Week 2 - Wound Healing, Hemostasis, Drains
1/111
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
112 Terms
What are the phases of wound healing?
1) Inflammatory and debridement phase (4-6 days)
2) Proliferation/repair phase (4-24 days)
3) Remodeling/Maturation Phase (21 days - 2 years)
What steps are involved in the inflammatory and debridement phase of wound healing?
- Involves stopping blood loss (reflex vascular constriction initially) an decreasing infection
- Activated platelets release wound repair mediators and create a provisional wound matrix which neutrophils bind to as they migrate to the site
- Result is a fibrin clot and debridement of nonviable tissues
Which cells are the first responders in the inflammatory and debridement phase of wound healing?
- Neutrophils are the first cells to come in
What occurs during the proliferation and repair phase of wound healing?
- Tissue formation phase
- Fibroplasia
- Granulation tissue and collagen deposition
- Epithelialization over granulation tissue (full thickness wound) or epidermis (partial thickness)
- Wound begins to contract
By day four of wound healing (entering proliferation/repair phase), what is the main cell involved in wound healing?
- Fibroblasts
Granulation tissue and collagen deposition occurs at up to what rate during the proliferation/repair phase of wound healing?
- Up to 1 mm/day
During the proliferation/repair phase of wound healing, wound contraction occurs at a rate up to what?
- Up to 0.8 mm/day
What occurs during the remodeling/maturation phase of wound healing?
- Stop fibroblast proliferation and migration
- Collagen type 3 fibers (granulation tissue) are converted to collage type 1 (prevalent in normal skin, organized, and closer to normal strength)
- Tensile strength gradually increases
What is the difference between an open and closed wound?
- Open: Epidermis compromised
- Closed: Epidermis intact
What are the various types of open wounds? Briefly describe them.
- Abrasion - Damage to epidermis and portions of dermis (blunt/shearing forces); More superficial
- Laceration - Compromise of epithelial layers, partial or full thickness
- Puncture - Penetrating injury with minimal skin damage, contamination is often high due to poor drainage
What are the various types of closed wounds? Briefly describe them.
- Crush - High degree of force between two objects
Bit more violent than a contusion; More deep tissue that is damaged
- Contusion - Blow to skin in which blood vessels damaged (substantial blood supply disruption -> Future skin loss and prolonged recovery)
How can open wounds be further classified?
- As clean, contaminated, or dirty/infected
Explain the difference between a clean, contaminated, and dirty/infected wound.
- Clean: Pretty much just when you are using a sterile scalpel blade
- Contaminated: <1x10^5 bacteria/gram tissue; Open and acute)
- Dirty/infected: > 1x10^5 bacteria/gram tissue; Old, devitalized, gross contamination
Between clean, contaminated, and dirty/infected classifications for open wounds, which is most common?
- Contaminated
Describe the typical progression between contaminated and dirty/infected wounds.
- When open/acute, they are usually contaminated. Bacterial load will sky rocket over a couple of days -> Reach "dirty" classification
What are the different types of wound repair?
- Primary closure
- Partial
- Delayed primary
- Closure by secondary intention
Which type of repair is ideal/standard of care when closure is possible and there is not significant swelling/hemorrhage/infection?
- Primary closure
The ability to complete a primary closure depends on which factors?
- How much skin is viable
- Blood supply
- Wound tension (too much tension -> The skin flap will not have sufficient blood flow)
When do partial wound closures occur?
- Some but not all regions of the wound have epithelial apposition OR A region of unepithelialized wound is decreased through suture closure
Partial closures of wound can be useful because they prevent what? What do they result in?
- Prevent further wound retraction
- Results in a smaller area for healing by second intention
When does delayed primary healing occur?
- With severely hemorrhaging wounds (can't see well enough to get sutures in -> Just bandage it at first)
- Significant soft tissue trauma/swelling (put a bandage on it and wait for swelling to go down so it is easy to oppose the skin edges)
- Delay in presentation of patient
- Debulking of chronic wounds
Describe the relative frequency of use of delayed primary wound healing in small animals vs. large animals.
- Small animals: Used a lot, especially in infected wounds, because there is thinner skin and less expansion of wounds
- Large animals: Infected wounds are usually debrided and closed as soon as possible due to expansion of the wound in the days following injury
What does closure by secondary intention involve?
- Wound is left open to heal without sutures
Closure by secondary intention is best for what types of wounds?
- Best for small puncture wounds
Treatment by secondary intention is assisted through the use of what?
- A moist wound environment
What are ways to promote a moist wound environment?
- Hydrophilic substances (Hydrogel)
- Occlusive (petroleum, silicone)
- Semi-occlusive bandages
Which heals more slowly, cats or dogs? Why?
- Cats heal more slowly than dogs due to decreased skin perfusion, slower granulation process
What are the steps of wound closure/management
1) Clean and assess wound
2) Develop a "gam plan"
3) Debridement (devitalized tissue removed to freshen wound edges, reduce bacterial numbers, foreign debris, and necrotic tissue)
4) Wound lavage
5) Drain placement
6) Suturing
What steps are involved in cleaning a wound?
- Clip hair
- Gel to cover the wound (Ideally sterile)
- Cleanse the skin surrounding the wound with 0.2% povidone iodine solution
- Rough and sterile prep methods
What can be used to lavage a wound and remove cleaning solutions? Is alcohol a good alternative?
- Saline
- Alcohol is cytotoxic
What is involved in a "hands on" evaluation of a wound?
- After sterile preparation, the wound can be probed w/sterilely gloved fingers +/- sterile probe/instruments
What can you do if you suspect a synovial structure may be involved in a wound?
- Sterile preparation of any suspected synovial structures that might be involved -> A synoviocentesis (2-3 mL fluid aspirated) followed by distension
Do all wounds need debriding if they appear clean and fresh?
- Yes; Even fresh wounds will have some diseased tissue at the very edges of them -> "Freshen" the edges of the epithelium to get to bleeding tissue
What are the 5 types of debridement? Briefly describe them.
1) Surgical (sharp dissection)
2) Mechanical (low-pressure with syringe 35 CC syringe + 19 G needle; 7-15 psi OR wet gauze abrasion)
3) Autolytic (use of innate autolysis)
4) Enzymatic (placement of topical enzymatic digestors)
5) Larval (maggots produce proteolytic enzymes and consume necrotic tissue)
Staples should only be used for wound closure if there is minimal....
- Wound tension
What suture pattern is generally most appropriate for wound closure?
- Simple interrupted
What are some methods for wound tension?
- Tension relieving suture patterns
- Pre-stretching
- Undermine the wound margins to create more "stretch"
- Close along the skin tension lines
- Use SQ sutures in SA
- Stent suture
- Tension relieving surgical techniques (advancement flaps, rotation flaps, relaxing incisions)
Suture material needs to be ______________ enough for ____________ enough.
- Strong
- Long
What are the desired characteristics when choosing a suture material?
- Retain tensile strength until purpose is achieved
- Knot security/ ease of use (multifilament better than mono)
- Minimal likelihood of becoming infected (monofilament better than multi)
Describe the tensile strength of absorbable vs. non-absorbable suture.
- Absorbable: Tensile strength lost between 15-48 days
- Non-absorbable: Tensile strength persists beyond 50 days
List the suture sizes from smallest to largest.
- 6-0 < 5-0 < 4-0 < 3-0 < 2-0 < 1-0 < 0 < 1 < 2 < 3
Why should you never use a non-absorbable suture under the skin if you don't want it to be there forever?
- Nidus for infection
Generally, where are absorbable vs. non-absorbable sutures used?
- Absorbable:Deeper tissues
- Non-absorbable: Only in epidermal/epithelial layer; You may use it in a cruciate ligament or lacerated tendons
In the following tissue types, indicate if you would use a absorbable or non-absorbable suture and what size you would use.
A. Cutaneous appositional
B. Intradermal
C. Skin tension
D. Subcutaneous
E. Fascia
F. Muscle
G. Tendon
H. Eyelid
I. Conjunctiva
A. Non-absorbable. 3-0 to 0
B. Absorbable; 3-0 to 2-0
C. Non-absorbable; 2-0 to 1
D. Absorbable; 4-0 to 2-0
E. Slow absorbable; 2-0 to 3
F. Absorbable; 2-0 to 1
G. Slow absorbable or non-absorbable; 0 to 2
H. Non-absorbable; 6-0 to 4-0
I. Absorbable; 6-0 to 4-0
What general category of needles are preferred?
- Swaged (needle attached to suture rather than suture being through an eye)
How does the curve of the needle required vary with the depth of the structure?
- Deeper body cavity, more curve required; 1/2 or 3/8 circle good general purpose needle.
What is the purpose of reverse cutting needles?
- Reverse cutting needles help prevent tearing of the tissue and needles are stronger than conventional cutting
When are cutting vs. taper needles used?
- Taper cut needles for subcutaneous tissue
- Cutting needle anytime you are going through the skin
When can staples be used for wound closure?
- Adequate for closure of wounds under no tension (facial injuries)
- Can be used between sutures to speed up closure or large, minimal tension wounds
What can dead space lead to?
- Seroma formation -> closure breakdown and a source of infection
What are methods for avoiding the formation of dead space?
- SubQ/muscle/fascia closure
- Placement of drains
What is the purpose of drains?
- Manage anticipated accumulation of fluid
How long should drains stay in?
- 3-5 days or until draining slows/stops
Drains should always exit the patient ____________ to the suture line.
- Remote
What are the two categories of drain types and examples of each?
- Passive: Penrose drains + rigid, fenestrated, polypropylene, silicone, and red rubber
- Active: Fenestrated silicone (Jackson Pratt) or polyurethane
Describe the mechanism by which passive drains work.
- Fluids moves by capillary action around the drain rather than through the middle
Describe the mechanism by which active drains work.
- Connected to a suction device (manual or mechanical)
When a drain is placed, how long should antibiotics be continued at the minimum?
- Until 24 hours post drain removal
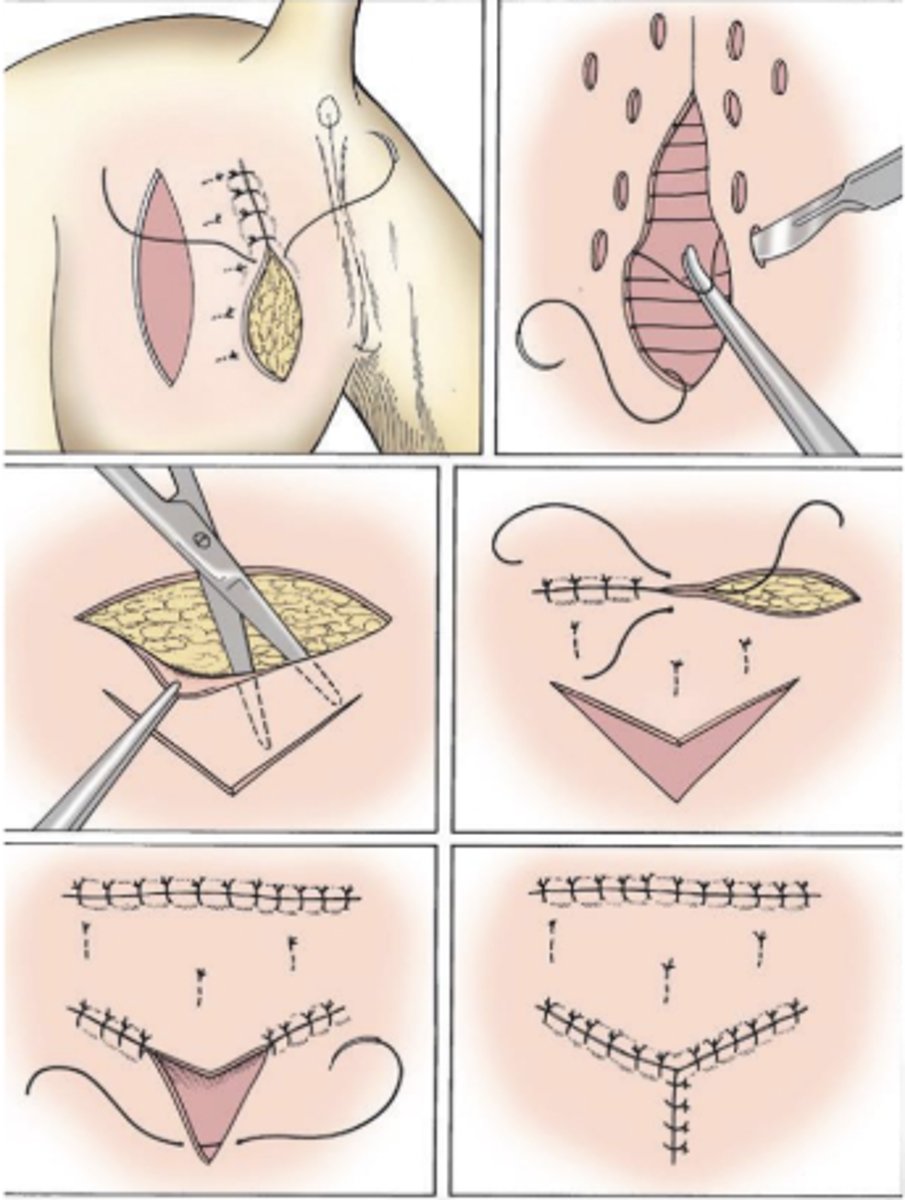
How should Penrose drains be placed?
- Secure at top of drain and exit through skin
How should Jackson Pratt drains be placed?
- Finger trap suture at exit
A drain should not extend out where?
- Drain should not extend out beyond laceration edges; Make a stab incision further away for it to exit the skin.
Antibiotics are used on _______________ wounds.
- Contaminated or dirty/infected
What route of administration of antibiotics is often sufficient for partial thickness or clean wounds?
- Topical
For contaminated and dirty/infected wounds, how long should antibiotics be systemically administered?
- Contaminated wound: 3-5 days
- Dirty/infected wound: Longer -> Culture wound after contamination is resolved
Excessive granulation tissue is common when?
- In LA limb wounds
Excessive granulation tissue can be prevented how?
- Occlusive dressing (petroleum, silicone)
How can excessive granulation tissue be treated?
- Sharp dissection
- Immobilization (cast or bandage cast)
- Skin graft
- No topical therapy has been shown to be consistently effective
What is the difference between horses and mules/donkeys in regards to bleeding?
- Mules/donkeys hemorrhage more
What clinical pathologic tests may you want to consider prior to going to surgery?
- Platlets
- Mucosal bleeding test
- ACT (Activated clotting times)
What percentage of body weight is the blood volume?
- 7-8% (can be as high as 10% in young animals or newborns)
Blood volume is how many mL per kg?
- BV = 70-80 ml\kg
What percentage of blood volume must be lost to require replacement?
- Loss of 20% (fast) to 50% (slow) may require replacement
What are methods for hemostasis at the surgical site?
- Pressure
- Cautery +/- instrumentation
- Ligation
- Surgical staples
- Primary repair of larger vessels
When using gauze and pressure, why should one "blot not wipe"
1) Avoids further tissue trauma to the area
2) Disrupts clot formation (removes venous clots)
What is the difference between electrocoagulation and electrocautery?
- Electrocoagulation: Electricity causes heating in tissues by putting currents through it and results in coagulation
- Electrocautery: Something heated first then applied to "sear" the tissue
Electrocoagulation can be used for what vessels?
- Used for vessels <1.0-2.0mm
Electrocoagulation can be _______________ (more commonly) OR _______________.
- Monopolar (more commonly)
- Bipolar
To use electrocautery or electrocoagulation, the patient needs to be _______________.
- Grounded
Describe the mechanism behind monopolar electrocoagulation.
- Flow of current from active electrode through patient to ground plate; Active electrode has small contact area while the patient ground plate has large contact area and reduces current density and results in minimal tissue heating
What are some complications of monopolar electrocoagulation?
- Thermal necrosis at wound site
- Thermal necrosis from inappropriate patient grounding
- Excessive use increases the risk for surgical wound infection (More tissue trauma/inflammation)
- Charring - irrigation of the wound
- Consider smoke evacuation if being produced, especially if arising from a tumor
Explain the mechanism behind the use of a bipolar coagulation system.
- Active and ground electrodes are on the forceps and the current passes from one tip, through the tissue, to the other tip. A hand-switch or foot-switch is used. It is more precise and commonly used for neuro or cosmetic surgery.
What is the benefit of a Ligasure (Tm)?
- Can be used for larger vessels (even 1 mm)
When does ligation need to be used?
- Vessels greater than 1 to 2 mm
When performing ligation, ________________ suture material has better holding power.
- Finer (0, 2-0, 3-0)
What type of suture is typically used for ligation and anastomosing vessels together?
- Monofilament absorbable
Hemostatic forceps can be used in a "tips up" or "tips down" fashion. Which is more precise and commonly used for picking up vessels?
- "Tips down"
When is primary repair of a vessel performed? What suture is usually used?
- For severed larger vessels
- Usually non-absorbable , 5-0 to 7-0, monofilament
How is primary repair of a vessel performed?
- Essentially simple interrupted around the two ends of the vessel; Sutures at 4 points, and then split those points and sutures at 45 degrees all the way around (6-8 sutures total)
What hemostatic agents are available and which can be "left behind" in the patient?
- Bone wax
- Surgical
- Gelfoam (can be left behind)
- Hemcon bandage
What is the purpose of Chitosan-based Wound bandages? How do they work?
- Hemorrhage control in trauma
- Positively charged chitosan acetate in bandage adheres to tissues and agglutinates RBCs
What are the indications for using drains?
1) Eliminate dead space
2) Evacuate existing collections of fluid (pus); provide drainage from contaminated/infected sites
3) Prevent anticipated collections of fluid or gas
What are some additional benefits of using drains?
- Speed the healing process
- Prevent complications
Why is it important that the end of a drain extends beyond the skin?
- When extending out of an incision or puncture site, if it adheres to the edge of the skin, it will not function properly.
Penrose drains are not fenestrated. Some people will intentionally fenestrate them. Why is this wrong?
- This will weaken the drain. It is possible a piece will break off into the animal. You will not get any more effective drainage.
Why can Penrose drains not be used for active drainage?
- Cannot be used for active drainage -> They will collapse (they are soft)
Which is more difficult to maintain, active or passive drains?
- Active
There is a rigid fenestrated tube placed in a horse's pleural cavity to drain purulent material. It has a one way Heimlich valve on the end. What type of drain is this, active or passive?
- Passive
There is a rigid fenestrated tube placed in a horse's pleural cavity to drain purulent material. It has a condom on the end of the tube. What type of drain is this, active or passive?
- Passive
The efficiency of a Penrose drain is related to its what?
- Surface area
A penrose drain should ideally be anchored with suture in the ___________ portion.
- Proximal