Micro 22 | DNA Virus Infections I
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
54 Terms
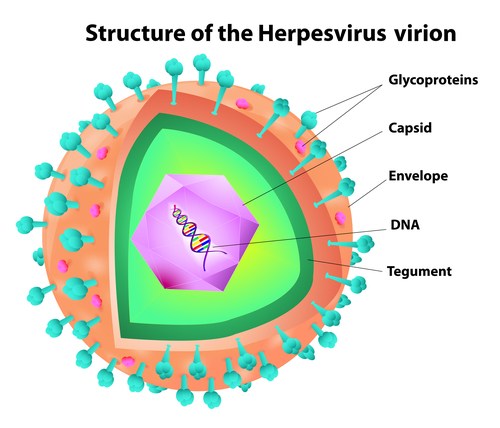
What is the genetic material of Herpesviridae?
Linear double-stranded DNA genome enclosed in an icosahedral capsid.
Why are herpesviruses sensitive to environmental factors?
They are enveloped viruses, making them sensitive to drying, acid, detergents, and solvents, which can disrupt the lipid envelope and inactivate the virus.
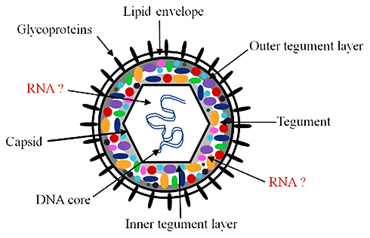
What is the tegument in herpesviruses?
A protein complex found between the viral capsid and envelope, playing a role in viral replication and immune evasion.
How do herpesviruses establish persistent infections?
They can cause both lytic (active replication and cell lysis) and latent (dormant) infections, allowing them to persist in the host and reactivate later.
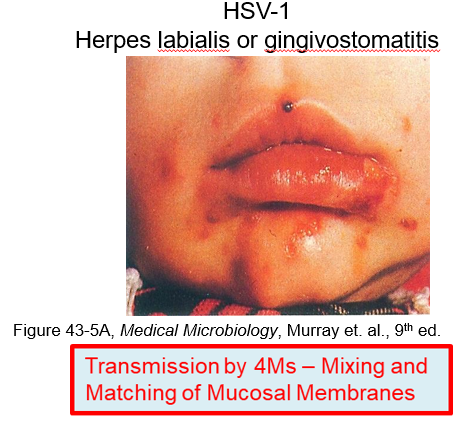
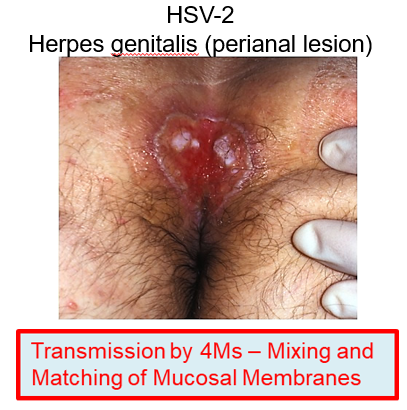
What is the main symptom of HSV-1 and HSV-2 infections?
Painful lesions with virus in vesicle fluid.
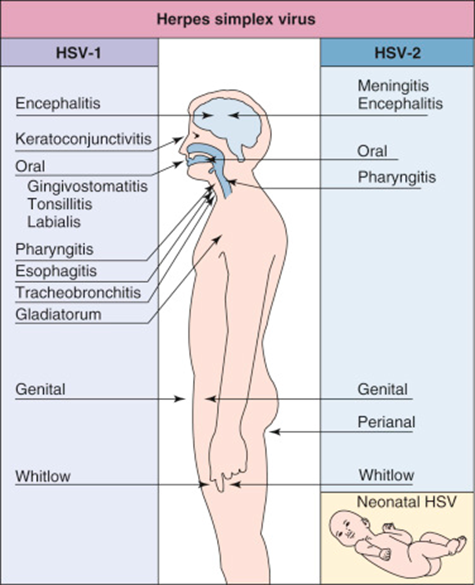
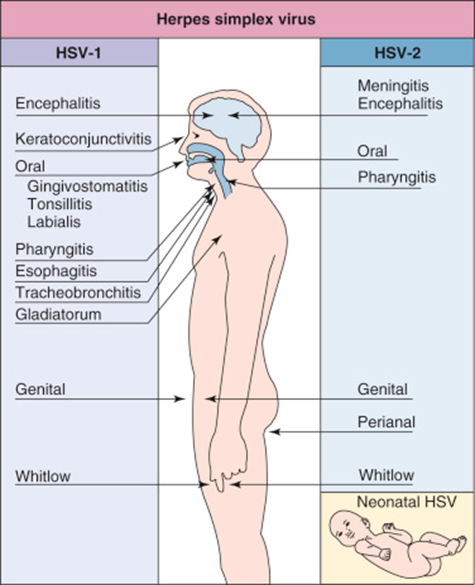
How are HSV-1 and HSV-2 traditionally divided by body location?
HSV-1 typically affects areas above the waist (e.g., oral infections)
HSV-2 is associated with areas below the waist (e.g., genital infections).
How is HSV-1 transmitted?
HSV-1 spreads through oral secretions, kissing, sharing utensils, or skin breaks (e.g., thumb-sucking).
How is HSV-2 transmitted?
HSV-2 is mainly spread through sexual contact via open lesions and genital fluids.

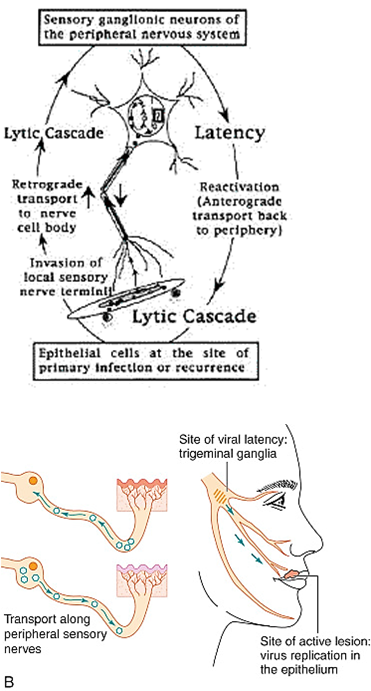
Describe the pathophysiology of HSV-1 and HSV-2
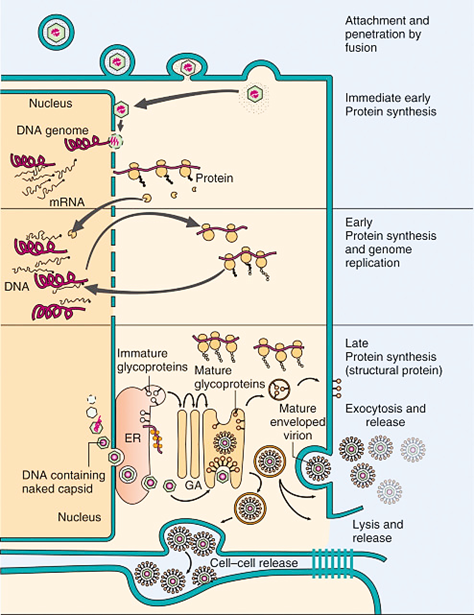
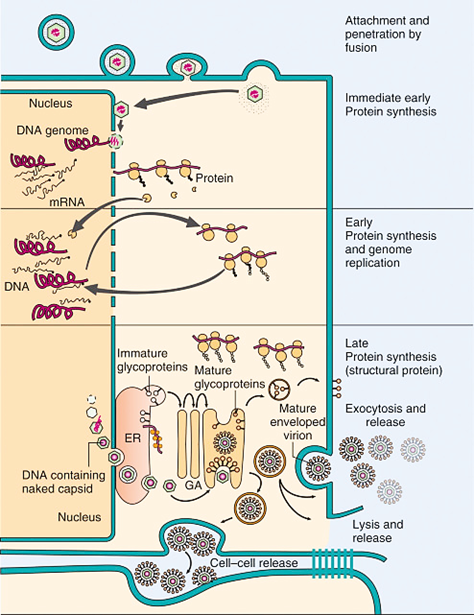
Virus binds to host cell using heparan sulfate and nectin-1 receptors.
Infects mucous membranes or enters through breaks in the skin.
Primary infection occurs, leading to lytic infection at the site of entry.
Direct cytolysis of infected cells causes vesicular lesions.
Immune response activates, and CD8 T cells contribute to tissue destruction.
Lesions heal, progressing from vesicle to crusty scabs.
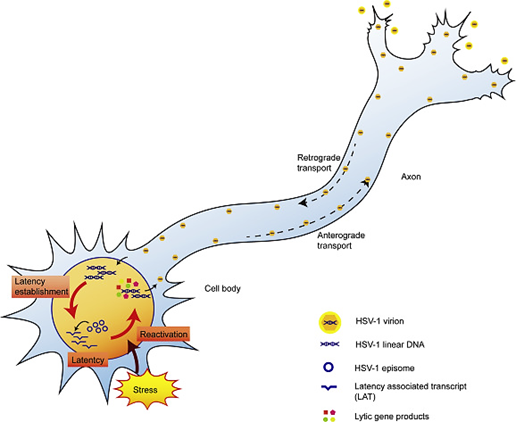
Virus establishes latency in neurons instead of being eliminated.
Reactivation occurs under certain conditions (e.g., stress, illness).
Virus travels back to the initial site of infection, causing symptoms again.
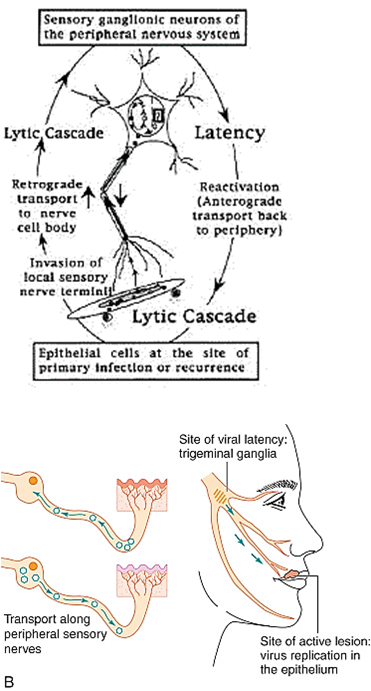
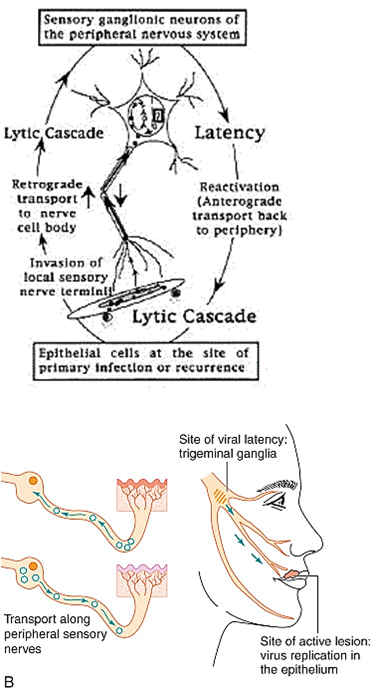
How does HSV-1/2 establish latency in the body?
HSV-1/2 travels retrograde to sensory ganglia, where it remains dormant.
Oral herpes establishes latency in the trigeminal ganglia
Genital herpes resides in the sacral ganglia.
What is asymptomatic shedding in HSV?
Occurs when HSV reactivates and spreads without causing symptoms, allowing transmission to others.
What are some common triggers for HSV-1/2 reactivation?
Reactivation can be triggered by physical stress (fever, menstruation), environmental factors (UV exposure, spicy/acidic foods), and immunosuppression (HIV, chemotherapy, radiotherapy).
What happens during HSV-1/2 reactivation?
LATs are downregulated, allowing viral replication to resume. The virus spreads anterograde along nerves to peripheral tissues, causing lesions at the site of primary infection.
How does recurrent HSV disease differ from primary infection?
Primary infection has a longer prodrome, more severe systemic symptoms, and prolonged local symptoms.
Recurrent disease is typically shorter and milder.
Why does HSV recur at the same site?
The virus remains latent in sensory ganglia and travels along the same nerve to the original site of infection when reactivated.
What causes lesions in HSV-1/2 disease?
Lesions result from direct tissue damage caused by lytic infection and the host immune response.
What immune cells are important in controlling HSV-1/2 infection?
CD8 T cells and Th1 CD4 T cells
How is HSV-1/2 diagnosed?
Clinical appearance and patient history
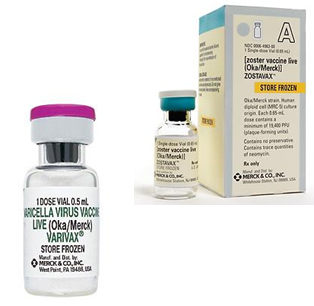
Cytopathic effects in skin scraping, including:
Tzank stain or Papanicolaou smears
Cowdry type A bodies – acidophilic intranuclear inclusion bodies with a ring of condensed chromatin
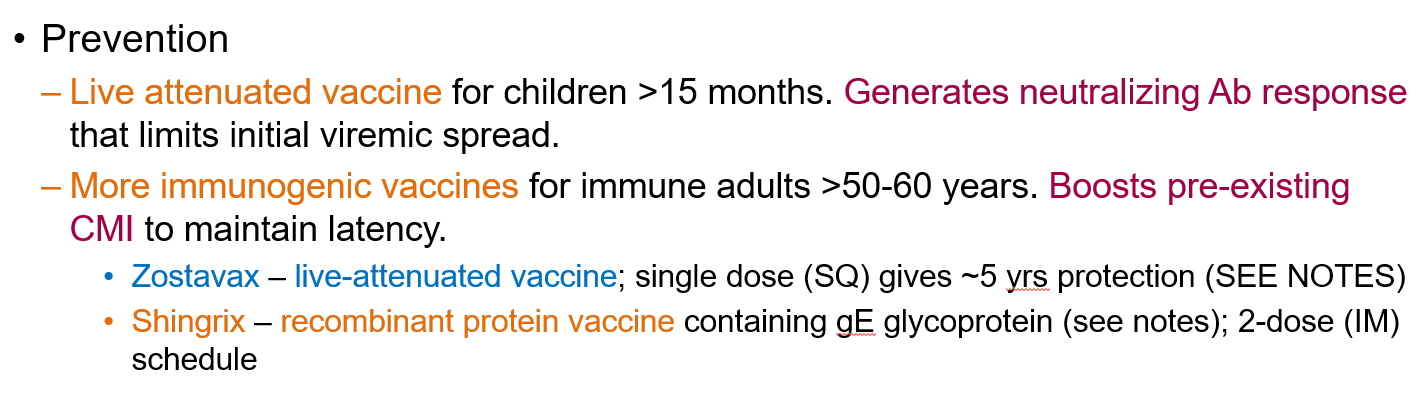
Syncytia formation – multinucleated giant cells aiding in viral dissemination and immune evasion
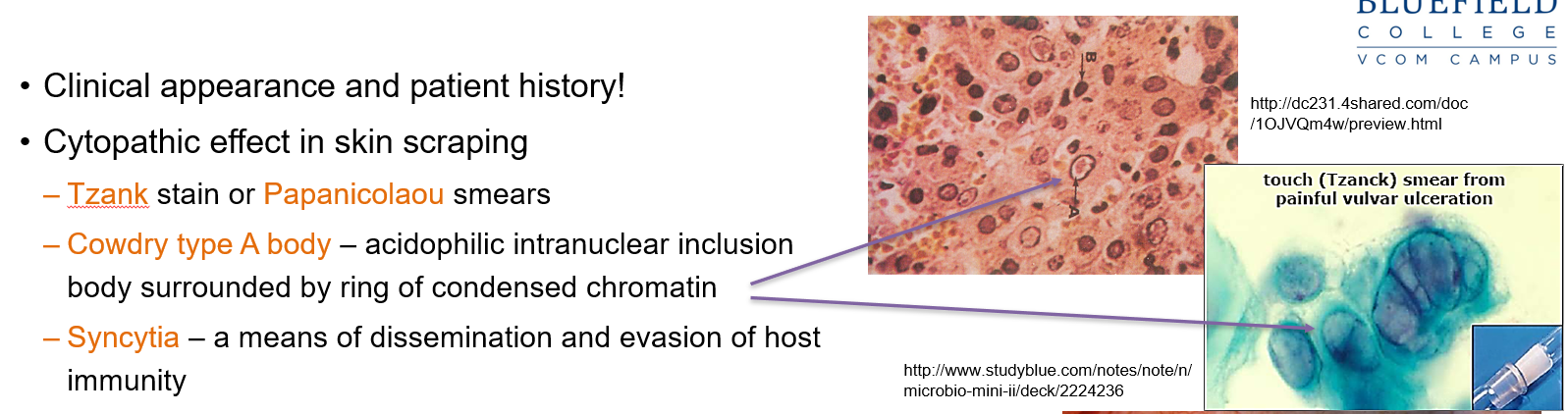
What stains are used for detecting HSV-1/2 in skin scrapings?
Tzanck stain and Papanicolaou smears are used to detect cytopathic effects.
What is a Cowdry type A body?
An acidophilic intranuclear inclusion body surrounded by condensed chromatin, seen in HSV infections.
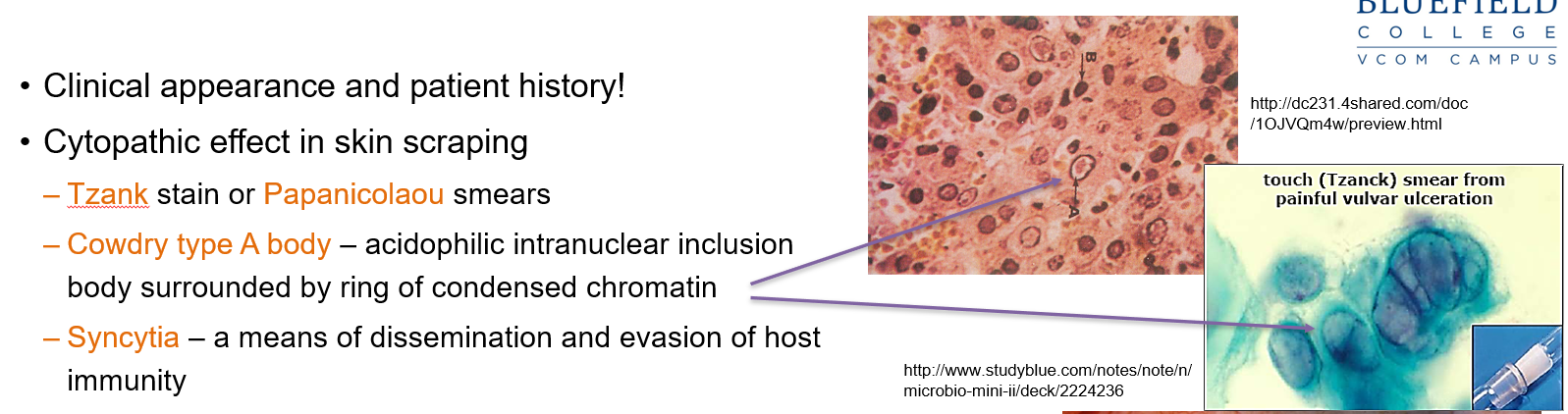
What role do syncytia play in HSV-1/2 infection?
Syncytia help the virus spread between cells and evade the host immune system.
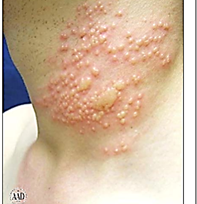
Which Herpes variant is this?
Herpes gladiatorum – occurs on the skin, often in athletes.

Which Herpes variant is this?
Herpetic whitlow – affects the fingers.
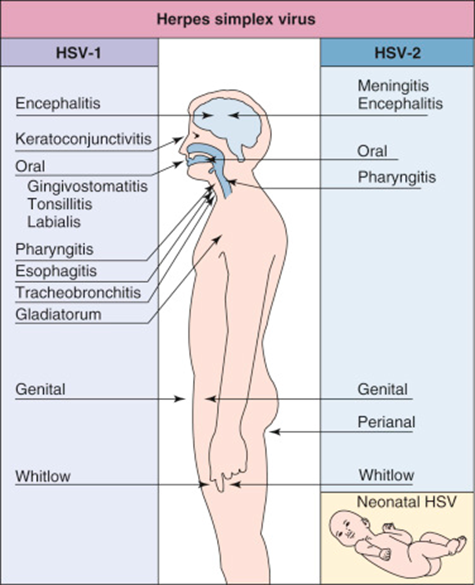
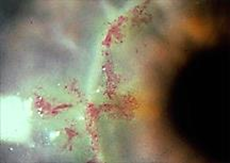
Which Herpes variant is this?
Herpetic keratitis/keratoconjunctivitis – affects the eyes.
What is the general rule for HSV recurrence?
Recurrent HSV infections occur at the original site of infection.
How is congenital herpes simplex infection transmitted?
Usually transmitted during childbirth through contact with infected genital secretions, but in utero transmission can also occur in rare cases.

Why is screening important for congenital herpes simplex infection?
Because the mother may not show symptoms, leading to undetected transmission of HSV to the neonate, which can cause severe disease.

How does acyclovir work against herpes viruses?
Acyclovir is a nucleoside analog that is phosphorylated by viral TK (but not by the host cell's TK), allowing it to inhibit viral DNA polymerase and prevent replication.
Can herpes virus infections be cured with treatment?
No, treatment like acyclovir controls the infection by limiting viral replication, but it does not cure herpes virus infections.
What is the primary infection caused by VZV?
Varicella, aka chickenpox.
What is the recurrent disease caused by Varicella Zoster Virus?
Herpes zoster, also called shingles.
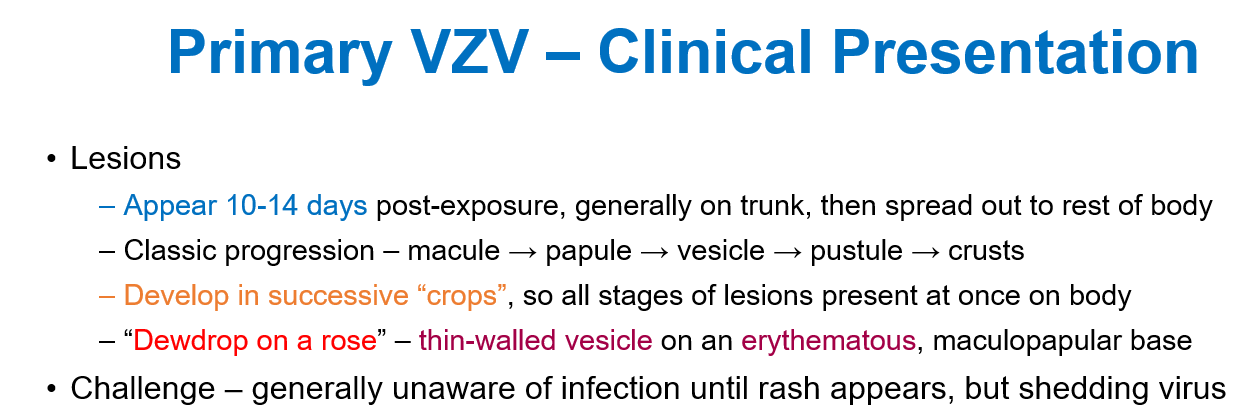
How does Varicella Zoster Virus spread in the body?
It spreads through the lymphatic system and bloodstream, causing a rash. The virus is also present in vesicles.
Transmission of Varicella Zoster Virus?
Through respiratory secretions before the onset of symptoms
From lesion secretions via direct contact or inhalation of aerosolized secretions (vescicles)
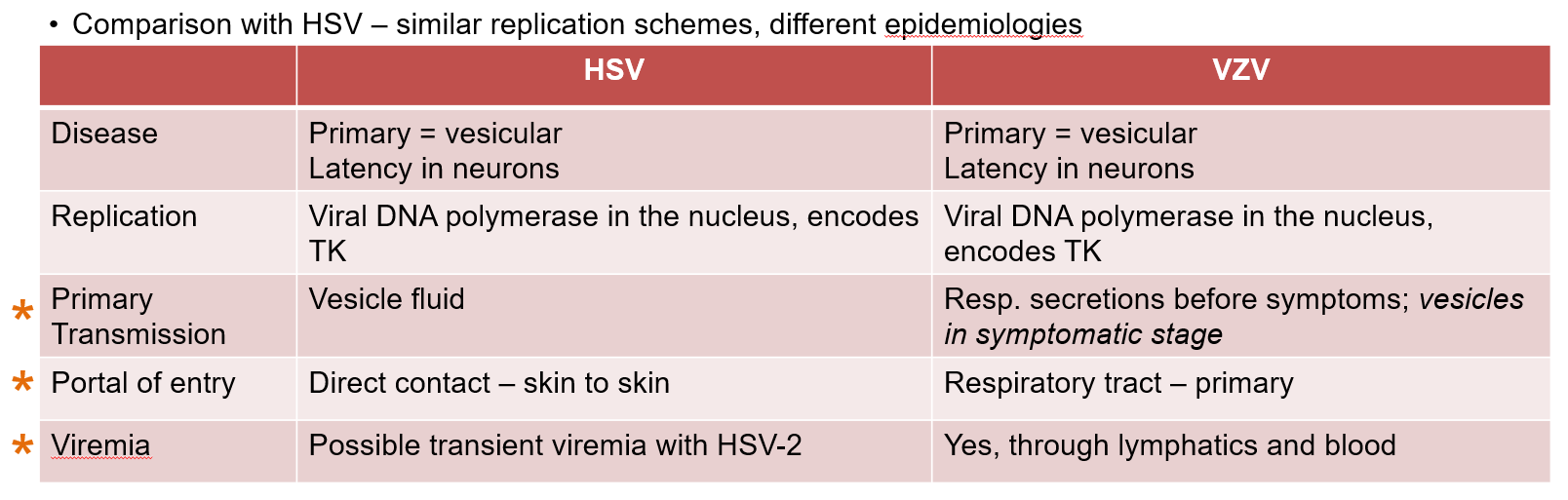
Portal of entry of Varicella Zoster Virus
Respiratory tract
Does Varicella Zoster Virus travel through the blood?
Yes, through lymphatics and blood
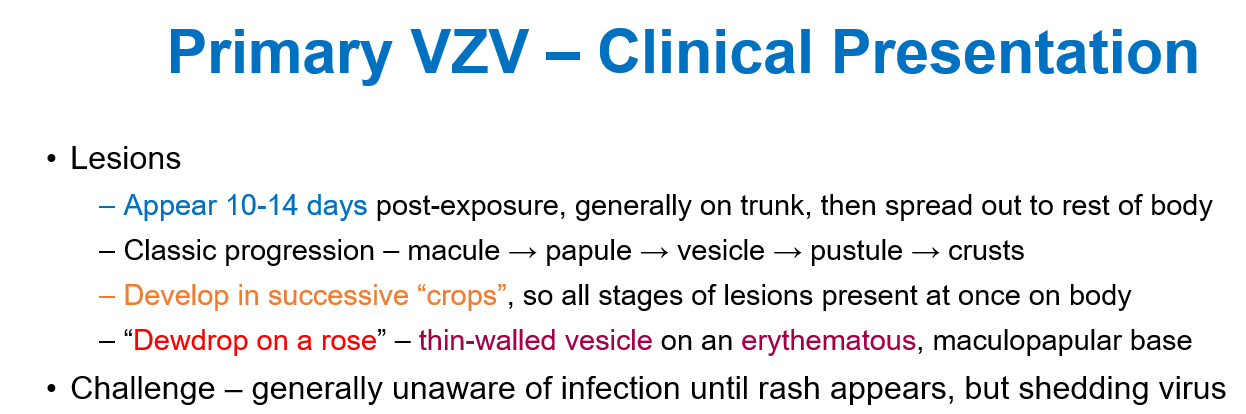
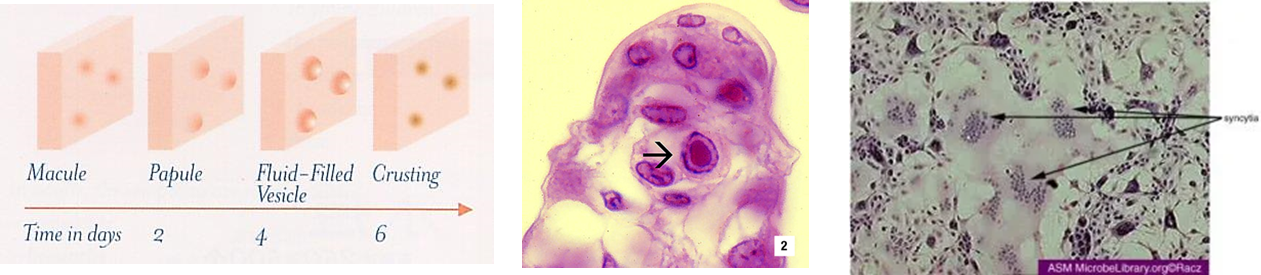
Clinical Presentation of Primary Varicella Zoster Virus
"Dewdrop on a rose"
A clear, fragile blister sitting on top of a small red bump on the skin.

How do the lesions of Varicella Zoster Virus develop?
Lesions develop in successive “crops”, meaning different stages of lesions are present at the same time on the body.

How does Varicella Zoster Virus spread within the body?
From the skin and mucous membranes, the virus spreads to neurons and establishes latent infection in the nervous system.
What disease results from the reactivation of latent Varicella-Zoster Virus?
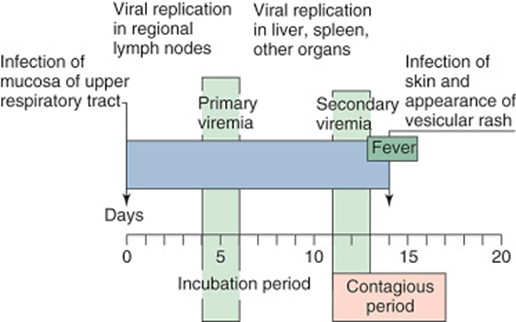
Herpes Zoster, also known as shingles.
It usually happens many years after the primary infection (chickenpox).

Which structure does Varicella Zoster Virus stay dormant in the body?
In the dorsal root ganglia

When does VZV reactivate and cause shingles?
When cell-mediated immunity weakens and there are insufficient CD8+ T cells to keep the virus in check.
Clinical Presentation of Shingles (Herpes Zoster)?
It begins with sharp, tingling pain along a dermatome innervated by the infected nerve.
Followed by the eruption of a “belt” of maculopapular lesions with a red base, resembling chickenpox.
The lesions typically progress along a single dermatome.
Why is shingles sometimes described as a “belt” of lesions?
Because the rash wraps around the body in a band-like pattern, especially in the thoracic region, where it follows the path of the infected nerve.

Which immune cells are important for controlling Varicella Zoster Virus?
CD8 T cells and IFN-γ help control the virus, maintain latency, and kill infected cells.
How is Varicella Zoster Virus diagnosed?
By symptoms because the rash and presentation of chickenpox and shingles are very characteristic.
Also can be confirmed by CPE (cytopathic effect), such as finding Cowdry type A intranuclear inclusion bodies and syncytia in skin scrapings, similar to how Herpes Simplex Virus is diagnosed.
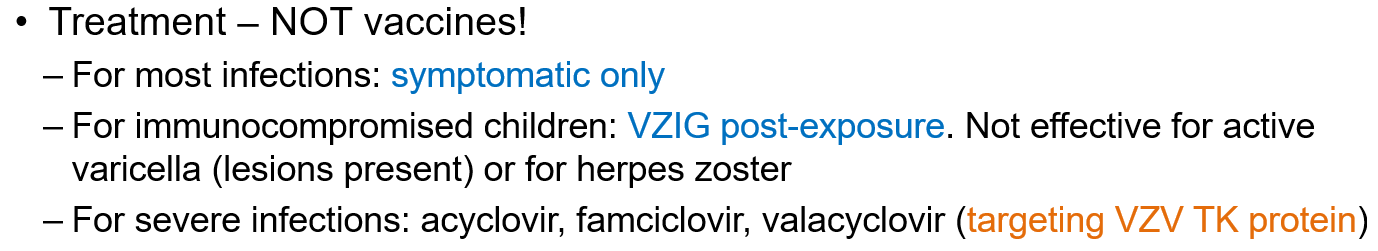
How can Varicella Zoster Virus be prevented?
Vaccination is the main prevention method.
Live attenuated vaccine for children over 15 months, which generates neutralizing antibodies to limit virus spread.
Immunogenic vaccines: Shingrix, a recombinant protein vaccine
How is Varicella Zoster Virus treated?
With antivirals like acyclovir, famciclovir, or valacyclovir that target the VZV TK (thymidine kinase) protein.
What disease is caused by HHV-6 and HHV-7?
Exanthem subitum, aka roseola

How is HHV-6/HHV-7 transmitted?
Through saliva.
What cells do HHV-6/HHV-7 target?
They initially replicate in the salivary gland.
Then spread to T cells, especially CD4 T cells, where they can set up latent infection.
How is HHV-6/HHV-7 infection controlled?
By cell-mediated immunity
How does HHV-6 disease progress?
Starts with high fever (103-105°C) that can trigger seizures in 20-25% of children.
Fever lasts several days, followed by a sudden return to normal temperature.
Diffuse macular rash appears after the fever resolves, often spreading over the body.
What is the most common cause of febrile seizures in children?
HHV-6
How does HHV-7 disease compare to HHV-6?
HHV-7 usually causes a milder disease than HHV-6.