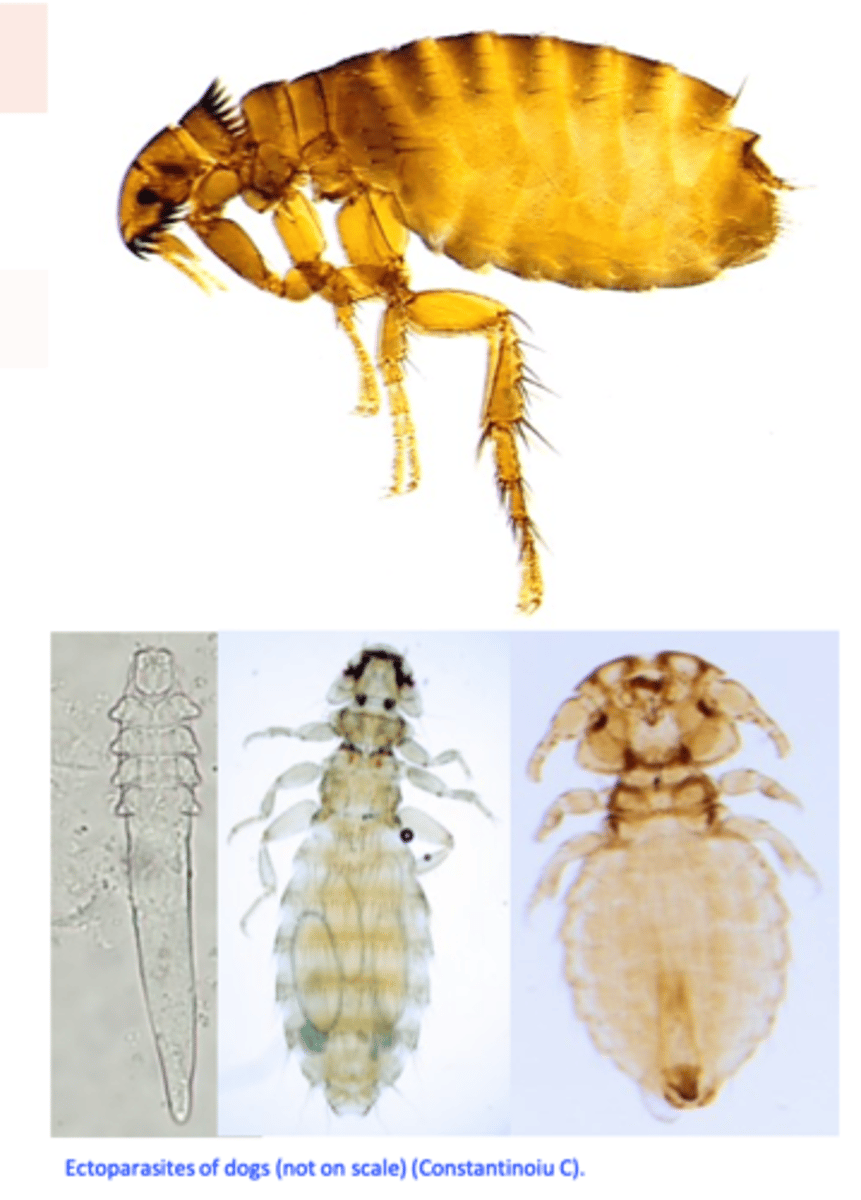
Small animal ectoparasites
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
Sarcoptes scabiei var canis
Hosts: dog, rarely cats
Morphology
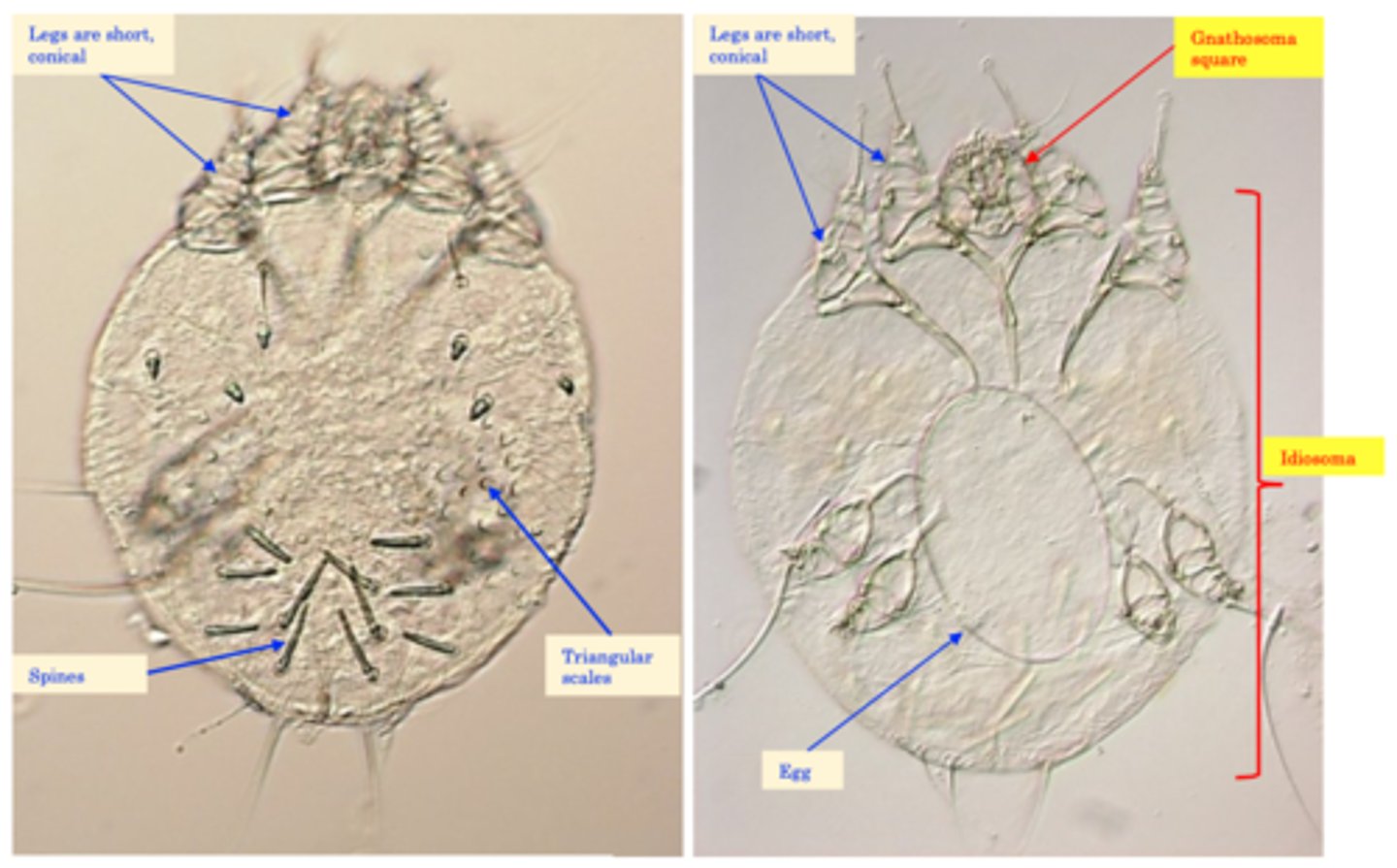
• Nothing regarding the morphology of the parasite has changed since we talked about Sarcoptes scabiei in pigs

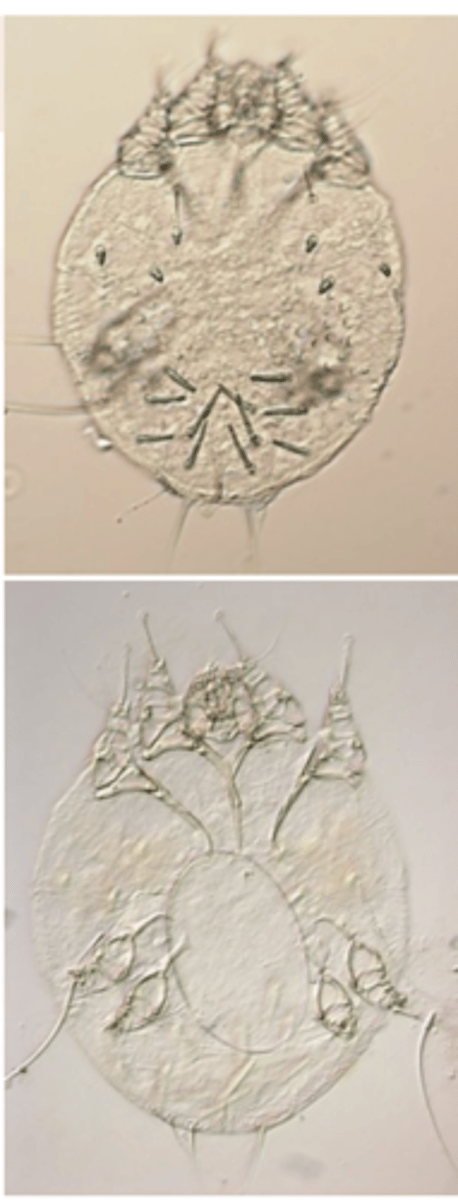
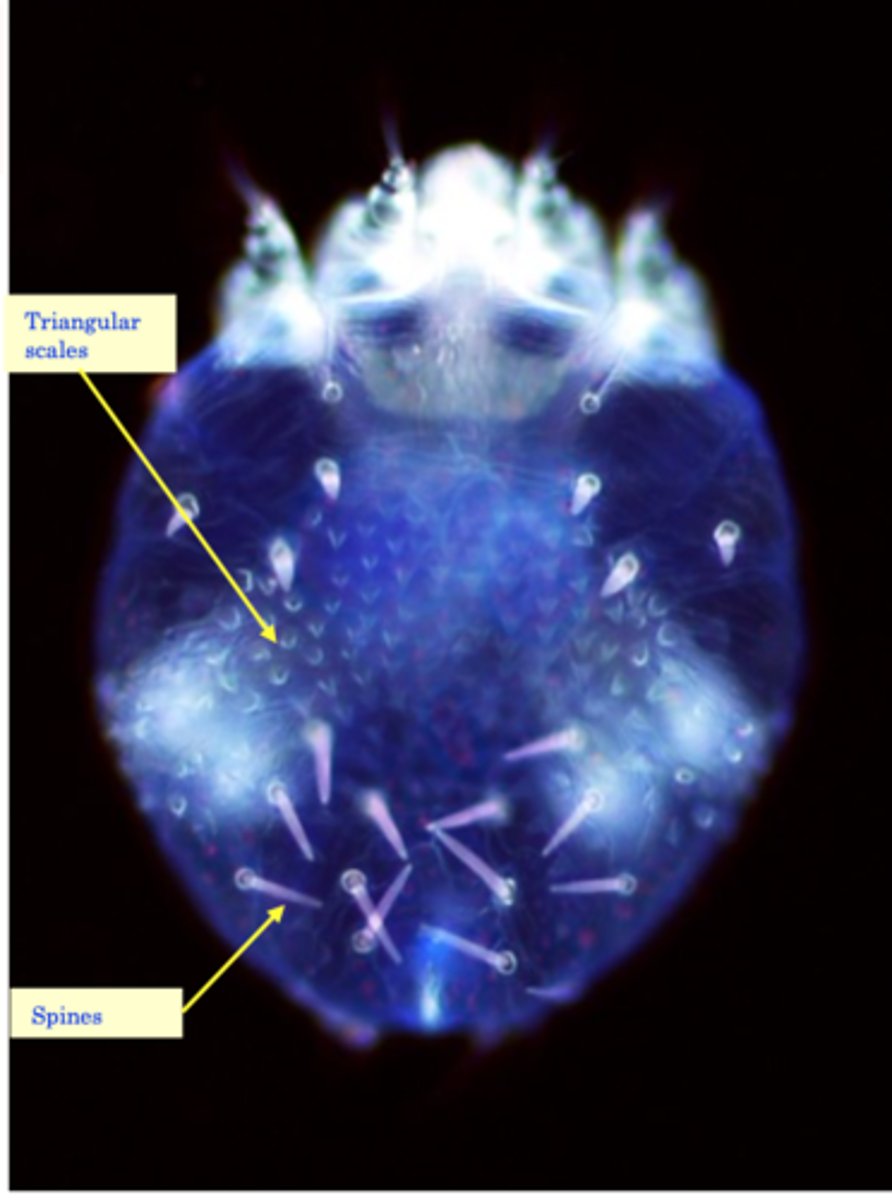
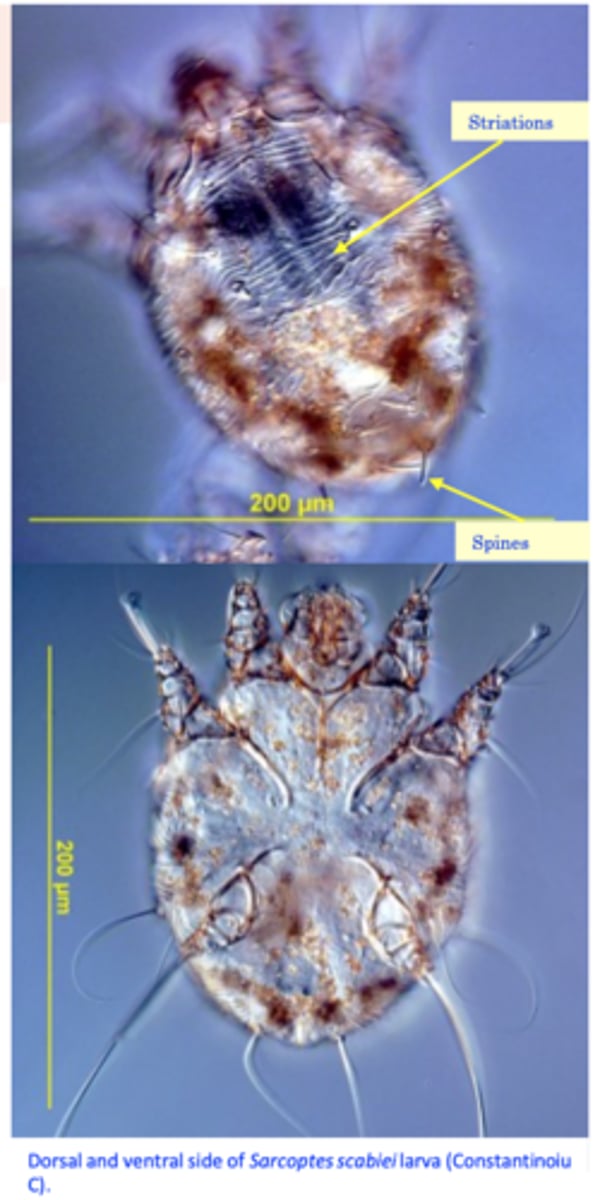
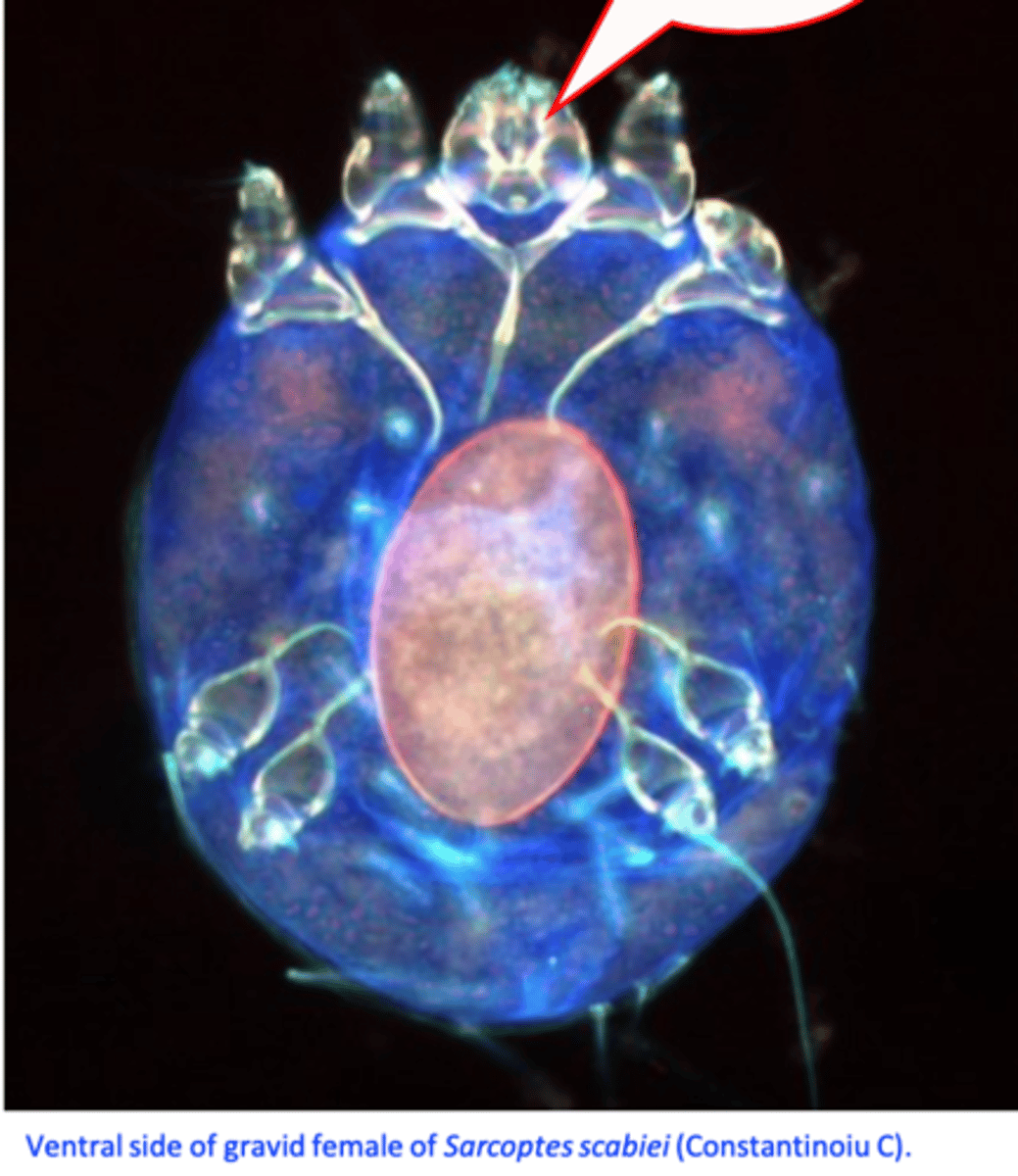
Sarcoptes scabiei var canis morphology
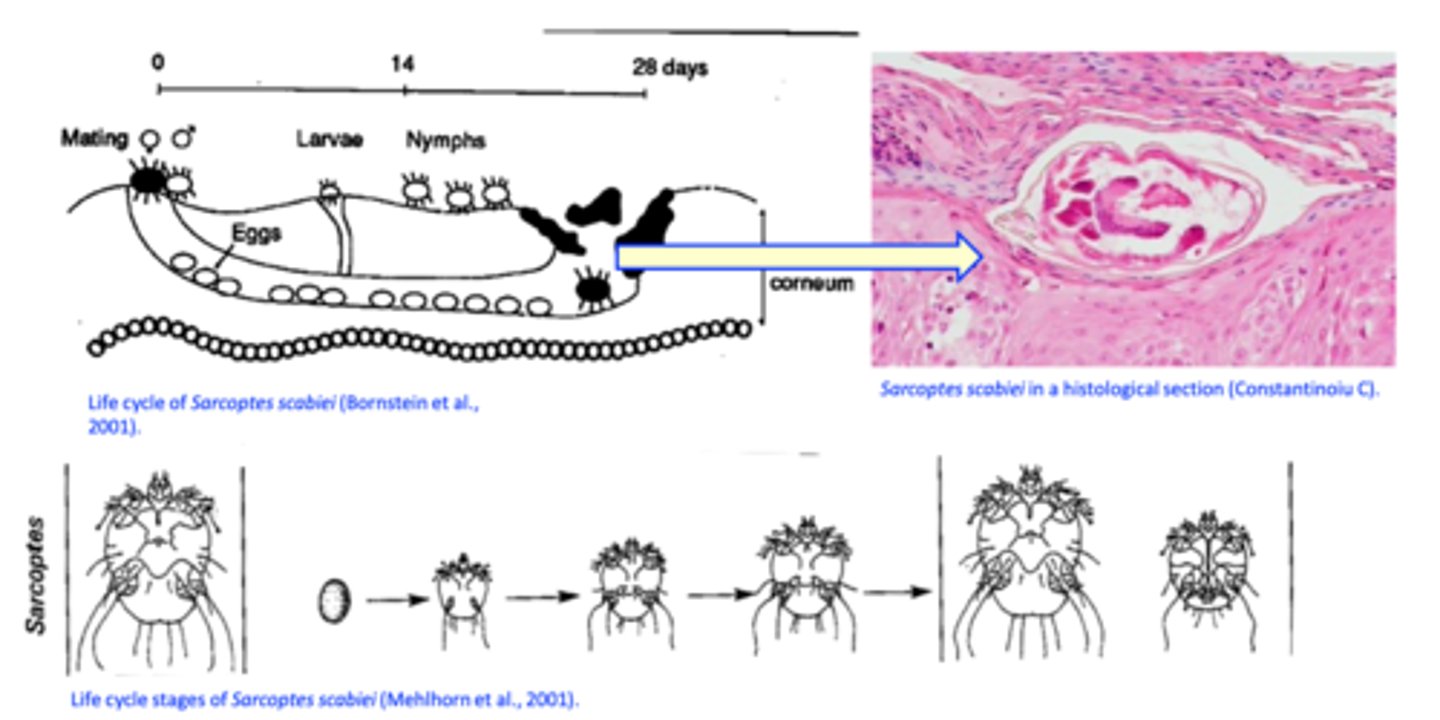
Sarcoptes scabiei var canis - Life cycle
Nothing has changed since we last talked about life cycle, either
Sarcoptes scabiei var canis
Significance for humans
S. scabiei var canis can be transmitted to humans but the parasites do not complete the life cycle
on humans => self-limited (however, the humans might get re-infested);
Human involvement has been reported in up to 50% of canine cases;
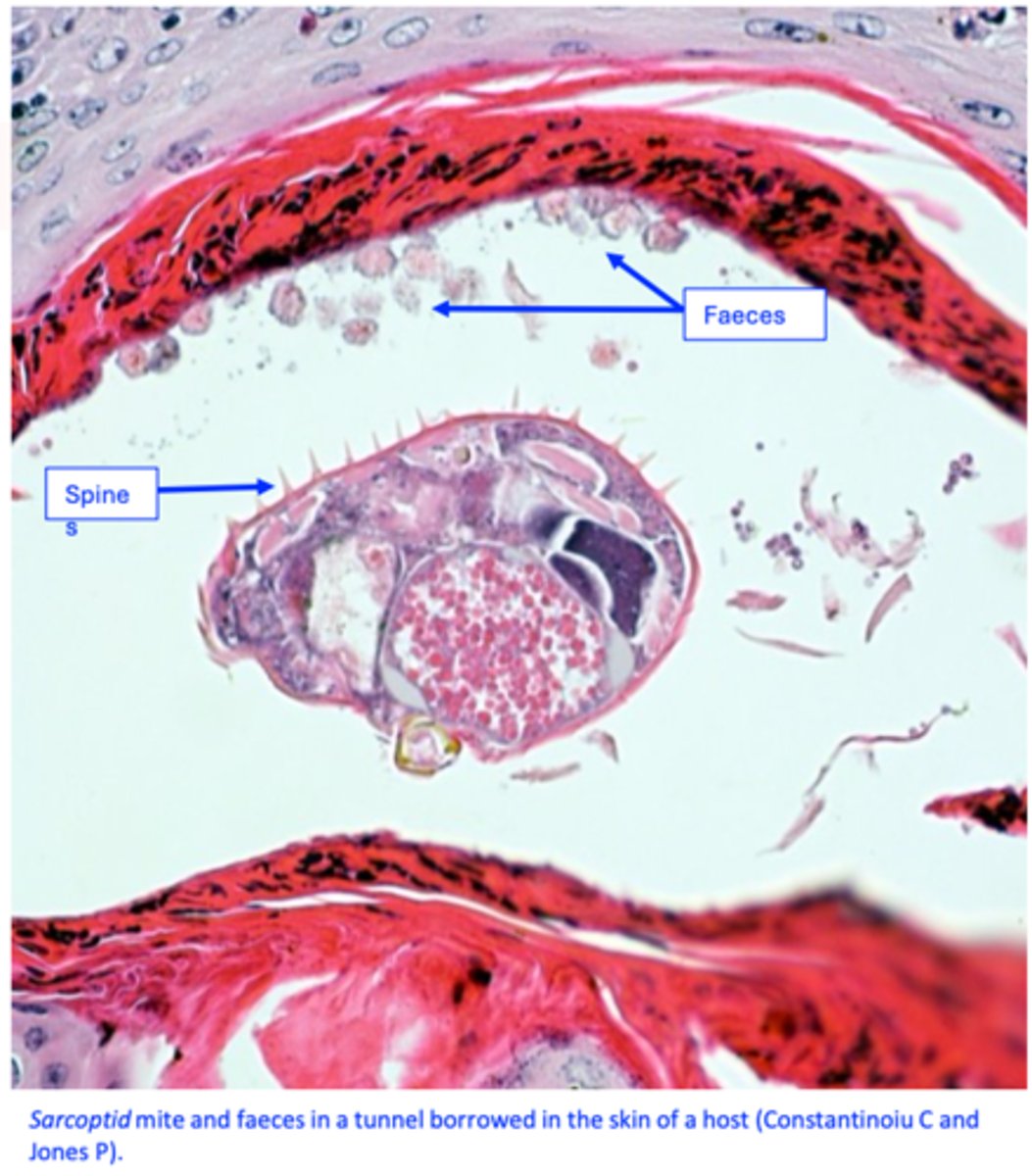
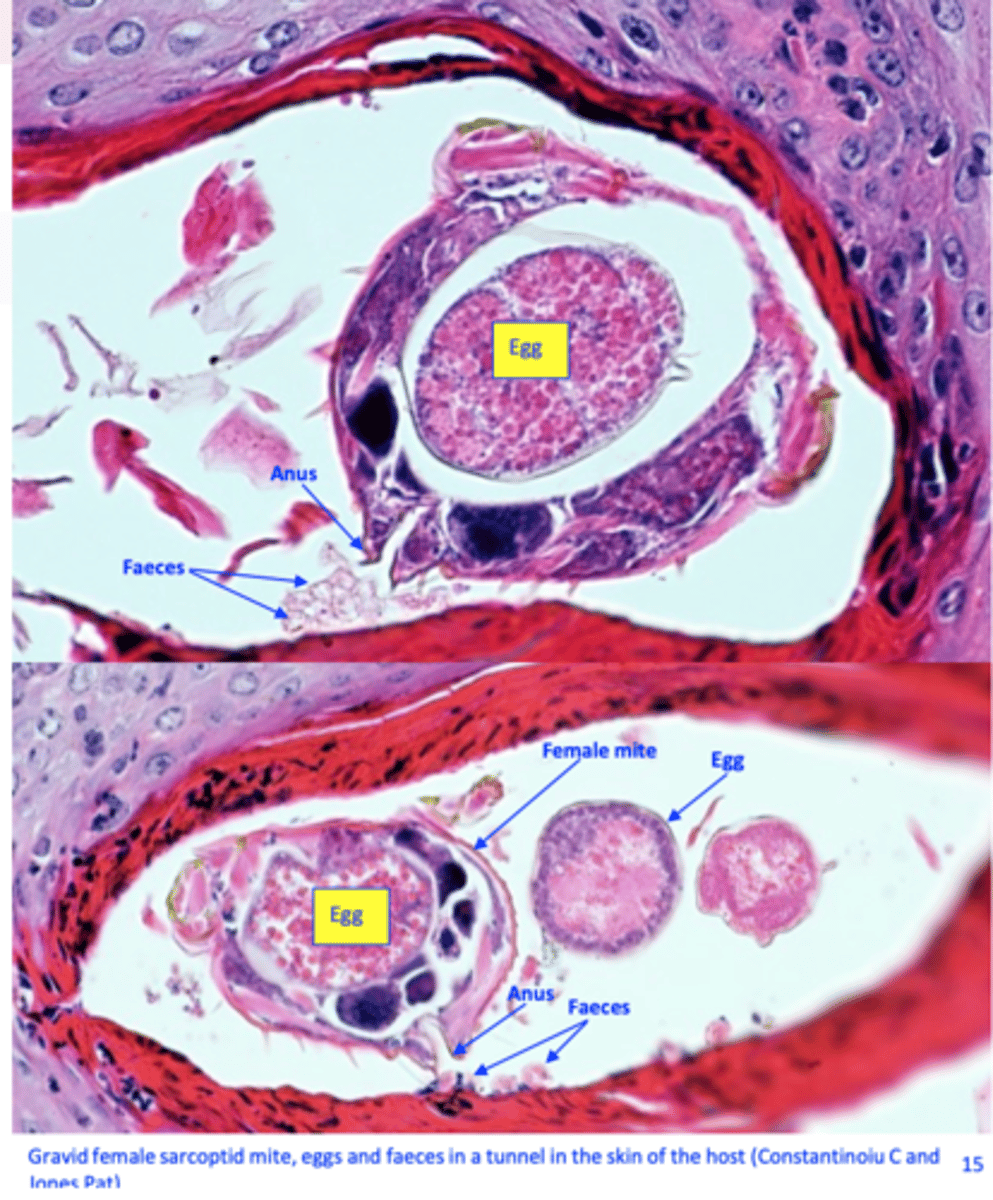
sarcoptes scabiei burrowing image
Sarcoptes scabiei var canis
Epidemiology
Distribution
Worldwide, can occur at any time of the year;
The disease is very contagious;
In multiple dog households, more than one dog is usually affected (the disease is very contagious);
Susceptibility
No differences in age, breed or sex ;
Usually, the infested dogs have a history of being in an animal shelter, having contact with stray dogs, or visiting a grooming or boarding facility;
Sarcoptes scabiei var canis
Transmission
• Direct;
• Indirect (via fur or fomites): depending on temperature and humidity the parasites might survive up to 21 days in the environment but it seems they are infective for less than 2 days;
Sarcoptes scabiei var canis
Pathogenesis
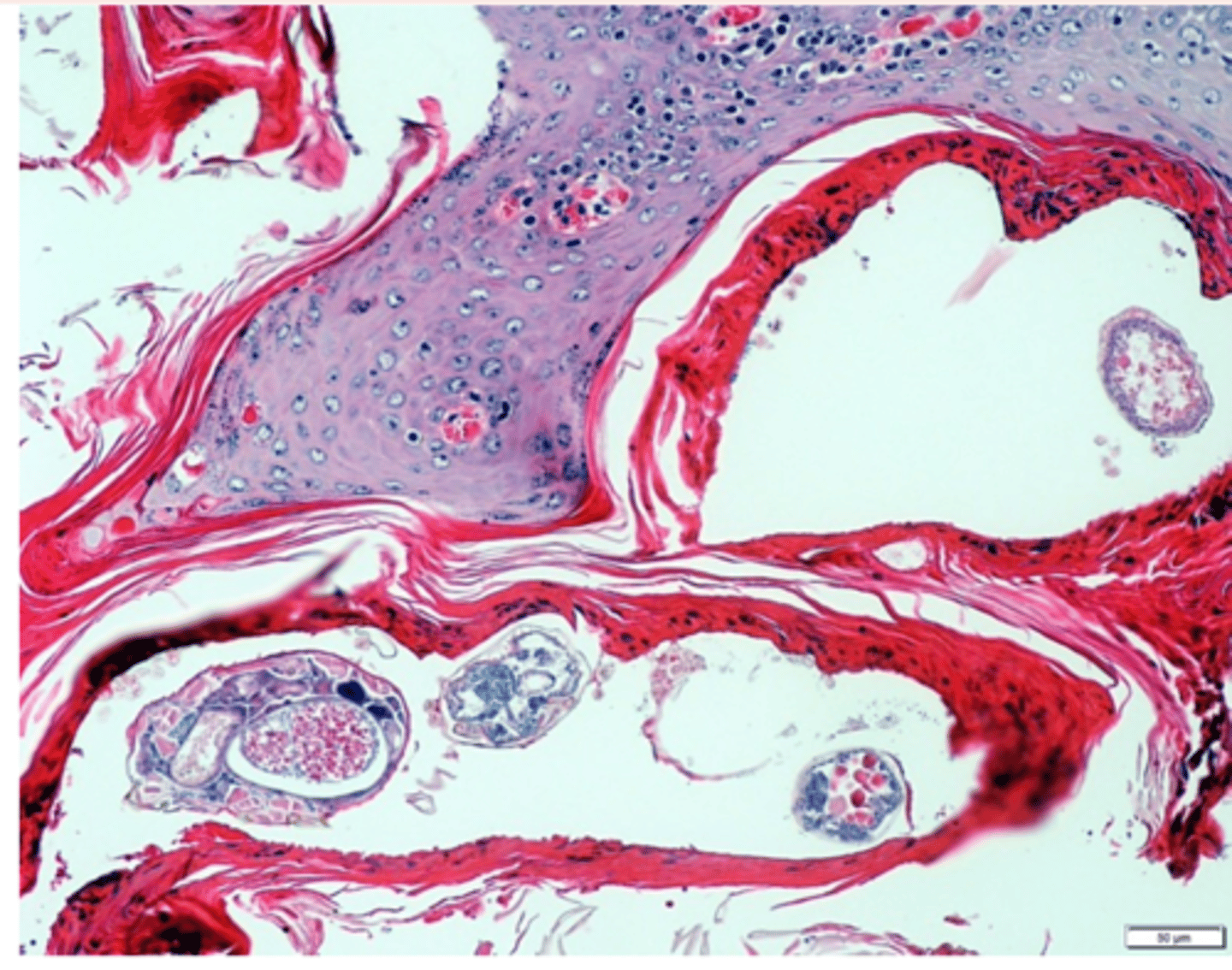
The mites act:
• Mechanically, while burrowing in the epidermis (chelicerae, gnatosoma, first pair of legs) => irritation, hyperkeratosis;
• Secretions, faeces, eggs induce both immediate and delayed hypersensitivity reactions 3-4 weeks after infestation => intense pruritus, congestion, papules.
Sarcoptes scabiei PATHOGENESIS
Sarcoptes scabiei var canis
Clinical signs
Incubation period: 10-30 days;
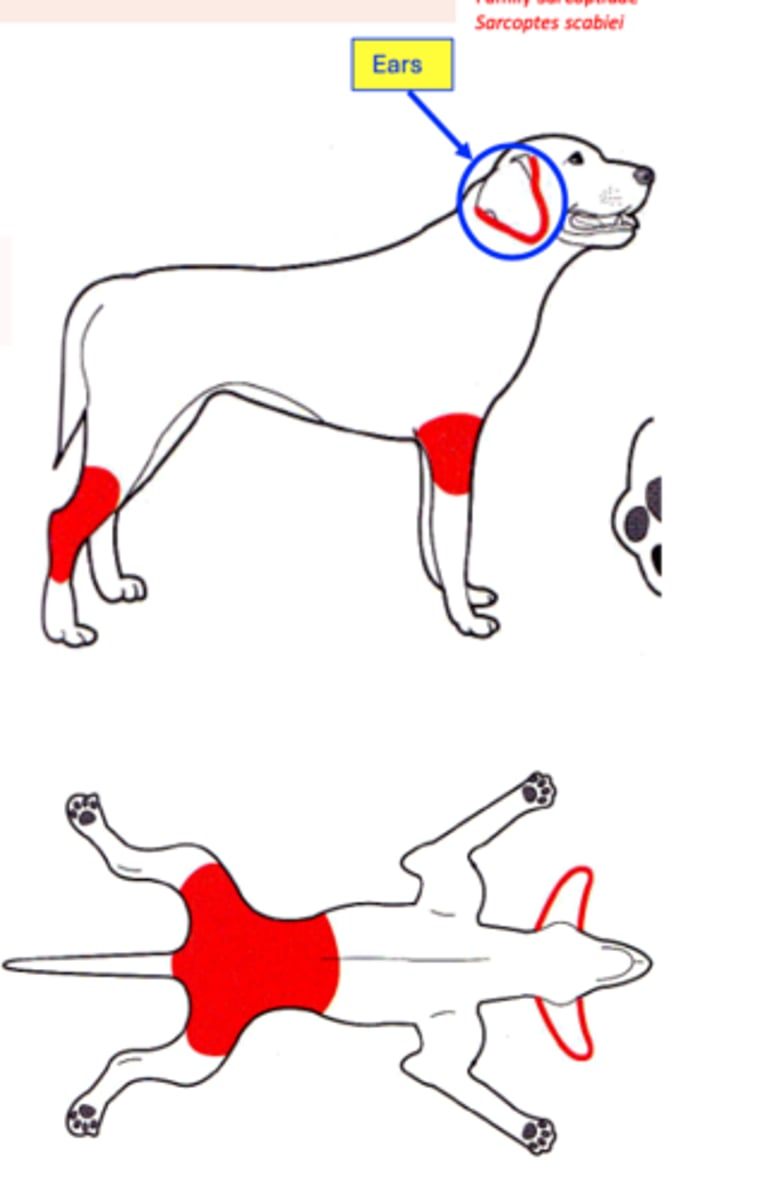
The mites prefer skin areas with little hair => initial lesions are observed on the ears, the elbows, the abdomen, and the hocks => as the disease progress the parasites might infest large areas of the host's body
Sarcoptes scabiei var canis
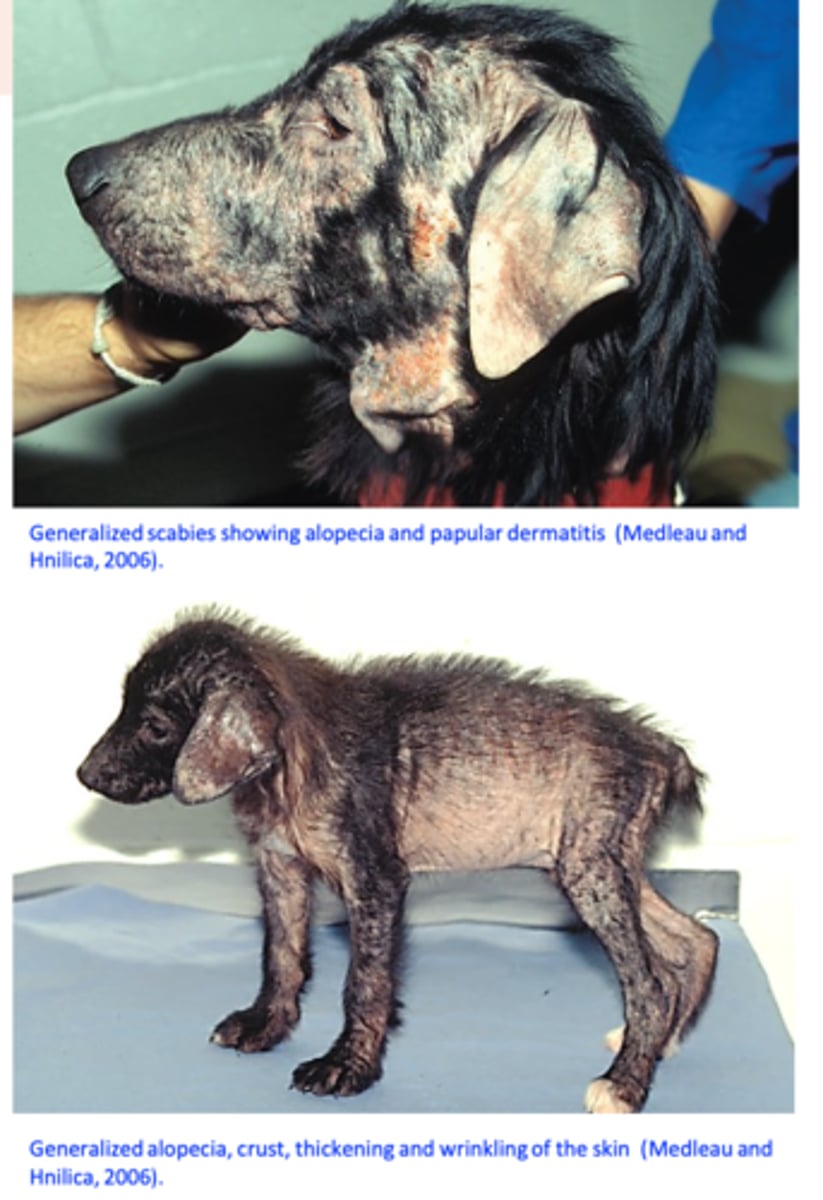
• Congestion, papules, intense pruritus, alopecia, crusts;
Initially the pruritus is reduced and proportional to the number of mites, it becomes very intense 20-30 days after exposure because of hypersensitivity;

Sarcoptes scabiei var canis
CLIN SIGNS CONTINUED
Initially the pruritus is reduced and proportional to the number of mites, it becomes very intense 20-30 days after exposure because of hypersensitivity;

CLIN SIGNS CONTINUED AGAIN IMAGE

Overall clinical signs for sarcoptes scabiei var Canis
Intense pruritus -> intense and constant itching -> extensive excoriations, self- trauma;
• Itching seems be more severe in warm environments;
• Some dogs (heavily infested?) may develop severe scaling and crusting;
• Bacterial complications, haemorrhage, thickening and wrinkling of the skin, weight loss and death might follow;
- Emaciation and death
Although they are uncommon, asymptomatic carriers exist.

sarcoptes clin signs on dog
Sarcoptes scabiei var canis
Diagnosis
Clinical signs (intense pruritus, alopecia, crusts, location of the lesions) and history (contact with other dogs, visits to kennels, owners affected etc);
Skin scrapings: detection of mites, eggs or faeces:
- Primary scraping sites: ear margins, the elbows, or the hocks (deep scrapings);
- Finding a mite, an egg or faeces is diagnostic, not finding does not exclude the disease;
Response to treatment;
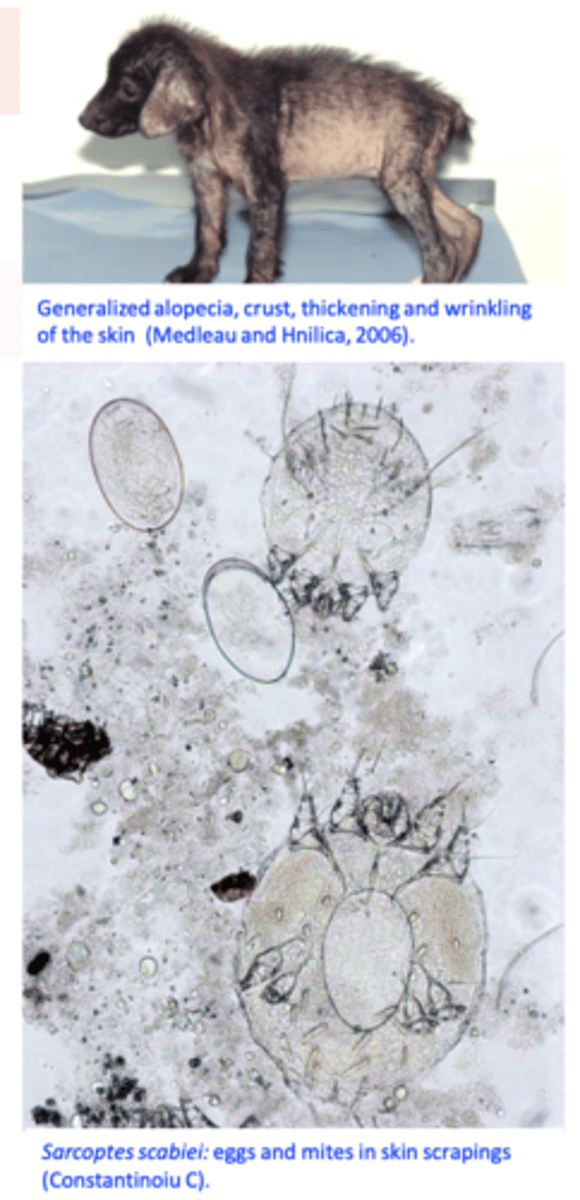
Sarcoptes scabiei var canis EXAM IMAGE POSSIBLY
FURTHER DIAGNOSIS:
• Detection of specific antibodies by ELISA
• Pinnal-pedal reflex:
Sarcoptes scabiei var canis
Differential diagnosis
Allergy (flea bites, food, contact)
Cheyletiellosis
Demodicosis
Pediculosis
Malassezia dermatitis
Sarcoptes scabiei var canis
Treatment
Treat all in-contact dogs (and the dogs known to have been in recent contact with the affected animal) (the disease is highly contagious);
Antibiotics for secondary pyoderma; corticosteroids for pruritus?
Clean the bedding/environment, grooming equipment, use acaricides?

Sarcoptes scabiei var canis
Macrocyclic lactones
Selamectin (Revolution/Stronghold);
Moxidectin (Advocate: Moxidectin & Imidacloprid);
Sarcoptes scabiei var canis
Isoxazolines
Afoxolaner (Nexgard, Nexgard Spectra)
Sarolaner (Simparica, Simparica Trio)
Fluralaner (Bravecto)
Notoedric mange
Notoedres cati
Hosts: cat and rabbits but it was also reported from foxes and dogs (it
can transiently infest humans).
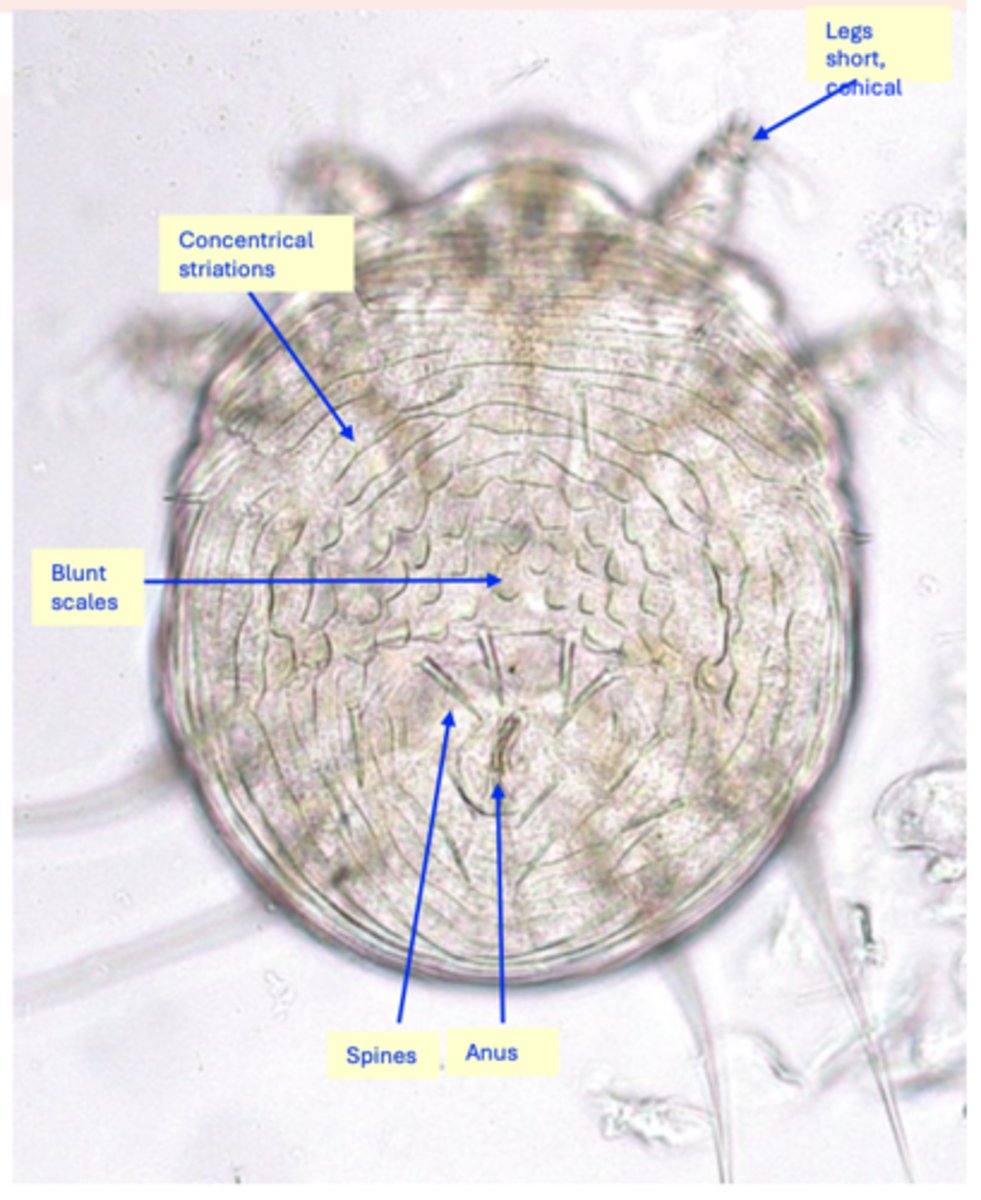
Morphology
Body: circular, translucent white;
Gnatosoma: short, rounded;
On the dorsal side of idiosoma there are:
Concentrical striations;
Spines (4 anterior pairs and 6 posterior pairs);
Blunt scales;
Legs: small, conical;
Anus: located dorsally.
Notoedres cati
Life cycle
Considered to be similar to that of Sarcoptes scabiei (egg, larva, two nymphal stages, adults);
Mites live in burrows in the epidermis;
Life cycle lasts 2-3 weeks;

Notoedres cati
Epidemiology
Worldwide distribution but might be rare in some countries
The disease is highly contagious => all of the cats in a household or neighborhood might become infested;
Transmission: usually by direct contact (the mites might seem to survive less than 3 days in the environment);
It usually affects the adult cats but it might present as a fulminating dermatitis in kittens.

Notoedres cati: Clinical signs
Clinical signs appear on the edge of the pinna and they spread around the eyes, nose, face, head, neck, anterior legs etc.
Alopecia, erythema, papules, thick gray crusts, thickening of the skin and formation of wrinkles;
Intense pruritus => excoriations and self- mutilation => bacterial skin complications;
• The intense pruritus and inflammation might be due to the proximity of the burrowing tunnels to the nerve endings and development of a hypersensitivity reaction;
Young cats can die;
Older cats become emaciated, apathic and die after 4-5 months if left untreated;

Notoedres cati
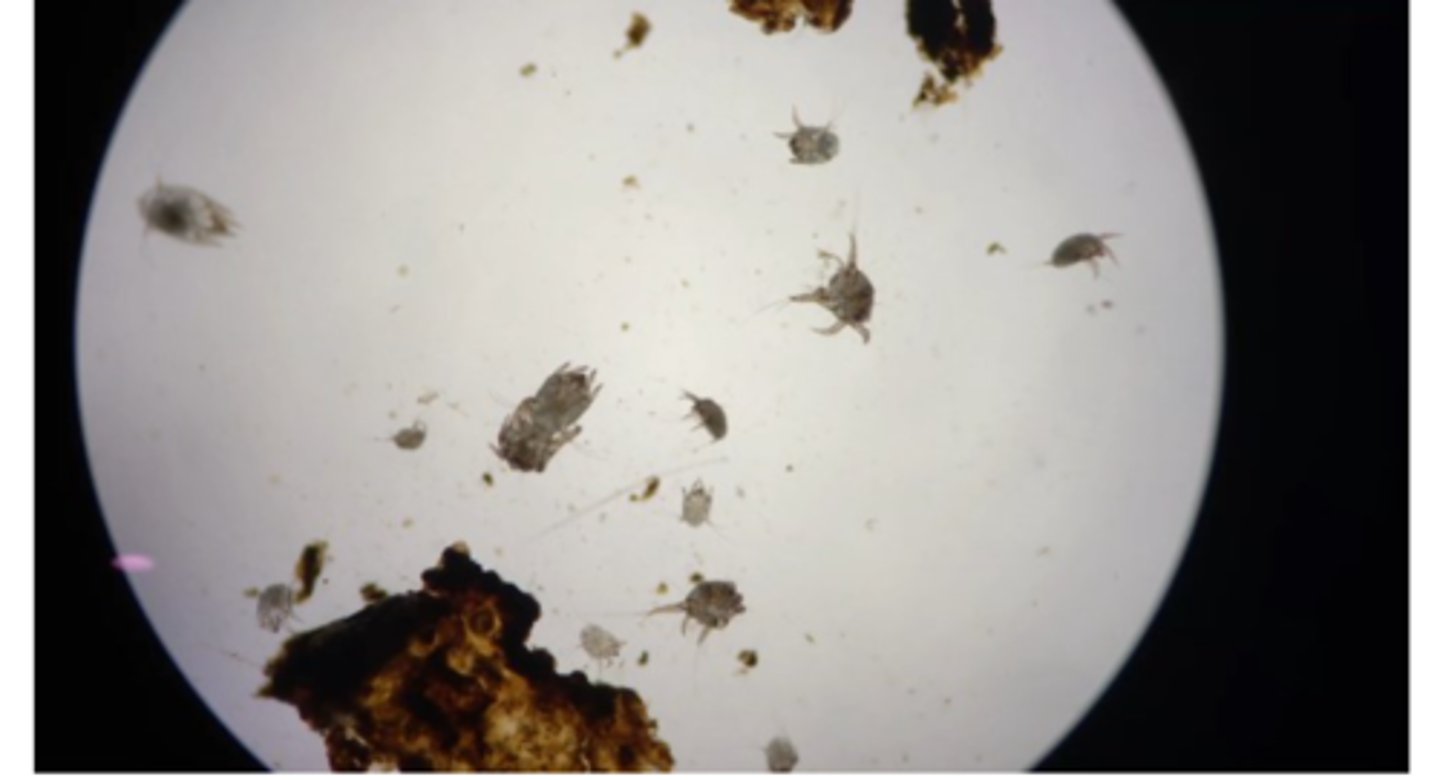
Diagnosis
Clinical signs and history;
Visualization of the parasites in the deep
skin scrapings:
Usually large numbers of mites are found in the scrapings of infested animals

Notoedres cati
Treatment
• All the cats in the household or cattery should be treated;
Clean/remove the bedding;
Supportive therapy;
Antibiotics for bacterial complications;
Bathe the animal with a mild antiseborrheic shampoo to loosen and remove crusts?

Notoedres cati
Treatment- Macrocyclic lactones
• Selamectin (Revolution)
• Moxidectin (Advocate)
Notoedres cati
Treatment- • Isoxazolines
• Esafoxolaner (Nexgard Spectra spot on for cats);
Notoedres cati
Treatment - Bispyrazoles
Tigolaner (Felpreva): a single treatment
recommended by the manufacturer;
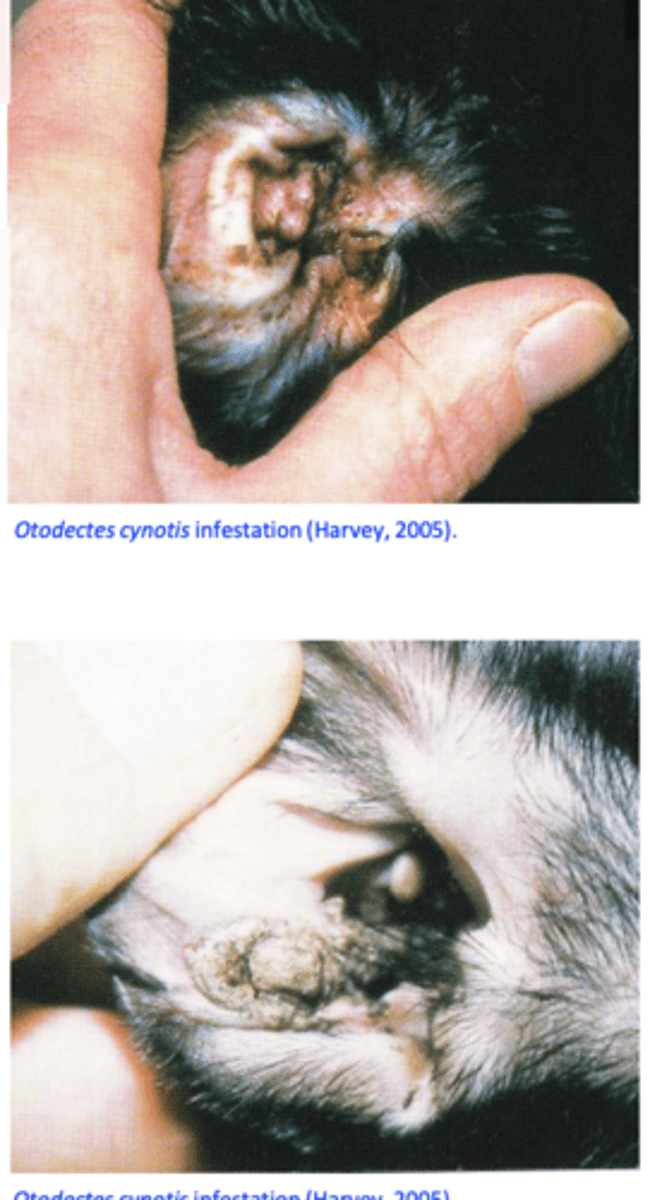
Otodectic mange
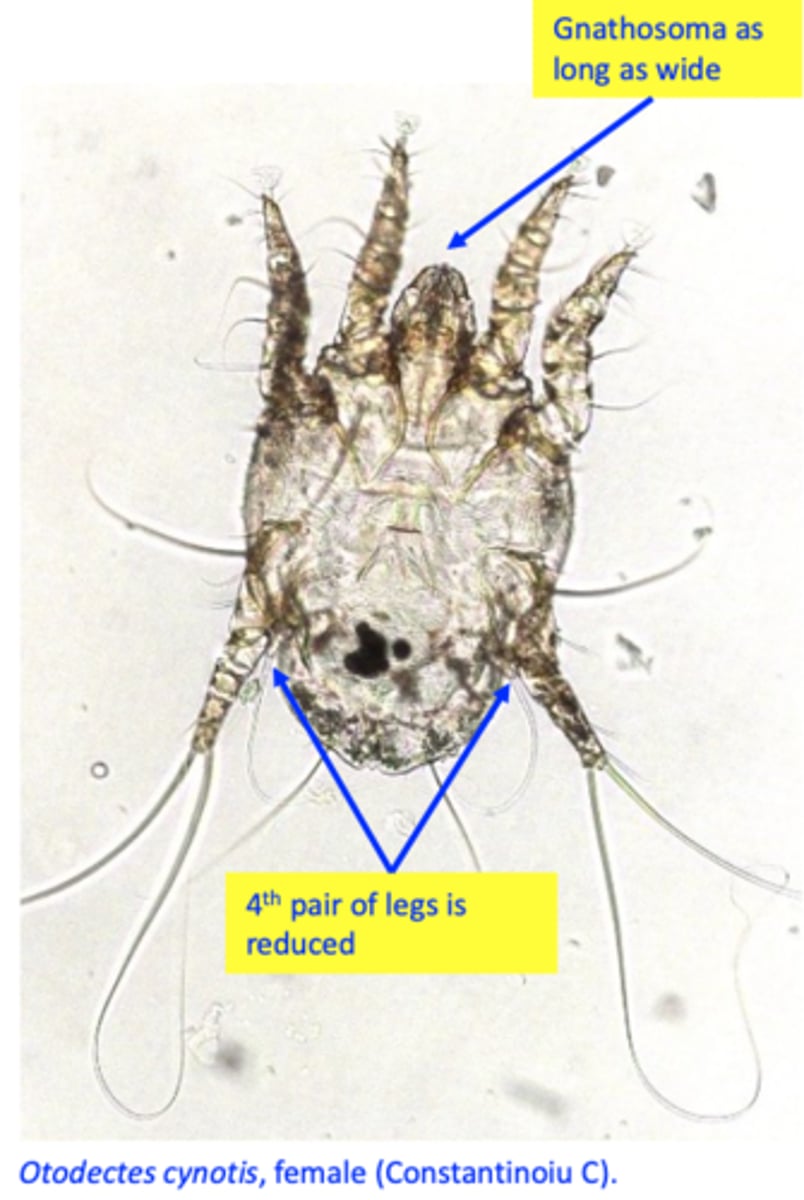
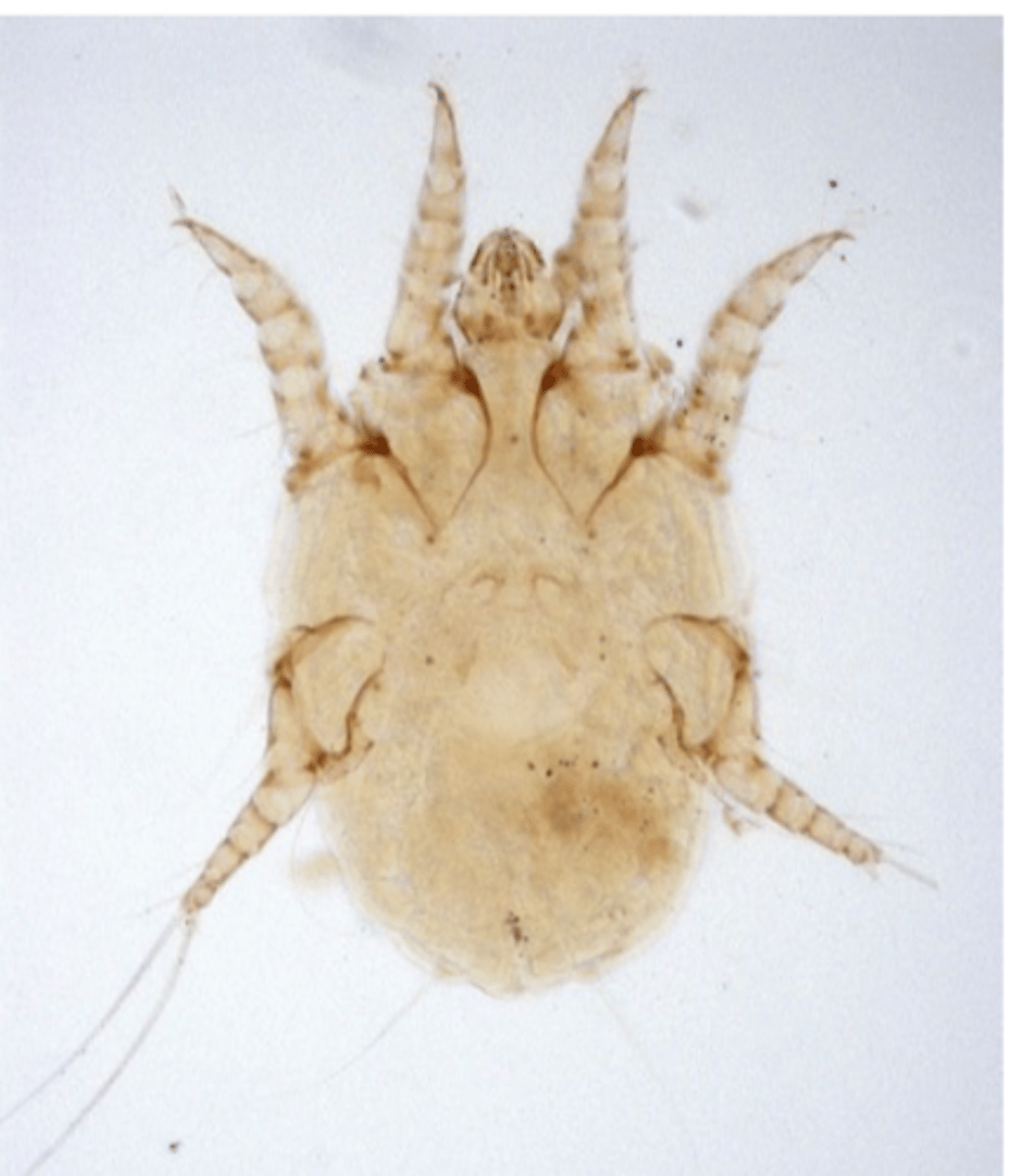
Otodectes cynotis (ear mite)
Hosts: cat, dog, fox and accidentally humans;
Location: external ear canal and adjacent skin of the head.
Morphology
Body: oval;
Gnatosoma: short, length same as width;
Legs: Pairs I and II of similar size and shape, long;
IVth pair is very small (especially in the female);

Otodectes cynotis (ear mite)
Otodectes cynotis (ear mite) Life cycle
Otodectes cynotis does not burrow, it lives on the skin and feeds on the tissue fluids and debris;
Life cycle takes about 3 weeks and it comprises egg (attached by the females to the skin of the ear canal), hexapod larva, two nymphal stages and adults;
Mites locate in the ear canal but in heavy infestations they may be found on the tail, back and head;

Otodectes cynotis (ear mite)
Epidemiology
• Worldwide distribution
Otodectes cynotis is responsible for 50–84% of all diagnosed cases of otitis externa of cat but less than 10% of otitis externa in dogs;
Young dogs and cats appear to be more commonly infested;
Asymptomatic carriers exist;
• Transmission is by direct contact, especially during nursing but also indirect
Otodectes cynotis: Pathogenesis
As few as 3 parasites may cause clinical signs
(difficulties in the diagnosis);
Cats differ in their ability to serve as hosts for O. cynotis
Physical presence of the mite, feeding on the epithelium => mechanical irritation which accounts for some of the pruritus;
Hypersensitivity reaction against saliva, that develops after 2 weeks is responsible for most of the pruritus;
Secondary bacterial infections may occur;

Otodectes cynotis (ear mite)
Clinical signs
Brownish waxy exudate/cerumen in the ear canal that can dry => crusts might develop;
Pruritus => scratching or rubbing of the ears and shaking of the head, hematoma formation, self- trauma;
Otodectes cynotis (ear mite)
Diagnosis
Clinical signs and history;
Microscopic examination of the material collected from the ear canal (ear swabs) => mites, eggs;
• Otoscopy: direct visualization of mites (moving white specks);
• Positive pinnal-pedal reflex (cats): cat moves very quickly the hindlimb when ear canal is massaged/swabbed.

Otodectes cynotis (ear mite)
Treatment
Treat affected animals and all in-contact dogs and cats (inapparent carriers might exist);
Cleaning of the house/place where animals spend most of the time is
recommended
a) Topical otic acaricidal treatments are usually sufficient:
• Macrocyclic lactones
b) Systemic treatments: MLs, Isoxazolines, Bispyrazoles
How many mites of otodectes cynotis to cause clinical signs
3 MITES