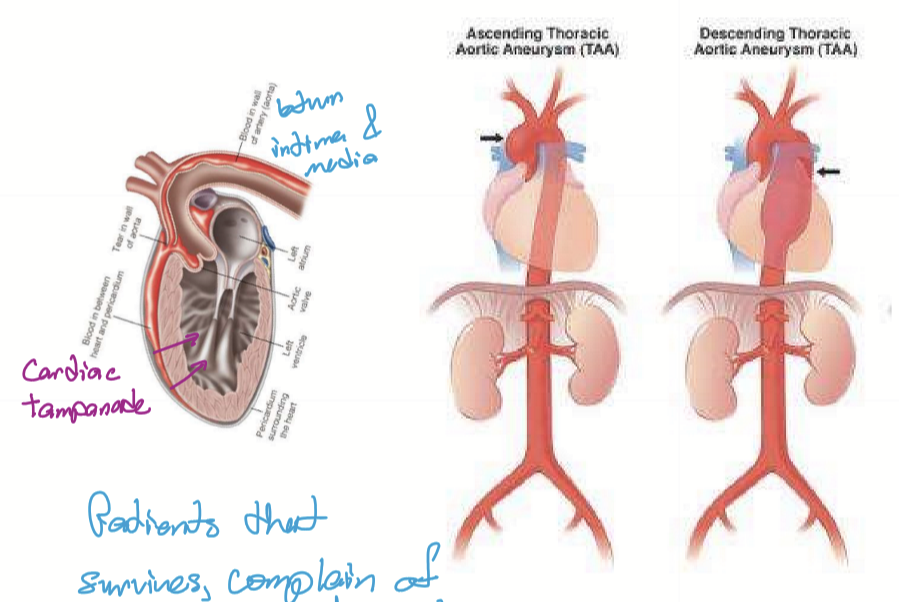
What is the pathogenesis of Dissecting Aneurysm?
Thunic intima breaks and blood can enter between tunica intima and tunica media. The blood separates the vessel layers. Hematoma can form in the dissected layers → source of emboli. Intima can fall into lumen and cause an occlusion → ischemia/infarct.
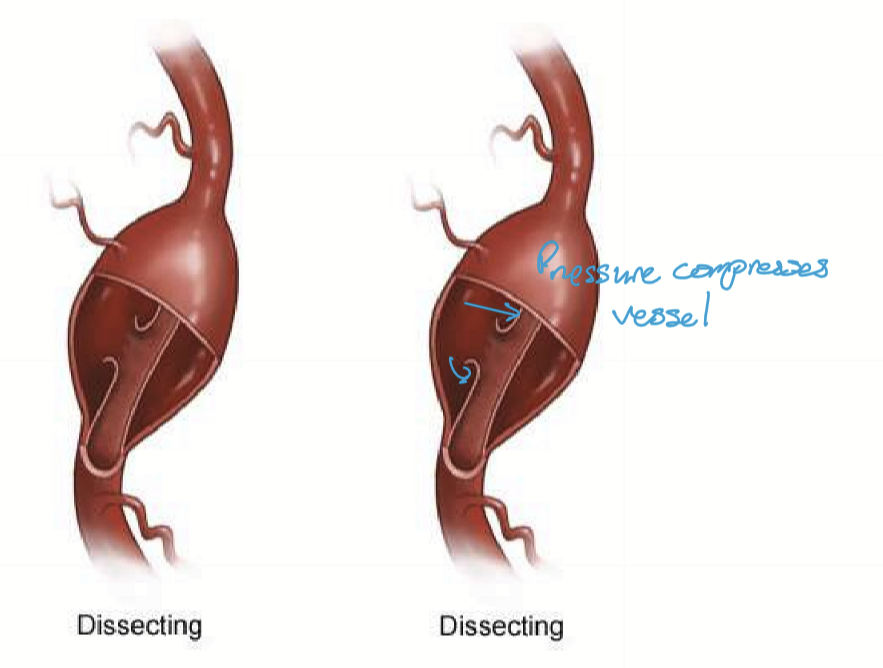
What are 2 examples of dissecting aneurysms?
Carotid dissection & Thoracic aortic dissection
What is the etiology of a carotid dissection?
Trauma: major and minor
What is the sequelae of a carotid dissection?
Ischemic Stroke (global or focal)
BRAO/CRAO
Horner’s Syndrome (sympathetic affected postganglion neuron)
What part of the aorta does a thoracic aortic dissection affect?
Any part of the thoracic aorta.
What genetic condition can cause both thoracic aortic aneurysm and aortic dissection?
Marfan Syndrome
What can an ascending aortic aneurysm lead to if it tears into the pericardial sac?
Cardiac tamponade (a life-threatening condition where fluid accumulates in the pericardial sac)
Death
What happens in a thoracic descending aortic aneurysm?
The aneurysm can tear down the descending aorta (thorax).
What symptoms might survivors of aortic dissection complain of?
A ripping sensation along the roots of the aorta
In an aortic dissection, which layers of the aorta are separated?
The intima and media
What is vasculitis?
A general term for vessel wall inflammation with presentations based on location of inflammation.
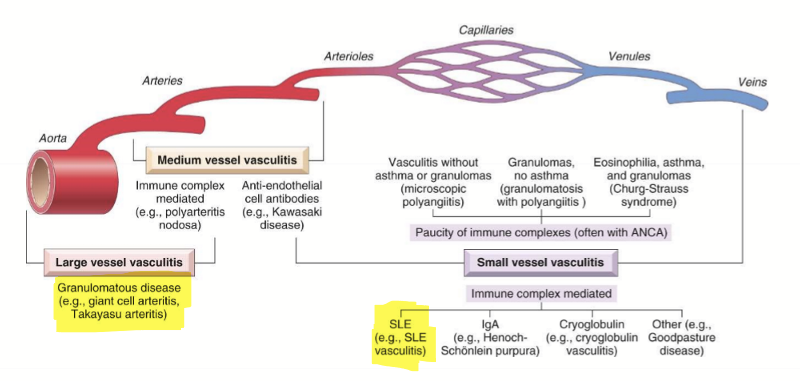
What is immune-complex mediated vasculitis
When the patient makes autoantibodies following an infection. It causes petechiae on skin and retina due to capillary hemorrhage. It is a type III hypersensitivity reactions.

What is the pathogenesis of Immune-complex mediated vasculitis?
sensitization
antibodies produced
circulating immune complex forms and deposits on vessel wall
activates PMNs and compliment
intimal inflammation/damage
blood seeps out of vessel, causing petechiae
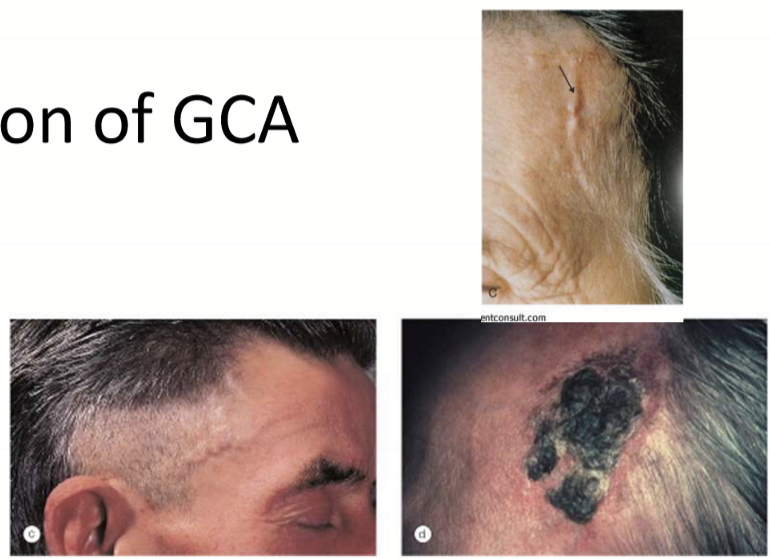
What is Giant Cell Arteritis (GCA)?
A systemic autoimmune disease affecting temporal, ophthalmic, and vertebral arteries.
What is typically associated with GCA?
Chronic granulomatous disease (DTH)
Elevated ESR >60mm/hr
ELevated CRP
What is the epidemiology of GCA?
70+ yrs old
Most common vasculitis in elderly in US, Canada, and Europe
What arteries can be affected by GCA?
Temporal artery
Vertebral artery
Ophthalmic artery
What are the presentations of the temporal artery being affected by GCA?
Scalp pain and potential necrosis
headache
jaw claudication/hurts to chew
What are the presentations of the vertebral artery being affected by GCA?
Stroke
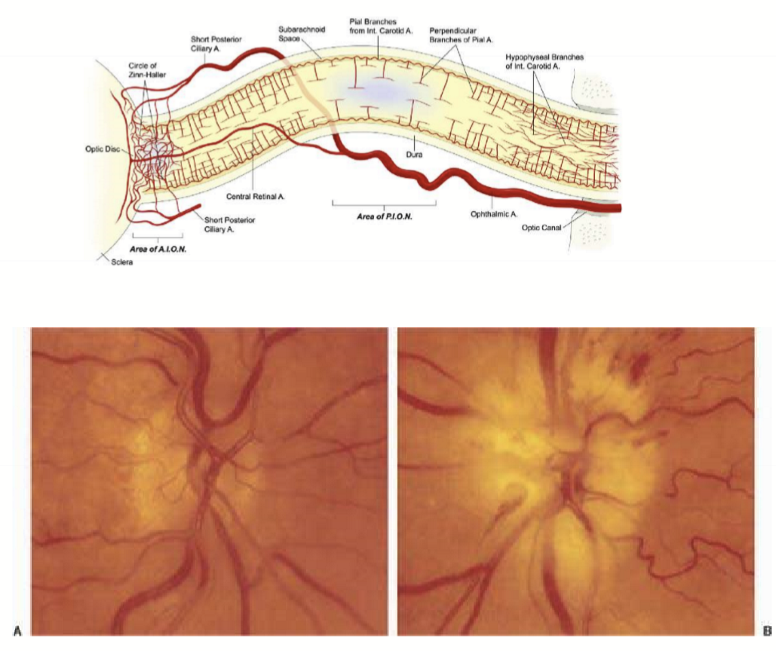
What are the presentations of the ophthalmic artery being affected by GCA?
Sudden painful unilateral irreversible vision loss: diffuse vision loss or inferior altitudinal defect; Relative afferent pupillary defect (RAPD)
Pale, edematous optic nerve; often with flame-shaped hemorrhages
Can become bilateral vision loss within 24 hours
What is the pathogenesis of GCA?
Granulomatous inflammation in the tunica intima and tunica media disrupts the internal elastic membrane
Inflammation causes swelling of vessel wall
Lumen narrows
Vessel can become occluded if the lumen causes pressure to fall below the critical closing pressure
Ischemia of downstream tissues
What blood tests should be ordered to determine GCA?
ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein)
Why are ESR and CRP ordered in suspected Giant Cell Arteritis (GCA)?
They are markers of systemic inflammation. Both are typically elevated in GCA and support the diagnosis, but confirmation is via temporal artery biopsy.
What should you do if you suspect the patient has GCA?
Steroids immediately
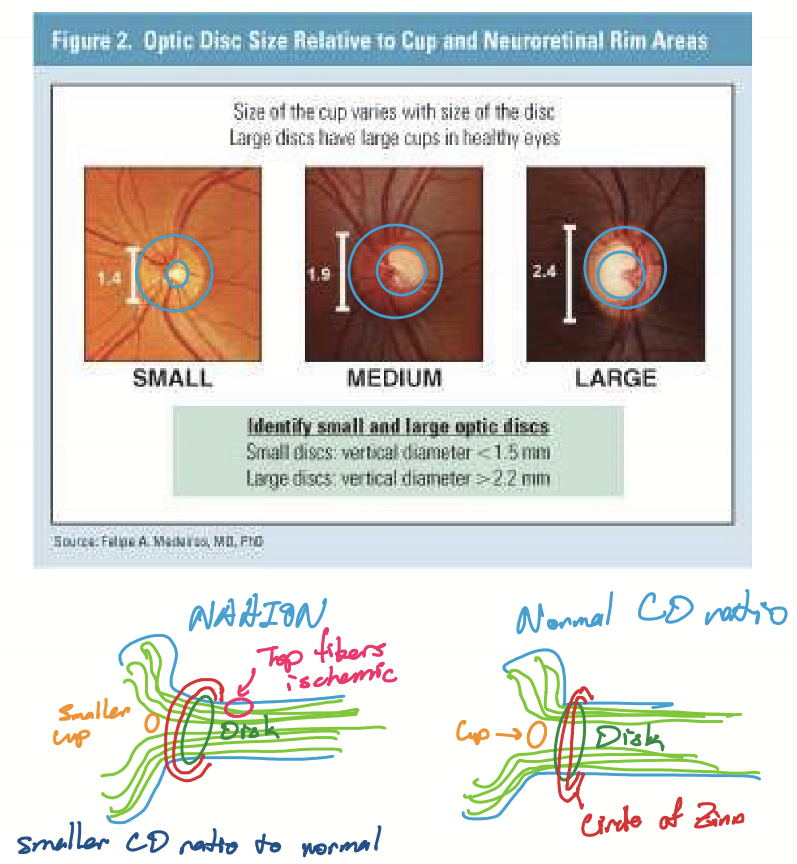
What is Non-arteritic Anterior Ischemic Optic Neuropathy (NAAION)?
Ischemia of the optic head that is not caused by GCA.

What are the characteristic of NAAION?
Ischemia to optic nerve head
reduced perfusion of superior circle (believed to caused by poor autoregulation)
Normal ESR and CRP = non-inflammatory
2nd most common optic neuropathy after glaucoma

What are the presentations of NAAION?
Sudden painless unilateral vision loss (somewhat reversible)
Inferior altitudinal defect
RAPD
Pale, edematous optic nerve, possible flame-shaped hemorrhages
Less likely to become bilateral
Typically noticed in the morning
What are predisposing factors for NAAION?
Having a small crowded disc: nerve fibers packed into small disc are thicker and increases the distance O2 needs to diffuse, thus increases risk of ischemia.
What are factors that cause NAION?
Nocturnal hypotension with poor autoregulation
High cholesterol
Sleep apnea
Rx:
Antihypertensive Rx
Erectile dysfunction Rx (within 24 hours)
GLP-1?
How can some factors of NAION be prevented?
Take antihypertensives in the morning to counteract nocturnal hypotension
Use CPAP for sleep apnea
Statin for high cholesterol
Do not take ED meds/lifesyle chagnes if possible
What is the pathogenesis of NAION?
Dysfunction of autoregulation mechanisms
poor filling pressures
Poor venous drainage
What are the differences between arteritic anterior ischemic optic neuropathy (AAION) vs non-arteritic anterior ischemic optic neuropathy (NAAION)
What is Raynaud’s Phenomenon?
Abnormal vasospasm triggered by cold or emotion affecting fingers and toes.
What is raynaud’s phenomenon linked to?
Glaucoma
What does raynaud’s phenomenon cause?
triphasic discoloration “red, white, blue”. Red = vasodilated; white = area vasoconstricted; blue = cyanosis
What can happen if raynaud’s phenomenon is severe?
Gangrene
What is emboli defined as?
Any substance that originates in one vessel and is relocated by blood flow to a new location and is a potential for infarct.
What is Virchow’s triad?
Three main factors that contribute to thrombosis: Stasis of blood flow, endothelial injury, and hypercoagulability.
What substances can become an emboli?
Atherosclerosis-related
thromboemboli
hollenhorst
calcium
Air
Amniotic fluid (during labor and delivery)
Cancer cells (metastases)
Venous Thrombosis
Fat from bone marrow