Climate change - heat
1/28
Earn XP
Description and Tags
Overview of how climate change affects human health • Specific focus on human health consequences related to heat • Characterisation of physiological response to heat • Impact of age on thermoregulation
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
29 Terms
Climate change vs global warning
Climate Change = long-term changes in average weather patterns, including rising sea levels, extreme weather events, droughts, and shifting ecosystems.
Global Warming = a consequence of climate change, describing the long-term warming of Earth's surface temperature due to human activities like greenhouse gas emissions.
In essence:
🔹 Climate change = broad pattern of environmental shifts
🔹 Global warming = specific trend of rising temperatures
List health outcomes (9) and impact on health system & facilities (2) from climate change

What is the significance of the 1.5°C threshold in climate change? (4)
The 1.5°C threshold = the goal of limiting the rise in global average surface temperature to no more than 1.5°C above pre-industrial levels (circa 1900)
(It was established in the 2015 Paris Agreement, signed by 195 countries)
Exceeding this threshold increases the frequency, severity, and unpredictability of climate-related hazards like:
🌡 Heatwaves
🌊 Sea level rise
🌾 Food insecurity
🦟 Spread of vector-borne diseases
Although 1.5°C still brings risks, it is considered a "slower" rate of change, giving nations more time to adapt and reduce long-term harm.
🌡 In 2023, temperatures temporarily approached this limit—raising concern that we’re nearing critical tipping points earlier than predicted
Direct effects on how heat effects health? (4)
Heatstroke, hospitalisations, and death
(Especially in vulnerable populations)
Exacerbation of pre-existing conditions like cardiovascular disease, asthma, and diabetes, anxiety, PTSD
Severity of asthma can be worsened by pollen → more flares
Older adults have reduced sweating, weaker thermoregulation, and more inflammation, increasing risk
Poor sleep due to high night-time temperatures
Mental health issues like anxiety and PTSD (especially from climate displacement)
Physiological strain: increases heart rate, vasodilation, sweating → dehydration, hyperosmolarity, hypovolemia (low blood volume), kidney strain via RAS activation
Indirect effects on how heat effects health? (7)
Spread of vector-borne diseases (e.g., mosquitoes migrating to new areas)
Disruption to health services (overwhelmed) and critical infrastructure & technology (eg power cuts affecting cooling systems in heatwaves)
Increased pollen due to longer growing seasons → worsens asthma and allergies
Urban heat island effect intensifies city temperatures
Dehydration and cardiovascular strain from repeated heat exposure
Ecosystem damage (eg drought, poor air quality, fire)
Impacts related to changes in behaviour eg increased accidents risk
How can extreme heat lead to behavioural changes that increase health risks? (5)
Extreme heat can impair cognitive and physical functioning, leading to:
Increased risk of accidents due to fatigue, dizziness, or reduced concentration
Irritability or aggression
Reduced physical performance or poor decision-making (especially in outdoor workers)
Avoidance of outdoor activity → impacts physical & mental health
Disruption of sleep → contributes to chronic stress, anxiety
What is a heatwave? (4)
A period of abnormally hot weather lasting several days, where both the maximum daytime temperature and the minimum night-time temperature remain unusually high for a region.
There's no universal definition, but it's broadly accepted that:
➤ High daytime temperatures + elevated night-time temperatures = heatwave.The lack of cooler nights leads to heat build-up and increases the risk of heat-related illnesses.
Heatwaves vary by region, depending on what's considered 'normal' temperature there.
How do night temperatures affect health?
High night temperatures prevent the body from cooling down, leading to cumulative heat stress.
Without cooler nights, core body temperature stays elevated, increasing the risk of heat-related illness, especially in vulnerable groups (elderly, those with chronic illness).
Prolonged heat exposure without recovery increases the risk of heatstroke, cardiovascular strain, and death.
Sleep quality is reduced, which affects immune function, mental health, and increases risk of chronic diseases.
Heatwaves are defined not just by high daytime temps but also persistently high minimum temperatures.
How does increased heat from climate change affect morbidity and mortality? (5)
Heatwaves are increasing in frequency and severity due to climate change.
This is linked to higher morbidity (illness) and mortality (death), especially during temperature extremes.
Relative risk of death rises steeply with temperatures above local norms (e.g., >28°C in Paris, >30°C in São Paulo)
(UK projections: 7,000 heat-related deaths/year by 2050; 1 in 5 homes expected to overheat)
Heat affects vulnerable populations more (e.g., elderly, those with chronic illness).
Physiological stress from heat (e.g., dehydration, cardiovascular strain) contributes to these outcomes.
What factors influence the amount of heat stored in the body during hot weather? (4)
Inability to eliminate internally generated heat from metabolic processes (e.g. physical activity like exercise).
Clothing, which acts as a barrier to heat loss, trapping heat against the skin.
External environmental heat gain, which adds to the body’s heat load (e.g. hot temperatures or being outdoors in the sun).
➡ These factors can exceed the body’s natural thermoregulatory capacity (sweating and vasodilation), especially in vulnerable groups like the elderly, pregnant women, or outdoor workers — leading to increased heat stress, morbidity, and mortality.
What physiological factors (4) and exposure factors (4) increase vulnerability to heat-related health risks?
▶ Physiological Factors (from slide + transcript):
Older and less-abled people – reduced sweating, lower cardiac output, poor thermal perception.
People with medical conditions or on certain medications – especially cardiovascular or renal diseases.
Pregnant people – particularly vulnerable due to changes in circulation and fluid balance.
Infants and children – underdeveloped thermoregulatory systems.
▶ Exposure Factors (from slide + transcript):
Outdoor and manual workers – prolonged heat exposure increases risk.
People in sub-par housing or without cooling – heat builds up, especially during warm nights.
Those who are poor, displaced, or experiencing homelessness – lack protective infrastructure.
Athletes and attendees of outdoor events – physically active in heat increases internal heat load.
🧠 These factors make it harder to thermoregulate, increasing the risk of heat exhaustion, heat stroke, and cardiovascular strain
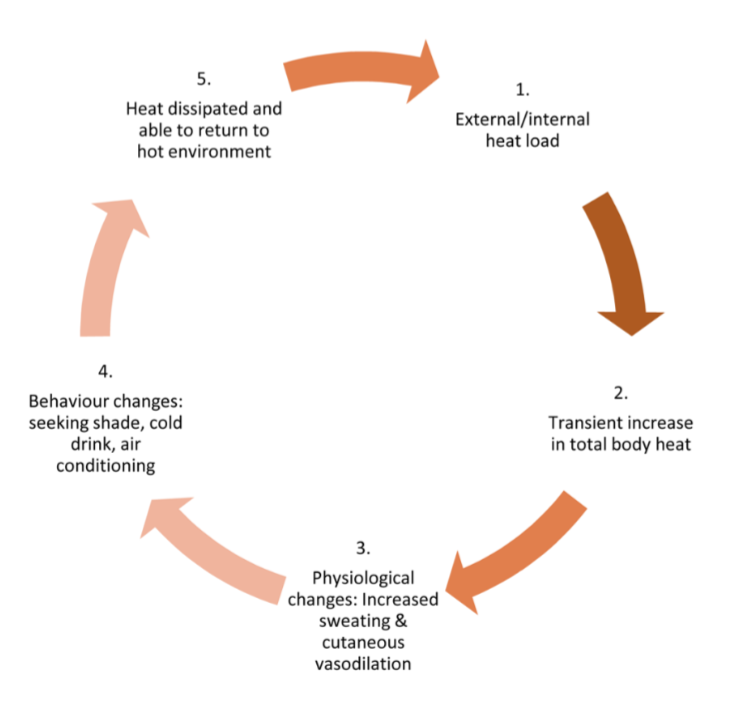
Our responses to heat (3)
Body responds to heat stress approx 45 minutes after exposure (increases if metabolic heat stress such as exercise), (Body takes ~45 mins to mount a heat stress response, longer during exertion)
Behavioural responses - alter behaviours to adapt to heat (eg seeking shade, increase hydration)
Physiological responses - finite response to heat; body is limited in what it can do to maintain thermoregulation; no conscious effect
Eg: Sweating, cutaneous vasodilation
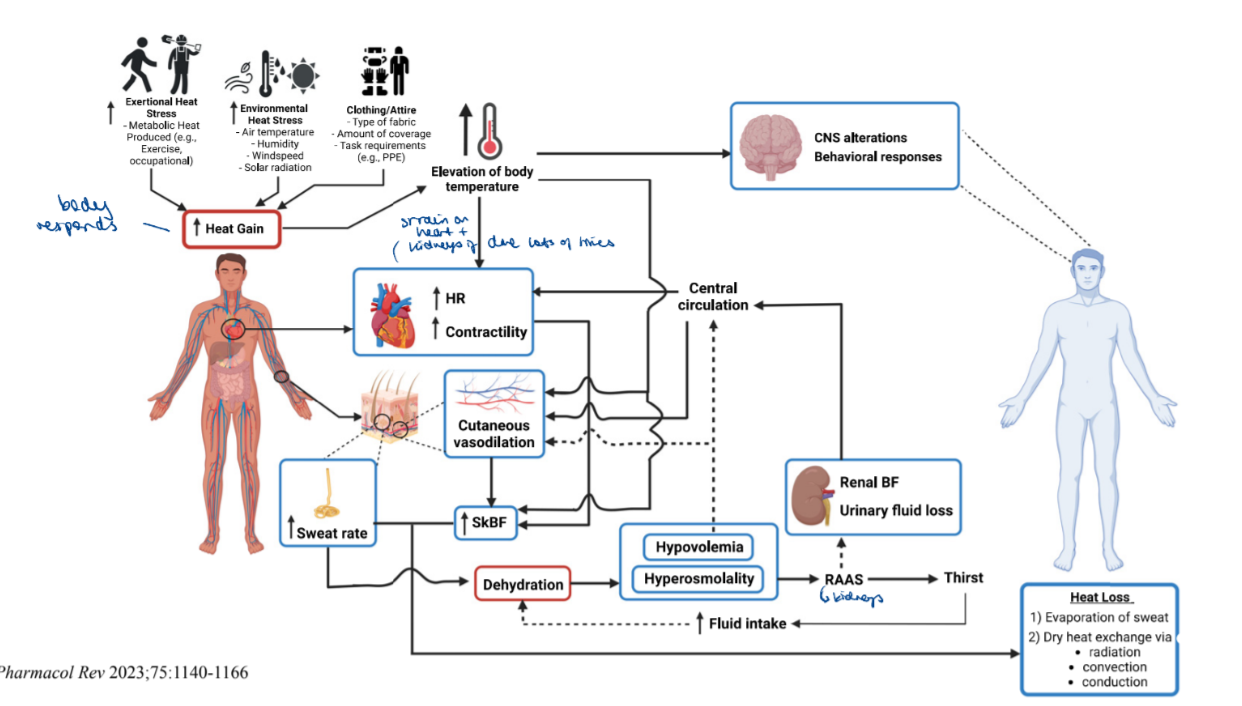
How does the body physiologically respond to heat exposure, and what mechanisms regulate this response? (4)
The internal body temperature is maintained around 37°C, which is optimal for enzymatic reactions.
Body temperature is regulated by homeostatic mechanisms controlled by the hypothalamus.
We gain heat from:
The environment
Internal tasks such as metabolic rate
Clothing, which creates a barrier to heat loss
Skin temperature plays a key role by sending afferent and efferent signals that activate:
Behavioural, neural, and biophysical heat exchange responses (e.g., sweating, vasodilation).
Explain the body’s physiological (thermoeffector) responses to heat? (4)
The body activates thermoeffector responses to lose excess heat and maintain homeostasis:
Sweating – evaporative cooling mechanism that helps release body heat.
Cutaneous vasodilation – blood vessels dilate to increase blood flow to the skin.
Leads to ↓ central blood volume, redistributing blood away from internal organs to skin for heat dissipation.
↓ Renal blood flow – activates the RAAS (Renin-Angiotensin-Aldosterone System), inducing thirst and conserving fluid to maintain blood pressure.
Dry heat loss mechanisms – through conduction, convection, and radiation.
🔁 These responses are finite, and excessive or prolonged activation increases cardiovascular strain, especially in vulnerable groups (from transcript).
List processes of heat gain (4) and heat loss (3)
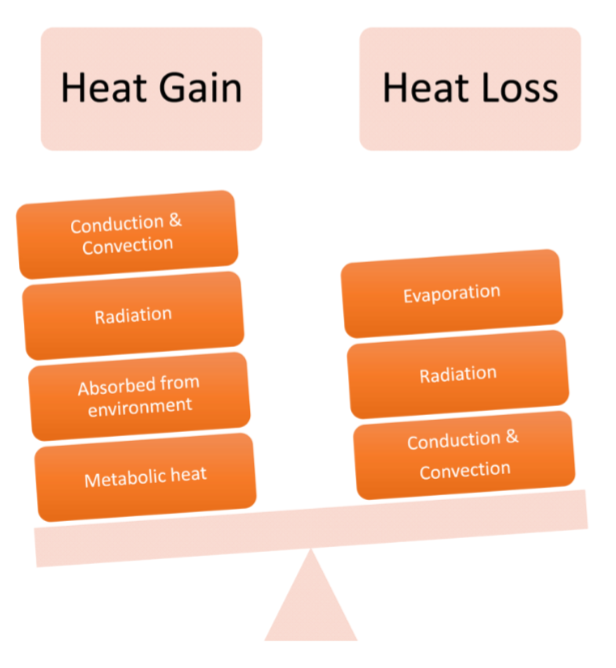
Explain 4 modes of heat transfer (6)
Conduction: Body touching solid mass (e.g. hot sand vs ice pack)
Convection: media carries heat between body and temperature (e.g. airflow, radiator)
Radiation: infrared portion of energy carries warm energy
Rate of absorption directly correlated to difference in temperature between skin and environment (the amount of energy absorbed depends on the temperature difference between your body and the environment)
Evaporation: removal of heat through liquid (e.g. sweat).
Proportional to water vapor-pressure gradient between skin and environment (the drier the air, the more efficiently your sweat evaporates)

How is thermoregulation controlled in response to heat stress? (8)
Thermoregulation is controlled by a negative feedback loop regulated by the hypothalamus.
When body temperature exceeds 37°C, nerve cells in the skin and brain detect the change.
Skin temperature activates afferent & efferent signals to hypothalamus → drives neural, behavioural, and biophysical mechanisms
The hypothalamus activates heat-loss responses:
Sweat glands secrete sweat → heat loss by evaporation.
Vasodilation of skin vessels → heat dissipates via radiation, convection, and conduction.
These responses reduce body temperature, restoring homeostasis.
Prolonged activation leads to CV strain (↑HR, ↓central volume) and renal compensation via the RAAS pathway (↑thirst, ↓urine).
What physiological changes occur during prolonged heat exposure? (5)
↑ HR and contractility.
↑ Sweat rate, leading to dehydration.
↑ Cutaneous vasodilation, shifting blood to the skin.
↓ Renal blood flow, activating RAAS to preserve fluids.
Can result in hypovolemia, hyperosmolality, and strain on heart and kidneys
(Physiological responses to heat are limited and must be supported by behavioural changes such as seeking shade or increasing fluid intake.)
Why Chronic Exposure is Harmful?
Prolonged activation of sweat and vasodilation → persistent CV and renal strain, not sustainable long term
Hypovolemia meaning, cause, what happens in heat (3)
A state of low blood volume, especially plasma volume (the liquid part of blood).
Cause: Often due to excessive sweating, dehydration, or bleeding.
In Heat:
Cutaneous vasodilation and sweating reduce central blood volume
Leads to lower perfusion to vital organs if not corrected
Hyperosmolality meaning, cause, in heat (3)
Definition: An increased concentration of solutes (like sodium) in the blood due to loss of water.
Cause: Loss of more water than solutes — e.g. through sweating without adequate fluid intake.
In Heat:
Triggers thirst
Signals the release of ADH to conserve water by the kidneys
RAAS meaning
Renin–Angiotensin–Aldosterone System
A hormone system that helps regulate blood pressure, fluid, and electrolyte balance
Activated when body detects low BV or sodium
2 main types of sweat glands
4 million sweat glands in skin – eccrine and apocrine
Eccrine sweat gland structure and function (7)
Tightly coiled tube in dermis or hypodermis
2 types of cells:
Clear/secretory cells: watery component of sweat
Dark cells: secrete glycoproteins
Sweat produced in coiled tube, travels through duct and duct opens at skin surface, exits through pore
Surrounded by myoepithelial cells that push sweat through duct
Controlled by cholinergic sympathetic nerves releasing acetylcholine, triggered by a rise in core body temperature.
Activation results in evaporative cooling, helping maintain homeostasis during heat stress.

Apocrine sweat glands structure and function (5)
Larger, deeper glands with a glomerulus secretory tubule in subcutaneous fat
Produces thicker, milkier form of sweat containing proteins and lipids
This sweat is odourless until broken down by skin bacteria, causing body odour
Typically associated with hair follicles
Controlled by adrenergic nerves that release norepinephrine in response to hormonal or emotional stimuli (eg stress, anxiety, puberty), not heat
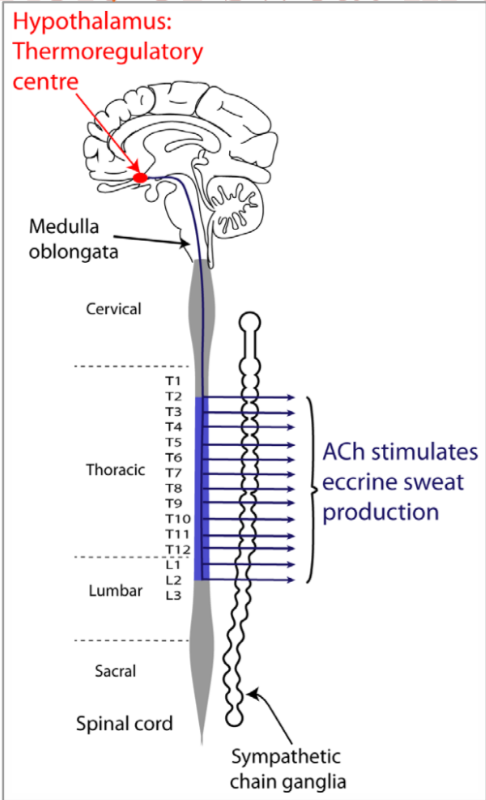
Neural Pathway of Sweat Secretion in Thermoregulation
How is sweat secretion triggered in response to heat? (5)
Thermoreceptors in the skin and CNS detect an increase in body temperature.
This activates the thermoregulatory centre in the hypothalamus.
Signals travel via the medulla oblongata to sympathetic ganglia in the spinal cord.
Post-ganglionic sympathetic nerves release acetylcholine (ACh).
ACh binds to muscarinic receptors on eccrine sweat glands, triggering sweat secretion.
How does thermoregulation ability change with age? (7)
These factors heighten vulnerability to what? (5)
Adults >50 years old store 1.3 – 1.8 times more body heat than young adults
Reduced sweat gland function: Sweating capacity and skin blood flow reduce with age
Smaller, shallower, and more coiled sweat glands reduce sweat output
Decreased skin blood flow: Impairs heat dissipation via vasodilation.
Cardiovascular decline: CV stress with age - decrease in total blood volume, ROS and NO availability decreases. Reduced cardiac output limits blood redistribution.
Heat exposure strains this system
Increase in basal inflammation in aging, alterations in gut microbiome and health - alters homeostatic mechanisms
Decreased renal function: Impairs fluid balance and RAAS response
Diminished thirst perception: Increases risk of dehydration
These factors heighten vulnerability to heatstroke, MI, thrombosis, AKI, and other heat-related illnesses

More effects of age on thermoregulation

How do sweat glands in thermoregulation change with age? (4)
Sweat gland number and volume: No significant difference in sweat gland density or volume between younger and older adults (abdominal skin).
Gland structure changes:
Older adults have shallower secretory ducts due to thinner dermis.
Increased tortuosity (coiling and twisting of ducts).
Greater rotation angle from the skin surface.
Functional impact: These morphological changes may impair efficient sweat delivery and reduce heat regulation capacity with age