L5: Fluid Balance
1/97
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
98 Terms
How much water is in the total body fluid?
60% of total body weight

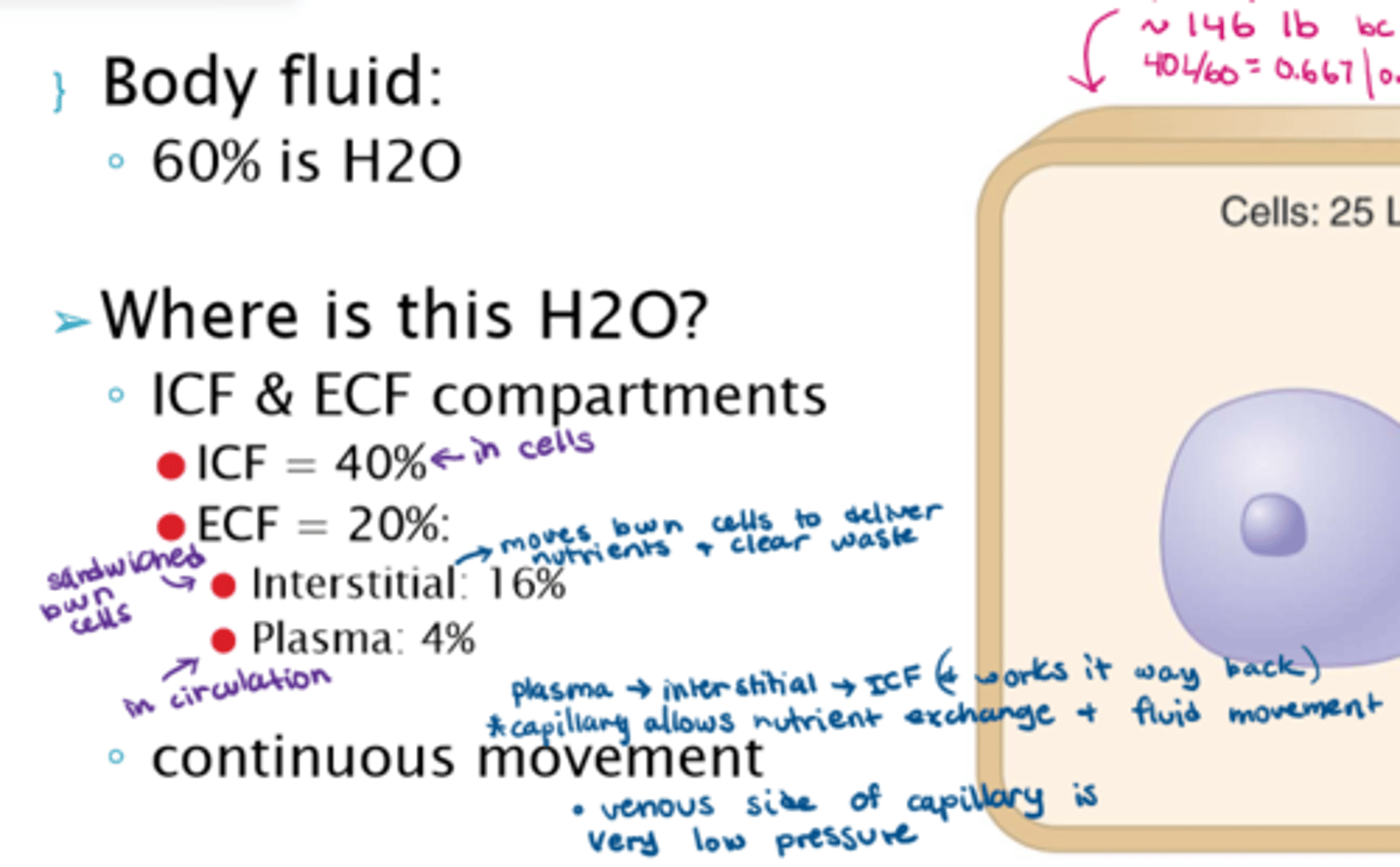
Where is water found in the body? How is it divided amongst body fluid?
- within the ICF & ECF compartments (there is continuous movement between them):
- ICF = 40% (25L)
- ECF = 20% (15L)
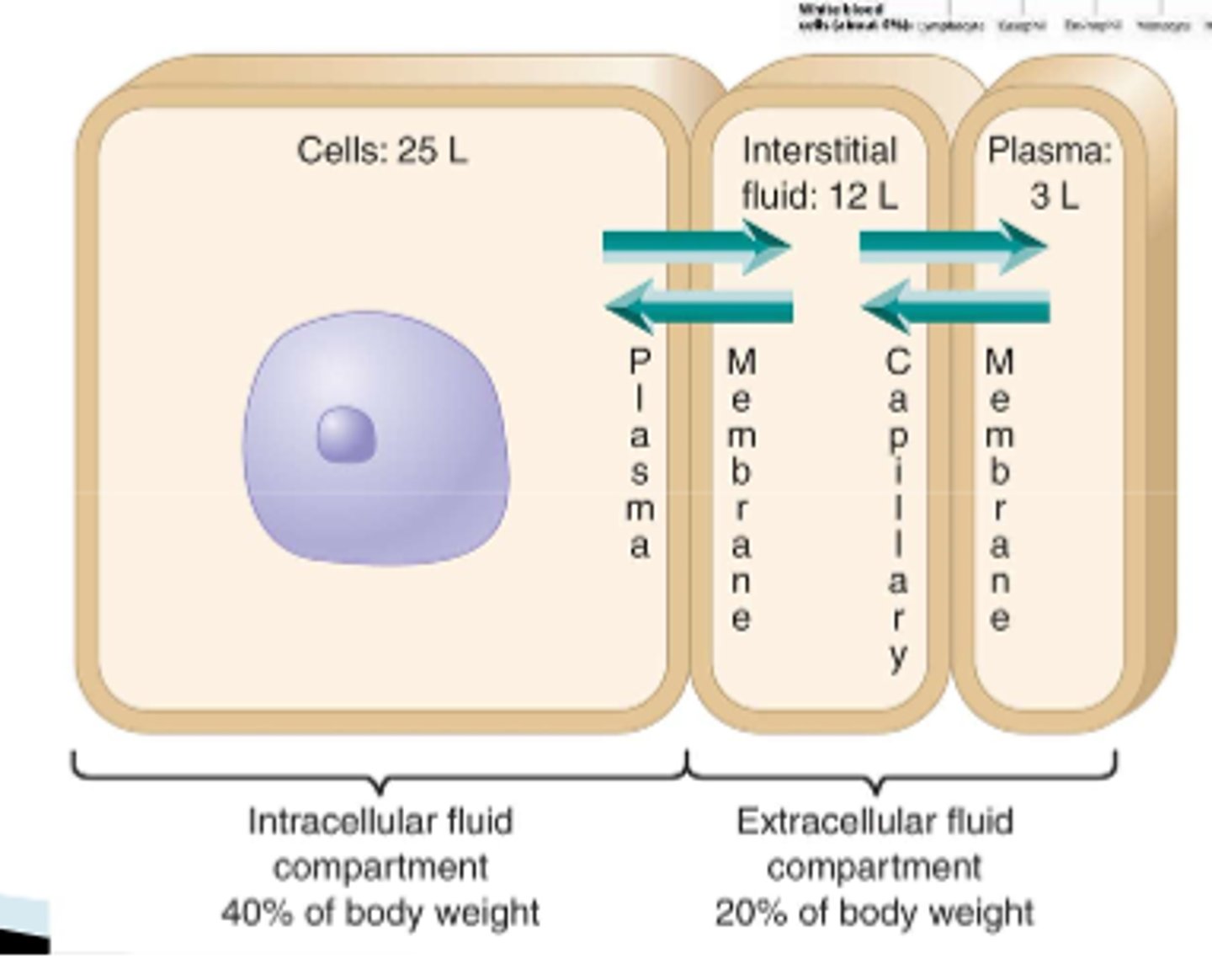
How is water divided amongst extracellular fluid?
- Interstitial fluid: 16% (12L)
- Plasma: 4% (3L)
How does high BP impact fluid movement?
- an increase in BP causes fluid pressure to increase
- this pushes more fluid interstitially, less fluid going back into the bloodstream
- results in edema (swelling) in patients

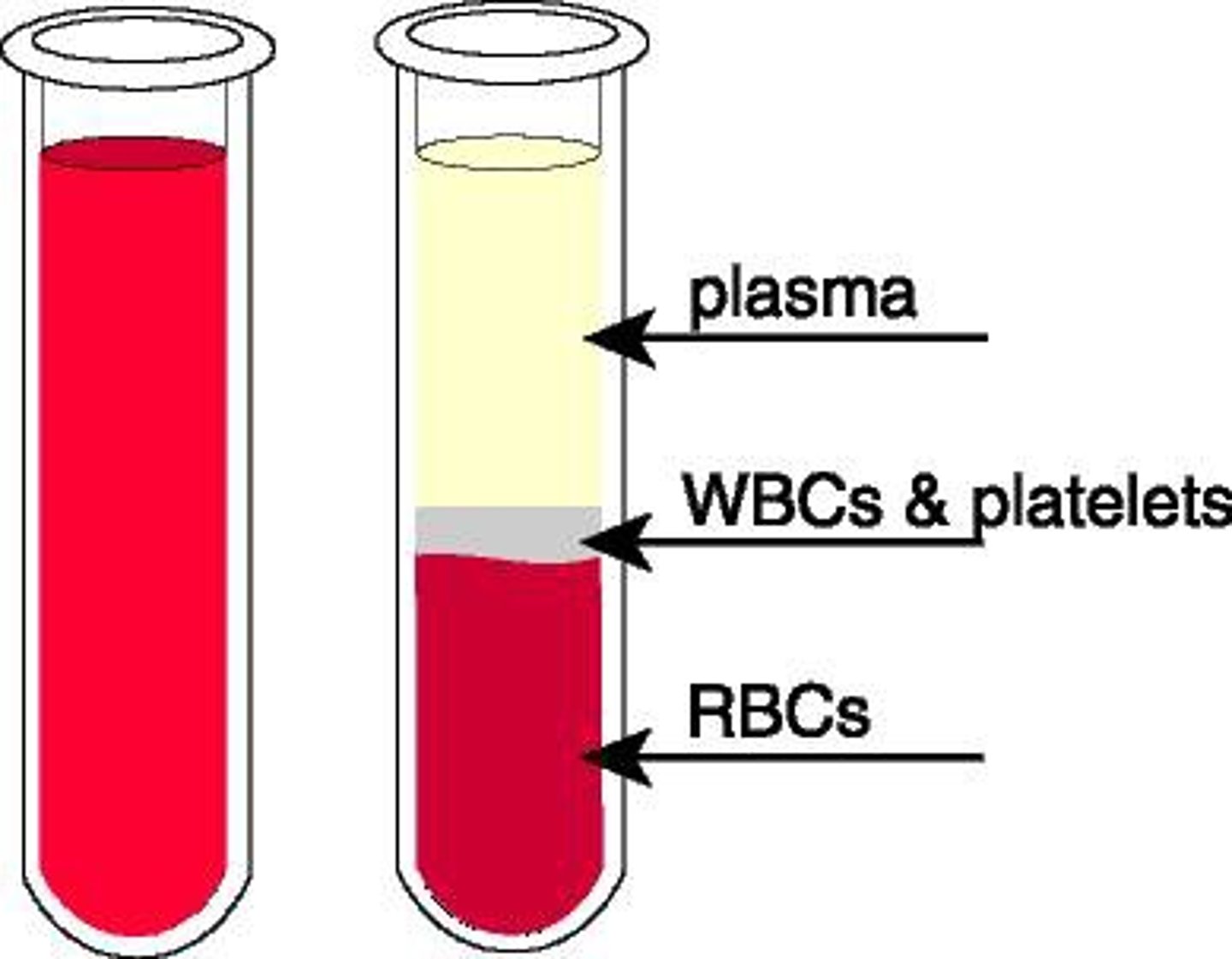
What are the elements of blood?
- plasma: 55%
- platelets: 0.01%
- RBC: 41%
- WBC: 4% (lymphocytes, basophils, eosinophils, monocytes, neutrophils)
What are the different body fluids?
- blood, urine, semen, vaginal secretions
- CSF, synovial fluid, pleural fluid,
- pericardial fluid, peritoneal fluid, amniotic fluid (water-like, surrounding fetus)
- saliva, nasal fluid, otic fluid, gastric fluid, breast milk, and more
What are the recommendations of daily fluid intake?
10 cups of fluid a day (2.5 L)
What major electrolytes do our cells need to function?
sodium, potassium, chloride, magnesium, calcium, phosphate, and bicarbonates
What patients would most likely experience fluid balance issues or fluid loss?
- patients in a hypermetabolic state: fever => lots of sweating and fluid loss
- patients on diuretics and other meds that increases urine excretion
- GI patients: N&V and diarrhea issues
- pts with a high or low BP
- overhydrated/dehydrated patients
- very active patients: sweating out fluid AND electrolytes, need to replenish BOTH

Function of norepinephrine and epinephrine
Potent vasoconstrictors
What happens in the body to regulate fluid balance when BP is low?
1. baroreceptors (located in glomerulus and heart) notice low BP, and communicate with the vasomotor centre in the medulla
2. norepinephrine is secreted via the vasomotor centre as a HORMONE because it is being secreted into circulation (it is a NT within CNS), causing vasoconstriction
3. NE secretions stimulate E and NE secretions via the adrenal glands, causing potent vasoconstriction in the arterioles
4. Adrenal glands also secrete aldosterone, causing urinary retention.
5. Aldosterone stimulates renin in the kidneys
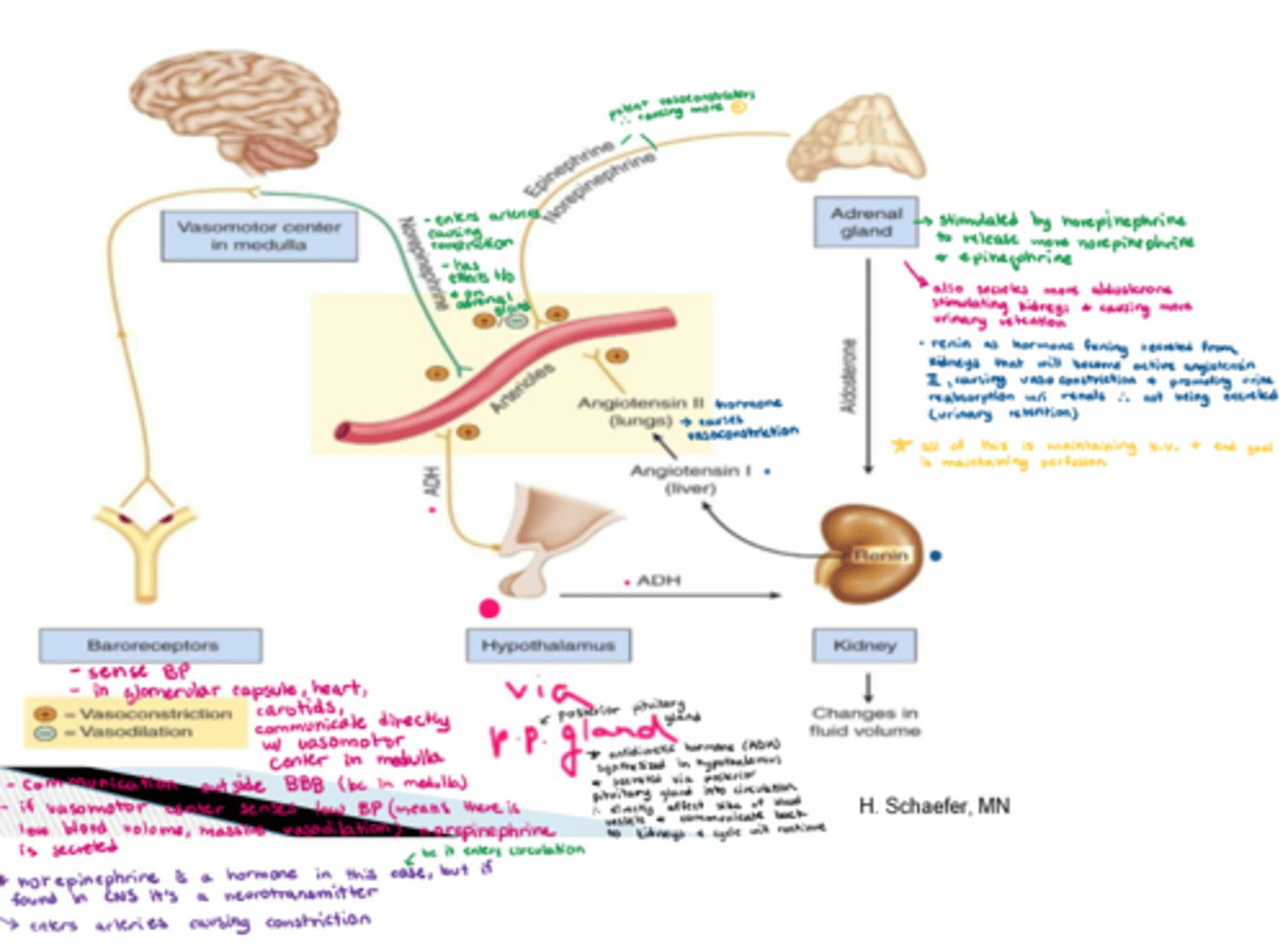
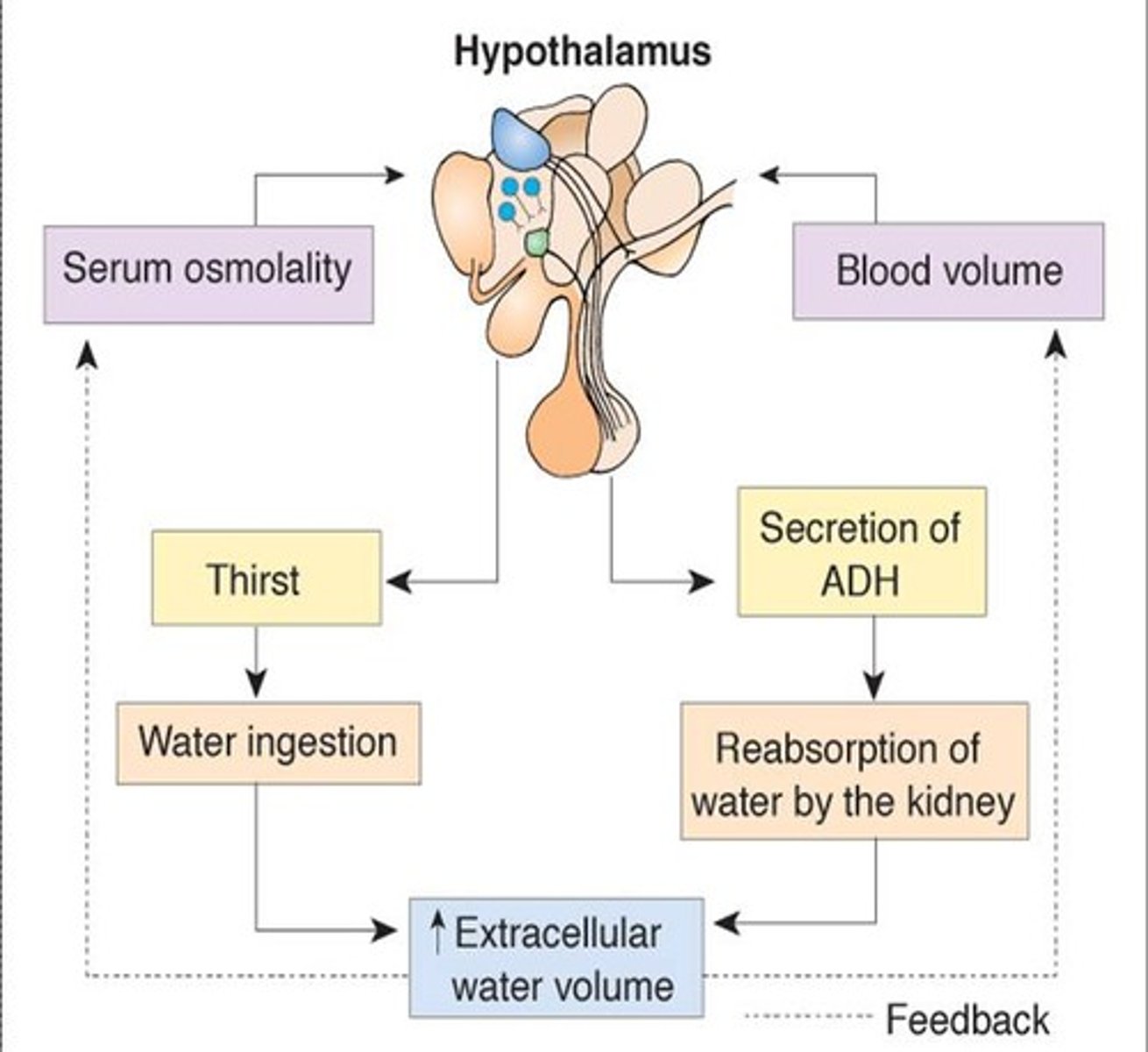
How does ADH control fluid balance regulation? How is renin involved?
1. ADH is synthesized in the hypothalamus and secreted via the posterior pituitary gland
2. ADH secretion stimulates renin in the kidneys (changing fluid vol), which is converted to inactive angiotensin I in the liver, and then active angiotensin II in the lungs. This causes vasoconstriction in the arterioles as well, maintaining perfusion and urine absorption.
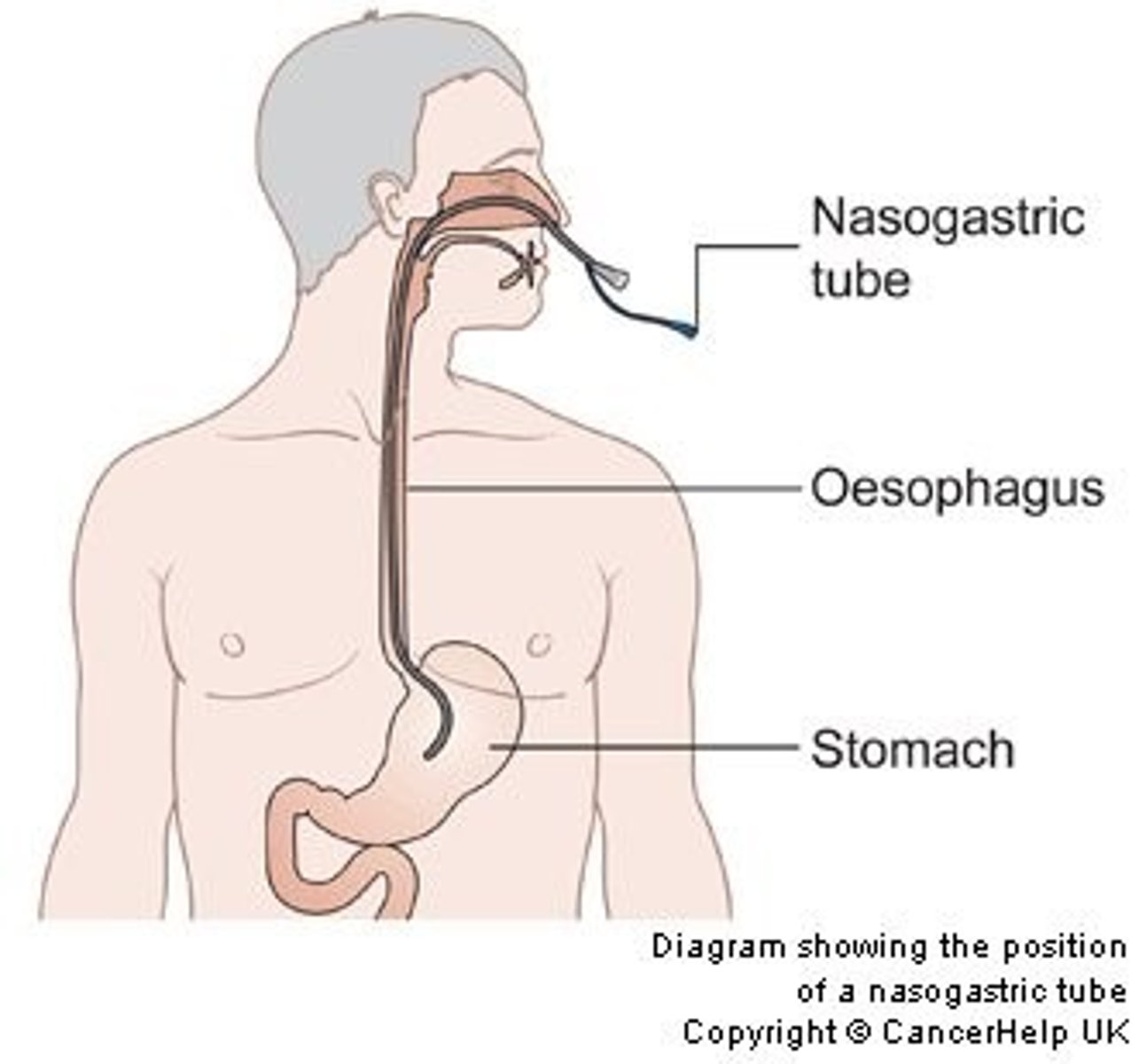
What fluids are usually measured in I/O in clinical?
- Intake: oral liquids, NJ/NG tubes, IV infusions
- Output (vol): urine (hat used to measure), stool, catheter, diaper weight (weight-dry weight of diaper & convert to mL)
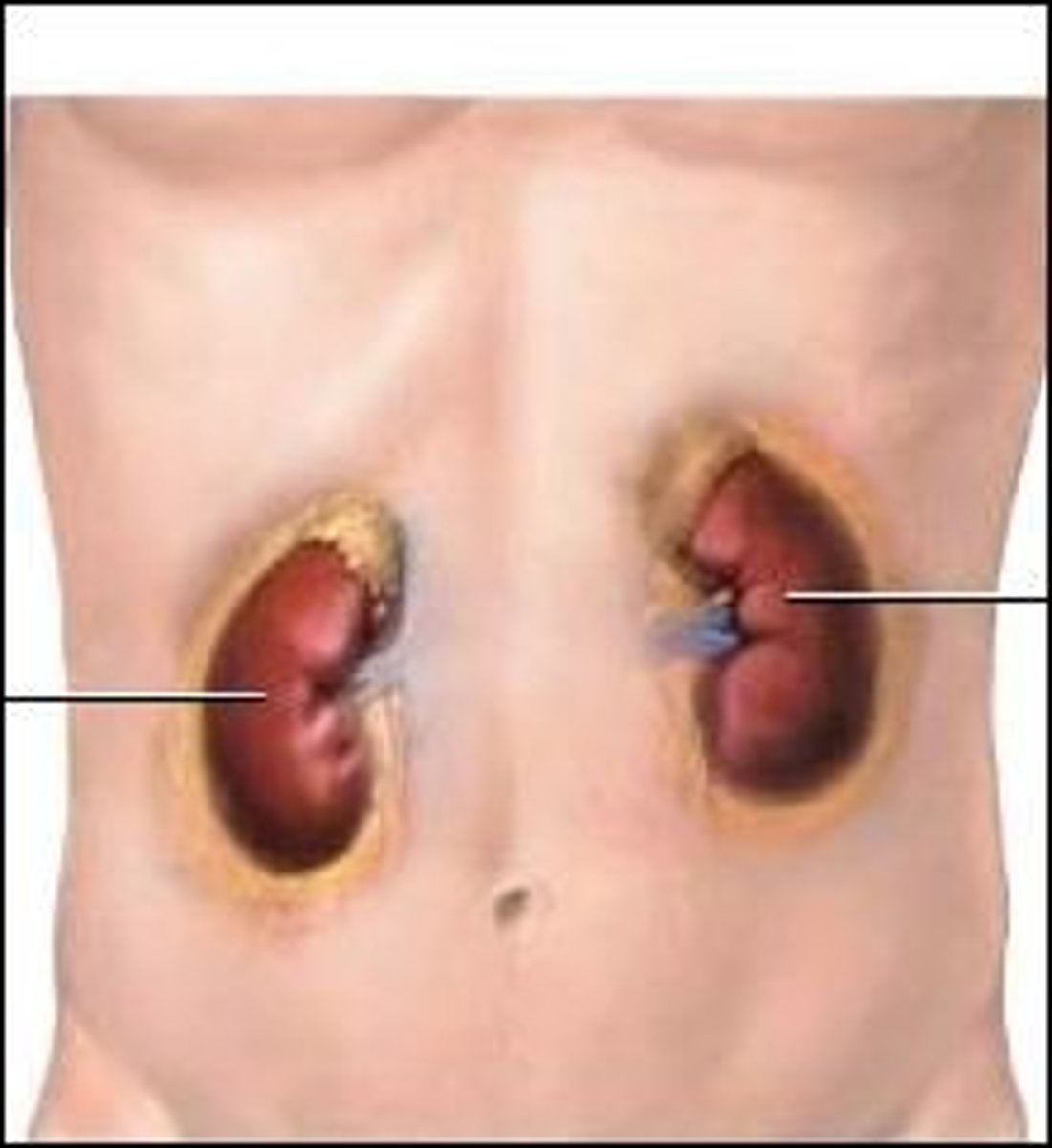
Primary organs of water excretion
- primary: kidneys
- secondary: lungs, liver, skin & sebaceous glands
How much urine is produced per hour?
0.5-1.5mL/kg/hr
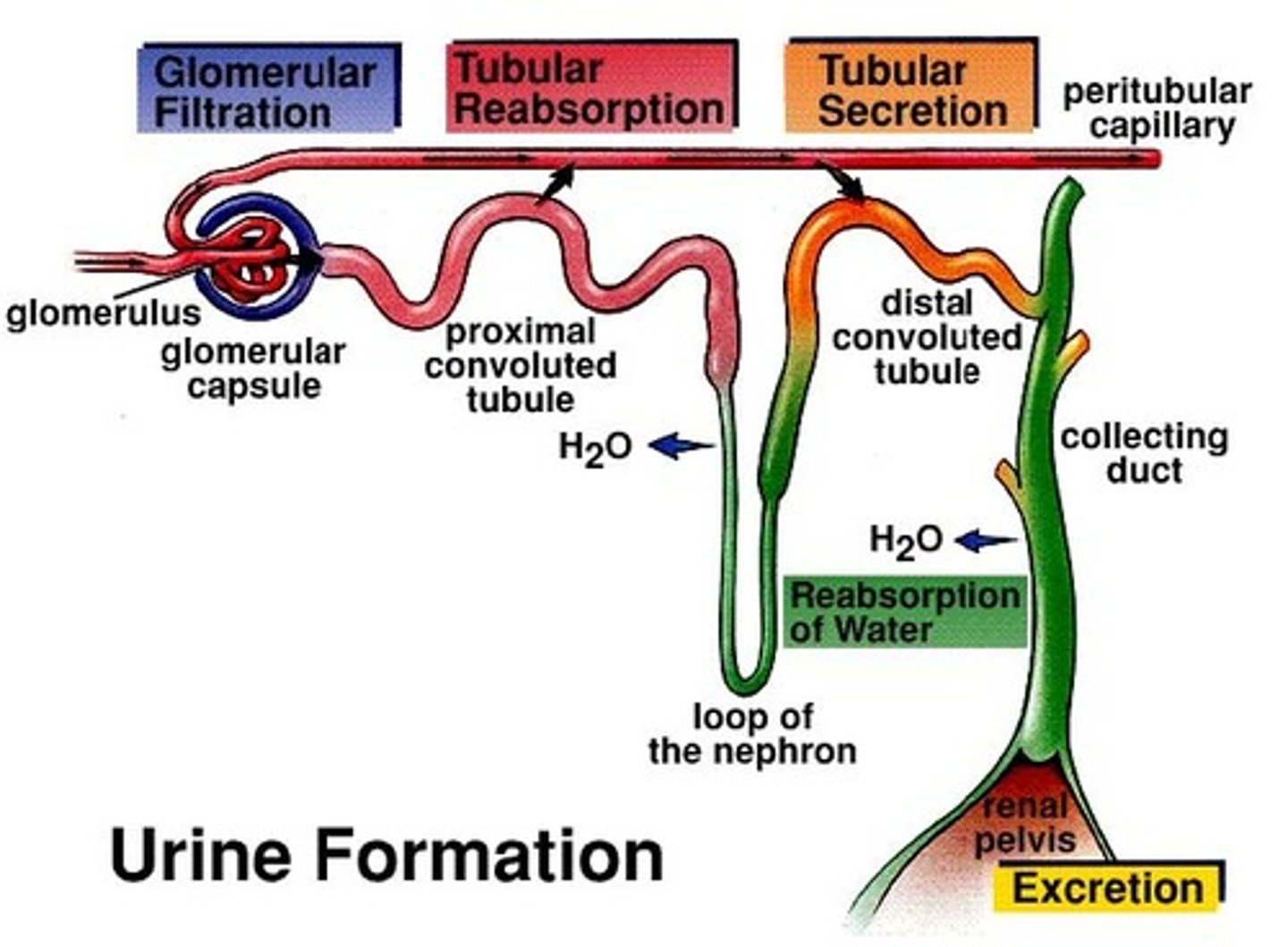
What is osmolality? What is the expected osmolality in blood?
- the concentration of dissolved particles in your blood (can be measured)
- expected osmolality of blood: 275-295 mOsm/kgH20 (around 280 mOsm/kg)
- sodium is a major determinant of osmolality
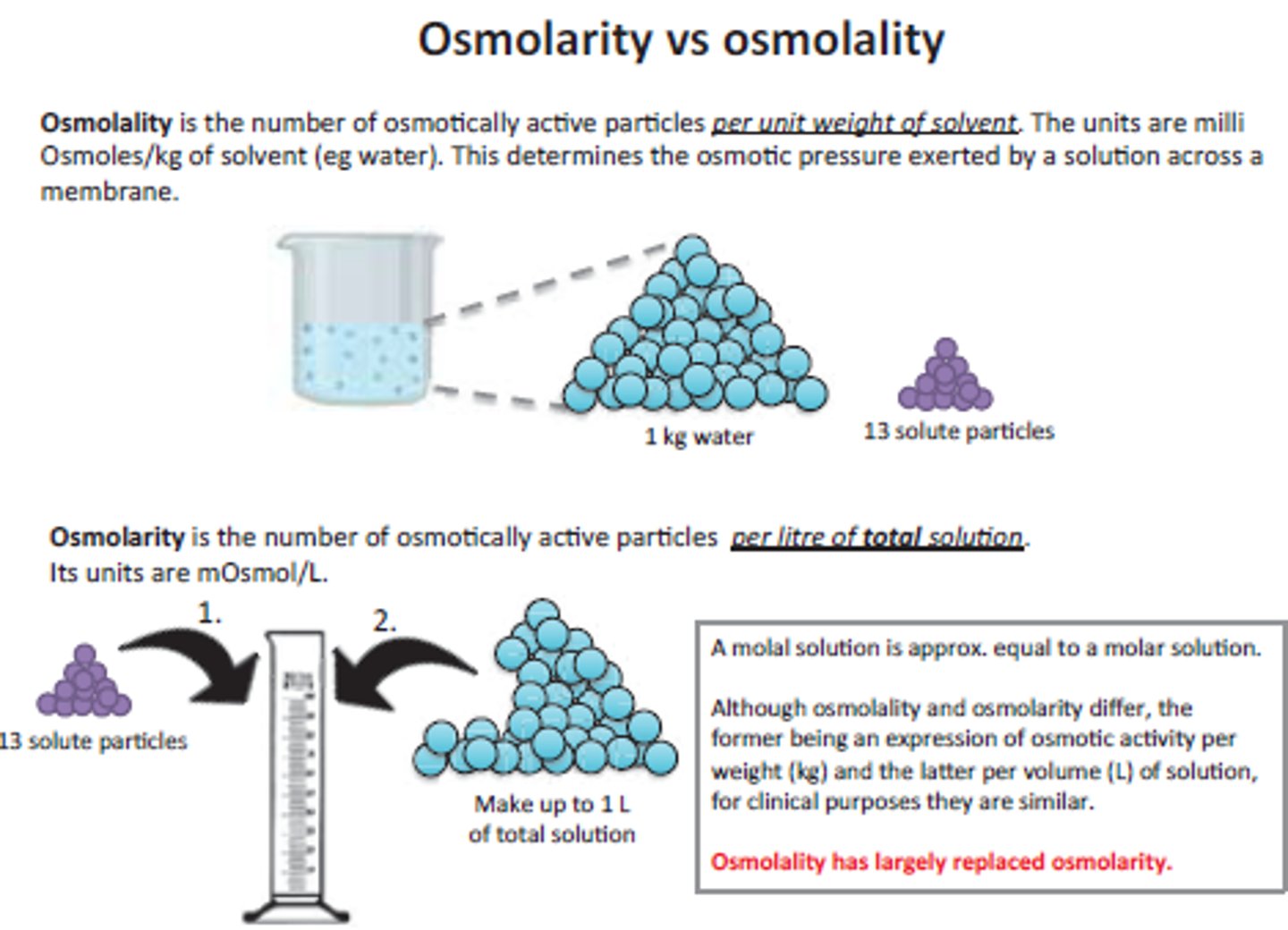
How does osmolality help us determine fluid balance?
- depends on number of dissolved solutes in a fluid
- can include: sodium, glucose & urea (these primarily control H2O balance)
What is the result of change in osmolality? How does this impact water movement?
- changes in osmolality can cause water to move to different compartments
- water moves between circulation and cells via 'osmosis' & aquaporin channels that allow the water to move quickly
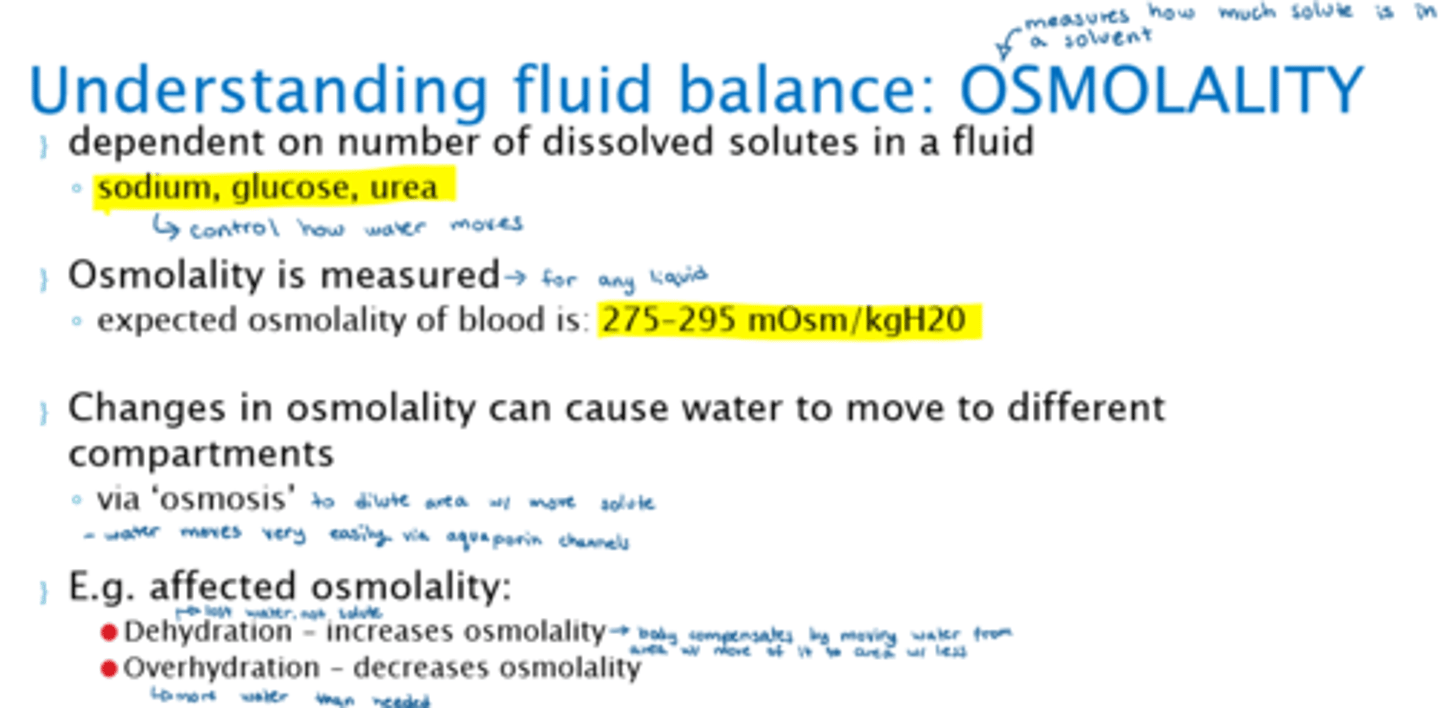
What different clinical factors impact osmolality?
- Dehydration: increases osmolality (b/c only water is lost, not solute)
- Overhydration: decreases osmolality (more H2O, less solute)

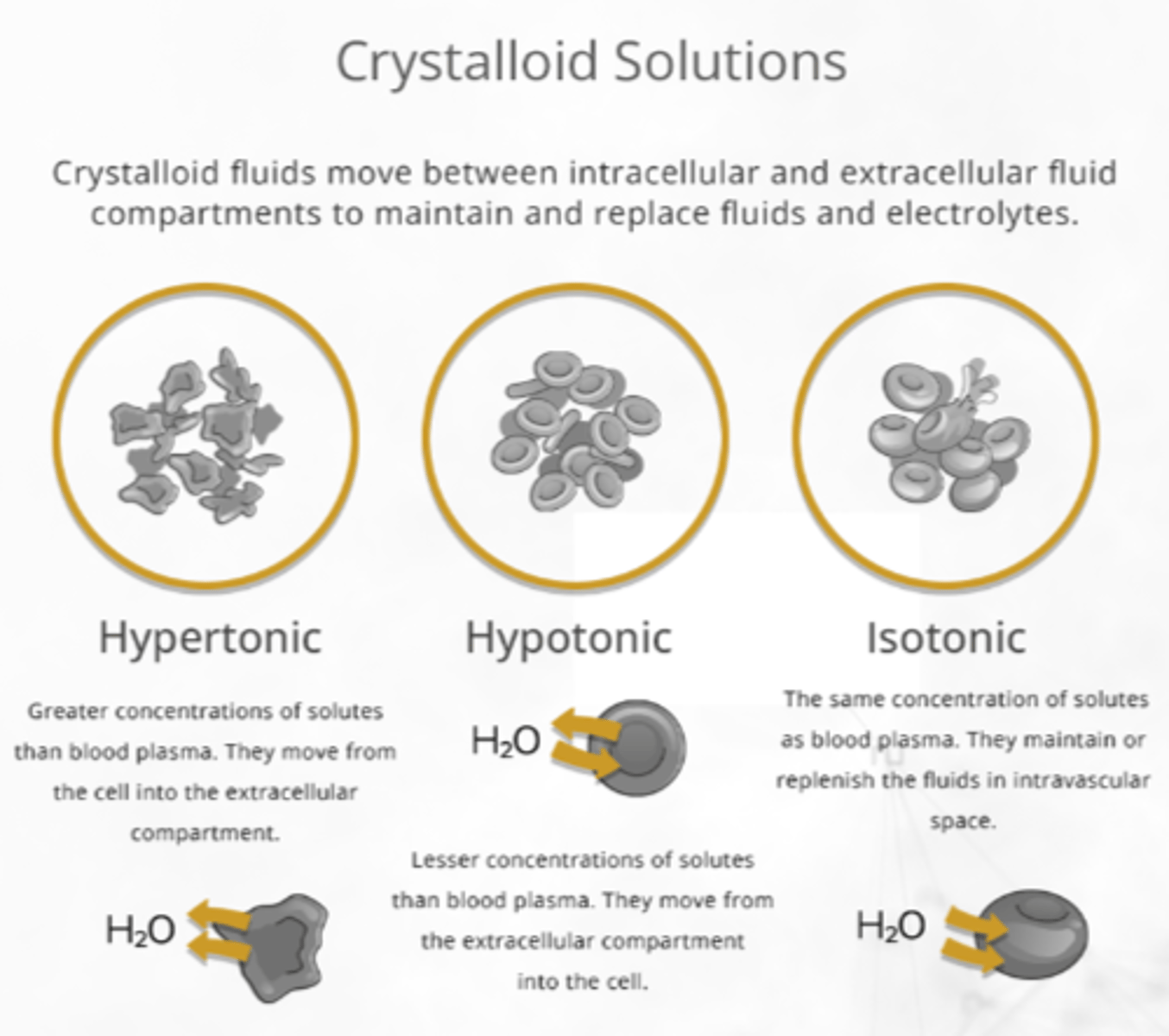
What is 'tonicity'?
- 'tonicity' - is a relative measurement of IV fluid's osmolality
- tonicity will dictate movement of fluid between compartments
What is the goal of IV fluid administration? How does it move throughout the body once administered?
- aims to correct fluid imbalances & maintain homeostasis
- does this via osmosis (moves H2O from low solute to high solute ('dilutes'))
- the correct IV fluid will achieve the desired shift
What are the main solutes within IV fluid tonicity?
sodium & dextrose

What are the different 'tonicity' categories of IV fluids?
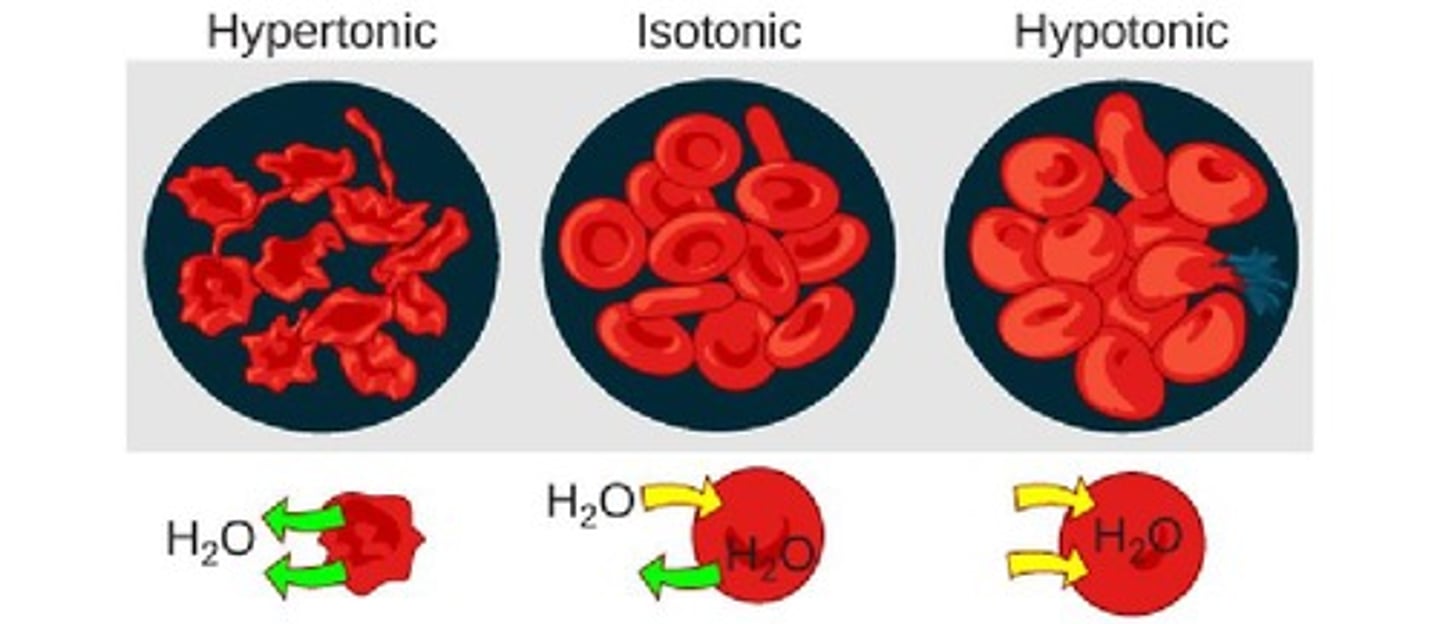
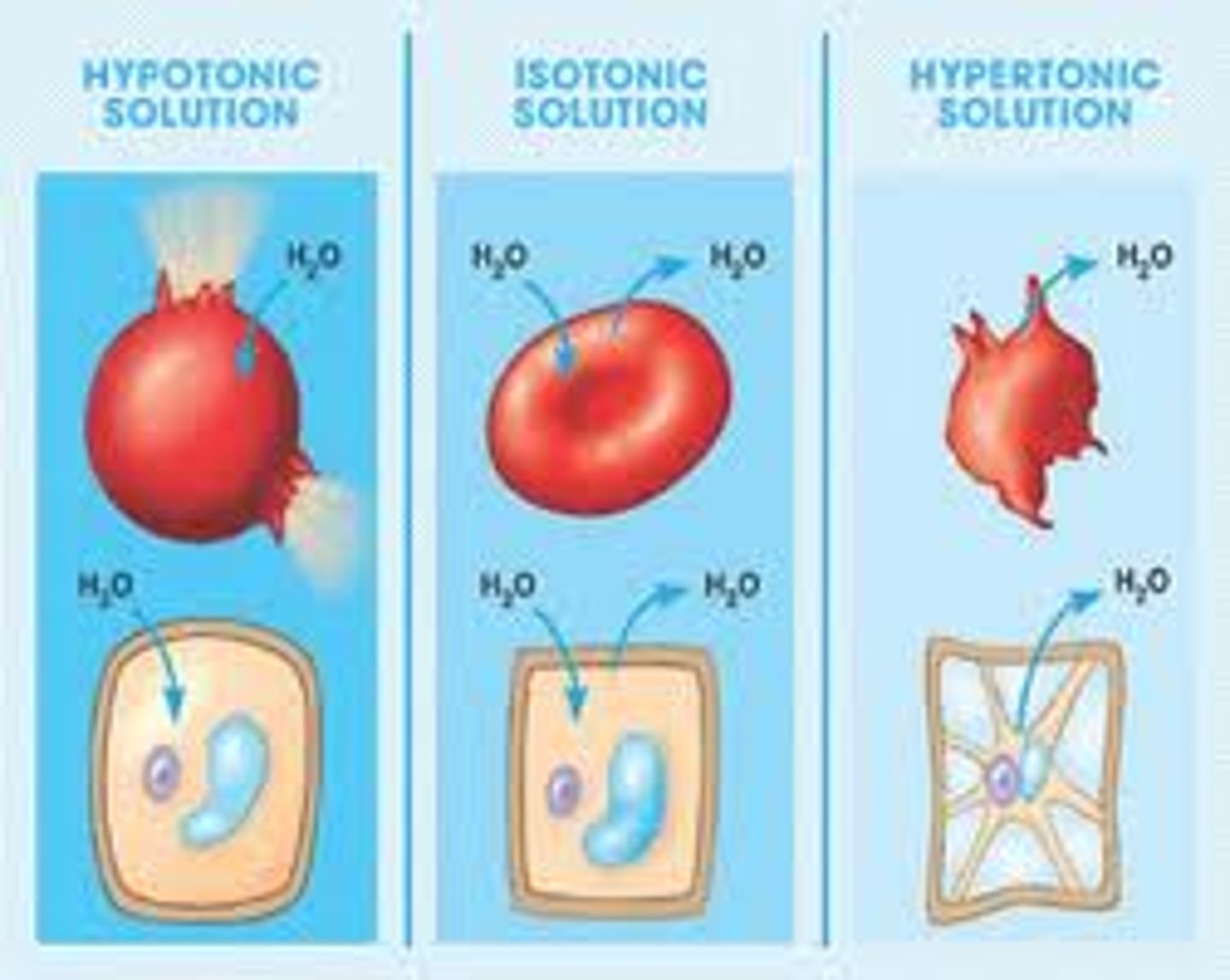
- Isotonic = same as plasma (same osmolality)
- Hypertonic = higher than plasma (more solute)
- Hypotonic = lower than plasma (less solute)
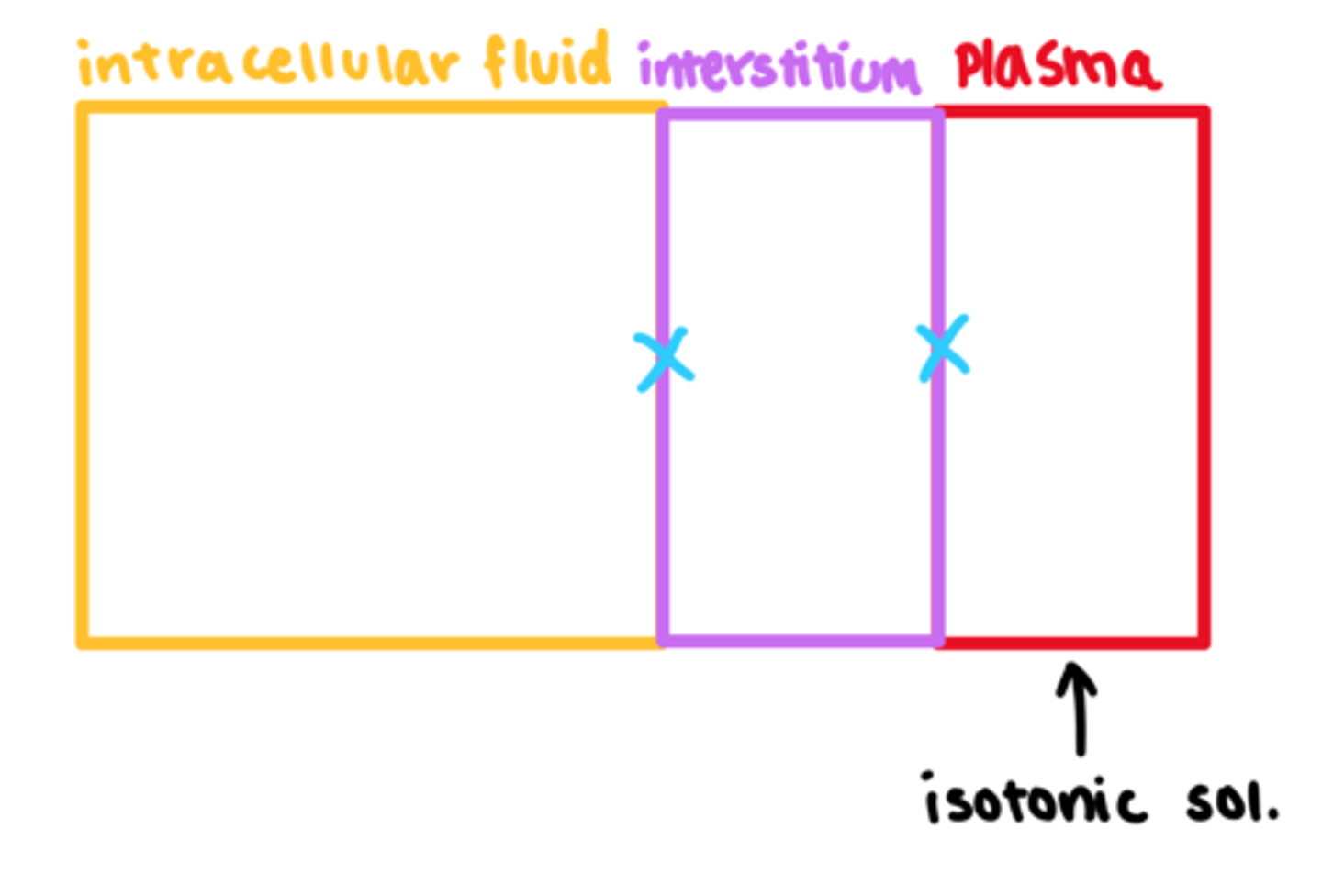
What is an isotonic movement of fluid?
- equal osmolality between fluids in the body
- no net fluid change, therefore normal plasma volume
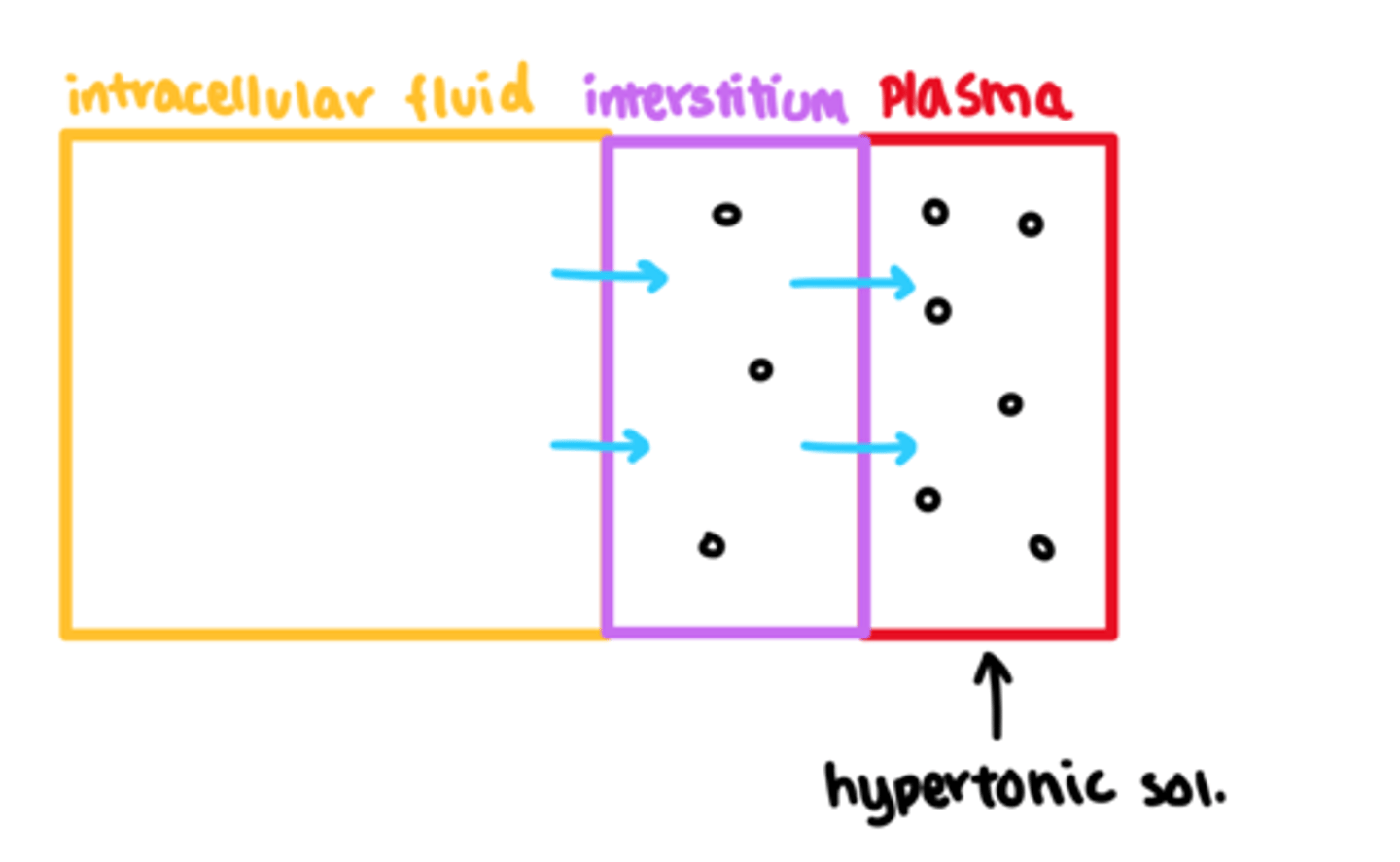
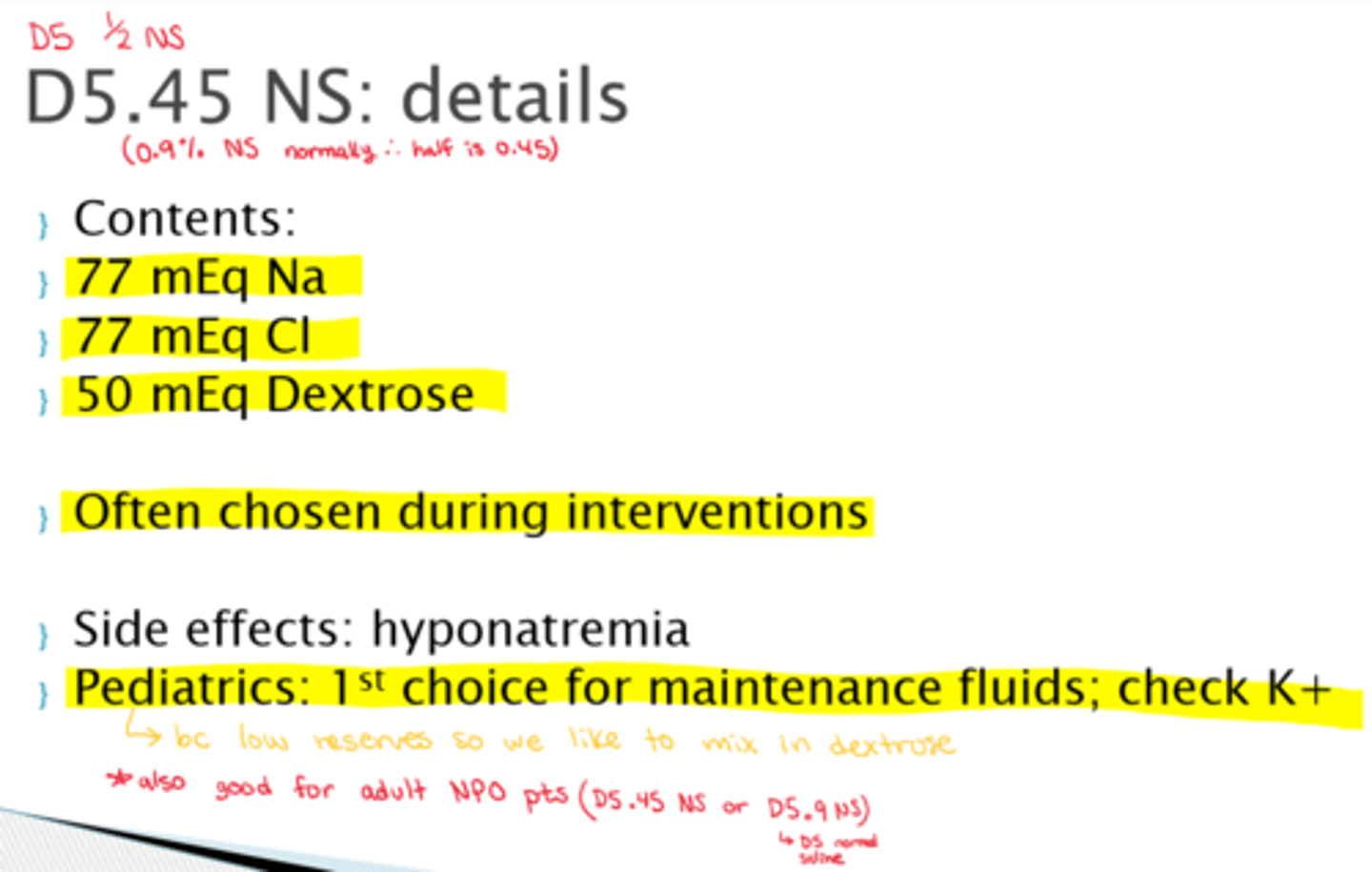
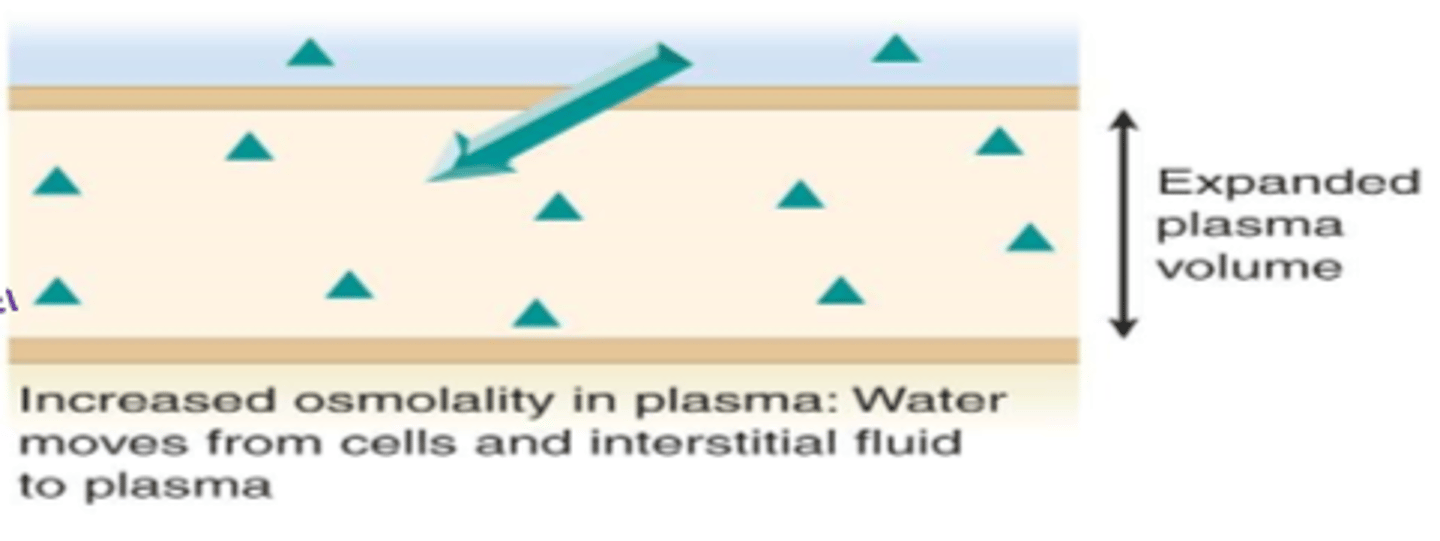
What is a hypertonic movement of fluid?
- increased osmolality in plasma
- water moves from cells and interstitial fluid into plasma
- expanded plasma volume & circulatory compartments
- tissues are losing fluid as water moves out of the cell & enters circulation, causing cell deflation
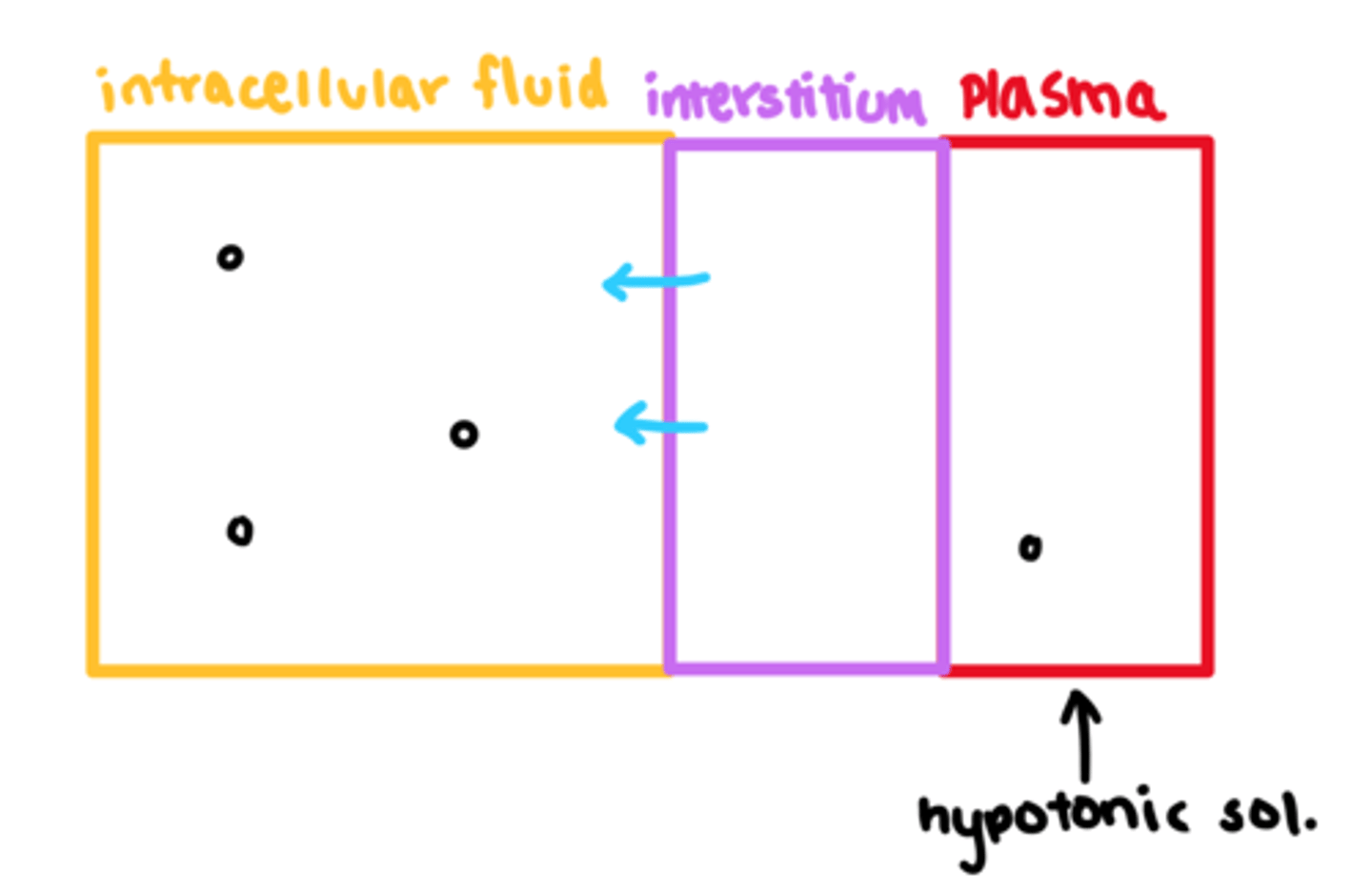
What is hypotonic movement of fluid?
- decreased osmolality in plasma
- water moves from plasma to interstitial fluid and cells
- smaller plasma volume & lack of solute in circulation
- increase in fluid/water in tissues, tissues may swell
How can hypotonicity be an issue for marathon runners?
- due to lack of adequate electrolytes
- overhydration of only water, drawing more water into tissues.
- causes cells to swell or explode
- may even swell in brain => cerebral edema results in increased ICP and possibly death

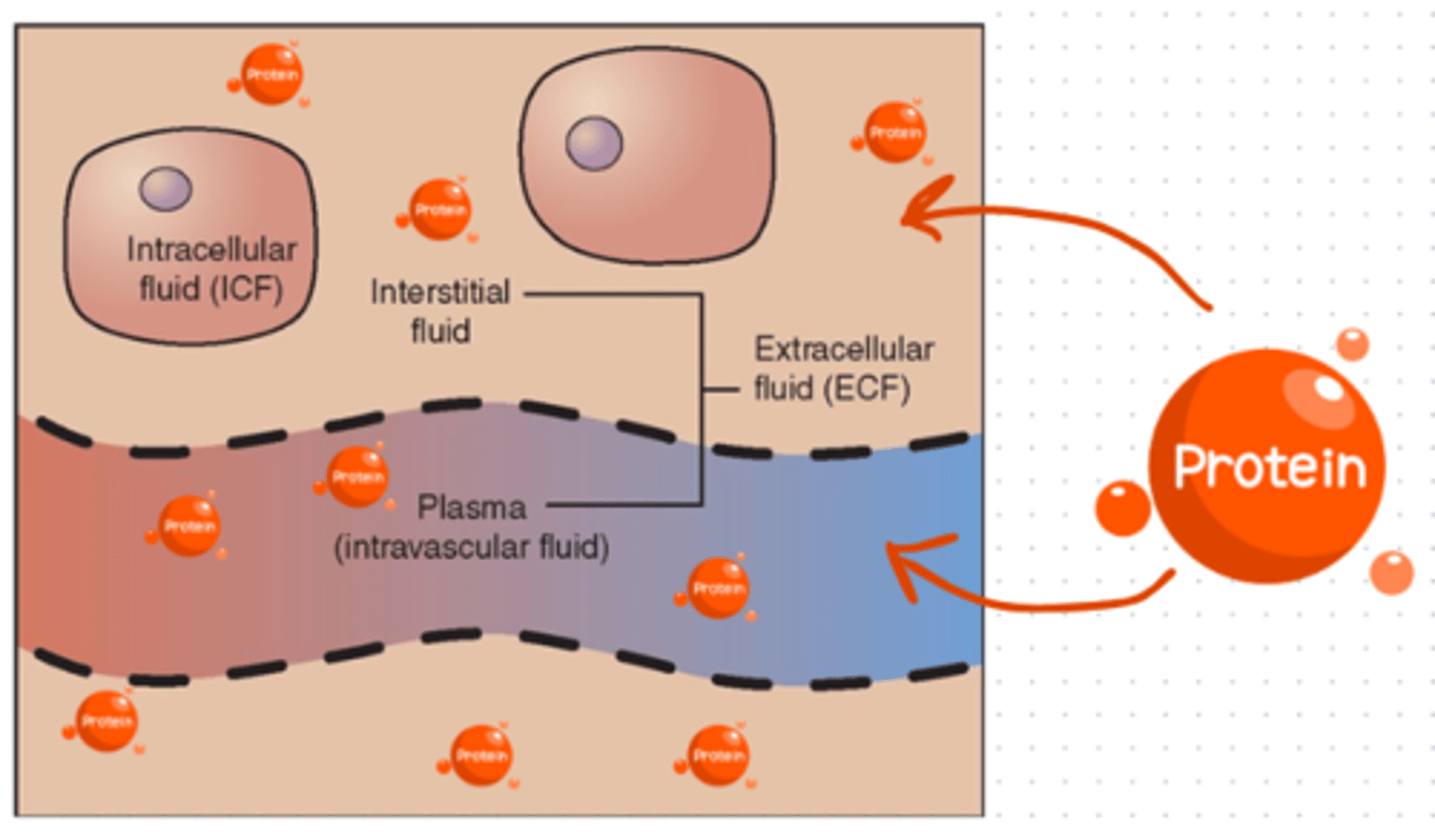
What are the 2 basic categories of IV fluids and how do they move in the body?
1. Colloid fluids = protein based
2. Crystalloid fluids = water based
(Osmosis = water moves by osmosis)

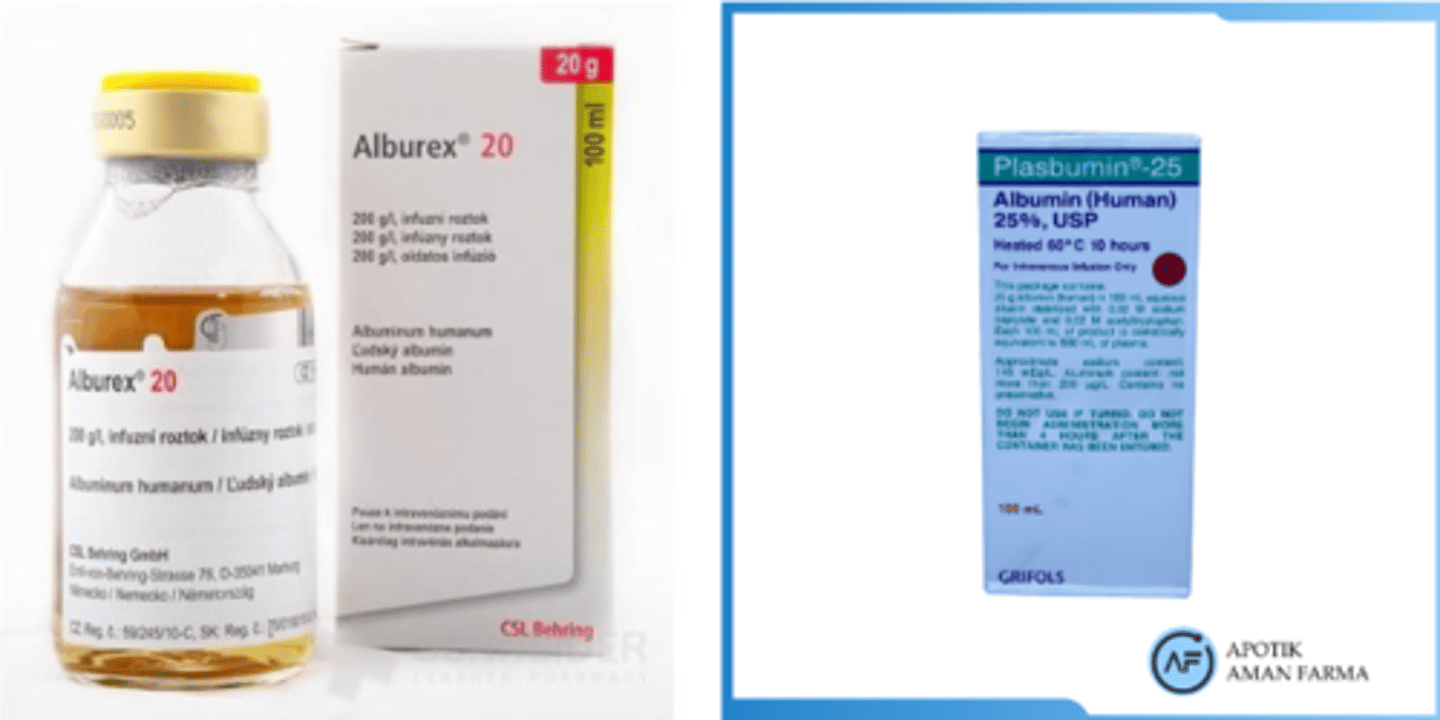
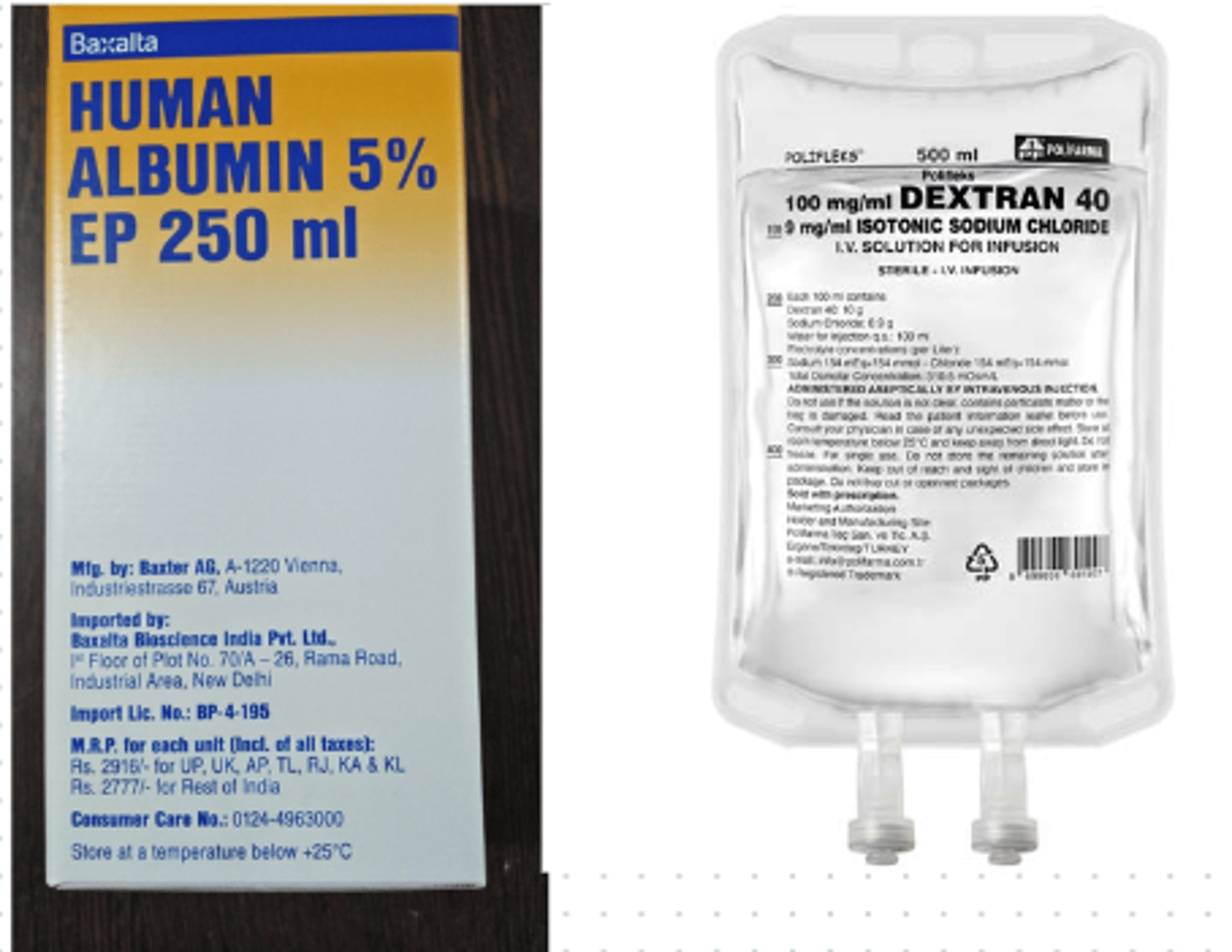
What are colloid IV fluids?
- aka 'plasma expanders' (as they leech water towards them)
- fluids that supply proteins into ECF
- stay in circulation (protein is too large to travel within tissues)
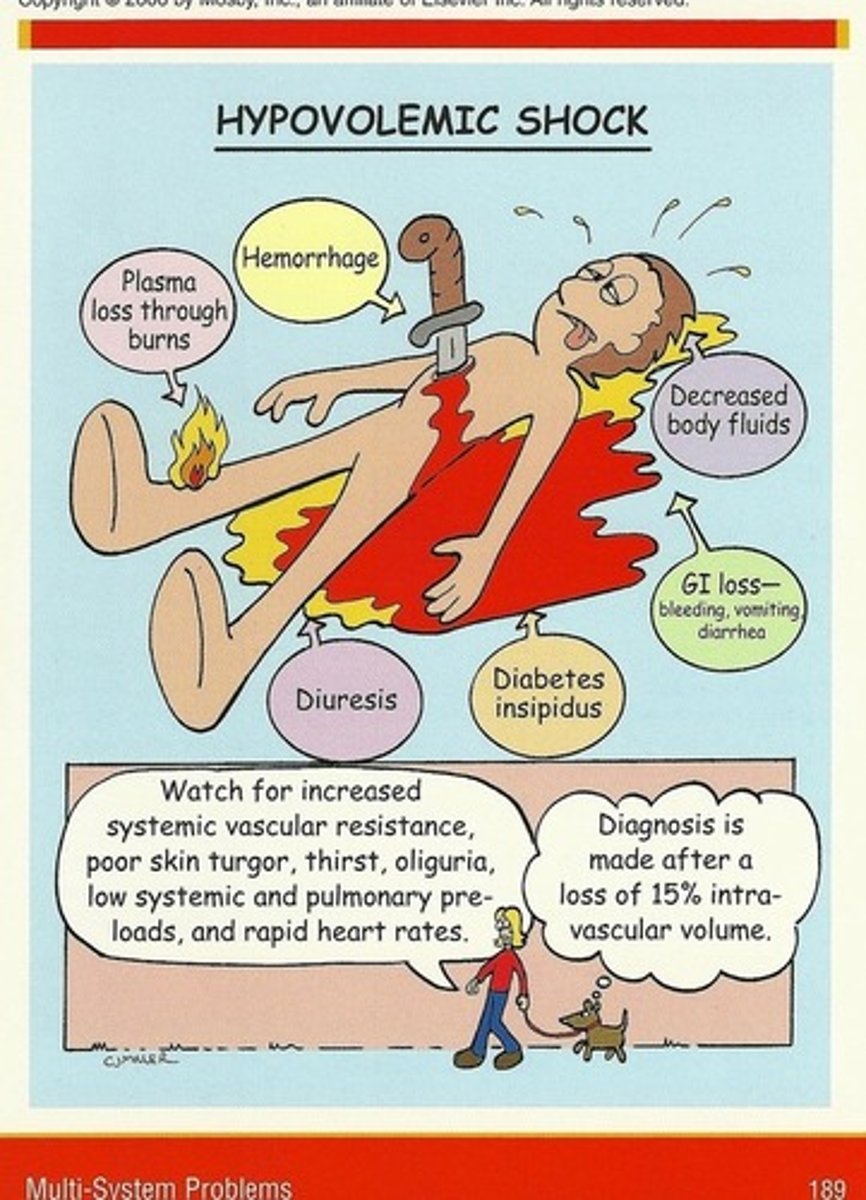
Why should we only use colloid IV fluids for specific tx like hypovolemic shock (colloid used in this case to replace volume lost in low volume shock)?
- contraindicated in most other cases (as we don't want fluid overload)
- due to no pass via capillaries & renal workload (the protein puts pressure on renal excretion)
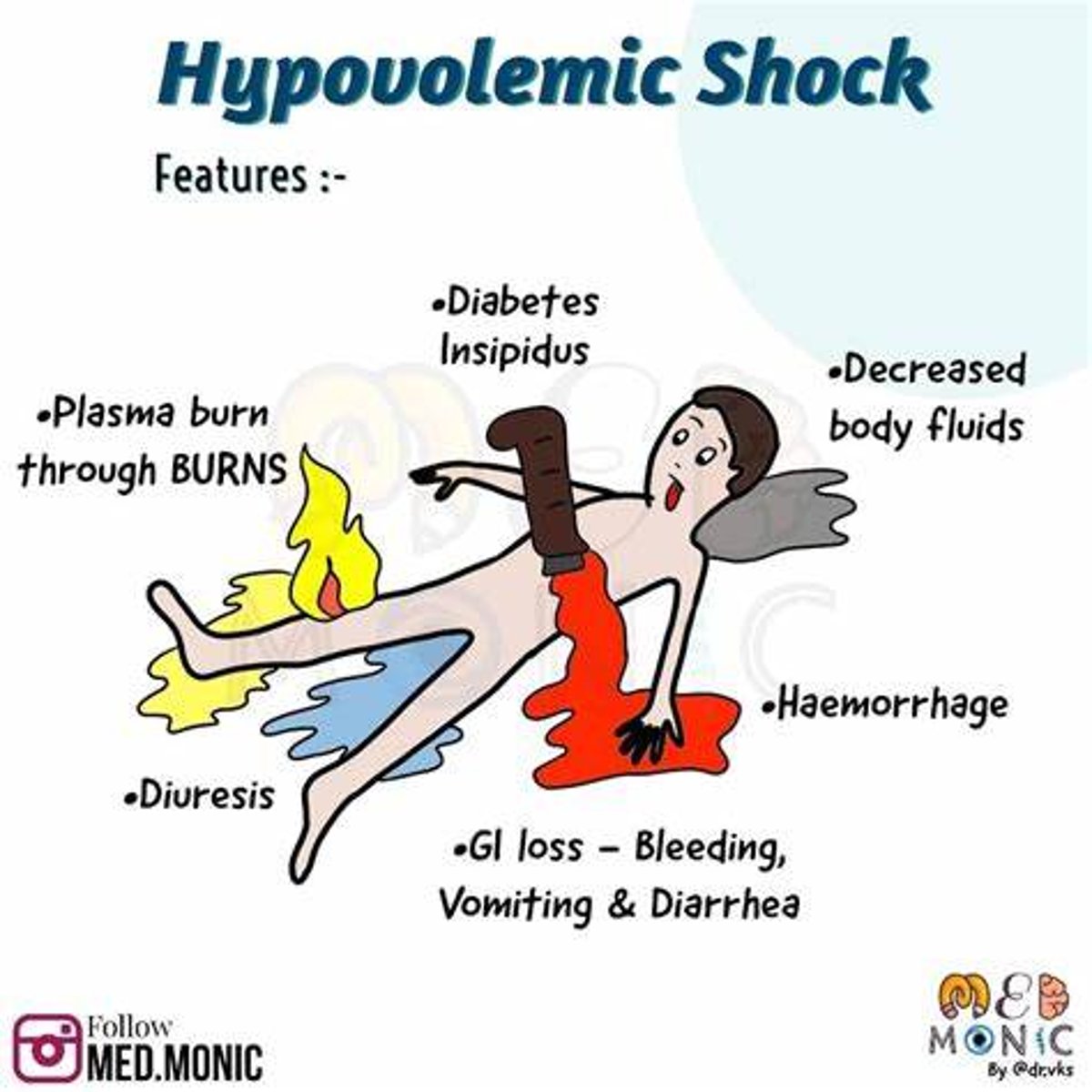
What would be a common tx that requires colloid fluids?
Tx of hypovolemic shock
What are the names of the most common colloid IV fluids?
- Plasbumin
- Alburex
What are crystalloid IV fluids?
- fluids that supply H2O, electrolytes, & other solutes (eg. glucose)
- moves easily btw ECF & ICF, tonicity dictates fluid movement (especially Na+ amount and dextrose)
How can IV fluid tonicity be different in the 'bag' vs the 'body'?
- some fluids behave differently once infused
- due to high protein content (eg. isotonic in the 'bag', but suddenly 'hypertonic in the body' - eg. albumin 5%)
What is dextrose?
- chemically identical to glucose
- primary energy fuel for the body via IV
- quickly metabolized and used as glucose

How does high dextrose levels behave in the IV bag vs in the body?
- in bag: mildly hypertonic (eg. D51/2NS)
- in body: mostly isotonic
=> dextrose is quickly utilized, & remainder fluid becomes isotonic or even hypotonic
What is meant by fluid maintenance?
- fluid maintenance = meeting body requirements
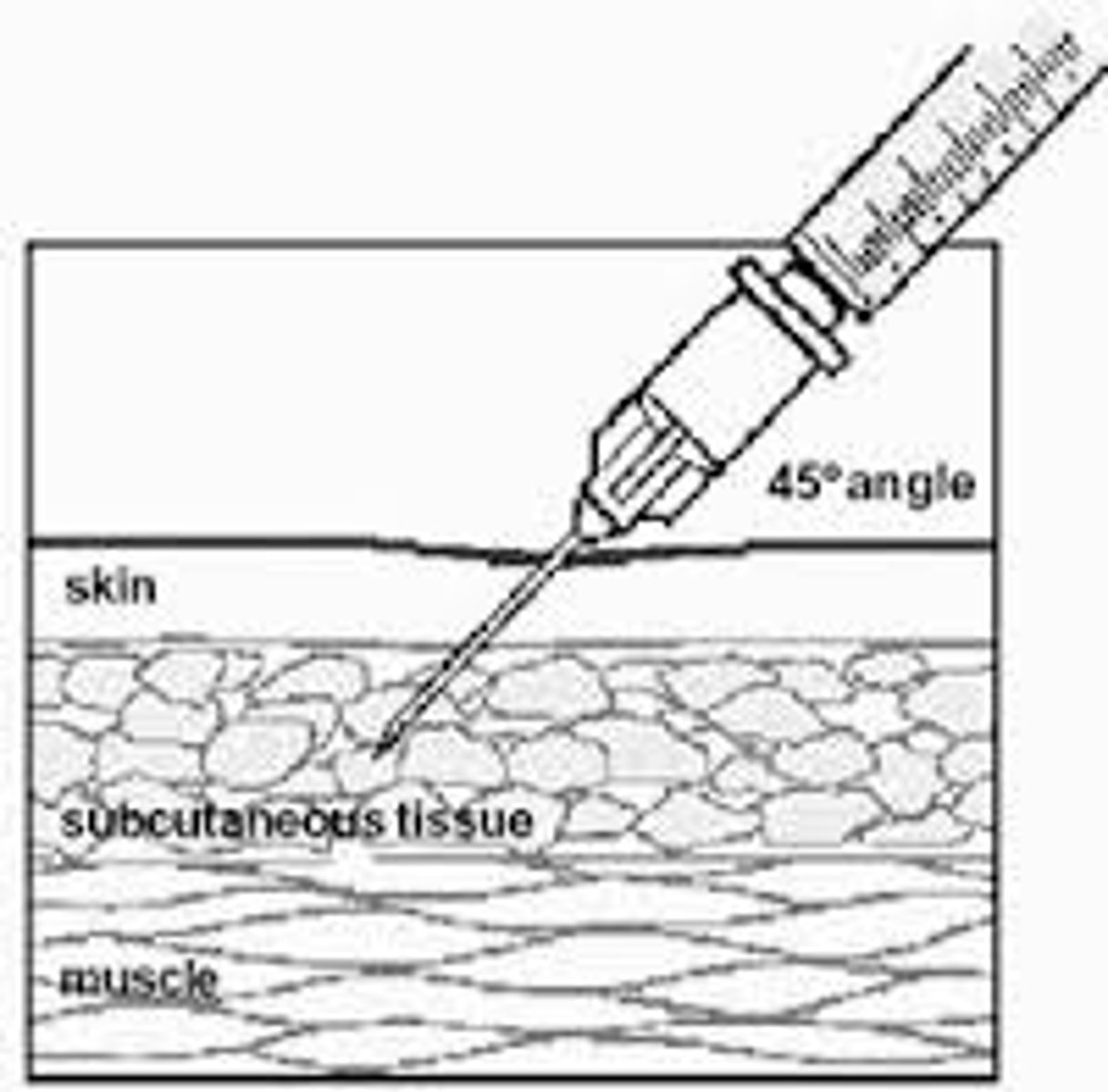
- oral intake (eating/tube feeding), IV infusion, SC infusion (erg. palliative care)
What is meant by fluid resuscitation?
- fluid resuscitation = replacing deficits (fixing a big problem quickly)
- oral if minor; IV if concerning
- goal: adequate perfusion => rescue intravascular volume

What is meant by fluid restriction?
- fluid restriction = restricted fluid intake (eg. high BP => less fluid intake)
- eg. NPO = nothing by mouth, all fluids given IV

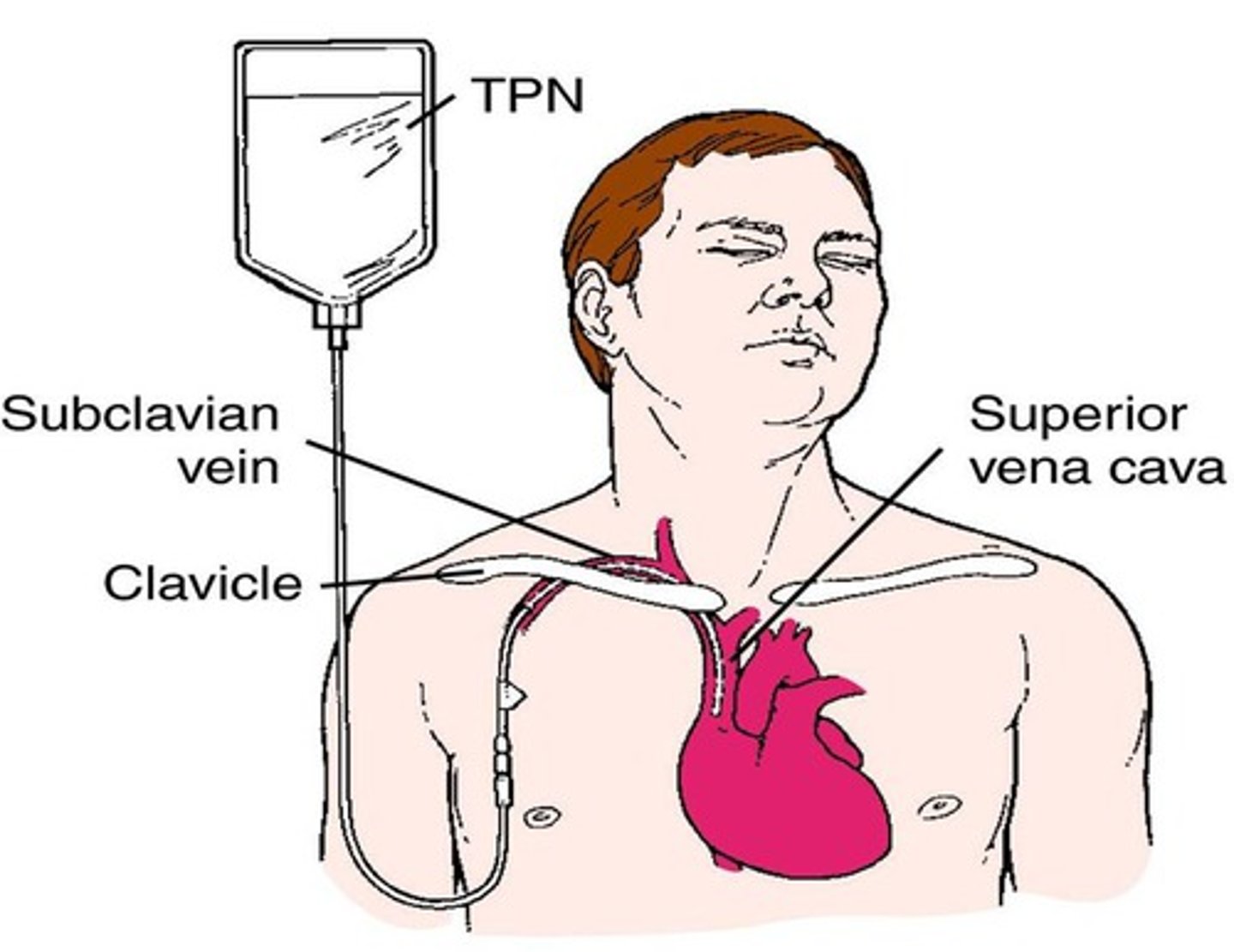
What does TPN stand for?
- total parenteral nutrition
- mostly used for NPO patients post-op, mixed and tailored to pt needs
- pt may have increased BMR b/c of fever, etc
- lipid admin is separate
What are the daily routine fluid maintenance levels?
- 35 ml/kg/day of water (fully grown adult)
- body needs electrolytes: potassium, sodium & chloride
- 50-100 g/day of glucose to limit 'starvation' ketosis => incomplete daily requirement if prolonged (body needs carbs/sugar to burn energy)
- *we are wanting to match these levels to what they should normally intake independently!

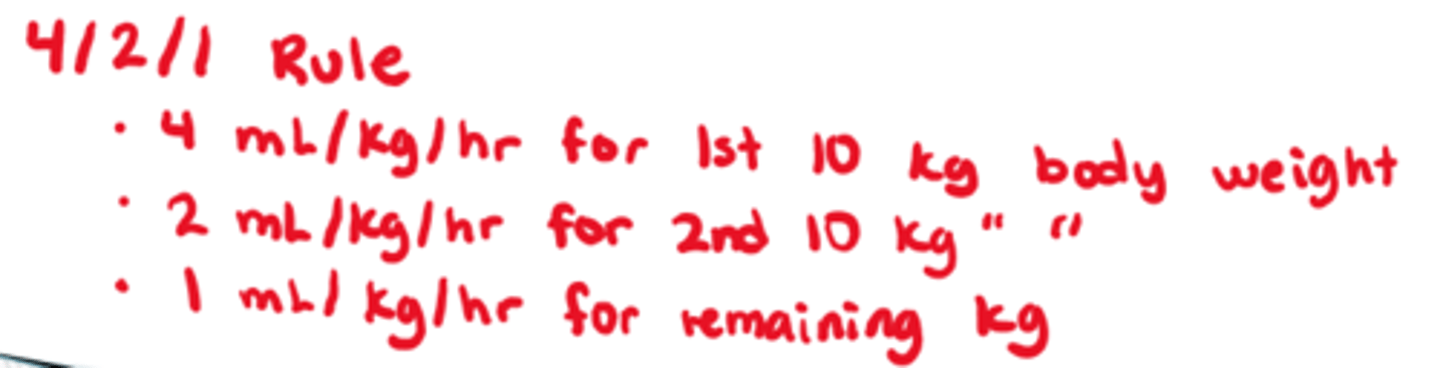
What is the "4/2/1" rule for finding out fluid maintenance needs (ml/kg/hr)
- 4ml/kg/hr for 1st 10 kg of body weight
- 2ml/kg/hr for 2nd 10 kg of body weight
- 1 ml/kg/hr for the remaining kgs
(primarily used for peds calculations, can be used for all pts though)
What are the most common isotonic fluids?
- Lactated Ringer's (aka LR/RL)
- Normal Saline (0.9%) (aka NS/NaCl)

What are the most common isotonic COLLOID fluids?
- 5% Albumin (Colloid) => isotonic in bag
- Dextran 40 (Colloid) => isotonic, however - hypertonic in the body
What is NS (0.9%) overall? Any s/e?
- isotonic IV fluid
- 1st choice resuscitation fluid! => adults 500 mL bolus & reassess
- s/e if long term use (>2 days): hypokalemia, no dextrose! need dextrose for nutrients
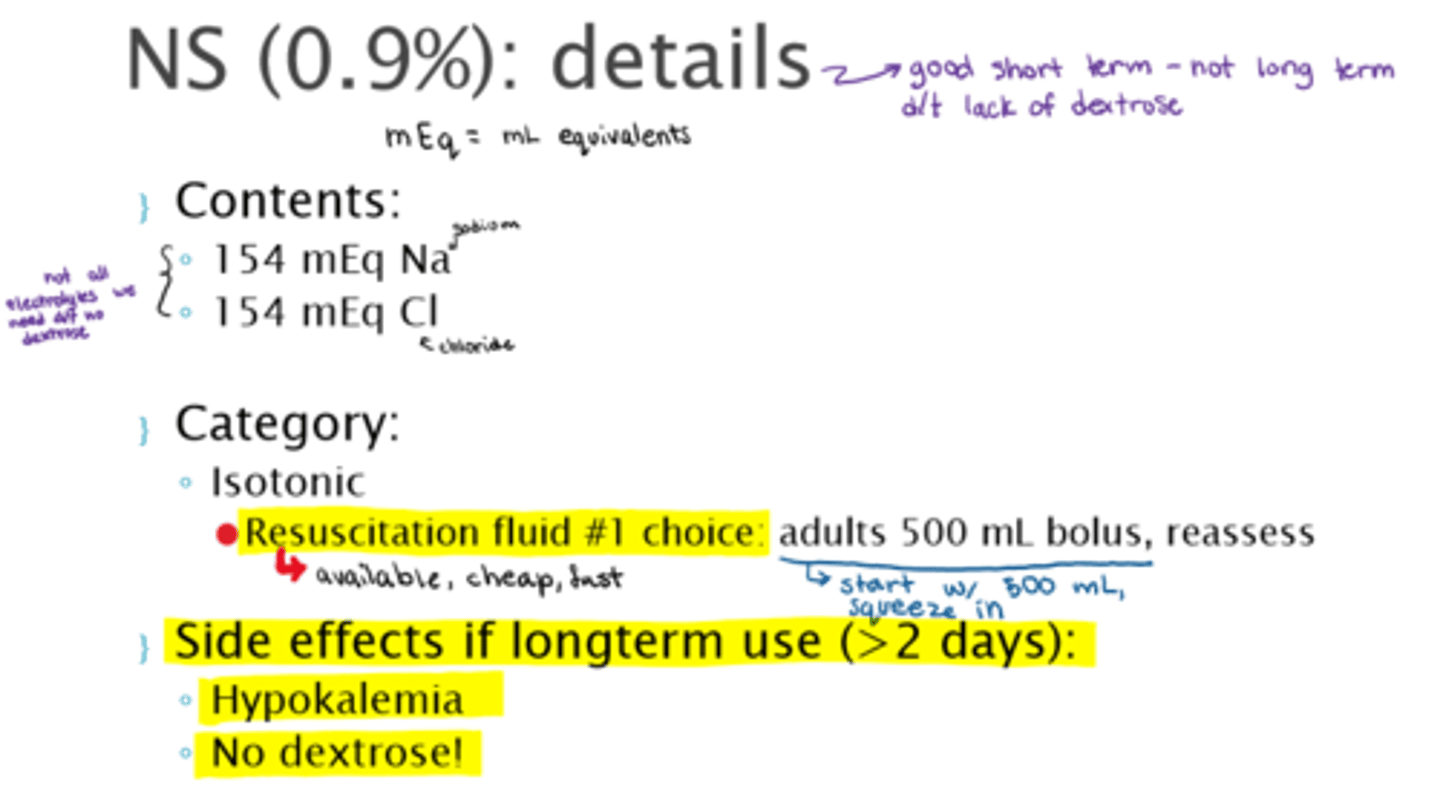
What are the contents that make up NS (0.9%)
- 154 mEq Na
- 154 mEq Cl
- rest sterile water
What is LR overall? Any s/e?
- isotonic IV fluid
- s/e: hyperkalemia, no dextrose
- peds contraindication: high electrolytes for kids (this solution is made for adults)
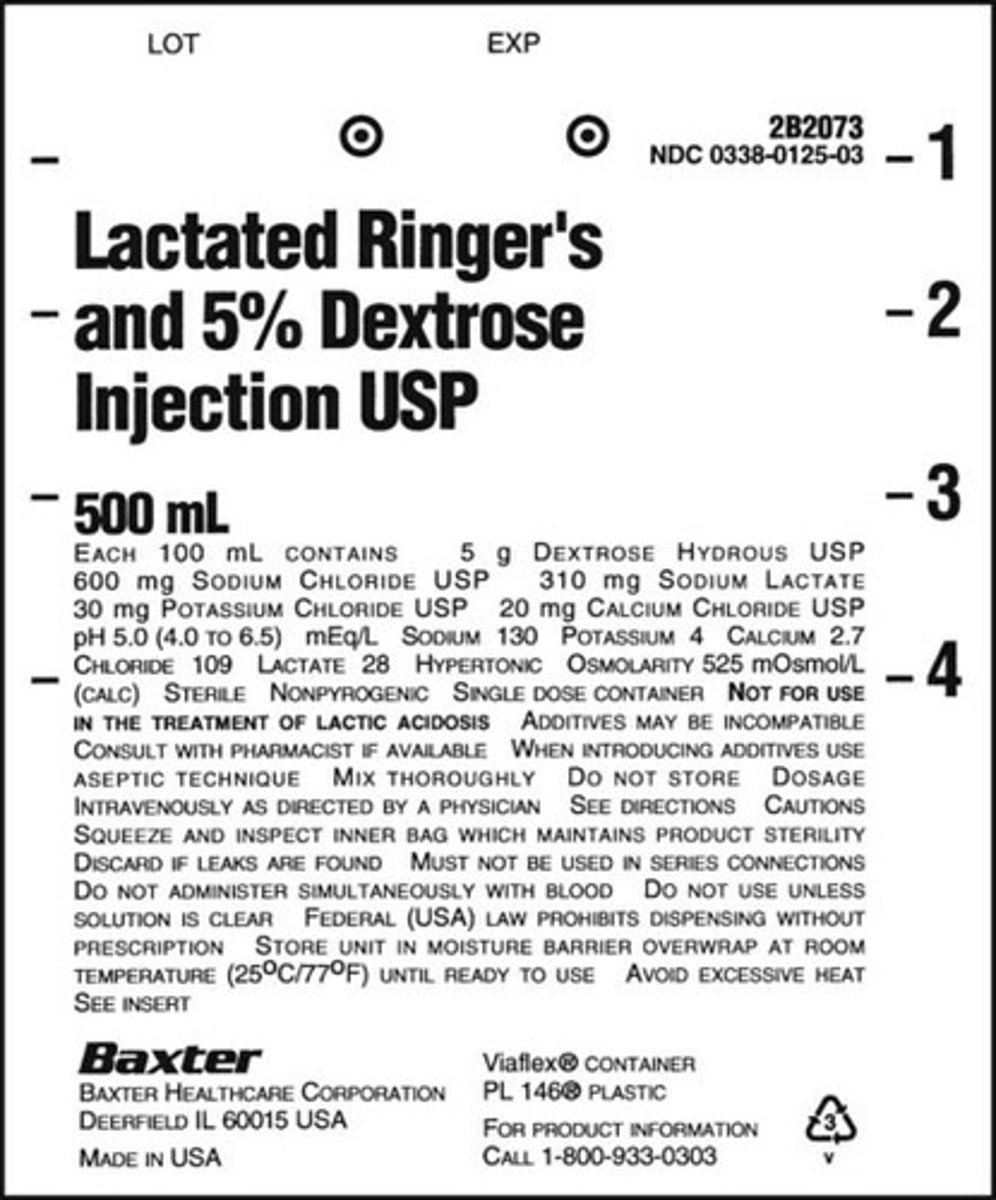
What are the contents that make up LR? How is it different from NS (0.9%)?
- Na 130 mEq
- Potassium 4 mEq
- Calcium 2.7 mEq
- Chloride 109 mEq
- Lactate 28 mEq
(**more electrolytes than NS 0.9%)
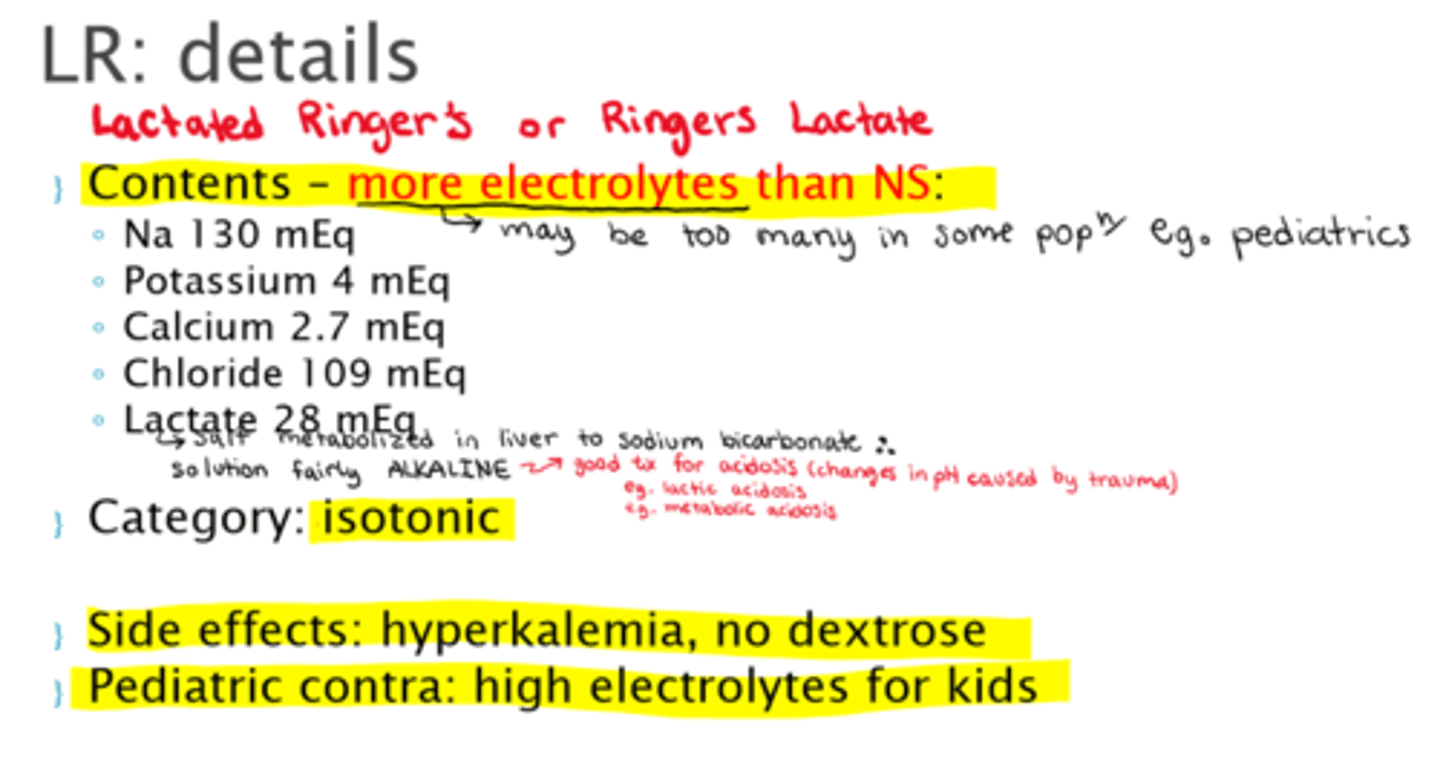
What is Lactate 28 mEq used for in LR IV fluids?
- a lactate salt that is metabolized in the liver into sodium lactate, to decrease acidity within the body
- high alkaline content, good for fluid resuscitation pts that also need pH restored

What are the most common hypertonic fluids (fluid out of cells)?
** have high glucose, high sodium, or both (or colloid)
- D5NS
- D5LR
- D10W
- D5 0.45%NaCl (D5 ½NS)
- 3%NaCl
- 25% Albumin
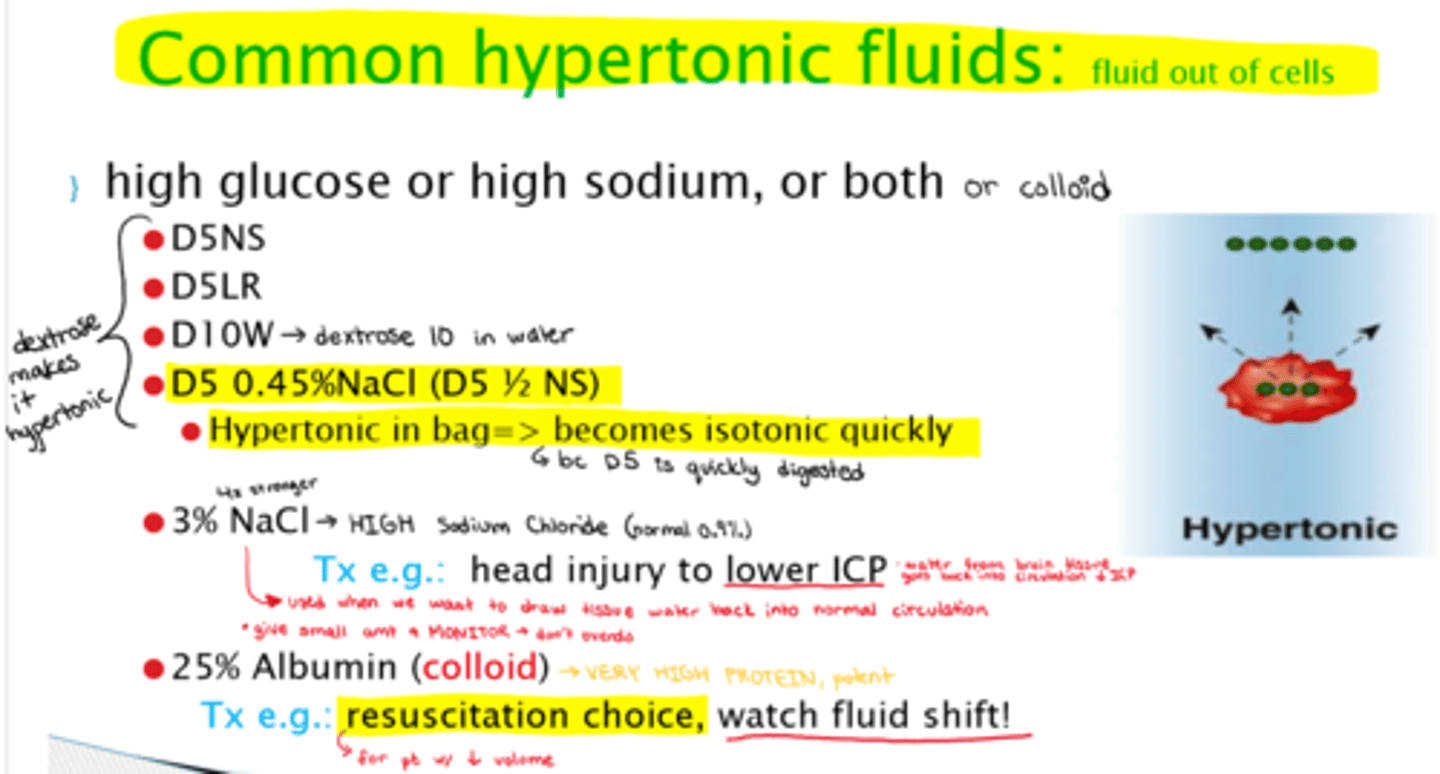
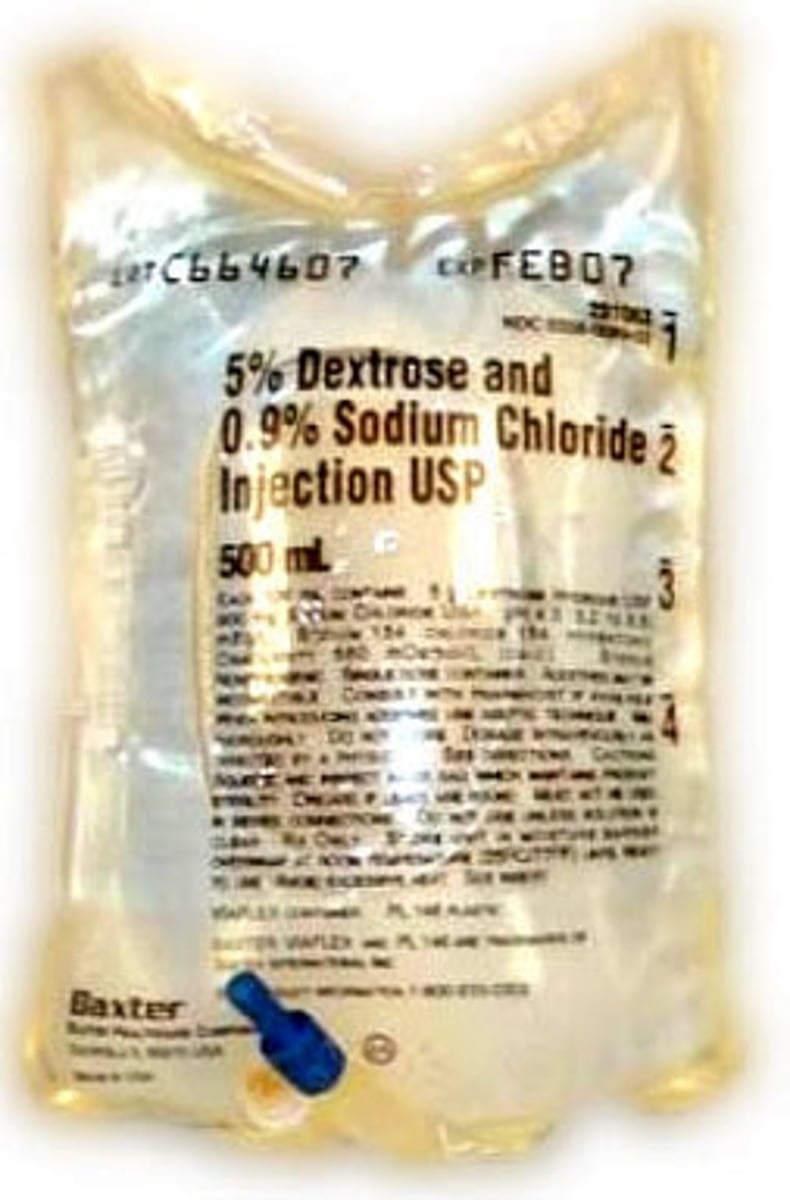
How is D5NS hypertonic
- NS is an isotonic fluid, uses addition of dextrose to make hypertonic
How is D5LR hypertonic
- LR are isotonic, dextrose addition used to make hypertonic
What is D10W
- dextrose 10% in water
- stronger admin of dextrose, therefore super hypertonic

What is D5.45 NS overall (aka D5 ½NS)? Any s/e? Why is it a good choice for peds?
- hypertonic infusion in bag => becomes isotonic quickly in body
- often chosen during interventions (good for NPO patients)
- s/e: hyponatremia
- peds: 1st choice for maintenance fluids b/c peds have lower reserves (note: check K+ levels)
What are the contents that make up D5.45 NS?
- Na => 77 mEq
- Cl => 77 mEq
- Dextrose => 50 mEq
What is 3% NaCl? What would we use it to tx?
- very strong dose of NS, hypertonic
- tx eg: head injury, tx to decrease ICP
What is 25% Albumin? What would we use it to tx? Any s/e?
- hypertonic colloid infusion (potent!)
- tx eg: resuscitation choice (watch fluid shift! => lots of H2O migration from tissues)
What are the contents that make up 25% Albumin (colloid)?
- 25% albumin
- up to 160 mEq Na
*high protein
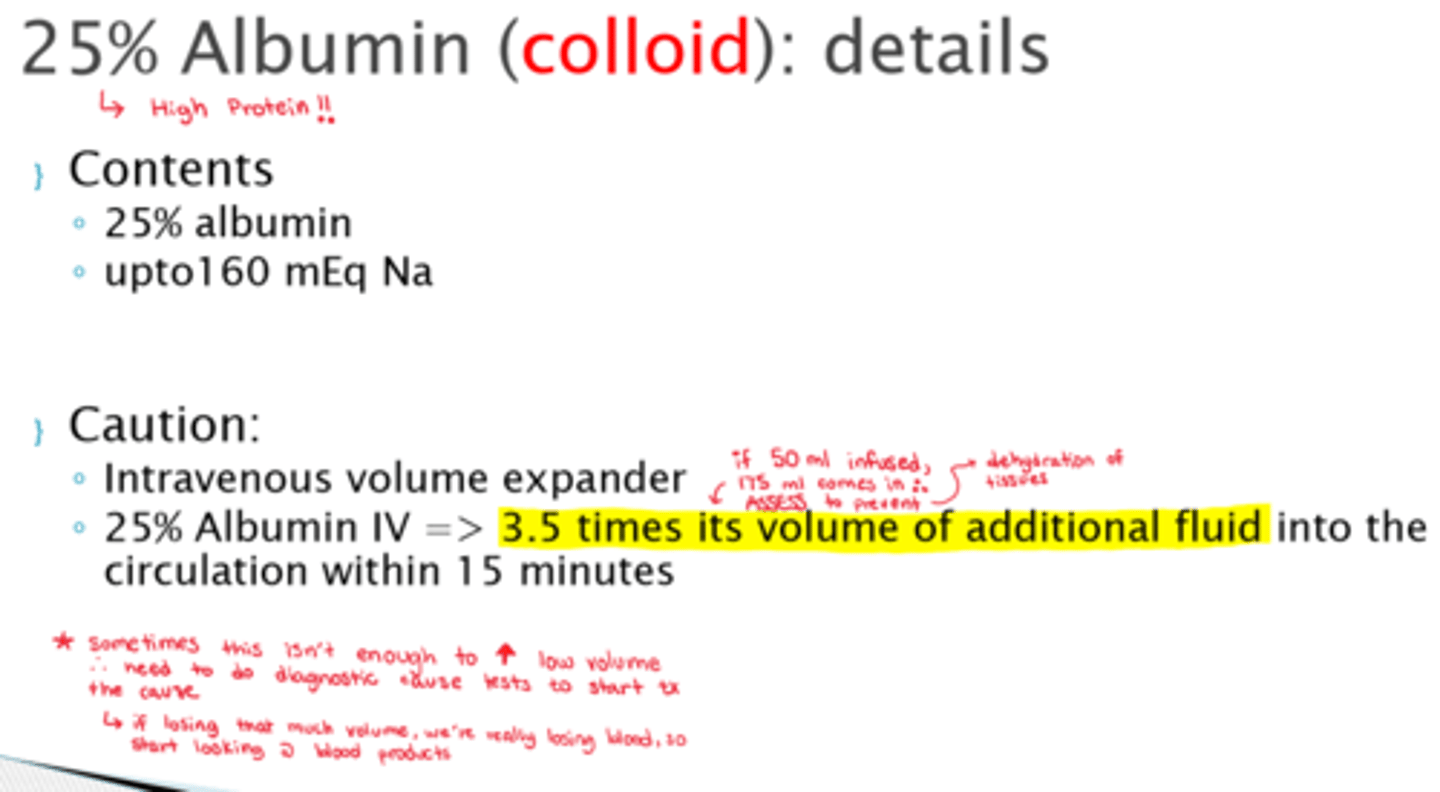
What do we need to watch out for with the admin of 25% Albumin?
- IV volume expander, therefore:
- 25% Albumin IV => once in body, 3.5x its volume of additional fluid into the circulation within 15 minutes! Make sure not to dehydrate tissues
- watch BP maintenance

What are the most common isotonic/hypotonic fluids (fluid into cells)?
- D5 0.2% NaCl (isotonic in bag, hypotonic in body)
- D5W (isotonic in bag, hypotonic in body)
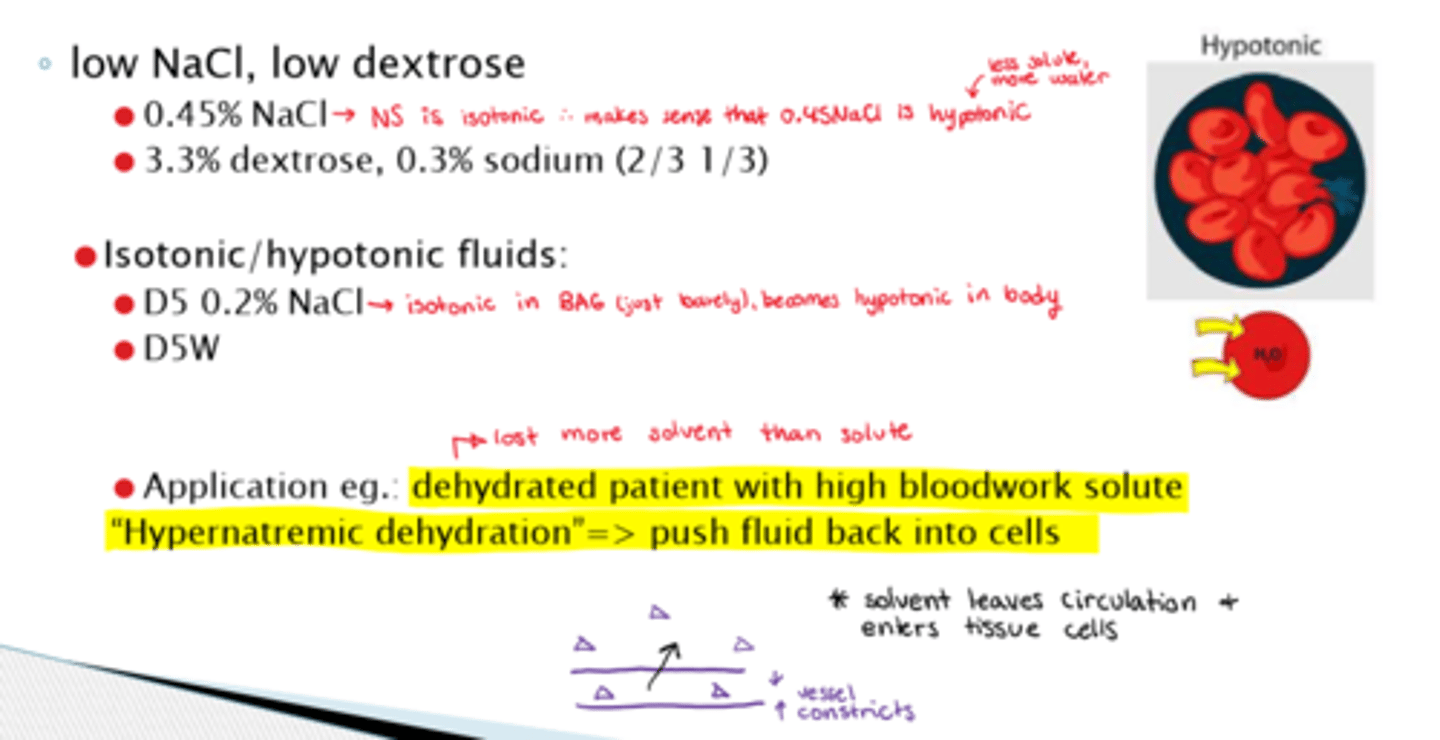
What are the most common types of low NaCl/low dextrose IV fluids?
- 0.45% NaCl (½ NS => hypotonic)
- 3.3% dextrose, 0.3% sodium (2/3 1/3))
What is a good example of why we would admin a hypotonic IV fluid?
- eg: dehydrated patient with high bloodwork solute - this is known as: "Hypernatremic dehydration"=> want to push fluid back into cells

Main causes of an upper GI bleed
- peptic ulcers
- esophageal varices (enlarged/dilated blood vessels in esophagus)
- esophagitis
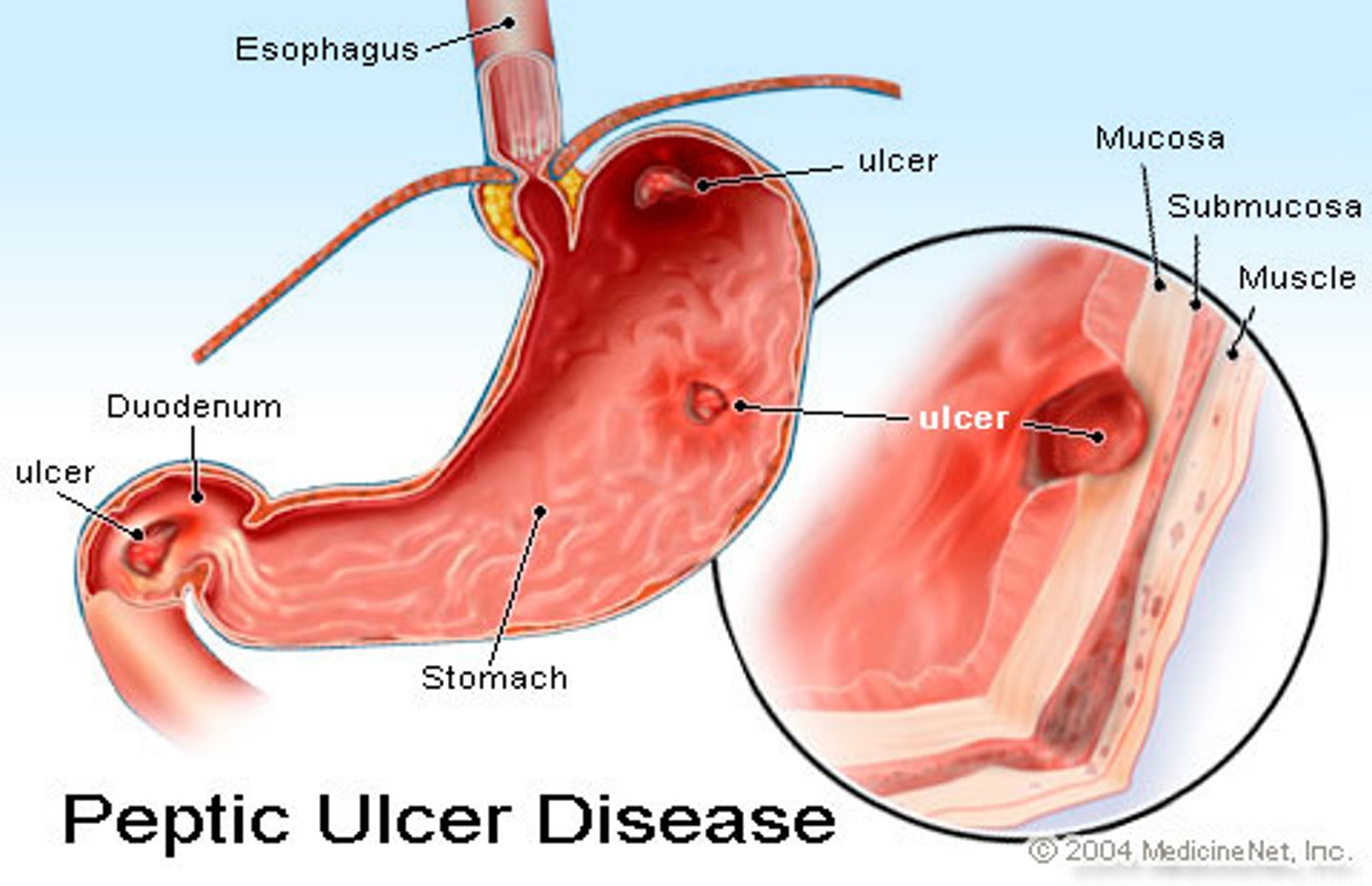
What are the main causes of a lower GI bleed
- IBD
- hemorrhoids
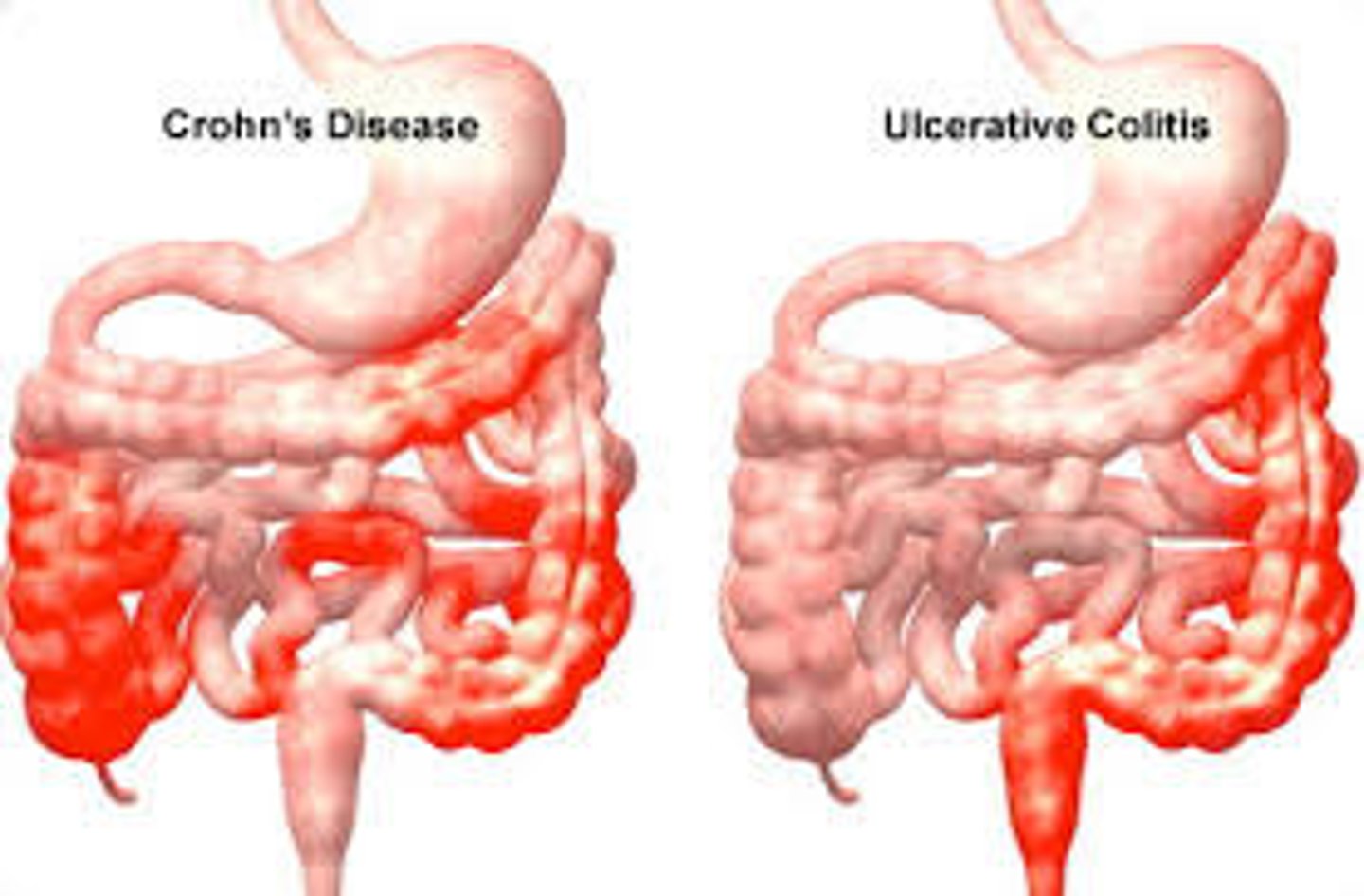
How would we assess and tx a GI bleed?
- assess: endoscopy or colonoscopy
- stop contributing drugs! (could be: NSAIDs or 'blood thinners' (eg. antiplatelets, anticoagulants, or thrombolytics)
- tx: IV fluids, blood products (because we are losing blood) or PPIs

What is a hemorrhage?
Loss of blood from a damaged blood vessel
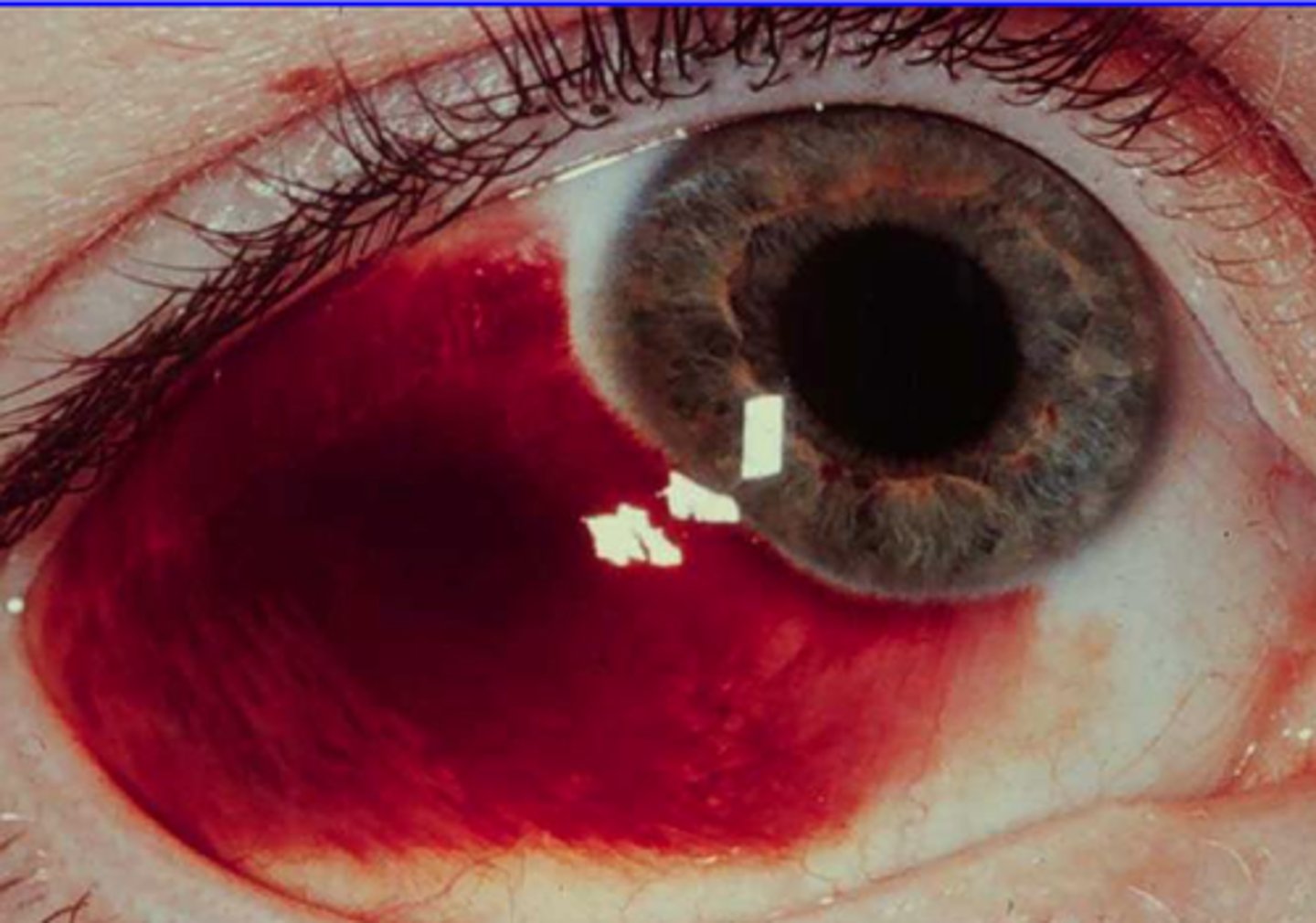
What is the complication of isotonic fluid IV admin to a hemorrhaging pt?
- their O2 carrying capacity is lost
- loss of protein & albumin
- lost platelets and other clotting factors

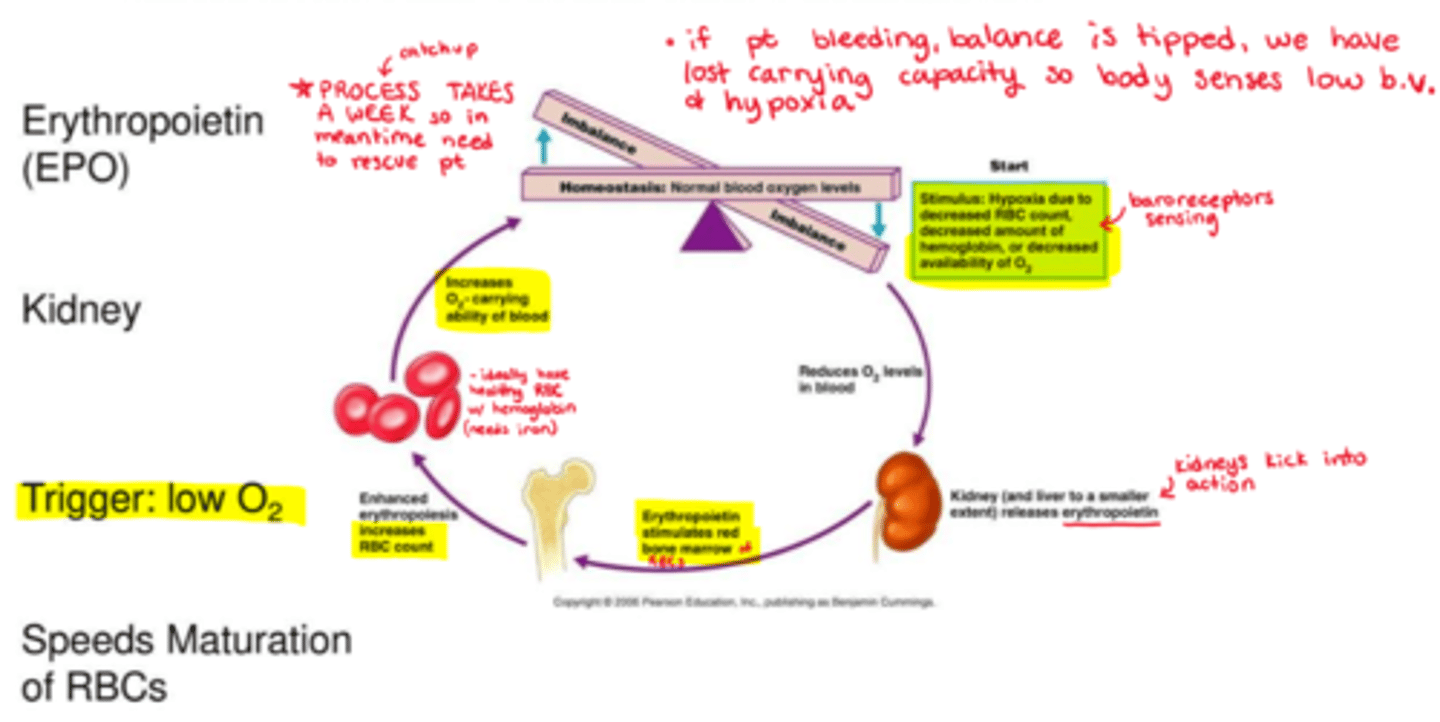
How does erythropoiesis work (RBC formation)
(takes 7 days to form!!!)
- imbalance in normal blood O2 levels triggers hypoxia
- hypoxia may be triggered by decreased RBC count, Hb levels, or availability of O2
- decreased O2 levels in blood trigger kidneys (and liver a tiny bit) into action, releasing erythropoietin
- erythropoietin stimulates red bone marrow
- enhanced erythropoiesis increases RBC count (& speeds up maturation process)
- this overall increases O2 carrying ability of blood now that more RBC are present, bringing the body back to homeostasis
What are we watching for in blood results?
- RBCs
- Hb (Hemoglobin)
- Hematocrit
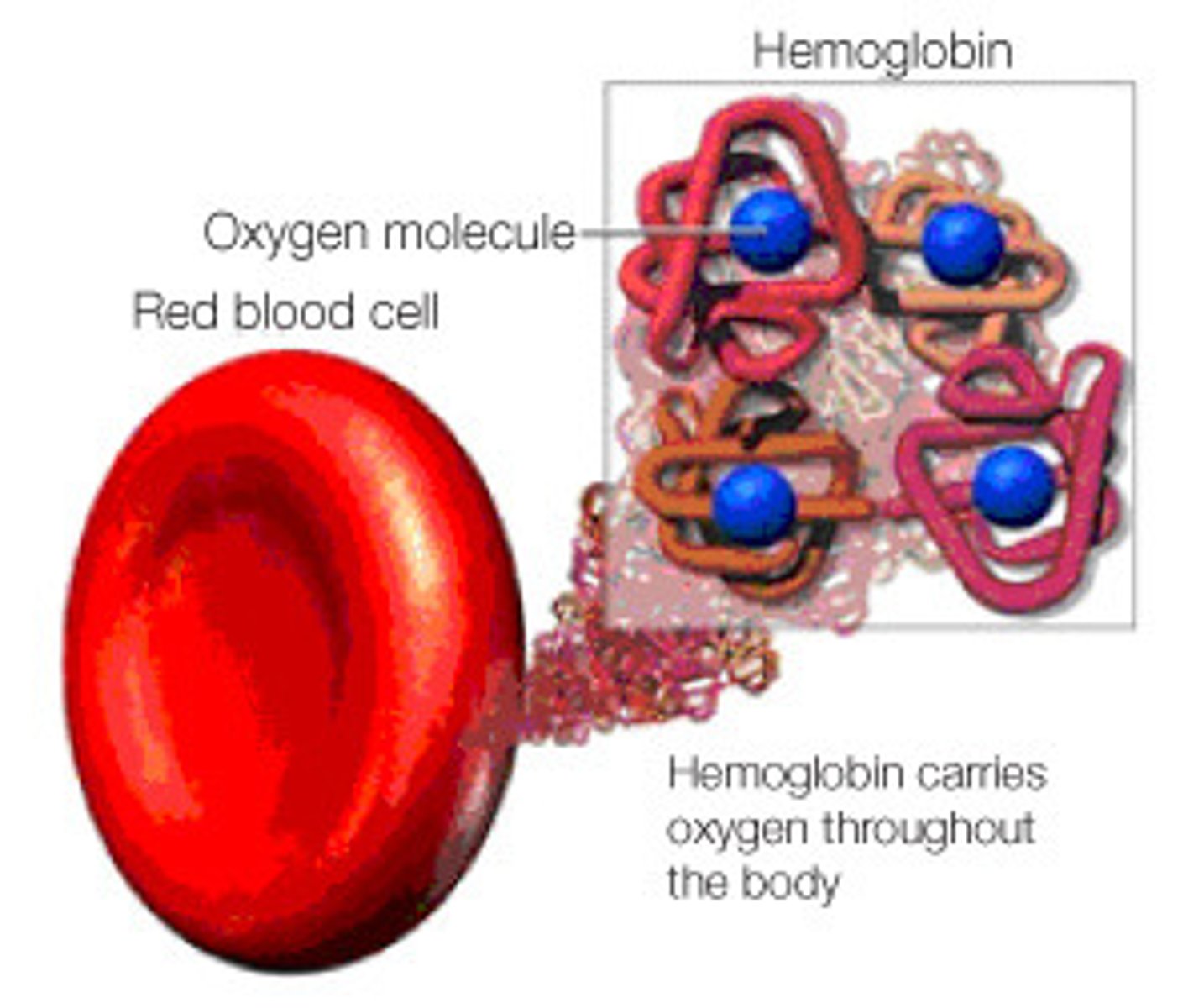
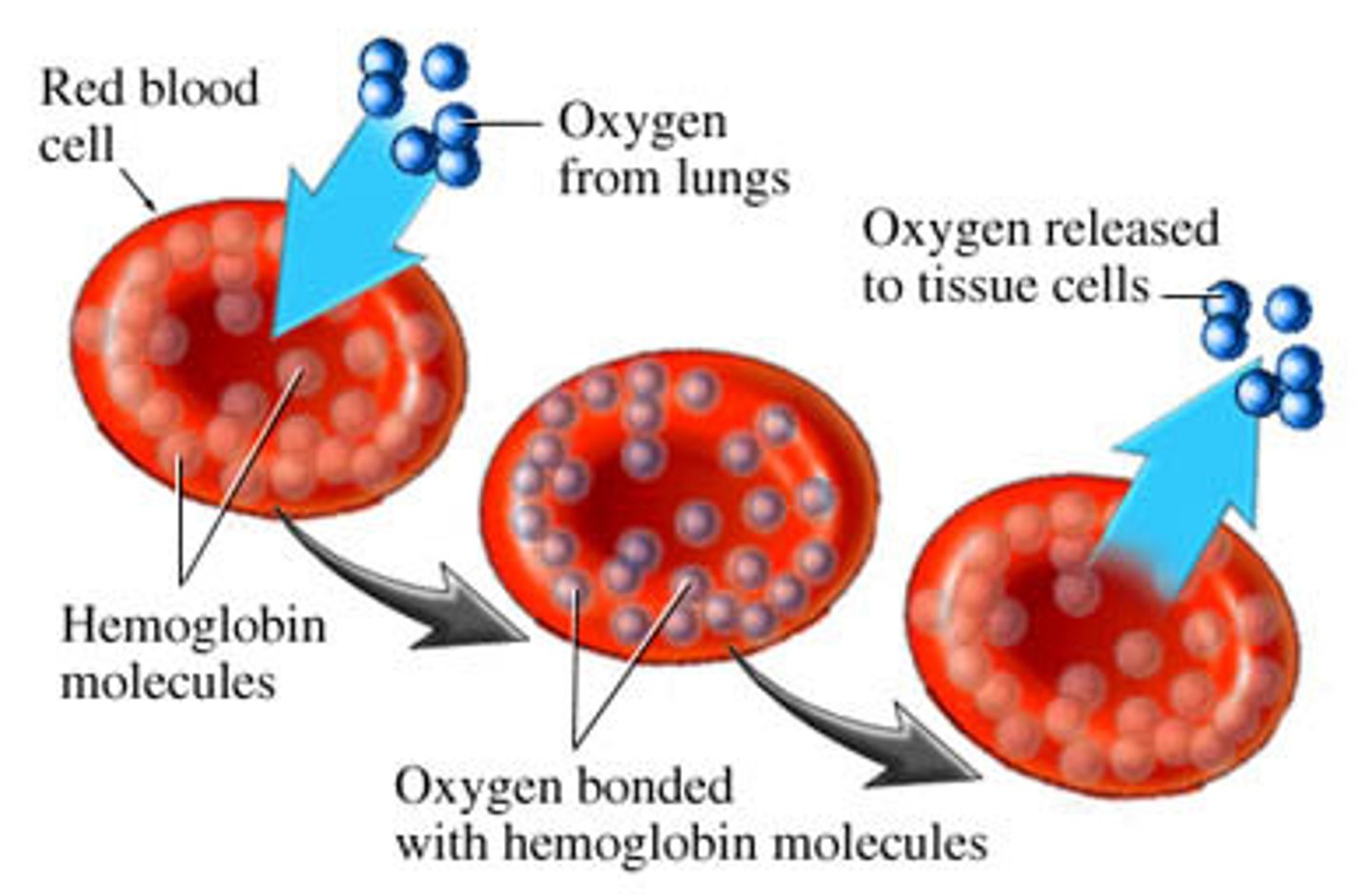
What is the relationship between RBC and Hb?
- each RBC contains hundreds of millions of Hb molecules that are transporting O2
- O2 binds to Heme on the HB molecule
What are the normal blood ranges vs unexpected?
- normal blood in females: 37-47% hematocrit
- normal blood in males: 42-52% hematocrit
- anemia: decreased hematocrit %
- polycythemia: elevated hematocrit %

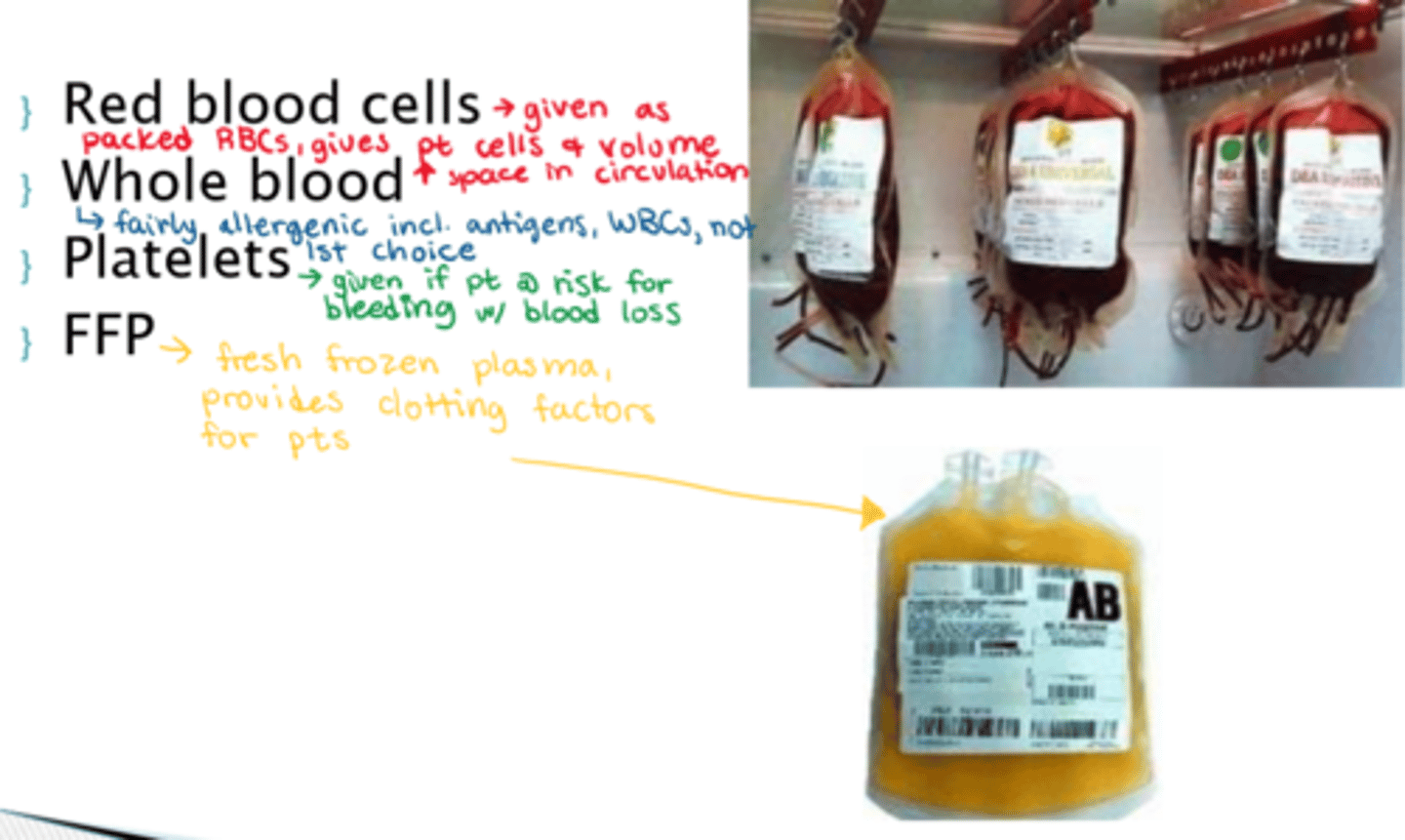
What can we admin for blood loss tx?
- red blood cells
- whole blood (allergenic risk - antigens/WBC present)
- platelets
- FFP (fresh frozen plasma - provides clotting factors for pts)
What are electrolytes and why are they important in our body?
- positively or negatively charged inorganic molecules
- essential to nerve conduction, membrane permeability, water balance & other critical body functions
- potassium and sodium imbalances are the most common (need sodium for osmosis!)
- imbalances can be serious, fatal
What is hyponatremia? How would we tx it?
- sodium levels are too low (< 135mEq/L) (low Na+, high H2O)
- most common cause: loss of sodium via GI or GU; sweating
(eg. diuretic drugs, dehydration - hyponatremic)
- tx: D5NS

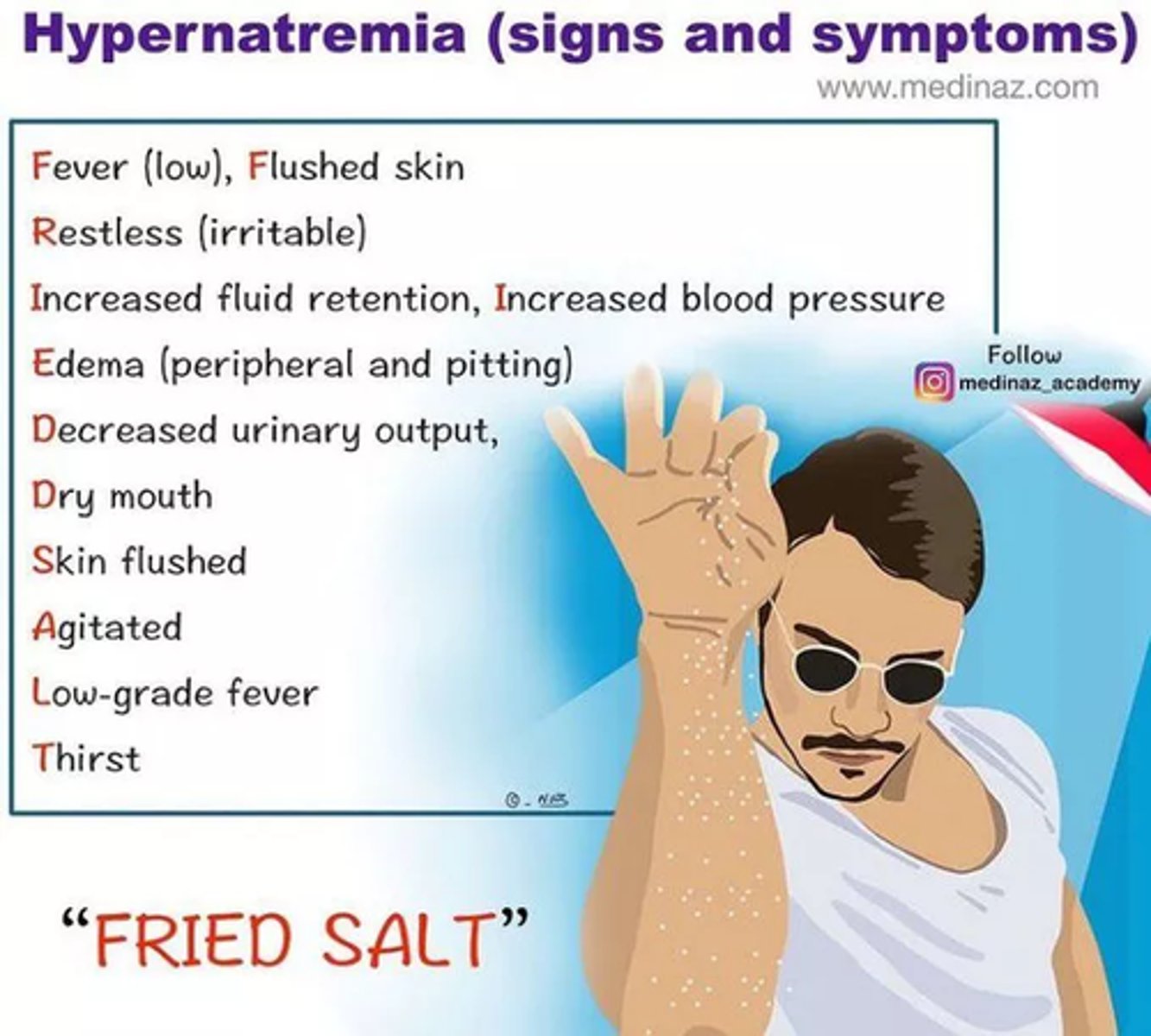
What is hypernatremia? How would we tx it?
- sodium levels are too high (> 145mEq/L) (too much Na+, not enough H2O)
- most common cause: renal failure, high Na intake; diarrhea
- tx: restrict salt intake; diuretics to remove Na+; LOW Na IV fluids
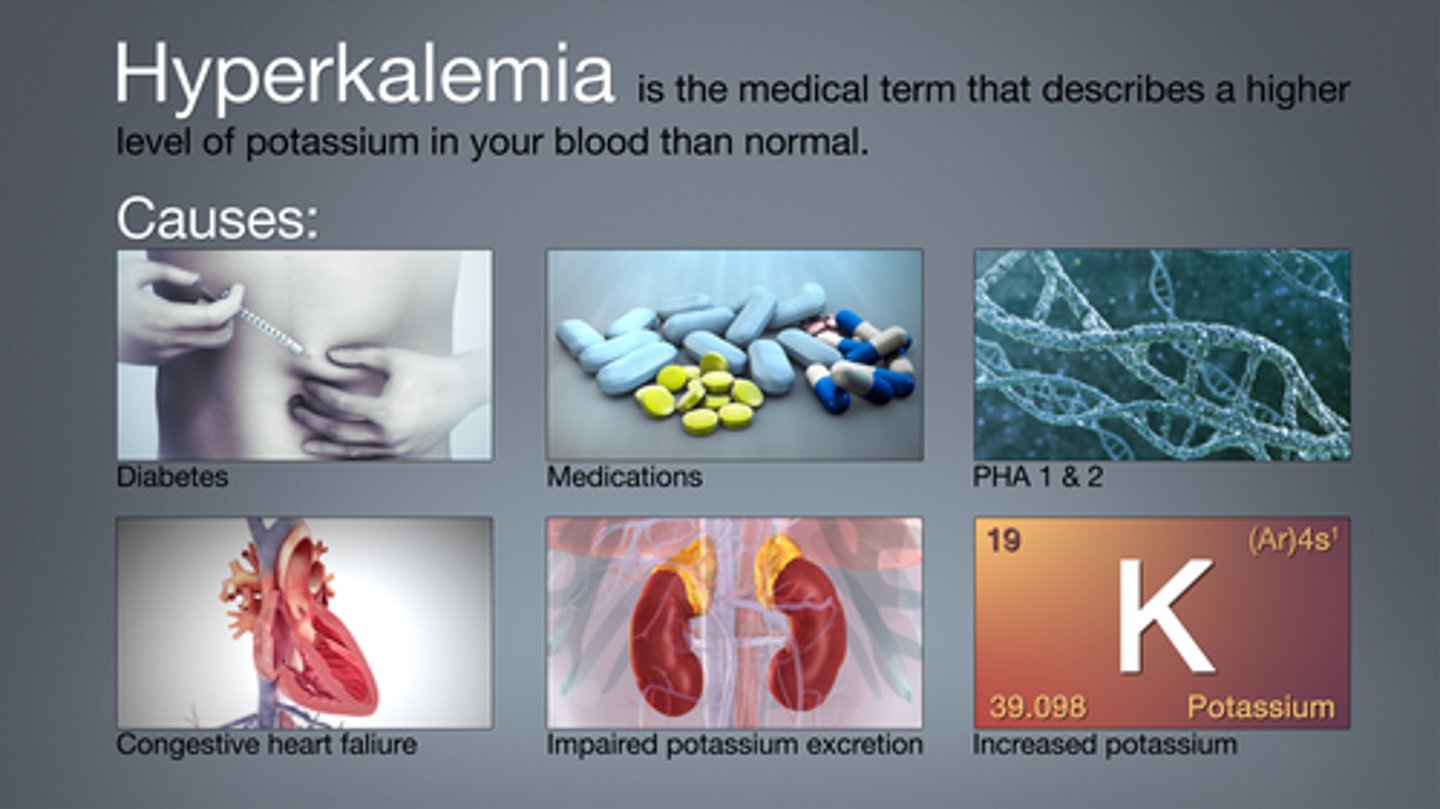
What is hyperkalemia?
- potassium levels are too high (K+ >5 mEq/L)
- most common cause: drugs (eg. potassium sparing diuretics), renal disease
- tx: Kayexalate (PO enteric, NG)
- fx: binds K+ in intestines & excrete via stool
How would we tx hyperkalemia?
- Kayexalate (PO enteric, NG)
- fx: binds K+ in intestines & excrete via stool

What is hypokalemia? How do we tx?
- potassium levels are too low (K+ <3.5 mEq/L)
- most common cause: drugs (eg. potassium wasting diuretics (furosemide!)), N&V
- tx: KCl (IV or PO)

What is the main difference between hypertonic and hypotonic fluid and how may edema occur?
- hypertonic: intracellular fluid is shifted into circulation
- hypotonic: fluid is shifted out of circulation to dilute cells in fluid
- may get stuck in interstitial fluid in between, causing swelling (edema)
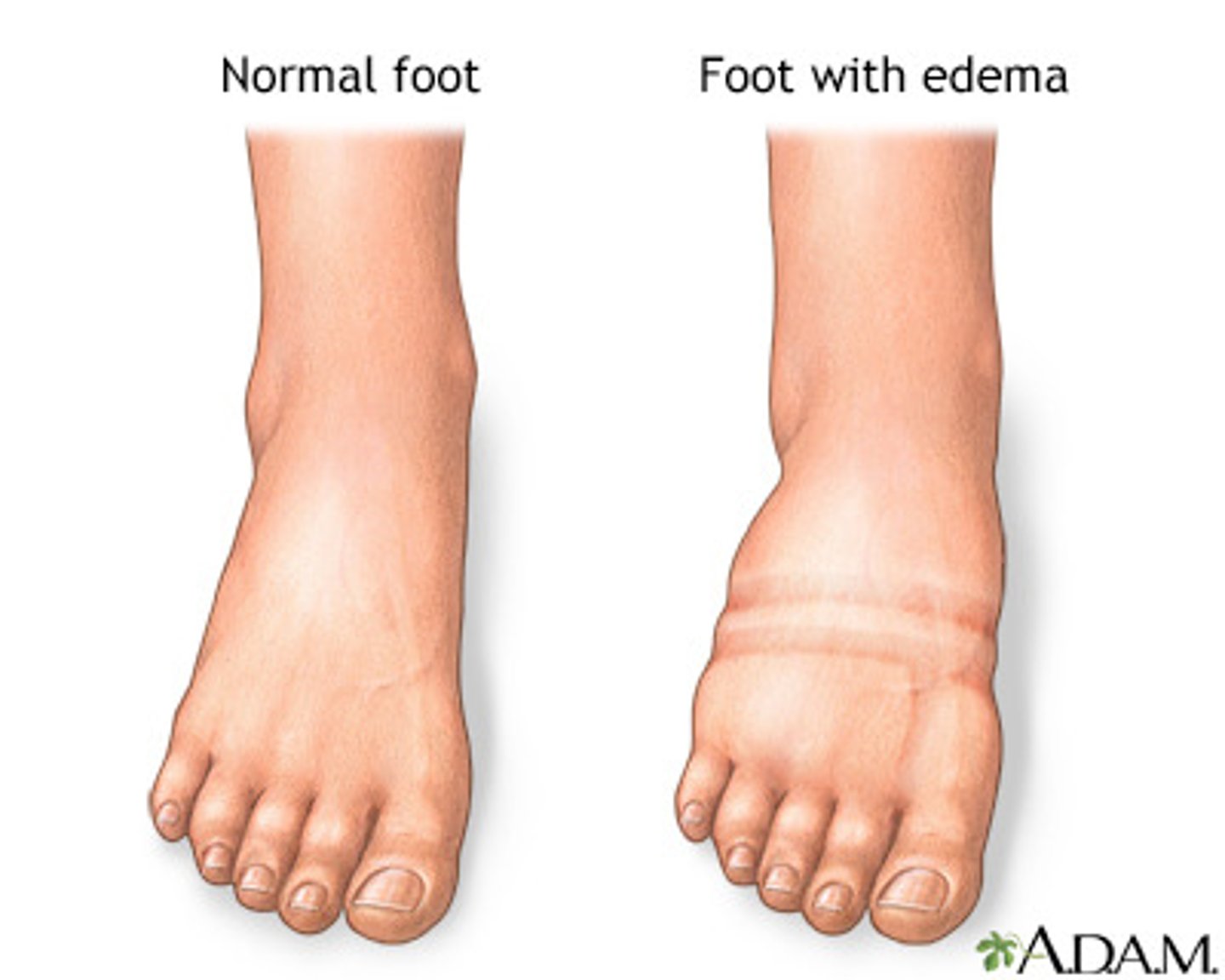
What patients would be considered fluid excess?
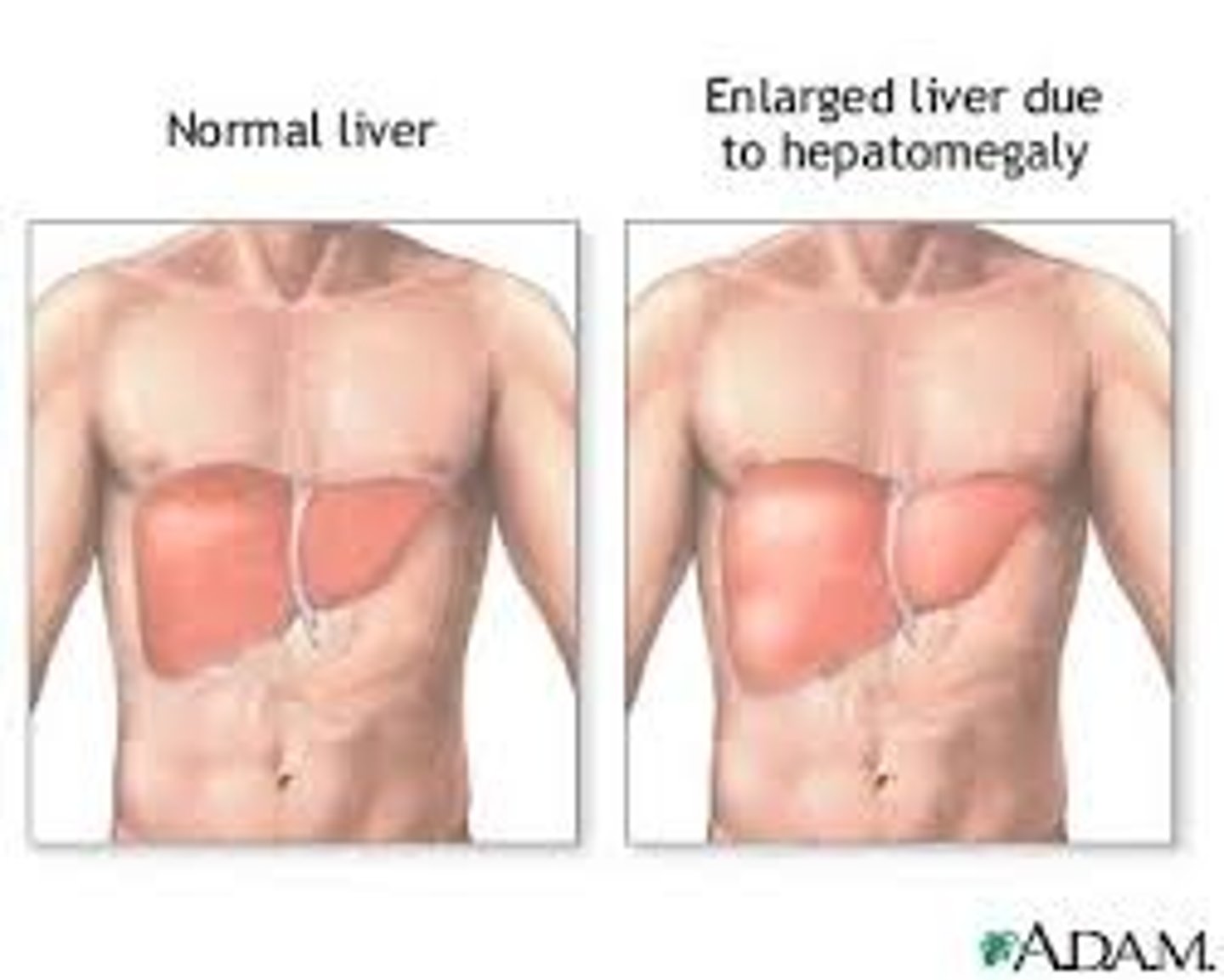
bounding pulses, high BP, edema, hepatomegaly, etc (might be on fluid restriction)

What is our maintenance/resuscitation fluid of choice?
- isotonic crystalloid (0.9% NS)
(eg. pt is NPO but VS are stable, no illnesses causing body fluid shifts b/w ICF and ECF)
- note! infusion choice is specific to patient need and maintenance, or for resuscitation (sudden fluid loss replacement)
- can be used for hyperglycemic pts (usually seen in diabetics)

What is the general rule when deciding if a solution is hypertonic?
General rule: fluids high in sodium &/or glucose are hypertonic
How do you choose what type of fluid a pt requires?
- choose the fluid type according to BP & electrolyte results (Sodium)
What does the patient require:
- Maintenance - replaces normal losses
- Resuscitation - replaces deficits
- Fluid restriction (no IV therapy required, restrict intake)
What is meant by hepatomegaly?
- large liver, caused by decreased venous return
- liver contains a lot of the venous circulation & therefore fluid movement*
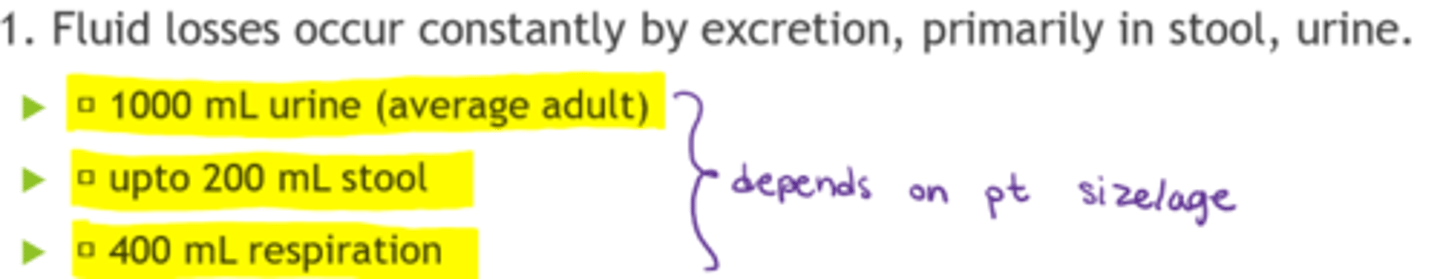
What are the normal fluid losses in a day?
- 1000 mL urine (average adult)
- up to 200 mL stool
- 400 mL respiration
Main causes of a patient being NPO?
- acute severe illness & unable to eat
- awaiting surgery (want to empty GI pre-op)
- ventilated patients (on 'breathing machine')

If a patient is NPO for prolonged periods of time (> 5 days), what needs to happen?
1. assessment required to provide more nutrition (admin of Total Parenteral Nutrition (TPN) & lipids (Given IV, mixed by pharmacy))
2. Is this a palliative care patient? (eg. hypodermoclysis - SC hydration)
What are our maintenance fluids of choice (adults vs peds)
- adults: great choices are LR, NS (if shorter term), D5NS if longer
- children: D5.45 NS
When should hypotonic IV fluids be used? When are they contraindicated?
- fluid shifts out of vasculature & into cells!!!
- good for: diabetic ketoacidosis (body cannot produce enough insulin), hypernatremia
- contraindicated in: cerebral edema patients
- s/e: monitor for hypotension & peripheral edema!
When should hypertonic IV fluids be used? When are they contraindicated?
- fluid shifts from cells into vasculature
- good for: cerebral edema (3% NS, pulling fluid towards circulation to decrease edema), severe hyponatremia
- contraindicated in: fluid overload
- cautious infusion, continuous monitoring!
- do not use it to correct peripheral edema!!!
What are resuscitation fluids (rescue) used for?
- hypovolemic shock
- dehydration
- trauma (hemorrhage)
- hypotension!!!
What is our 1st choice resuscitation fluid?
- NS or LR bolus (isotonic)
- 500 mL bolus, then reassess (are we supporting perfusion, or are we giving too much?)
- assess patient continuously (VS, circulation, etc), => high amounts lead to fluid overload & edema!
What is our 2nd choice resuscitation fluid?
- colloids (AKA plasma expanders):
- caution as colloids remain in circulation (don't travel easily by diffusion, can increase fluids rapidly)
- high % colloids are generally hypertonic & pull ICF fluid into circulation
- increase BP more rapidly & avoid peripheral edema
- monitor for fluid overload! (VS, lung crackles, etc)
S&S of fluid volume excess (overload)
- decreased HR
- increased BP
- pulmonary crackles
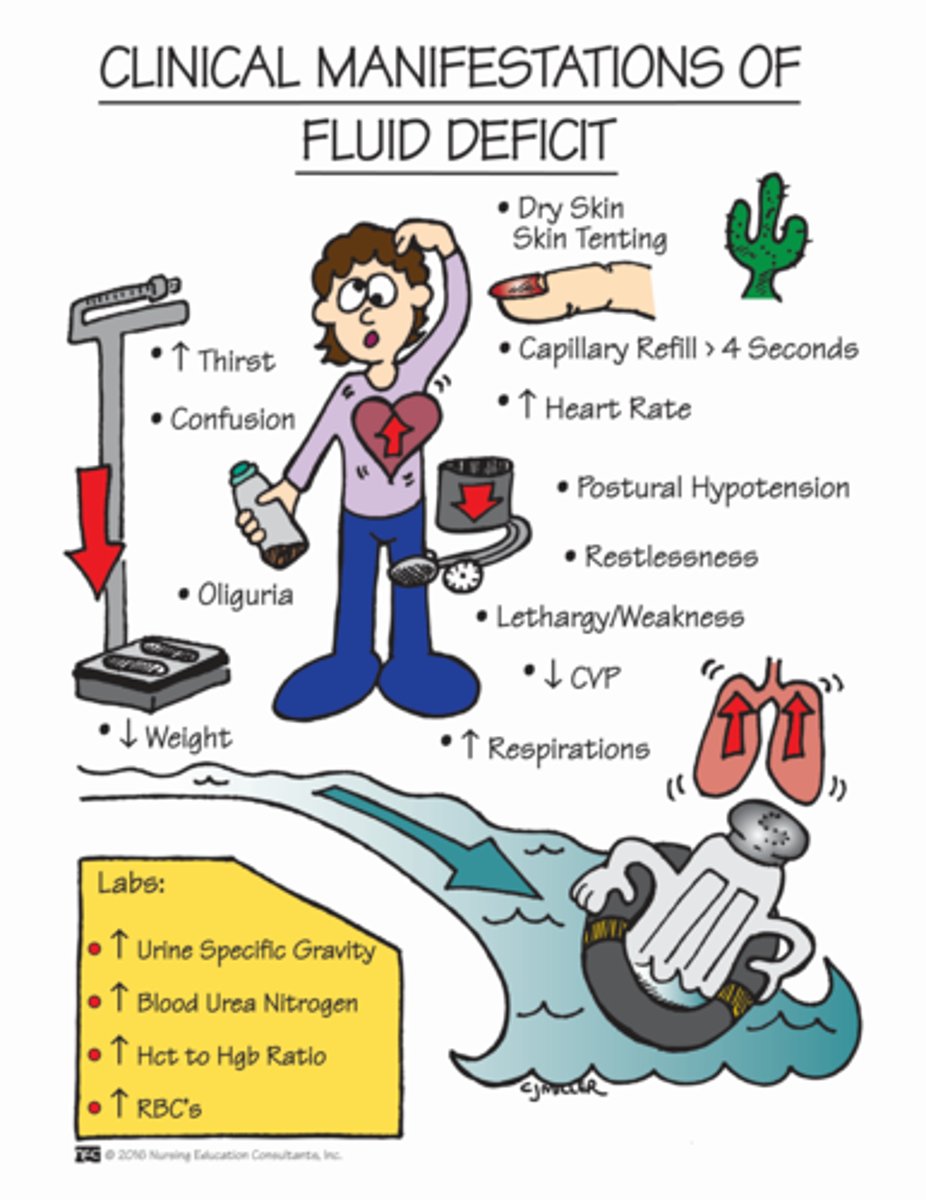
S&S of fluid deficit (hypovolemia)
- decreased LOC
- increased HR
- dizziness
What mostly causes dehydration and what type of IV infusion would we administer?
- dehydration mostly caused by vomiting & diarrhea
- isotonic IV infusion administered (if isotonic admin LR & check Na+ levels in lab work)
How does dextrose impact other IV fluid contents?
- dextrose in IV fluids is metabolized quite quickly
- this will alter the tonicity of the initial fluid
- (eg. D5W - isotonic, but will become hypotonic)
What do maintenance fluid in peds require ideally?
- electrolytes and dextrose (D5.45% NS with KCL (20mEq/L))
- return to normal balanced oral intake as soon as tolerated