Digestion physiology and metabolism
1/294
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
295 Terms
What are the utmost basic steps to the digestive process?
1) ingestion - food taken in
2) digestion - food broken down
3) absorption - nutrients absorbed
4) elimination - waste removed
What determines the differences in the structure of the gastrointestinal tract and what types are there?
shaped by the food types that the animal have been evolved to ingest
1) herbivores - eat plant material, ruminants=cattle and goats, non-ruminants=horses
2) carnivores - eat meat, cats
3) omnivores - eat combination of plants and meat, humans, pigs, (dogs)
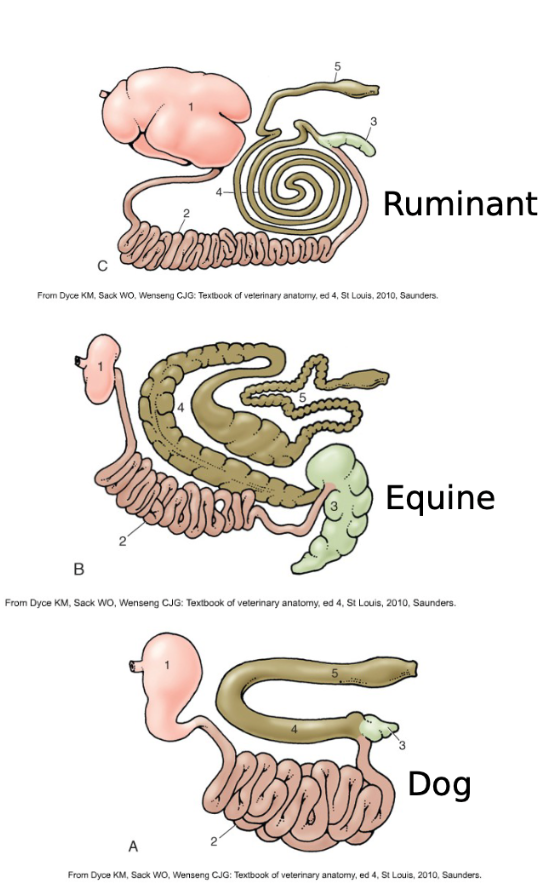
what are some characteristics of carnivores?
shearing teeth, large capacity dilatable stomach, short and simple digestive tract
what are some characteristics of herbivores?
“grinding” teeth, smaller true stomach and adaptations for fermentation, starches proteins and lipids digested normal (EXCEPT in ruminants), cellulose-needs fermentation by microbes, ruminants=fermentation in fore stomach, horses and rabbits=fermentation in mid and hindgut
what are some characteristics of omnivores?
both cutting and grinding teeth, relatively long gastrointestinal tract modified by domestication
What is the purpose of digestion?
large molecules broken down into smaller components eventually small enough to enter body, two types:
1) mechanical - chewing, GI tract movements
2) chemical - chemical digestions
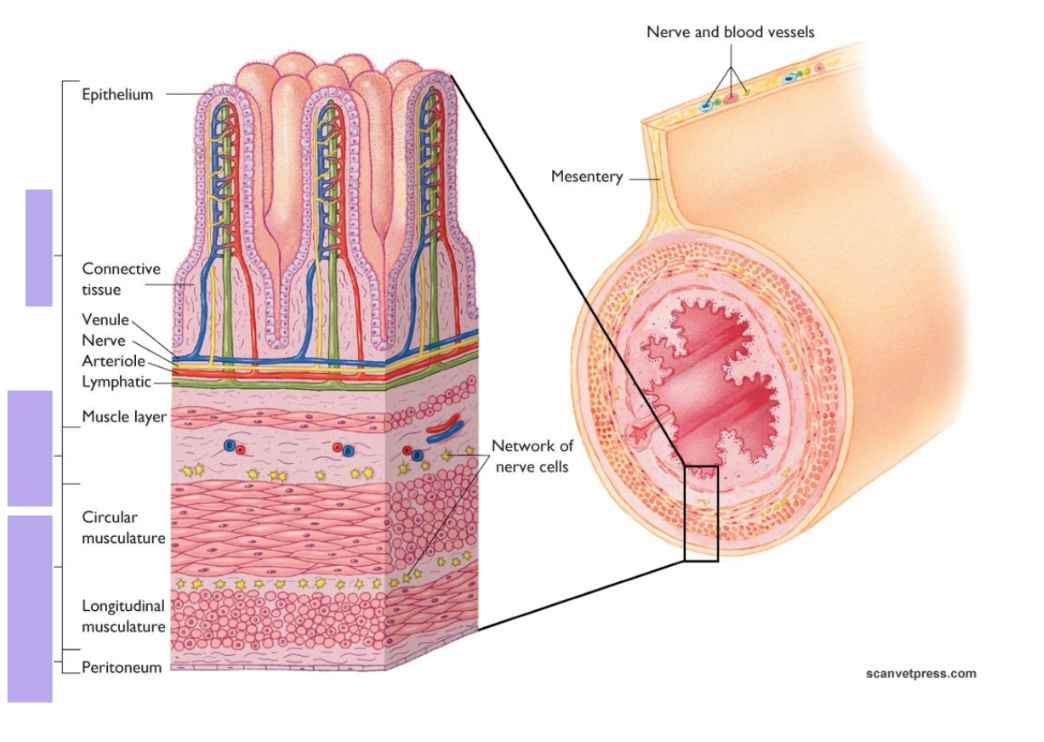
label top to bottom
mucosa
submucosa
muscularis
serosa
What is gut function regulated by on a general level?
it’s under direct regulation of the enteric nervous system and the gastrointestinal endocrine system
What is the enteric nervous system (ENS)?
A mesh-like system of neurons that governs the function of the GI tract consisting of nerve cells and glial (supporting cells) clustered into ganglions (plexuses), capable of acting independently of the sympathetic and the parasympathetic nervous systems (but may be influenced by them)
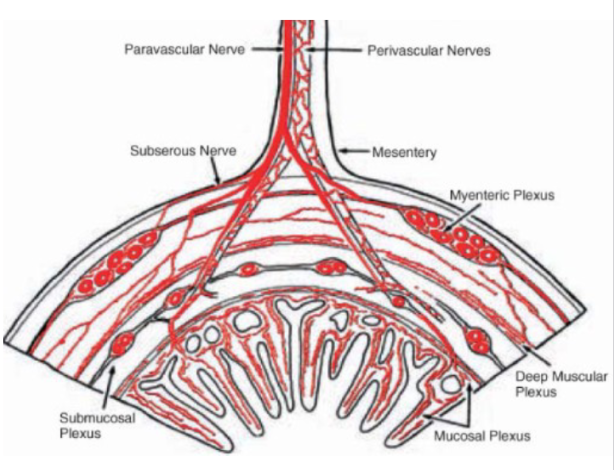
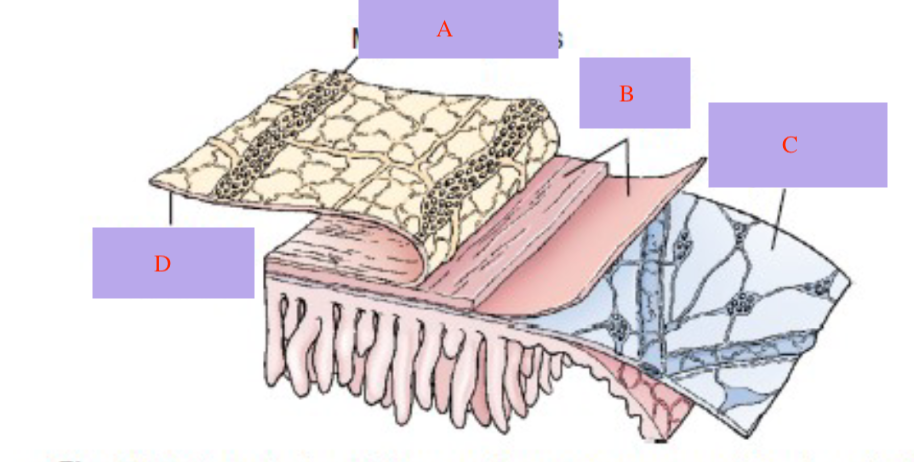
What are the sections of the ENS labeled in this image?
a) myenteric plexus
b) circular muscles
c) submucosal plexus
d) longitudinal muscle
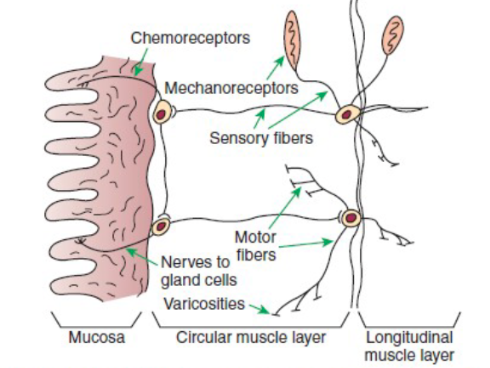
Describe what makes up the organization of the ENS?
1) sensory input comes form mechanoreceptors in the muscular layers and chemoreceptors in the mucosa
2) enteric motor nerves supply vascular muscle, gut muscle, and glands in the gut wall
3) axons end in arborizations (branches) containing vesicular varicosities that have neurocrines that secrete in response to action potential and act on nearby cells/structures (no distinct synapses like the neuromuscular junction)
4) efferent neurons of the ENS may be stimulatory or inhibitory!
What are some neurohumoral regulatory molecules released by the varicosities of the ENS?
Excitatory - acetylcholine, substance P
Inhibitory - somatostatin, NO, CO, PACAP, ATP
BOTH - 5-HT, neurotensin, VIP
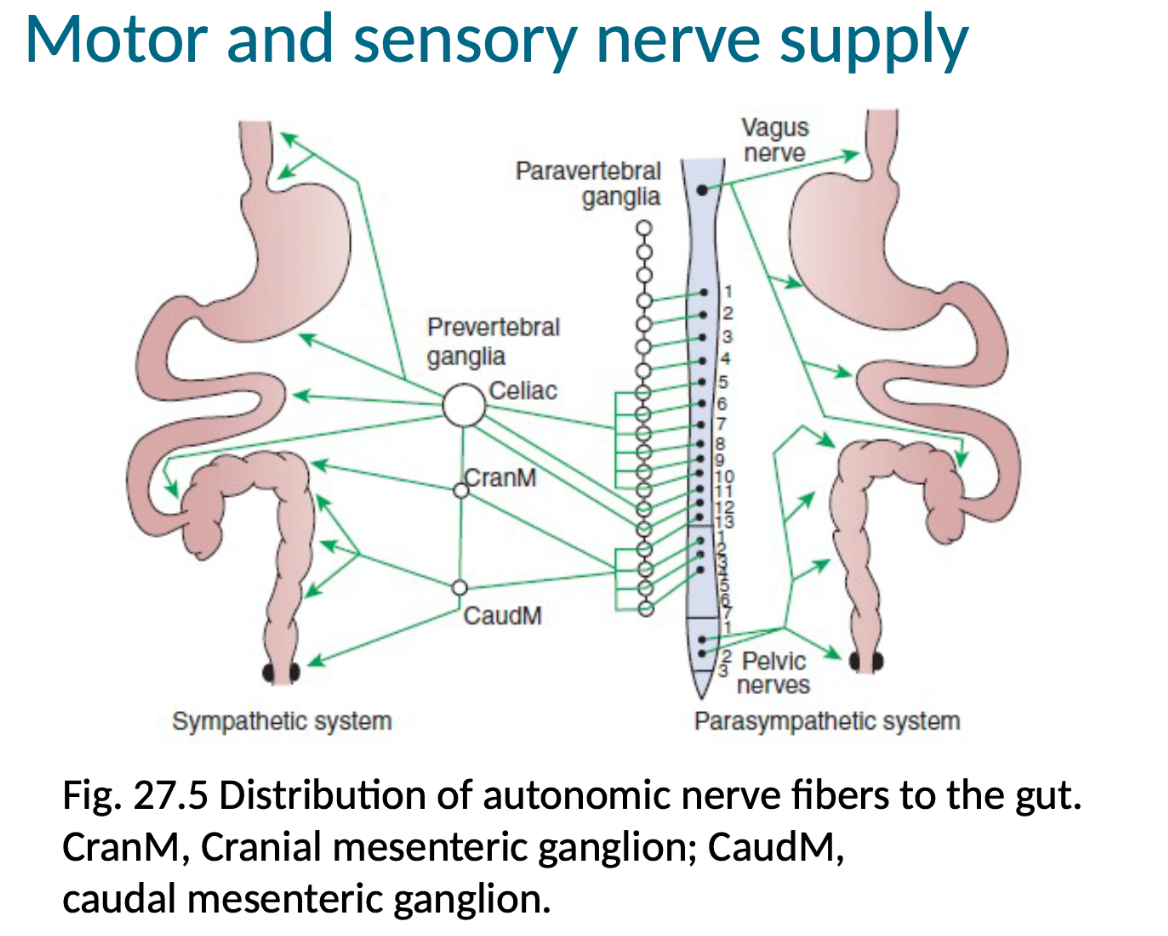
What are the main major motor and sensory nerve supplies of the gut?
Parasympathetic - Vagus (esophagus to beginning of colon), Pelvic nerves (all of colon and rectum)
Sympathetic - Celiac (esophagus to beginning of colon, through prevertebral ganglia), Cranial mesenteric ganglion (all of the above and transverse colon), Caudal mesenteric ganglion ( all of the above and descending colon + rectum)
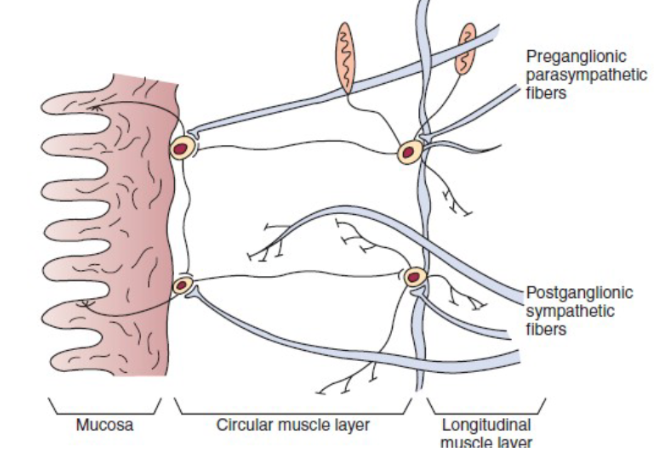
Describe the interface between the autonomic and enteric nervous systems.
Parasympathetic, preganglionic fibres reaching the gut and synapse on the cell bodies of the ENS
Extrinsic sympathetic fibres that enter the gut are primarily postganglionic
Parasympathetic = stimulatory
Sympathetic = inhibitory
What is the NTS?
nucleus tractus solitarii
What is the difference between the vagal afferent nerves and the splanchnic afferent nerves with information?
vagal afferent = parasympathetic, associated with mechanoreceptors and chemoreceptors, provide information about changes in gut muscle tension and chemical conditions of gut lumen
splanchnic afferent = sympathetic, signal presence of pathological conditions such as overdistension
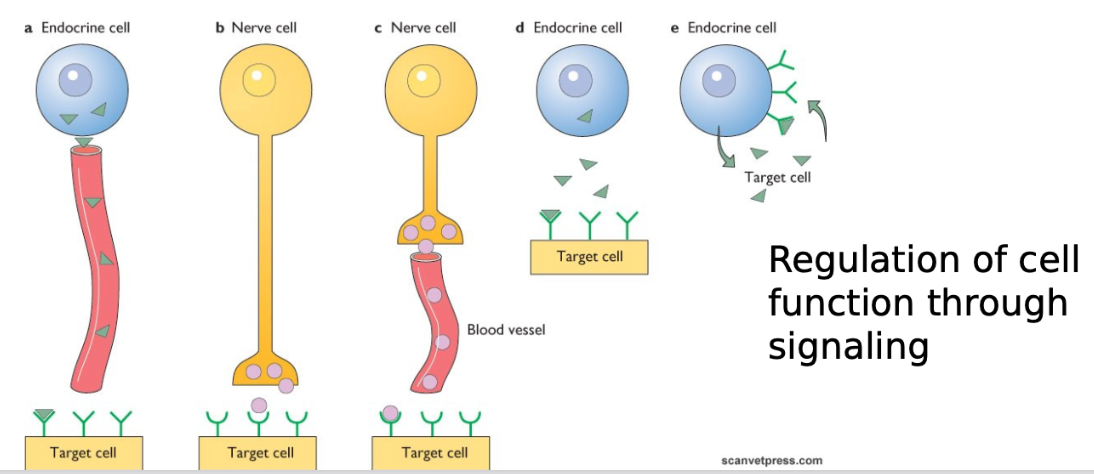
What are endocrine cells?
produce hormones that travel through blood to site of action
what are paracrine substances?
molecules secreted by one cell that have a local effect traveling by diffusion to nearby target cells
describe the structure and function of GI endocrine and paracrine cells.
GI endocrine cells have same structure as paracrine cells: narrow apex exposed to intestinal luminal contents AND broad base for storage of secretory granules
FUNCTION: REGULATORY
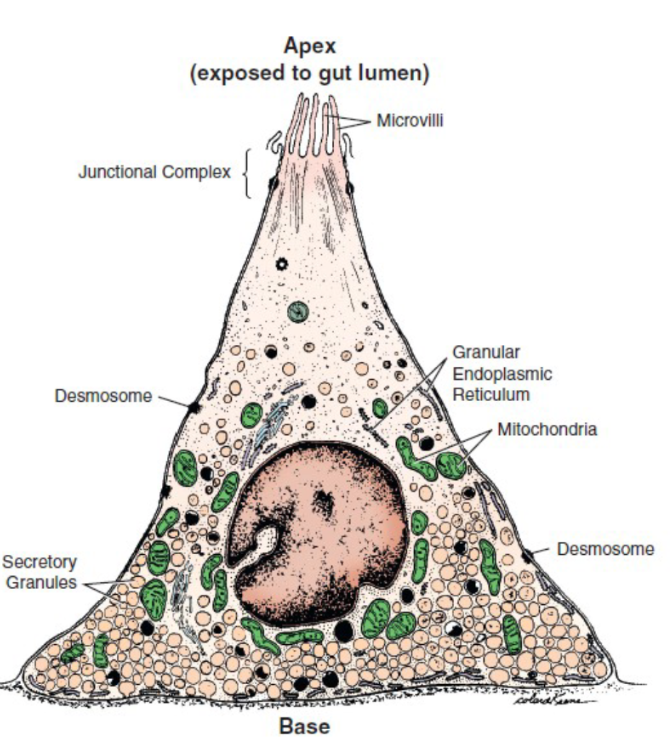
what is there difference between where GI endocrine and paracrine cells release their contents?
endocrine: secrete near blood vessels
paracrine: secrete into interstitial fluid
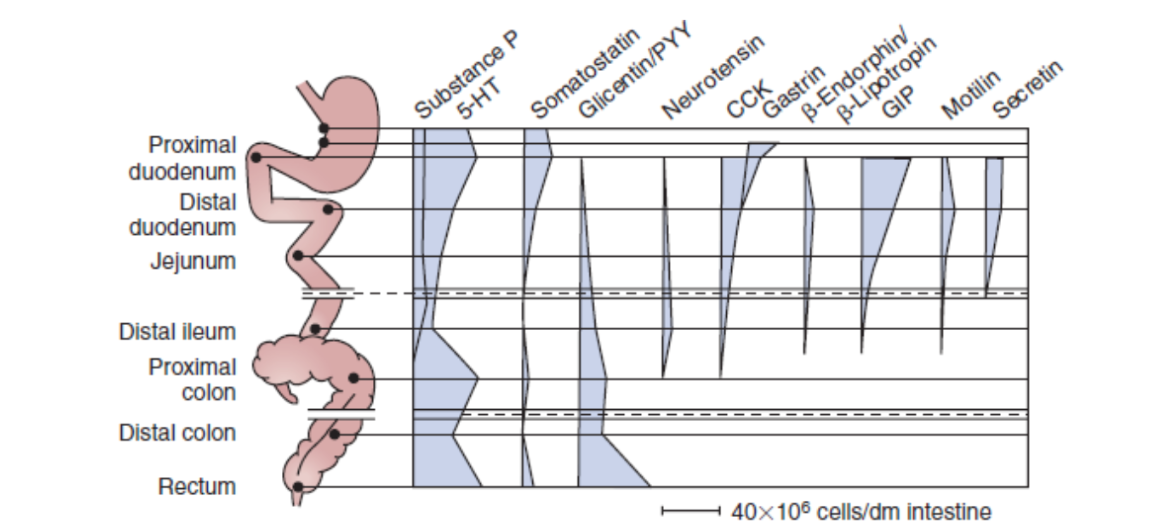
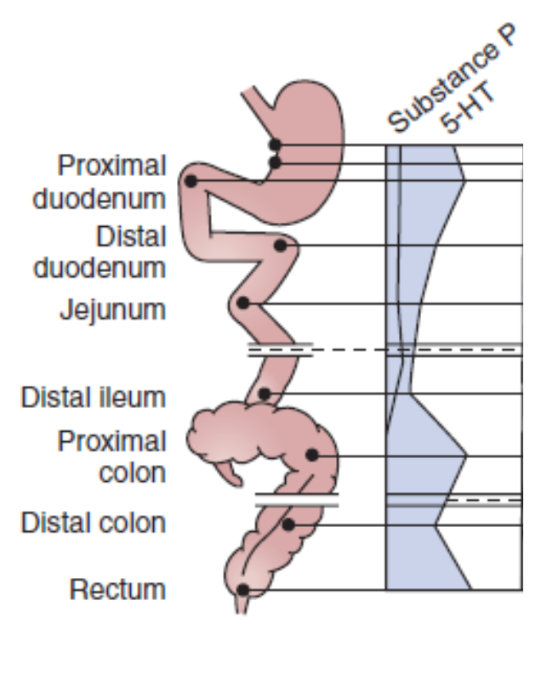
Where are the majority of GI endocrine and paracrine cells found?
stomach - distal ileum
*substance P, 5-HT(serotonin), and Glicentin/PYY found also in entirety of large intestine
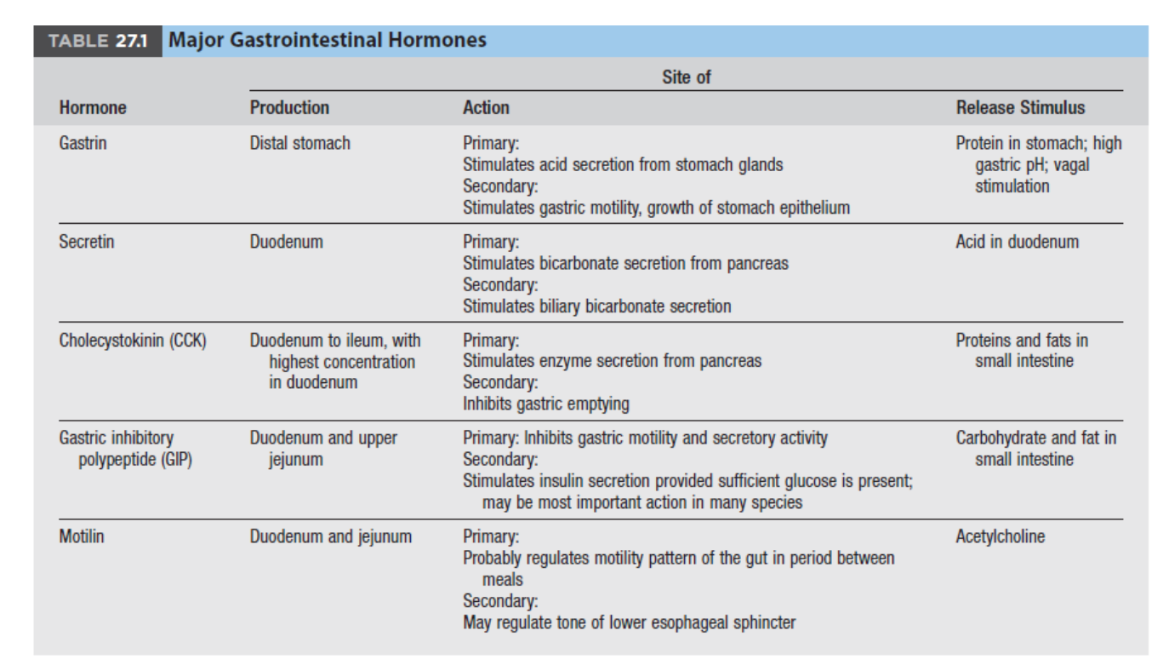
What are the 5 major GI hormones and what do they stimulate?
1) Gastrin - stimulates acid secretion and gastric motility
2) Secretin - stimulates bicarbonate secretion from pancreas and biliary bicarbonate
3) Cholecytokinin (CCK) - stimulates enzyme secretion from pancreas, inhibits gastric emptying
4) Gastric inhibitory polypeptide (GIP) - inhibits gastric motility and secretory activity, stimulates insulin secretion provided sufficient glucose is present
5) Motilin - regulates motility pattern of gut in-between meals, may regulate tone of lower esophageal sphincter
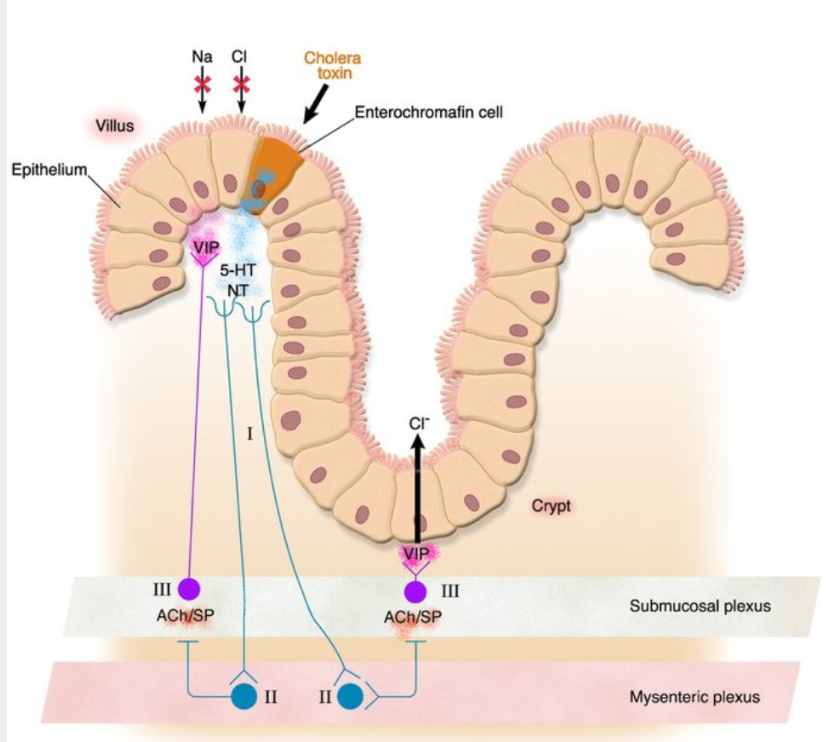
What are Enterochromaffin cells?
subset of GI paracrine cells, found extensively throughout gut and produce 5-HT (serotonin), important in signalling neurons that have excitatory influence on gut muscle and in generating sensory signals from gut mucosa, act as chemoreceptors
How would a enterochromaffin cell respond to stimulus?
presence of stimulus, ie cholera toxin, induces response via interaction with local neural networks in the submucosal and mesenteric plexuses
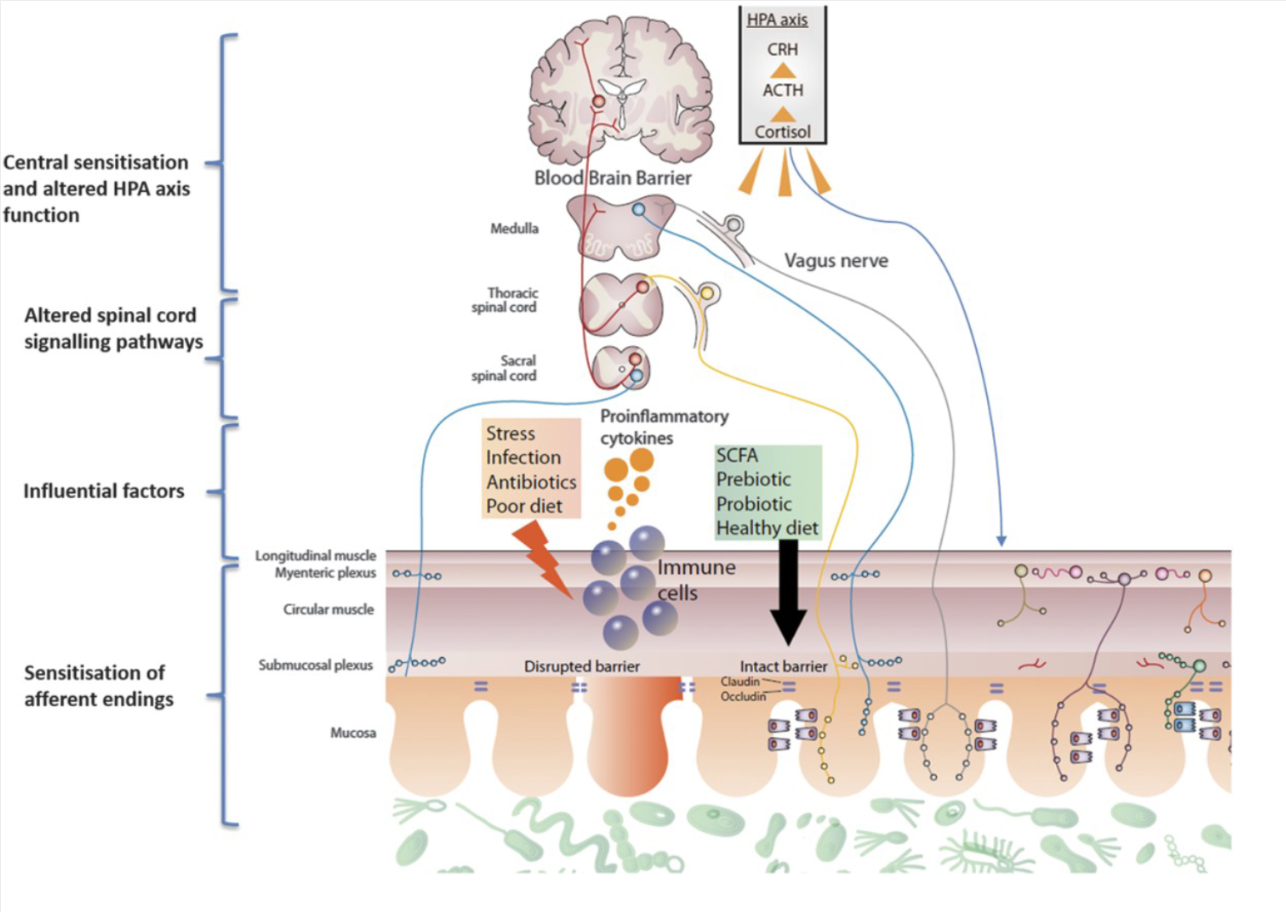
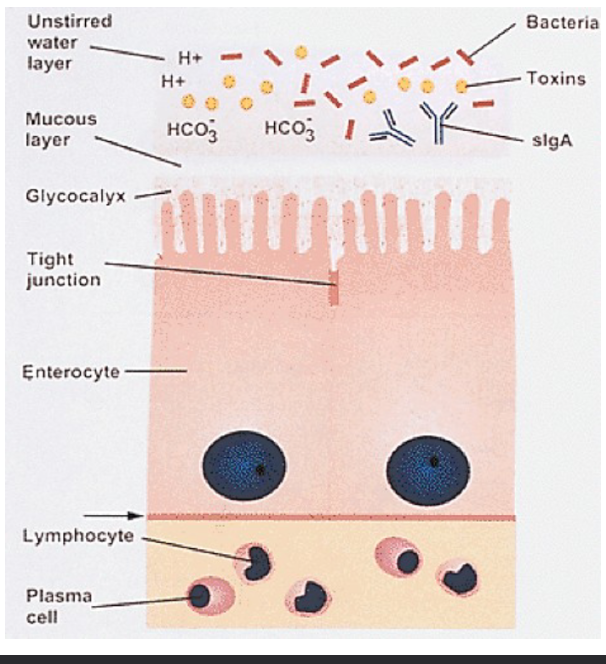
What is the enteric/intestine immune system?
barrier surveillance by immune cells (T and B lymphocytes, mast cells, eosinophils, etc.)
products of immune cells (cytokines, histamine, 5-HT(serotonin), prostaglandins) interact with other cells of the GIT
What are the 3 phases of regulation of the GIT and what are each stimulated by?
1) Cephalic phase - changes in secretion and motility before food enters the stomach, stimulated by sight, smell, taste, anticipation, chewing
2) Gastric phase - changes in secretions and motility initiated by entry of food into the stomach, stimulated by distention of stomach wall and peptides
3) Intestinal phase - entry into duodenum, stimulated by alterations in volume and composition of luminal content
What is maropitant and why is it less useful for the sensation of “nausea” produced, for example, by anti-cancer medications? What may be more useful?
maropitant - effective antiemetic to prevent vomiting
prevents vomiting but did not significantly change nausea scores compared to placebo dogs
none are great, but a better choice would be ondansetron but that isn’t approved (?) in animals
What is the function of gut motility?
motility = all forms of movement of gut
functions: propels ingesta; retains ingesta at given site for digestion, absorption, storage; breaks up food material physically; circulates ingesta
What is transit time and how can you affect it?
it’s the time taken for material to travel from one portion of the gut to another
increase in retentive motility = increase in transit time (slower)
increase in propulsive motility = decrease in transit time (faster)
What are the interstitial cells of Cajal?
specialized GI smooth muscle cells that form an interconnecting lattice around the circular and longitudinal layers of muscle of the gut (similar in structure and function to purkinje cells of the heart)
they are connected to one another and to cells of the general smooth muscle mass by tight junctions/nexuses and have spontaneous changes in membrane polarity occurring in coordinated manner
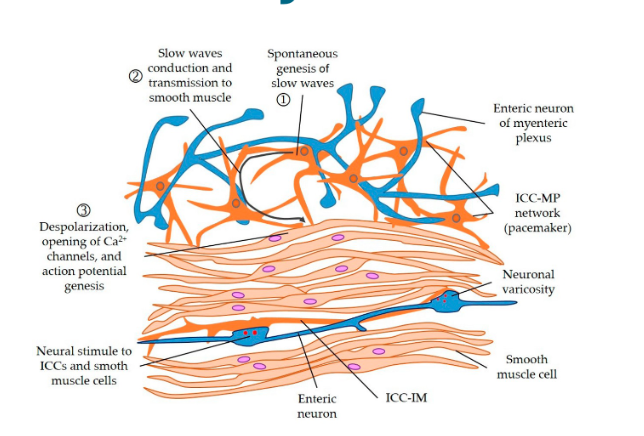
What are slow waves of the GI tract?
electrical waves constantly passing over the muscle regardless of contraction, more frequent in small intestine than in large, DOES NOT AUTOMATICALLY BRING ABOUT AN ACTION POTENTIAL
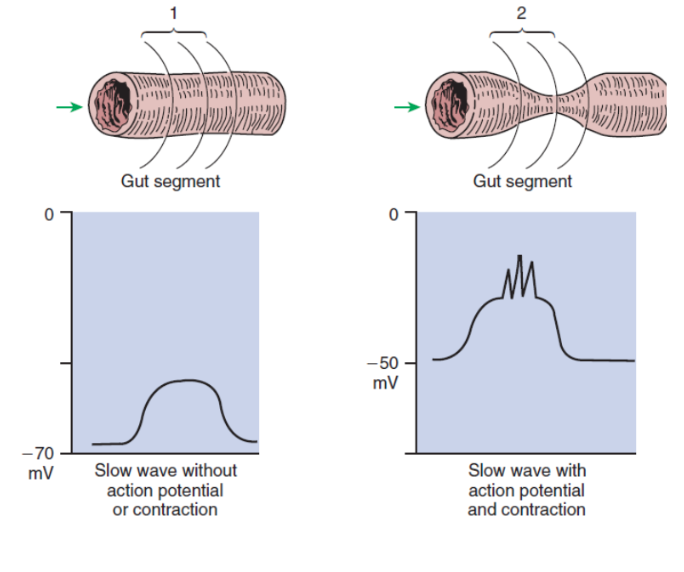
What are muscle contraction frequency limited by?
muscle contraction frequency is limited by the frequency of slow waves (ie. canine stomach slow wave frequency is 5 times a minute)
what consists of digestion in the oral cavity and pharynx?
1) mechanical processing of food by the teeth, tongue, and palatal surfaces
2) lubrication of food by mixing with salivary gland secretions for preparation of transport to the pharynx and oesophagus
3) initiation of swallowing reflex
In most species: lips and tongue have large concentration of sensory neurons capable of registering the texture of different foods
What is Prehension?
the ‘grabbing’ of food and bringing it into the oral cavity using the teeth, tongue, jaw, and head movements, under control of many voluntary muscles and highly coordinated by the CNS
Why are cattle special in terms of prehension?
their lips are not mobile so they use their tongue to pull forage into their mouth and press between incisors and dental pad and then forage is broken off
What is mastication?
largely voluntary actions of teeth, jaws, tongue and cheeks, also initiated by reflex when food in the oral cavity stimulates pressure (sensitive receptors)
reduces size of food particles and helps lubricate food, anatomy of teeth, jaw, and oral cavity match to natural lifestyle of the species
What are the steps to deglutition/swallowing?
Stage 1, voluntary: food rolled into bolus and passed to back on mouth by tongue
Stage 2, involuntary: breathing stops, soft palate elevated closing pharyngeal opening of nasopharynx, tongue pressed against hard palate closing off oral opening, hyoid bone and larynx pulled forward and pulls the glottis under the epiglottis, arytenoid cartilages constrict, muscular constriction of the pharynx pushes bolus to the opening of the oesophagus
Stage 3, involuntary: wave of peristalsis pushes food down oesophagus to stomach with 1 or 2 waves
What is the clinical significance of swallowing?
procedures that disturb coordination of respiration and swallowing may increase chance of pulmonary aspiration, timing is important
What are the two main peristaltic waves involved in stage three of swallowing?
Primary peristaltic wave - moves food down oesophagus to stomach
Secondary peristaltic wave - present if first wave fails, more forceful
How is food transferred to stomach?
through the lower oesophageal sphincter, which is normally closed due to pressure differences in the abdominal cavity versus thorax and anatomical relation, BUT opens due to peristaltic waves
What is the clinical significance of the oesophageal stricture?
ALWAYS pill a cat by following with 3-5mls of water to avoid blockages!
What is the role of muscular action of the stomach?
prepares stomach to store large amounts of food, divides chunks of food into smaller portions and mixes with gastric secretions, empty stomach contents onwards at a steady rate through the pyloric sphincter
What controls the rate of gastric emptying?
the pyloric sphincter
What is stomach musculature during eating regulated by?
regulated by vagus nerve that synapses with postganglionic fibres which release VIP and NO
What changes with the proximal stomach when empty versus eating?
empty = sustained tonic contractions
eating = receptive relaxation allows for food storage
What are the three steps to muscular contractions of the stomach?
starts in the funds (top)
1) contraction causing circular narrowing of lumen, moving in direction towards the duodenum
2) strength increases towards pylorus moving content into duodenum
3) when reaches sphincter, contraction closes it and contents squeezed back into body of the stomach
How long are stomach contractions in the dog?
occur every 15 seconds, lasting 2-3 seconds
What is the inter digestive motility complex?
following emptying, the stomach stays quiescent/dormant for 1-2 hours before intense peristaltic contractions begin and pyloric sphincter relaxes
this cycle continues until next meal
What is the clinical significance of indigestible solids?
they fail to pass through pylorus shortly after a meal do pass into small intestine during periods between meals
ie: corn cobs lodged into intestines and cause obstruction
What is emesis and what are its steps?
complex vomiting action coordinated by brain normally preceded by signs of nausea (salivation, lip smacking, grimace)
1) deep expansion of chest walls against closed glottis
2) relaxation of the Lower Oesophageal Sphincter
3) opening of the upper oesophageal sphinctor
4) forceful ejection of stomach/duodenum from mouth
What species cannot vomit/emesis?
horse, rabbit, rat
What are the two distinct phases and patterns of small intestine motility?
1) digestive period - occurs after food intake
a) non-propulsive (segmentation) = mixes and slows down movement through gut
b) propulsive (peristalsis) = pass over short segments and die out
2) interdigestive period - when little food in present in gut = powerful peristaltic contractions sweep over large length of small intestine, Migrating Motility Complex (MMC)
What is the migrating motor complex?
basic motor activity in the gut during the period between meals/interdigestive states, typically lasts 80-120 minutes in three phases:
1) 60-70 minutes - no contractions
2) 20-30 minutes - intermittent and irregular contractions
3) strong peristaltic contractions lasting 3-10 minutes and start from stomach and migrate distally to colon
has ‘housekeeping’ function and serves to push undigested material out of small intestine, important in controlling bacterial population in upper gut
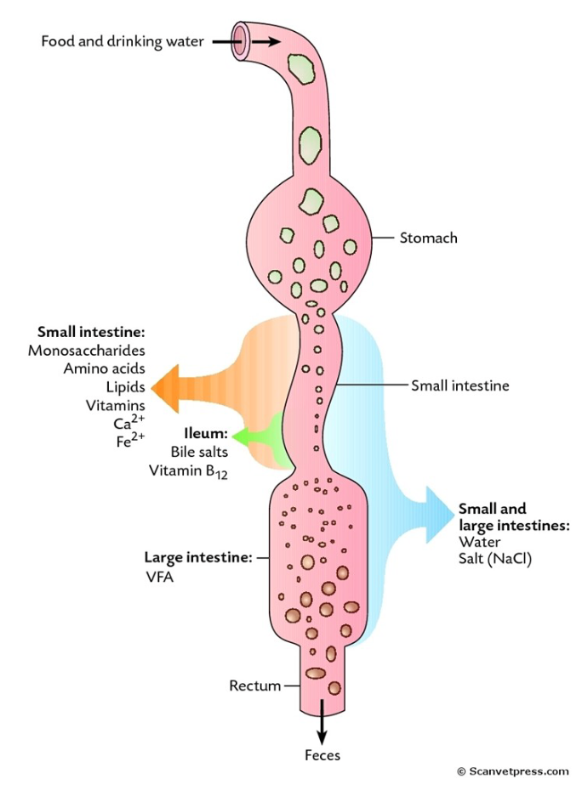
What is the function of the large intestine?
absorption of water and salts, microbial fermentation in mid and hind gut fermenters (horse, rabbit)
What are the different motilities of the large intestine?
segmentation (haustration contractions), peristalsis, anti peristalsis (retropropulsion), mass movement - intense propulsion movement towards the rectum
What is anti peristalsis/retropropulsion?
slows down transit to assist more absorption, arises from colonic slow wave activity, orcing, material accumulates in the proximal portions of the colon
What are the two sphincters of the rectum and anus?
1) internal sphincter of smooth muscle (direct extension of the circular muscle layer of rectum) - usually tonically contracted, is responsible for anal continence, recieves PARASYMPATHETIC innervation from sacral spinal segments through pelvic nerve and SYMPATHETIC interaction from lumbar spinal segments through hypogastric nerve, sympathetic stimulation = constriction, parasympathetic stimulation = relaxation
2) external sphincter of striated muscle - maintains some degree of tonic contraction, innervated by pudendal nerve
What is the rectosphincteric reflex?
presence of faeces in rectum leads to voluntary and semi-involuntary actions that result in peristaltic movements of rectal wall and relaxation of internal anal sphincter, postural changes associated with defaecation
What is megacolon in cats?
secondary to colonic inertia (functional obstruction) or outlet obstruction (mechanical obstruction)
idiopathic - colon loses its normal motility and becomes progressively large
mechanical obstruction - poorly healed pelvic fracture
overall = cat loses ability to defaecate
What are the special differences in organs for the avian digestive tract?
Crop - food storage, some species have crop milk
Proventriculus - glandular portion, propels food to gizzard
Gizzard - tough muscular structure, grinds food, glandular
Paired Ceca - motility characterized primarily by mixing and reverse peristalsis, with occasional mass movements resulting in evacuation of ceca
Colon and Rectum - reverse peristalsis into ceca, urinary excretions arriving at cloaca become incorporated with ingesta and move together into ceca
What is the purpose of saliva?
produced in response to neurological stimulation (ie anticipation of food), lubricates mouth and ingested food, helps form bolus for swallowing, commences chemical digestion:
AMYLASE = omnivorous species
LIPASE = young animals
describe the formation of saliva
initially secreted by acing cells then modified as it passes through intercalated/collecting ducts, transportation of ions and water
out of acini = Na+ and Cl- transported out of fluid, K+ and HCO3- transported into saliva
stimulated by aldosterone
What are the 3 types of salivary glands and what do they produce?
1) parotid - primarily serous (watery) saliva, 50% of total
2) mandibular - mixture of serous and mucoid saliva
3) sublingual - mixture of serous and mucoid saliva
How much saliva is produced cow versus dog per day?
cow = 200-250 l per day
dog = 0.5 l per day
What determines the saliva rate, volume and composition and in specifics in non ruminants?
overall determined by balance of action between sympathetic and parasympathetic neuronal tone
nonruminats:
during meals - copious secretion, parasympathetic predominates
between meals - basal saliva production, sympathetic predominates
Why is saliva so important in ruminants?
its alkaline (pH=8.4), and it buffers VFAs produced by microbes, extensive production during rumination, contains urea that is used as part of nitrogen recycling
what is a clinical example of the importance of saliva?
listerosis - infection that can paralize facial nerves and cause saliva loss from the mouth causing loss of large quantities of water, electrolytes and dehydration, muscle weakness, and death
ALSO IMPORTANT IN ANY DENTISTRY OR ORAL SURGERY for consideration
What are the salivary reflexes?
1) unconditioned (innate) - initiated by sensory information within mouth, taste, mechanical receptors at base of teeth, and oesophagus
2) conditioned (acquired) - sensory information that initially do not evoke salivation become associated with food (ie tractor noises, clattering of dishes)
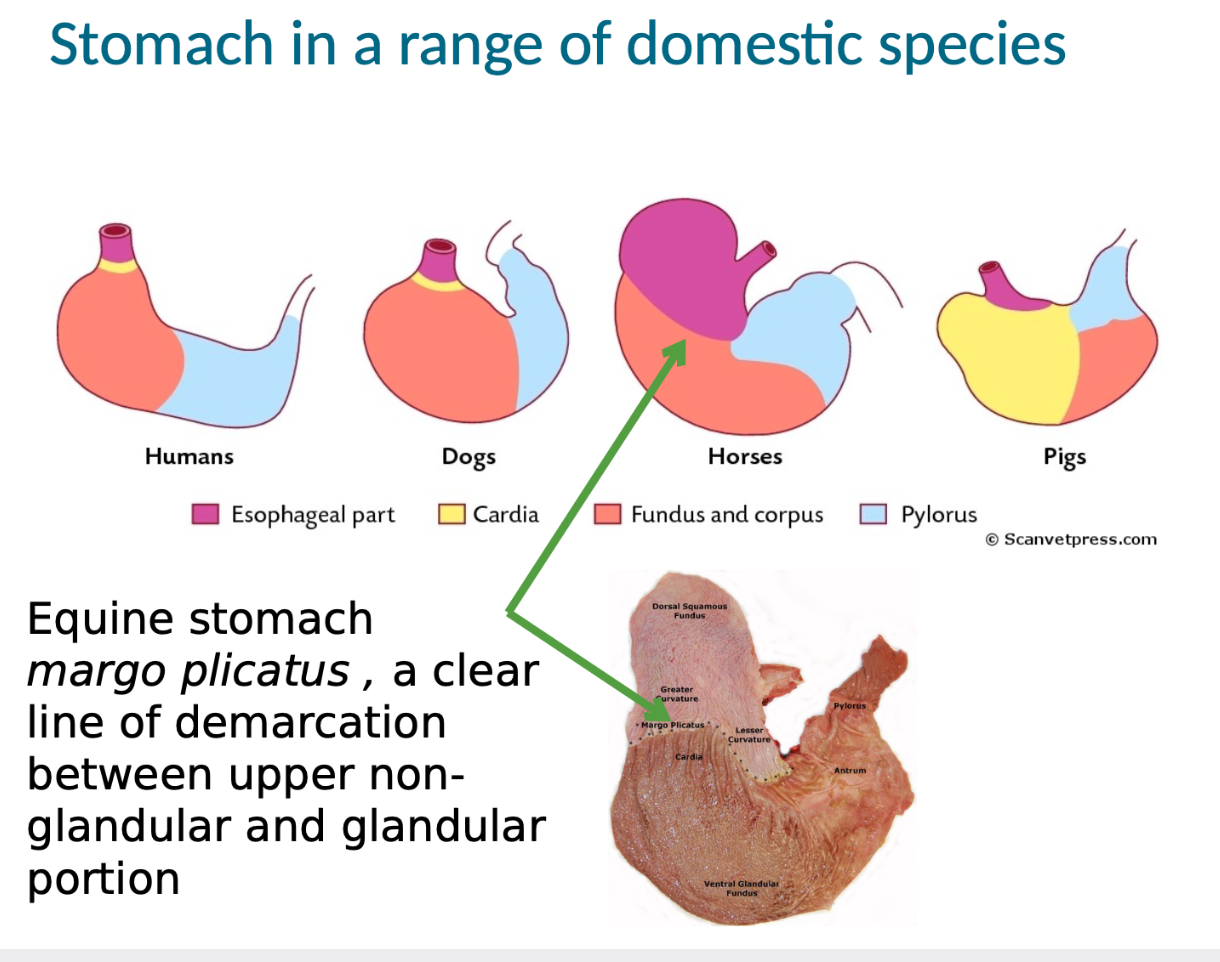
What is the margo plicatus in horses?
clear line of demarcation between upper non glandular and glandular portion of the stomach
What are gastric pits?
most numerous in the fund and corpus, different glandular cells, each with different secretions
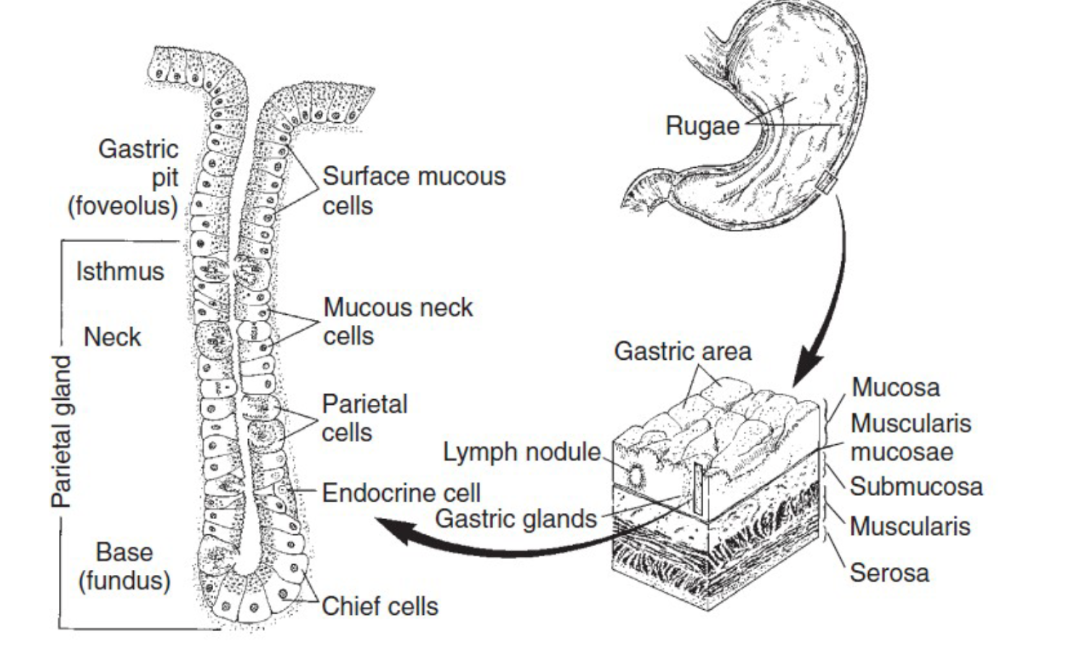
What are some cells and secretions of the gastric pits?
1) parietal cells - H and Cl ions, intrinsic factor (Vit B 12)
2) mucous neck cells - mucous containing bicarbonate, less viscous than produced by cells on surface, progenitor cells
3) chief cells - pepsinogen (inactive precursor to pepsin)
4) endocrine cells - endocrine (hormones) and paracrine molecules
What are the three main endocrine cells of the stomach?
1) G cells - numerous in pyloric part of stomach, on stimulation they release gastrin which stimulates secretion of HCL and pepsinogen
2) D cells - found in pyloric region, release somatostatin in paracrine fashion, effects generally inhibitory
3) enterocromaffin-like (ECL) cells - found in corpus and fungus, paracrine effect that releases histamine
What and were are the most prolific glands in the stomach that produce secretions?
most produced by glands in the fungus and corpus
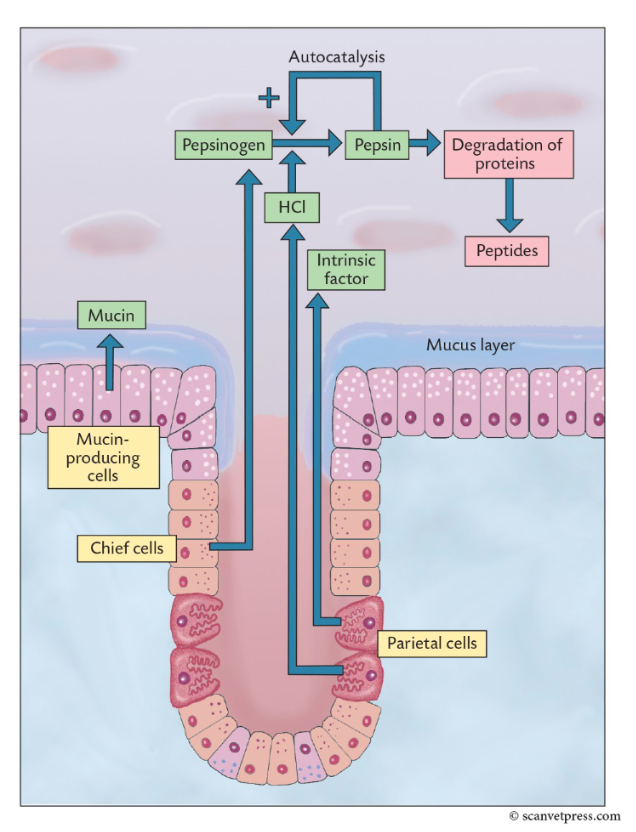
1) HCL - converts pepsinogen to pepsin, provides acid environment for pepsin action, degrades CT and muscle, denatures protein, kills bacteria
2) Pepsin - generated by cleaving pepsinogen, proteolytic enzyme(s), degrades proteins to peptides
What are the three main modes of stimulus of gastric secretions?
1) acetylcholine from cholinergic neurons
2) gastrin released by G cells
3) histamine secreted by enterochromaffin-like cells in gastric mucosa
What is the process of the secretion of HCL?
1) hydrogen ions formed in parietal cells by action of carbonic anhydrase on CO2 and H2O to corm carbonic acid
2) carbonic acid dissassociates to HCO3- and is pumped out of the cell in exchange for Cl-
3) H+-K+ATPase on apical membrane pumps H+ into lumen in exchange for K+
4) excess Cl- passes through Cl- channels to lumen
the increased acid secretion after a meal also results in a transient metabolic alkalosis = alkaline tide
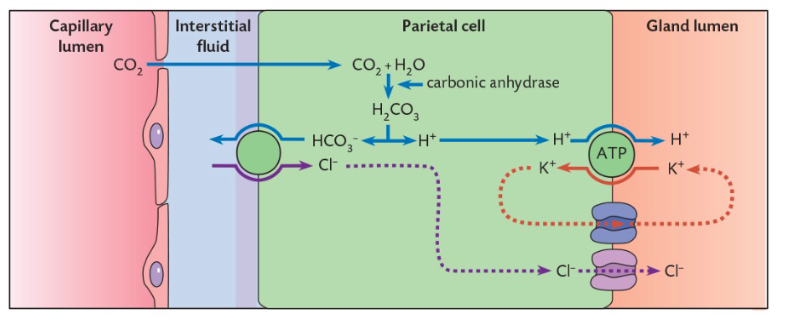
How is HCL production and secretion stimulated?
1) directly - ACh and gastrin binding to receptors on parietal cell, increasing Ca++ signalling
2) indirectly - gastrin and/or vagal stimulation on ECL cell causing release of histamine which binds stimulating intracellular increase of cAMP
What inhibits gastric secretions?
fall in stomach lumen pH towards 2 causes the release of somatostatin from D-cells, High H ion concentration also inhibits release of gastrin which further reduces H+ release (negative feedback loop)
What is the pancreas?
Lobular gland lying in the ‘U’ of the duodenum, outside of the digestive tract but is extrinsic, secretions are essential to digestive process, exocrine function is to secrete digestive enzymes and produce bicarbonate (neutralizes acids in chyme allowing for other enzymes to work)
What are some pancreatic enzymes?
secreted as inactive precursors that are converted to active by duodenal enzyme ENTEROKINASE
1) trypsin(ogen)
2) chymotrypsin(ogen)
3)(pro)elastase
4)(pro)carboxypeptidase
lipases are activated by bile salts and convert fats to fatty acids and glycerol
amylases act on starches and convert them to maltose
What are zymogen granules?
vesicles that store proenzymes near cellular apex, they fuse with the plasma membrane to release contents into lumen of gland
What are centoacinar cells?
modify the electrolyte composition of the fluid secreted by the acinar cells, chloride-bicarbonate exchange protein transports HCO3- out of the cell in exchange for chloride, facilitated by electrolyte transport proteins on basolateral surface of cell
Net result: a bicarbonate-rich alkaline fluid
What are the regulators of pancreatic secretion?
receptors for ACh, CCK, and secretin
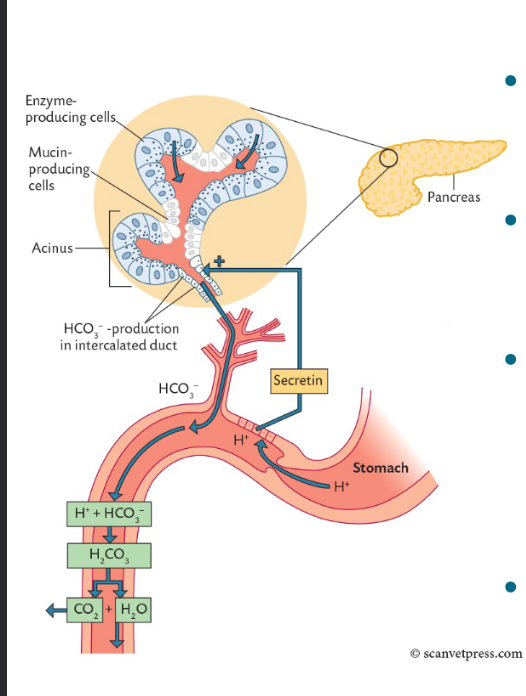
Secretin = stimulates intercalated cells of pancreas to produce watery fluid with bicarbonate
CCK = stimulates pancreas enzyme secretions dn gallbladder contraction
What are the phases of pancreatic secretion associated with the phases of digestion?
Cephalic phase = secretion of pancreatic juice from vagus nerve stimulation
Gastric phase = secretion of pancreatic juice from vagus and gastrin stimulation
Intestinal phase = secretion of pancreatic juice in bicarbonate from secretin stimulation, secretion of pancreatic juice rich in enzymes from vagus nerve, ENS, and cholecystokinin stimulation
why is the pancreas clinically important?
acute pancreatitis and exocrine pancreatic insufficiency
What are the functions of the liver?
1) metabolism - carbs (glycogen), protein (plans, urea, AAs), fats (conversion to glycerol)
2) vitamin storage - mainly fat soluble A, D, E, and K
3) iron storage - in hepatocytes following delivery via transferrin
4) regulation of body temp and heat production
5) detoxification of exogenous and endogenous substances
6) defence against pathogen invasion - kupffer cells (macrophages)
7) formation of bile - required for fat absorption
8) destruction of RBCs - Hb broken down to bilirubin
What is bile?
bile acids formed from cholesterol, have hydrophobic and hydrophilic ‘sides’, act like detergents, bile pigments = breakdown of heme to bilirubin
How is bile released and recycled?
The sphincter of Oddi closed during interdigestive phases, causes bile to be stored in gallbladder (in relevant species) so b ile becomes more concentrated (ion transport)
Gallbladder contracts in response to CCK
Bile duct adds bicarbonate in response to secretin
Bile salts recycled (enterohepatic recirculation), returning bile salts stimulate further bile synthesis
What are some mucosal adaptations fro absorption?
extremely large mucosal surface area, villi covered with brushlike surface membrane known as brush boarder (submicroscopic microvilli), villi and gland like structures are covered with continuous layer of cellular epithelium
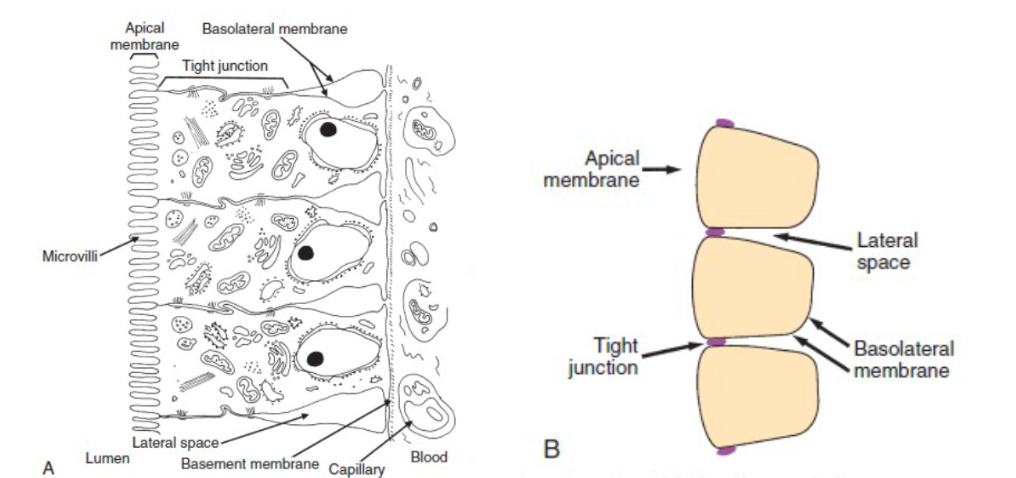
What is special about the arrangement of enterocytes?
tight junctions for a narrow band of attachment between adjacent enterocytes near the apical end of the cells, this divides the apical membrane from the basolateral membrane
nutrients absorbed into the enterocytes through the apical membrane must exit the cell though the basolateral membrane
What is the glycocalyx?
glycoproteins on the surface of the apical membranes, goblet cells secrete rich layer of mucus that covers mucosa and blends into glycocalyx forming a viscous coating that traps molecules
the unstirred water layer near the intestinal surface flows at a much slower rate than in the centre lumen
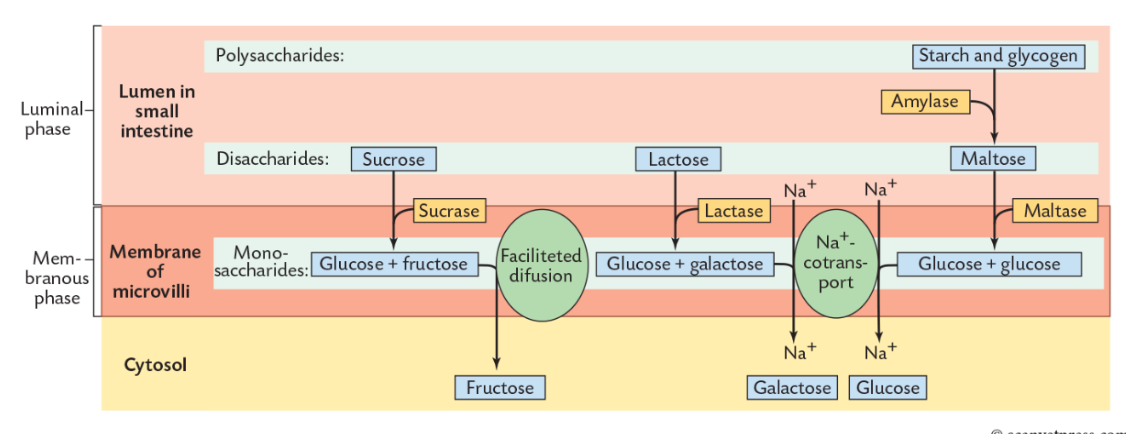
What are the 2 major steps of chemical digestion by hydrolysis?
1) Luminal phase - enzymes within general lumen, as secreted by major glands (pancreatic)
2) Membranous phase - enzymes that are bound to apical membrane of enterocytes (this is followed by absorption)
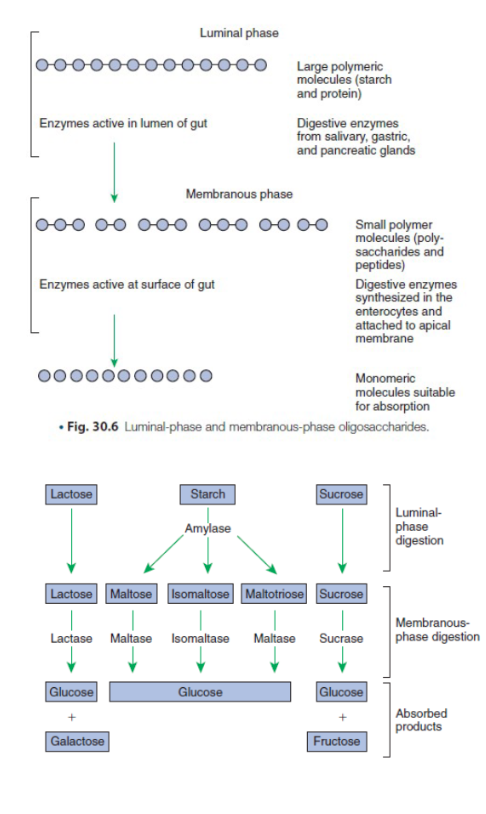
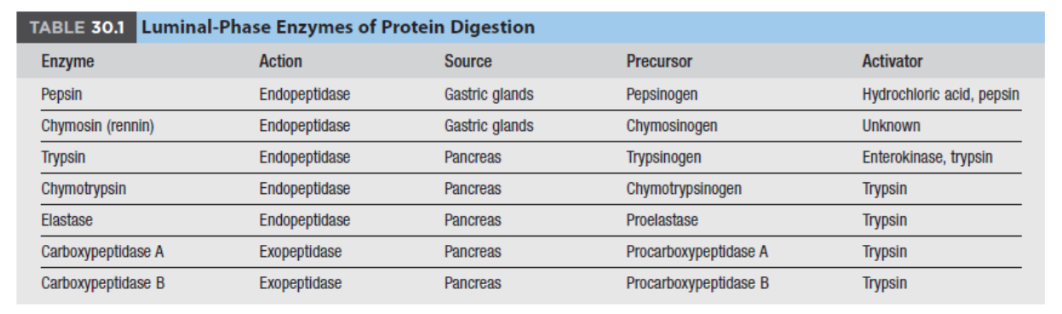
What are some luminal phase enzymes?
digestion of carbs is limited to starches (amylose and amylopectin) Therefore enzyme = AMYLASE (found in saliva and pancreas)
large variety of protein-digesting luminal-phase enzymes
Endopeptidases = break proteins at internal points along AA chain to short-chain peptides
Exopeptidases = release individual AAs from ends of peptide chains
What are some membranous phase enzymes?
structurally part of the enterocyte, synthesized within the enterocytes and subsequently transported to luminal surface of apical membrane enzymatic action occurs in microenvironment of UNSTIRRED water layer, intestinal MUCUS, and GLYCOCALYX
a specific membranous phase enzyme exists for digestion of each type of polysaccharide
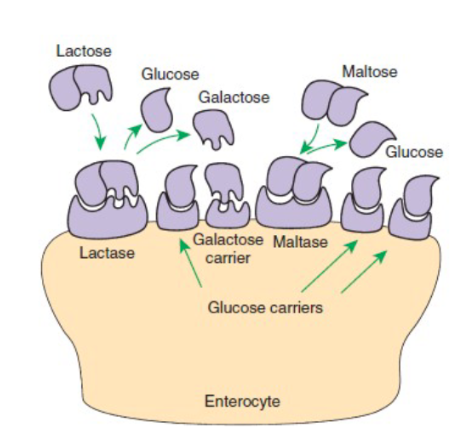
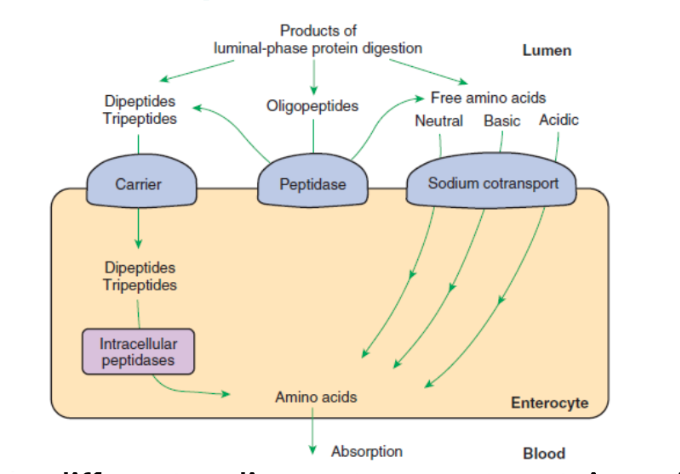
What are the differences between carbohydrate absorption and protein absorption?
carbs = all disaccharide hydrolysis occurs at APICAL MEMBRANE
protein = triple-tides and dipeptides can be hydrolyzed to AAs on either the apical membrane or IN the enterocyte, products are absorbed into the blood (free AAs)
Why are Na+K+ATPases so important?
help keep interior of cells electrically negative with respect to ECF and keep concentration of sodium very low in the intracellular fluid
very important to set up secondary active transport (ie glucose cotransported with 2 Na+ ions) and uses electrochemical gradient
How are carbohydrates absorbed?
absorption of glucose and galactose is by secondary active transport
fructose is absorbed by facilitated diffusion, accumulated in cytosol before transportation through basolateral membrane
following absorption everything travels by portal system to the liver
What is lactose and why is it special?
sugars in milk are >95% lactose, cannot be absorbed so must be broken down by lactase to glucose and galactose
lactase is active and high in newborn mammals but diminishes with age and lactose intolerance can occur in adult dogs and cats
can also arise in young animals as primary disease or following pathogen damage to intestine
How is protein absorbed?
at least 3 different sodium cotransport proteins exist for transport of AAs: for neutral, basic, and acidic
sodium cotransporters might be involved in absorption of dipeptides and tripeptides but not well established
How are fats digested?
warming and mixing action results in liquid fat globules, when exposed to bile it makes emulsified fat droplets and combined action of lipase, collapse, and biles it leads to micelle formation
*Colipase clears path through bile products of surface of fat globules giving lipase access to triglycerides, lipase then catalyzes formation of fatty acids and monoglycerides, surface components and product to lipase action combine to form micelles
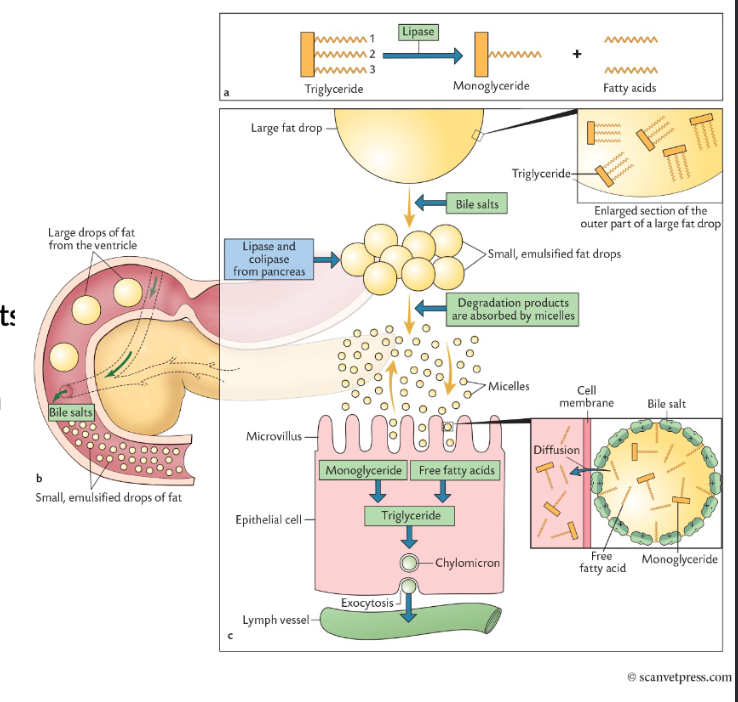
How are fats and resulting bile acids absorbed?
diffusion of micelles through unstirred water allows direct transport of most micelle components except bile acids through the cell membrane and into enterocytes, monoglycerides dissolve in plasma membrane, free fatty acids have facilitated diffusion, in the cytosol triglycerides are reformed from fatty acids and monoglycerides and then packaged into CHYLOMICRONS from transport out of the cell
specialized Na cotransport proteins in the ileum are responsible for bile acid absorption