Chapter 49: Reproductive System
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
83 Terms
asexual reproduction
a single individual gives rise to offspring without fusion of gametes - there is no genetic input from another individual
sexual reproduction
male and female parents produce offspring through the fusion of gametes (egg and sperm) generated by meiosis
Asexual Reproduction classification
also known as clonal reproduction, one or many cells of a parent develop directly into a new individual - the offspring are genetically identical to one another and to the parent
Advantages of Asexual reproduction
preserves genetic uniformity- advantageous in environments that remain stable and uniform
no energy expanded in producing gametes
No energy expended in finding a mate, especially in sparsely populated areas or in sessile organisms
Mitosis Mechanisms
Asexual reproduction involving mitosis occurs in animals by three mechanisms:
Fission
Budding
Fragmentation
Fission
the parent separates into two or more offspring of approximately equal size (Ex: planarians (flatworms)
Budding
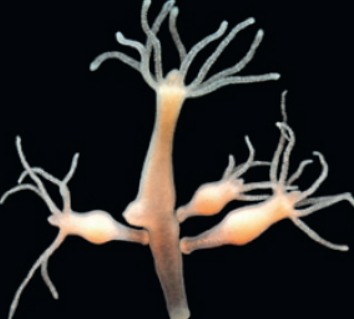
a new individual develops while attached to the parent - offspring may break free from the parent - offspring may break free from the parent or remain attached to form a colony (ex: Hydra)
Fragmentation
pieces separate from the body of a parent and develop and develop (regenerate) into new individuals (Ex: flatworms, annelids and some echinoderms)
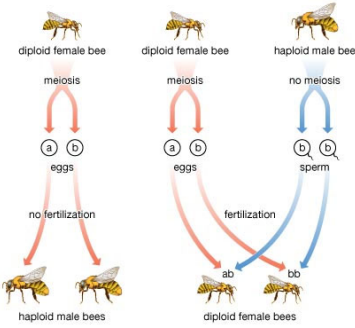
Parthenogenesis
animals that produce by development of an egg without fertilization
because the egg is produced by meiosis in the female parent, the offspring are not genetically identical to the parent or to each other
offspring may be haploid or diploid depending on the species
Example: bees
produce a female through the traditional sexual reproduction process
Sexual Reproduction Advantages
generation of genetic diversity among offspring - increases the chance that, in a changing environment, some offspring will grow and reproduce successfully
Sexual Reproduction Disadvantages
expenditure of energy and raw materials in producing gametes and finding mates
finding mates increases exposure to predation and takes time from finding food and shelter and caring for offspring
Sexual Reproduction and Genetic Diversity
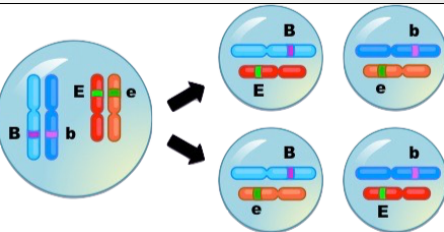
two mechanisms of meiosis give rise to genetic diversity in eggs and sperm: genetic recombination and independent assortment of chromosomes
additional variability is generated at fertilization when eggs and sperm fuse together randomly
random DNA mutations are the ultimate source of variability for both sexual and asexual reproduction
Cellular Mechanisms of Sexual Reproduction
Mating is the paring of a male and female for the purpose of sexual reproduction
The cellular mechanisms of sexual reproduction are gametogenesis, the formation of male and female gametes, and fertilization, the union of gametes
Fusion of a haploid sperm and egg during fertilization produces a diploid zygote, the first cell of a new individual
Gametogenesis
Gametes form from germ cells, a cell line in early embryonic development that remains distinct from other body cells (somatic cells)
Germ cells are located in specialized gamete‐producing organs (gonads) – testes in males and ovaries in females
Mitotic divisions of germ cells produce spermatogonia in males and oogonia in females – these cells enter meiosis to give rise to gametes (by spermatogenesis in males and oogenesis in females)
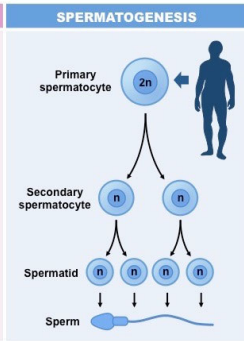
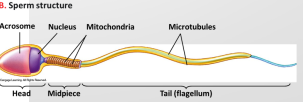
Spermatogenesis
Spermatogenesis produces four mature, haploid spermatozoa (sperm) – typically motile cells driven through a watery medium by a flagellum
At the last step of maturation spermatid to sperm, most of the cytoplasm is lost – except for mitochondria, which produce theATP that drive the flagellum
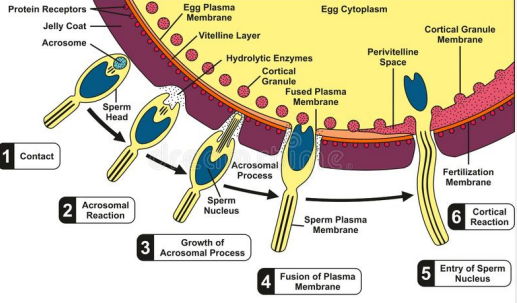
A specialized secretory vesicle (acrosome) containing enzymes and other proteins that help the sperm penetrate the egg forms a cap over the nucleus in the head of the sperm
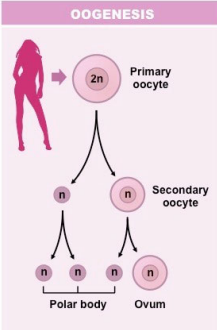
Oogenesis
Oogenesis produces one mature, haploid ovum (egg) – a large cell containing most of the cytoplasm of the parent cell
Unequal cytoplasmic divisions concentrate nutrients and other molecules required for development in the egg – other products form nonfunctional cells called polar bodies
Oocytes in the ovary remain in first meiotic prophase, then advance to metaphase of the second meiotic division at ovulation and do not complete meiosis until fertilization
The Features of the Egg
Stored Nutrients
required for at least the early stages of embryonic development
mammal eggs contain few nutrients
eggs of birds and reptiles contain all nutrients required for complete embryonic development
Egg Coats
protect the egg from injury and infection and, in some species, protect the embryo after fertilization
Mechanisms that prevent the egg from being fertilized by more than one sperm cell
External Fertilization
occurs in most aquatic invertebrates, bony fishes, and amphibians
Males and females synchronize release of large quantities of eggs and sperm into the surrounding water
The sperm swim until they collide with an egg of the same species
The process is helped by synchronization of female and male gamete release, and by the enormous quantities of gametes released
Advantages: Large number of offspring; no need for complex mating behavior.
Disadvantages: Low survival rate per egg; dependent on water and environment.

Internal Fertilization
takes place in invertebrates such as annelids, some arthropods, and some mollusks, and in vertebrates such as reptiles, birds, mammals, some fishes, and some salamanders
In these animals, the sperm are released by the male close to or inside the entrance of the reproductive tract of the female
The sperm swim through fluids in the reproductive tract until they reach and fertilize each egg. In some species, molecules released by the egg attract the sperm to its outer coats
Advantages: Higher chance of fertilization; embryos are protected; can survive in dry environments. higher success rate
Disadvantages: Fewer offspring; requires mating behaviors and sometimes more energy investment.
Physical Act of Mating
Introduction of the male’s accessory sex organ into the female’s accessory sex organ to accomplish internal fertilization is known as copulation
Internal fertilization makes terrestrial life possible by providing the aquatic medium required for fertilization inside the female’s body without the danger of gametes drying by exposure to the air
In mammals, the male’s penis delivers sperm into the female’s vagina, which is specialized for reproduction
Species Recognition
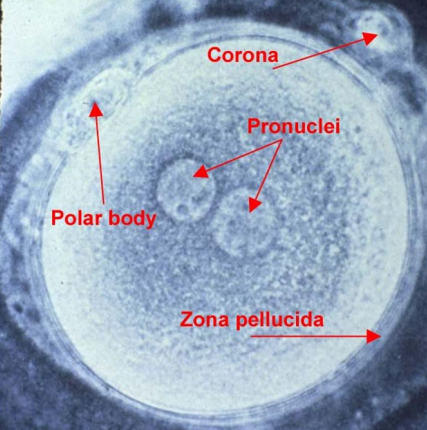
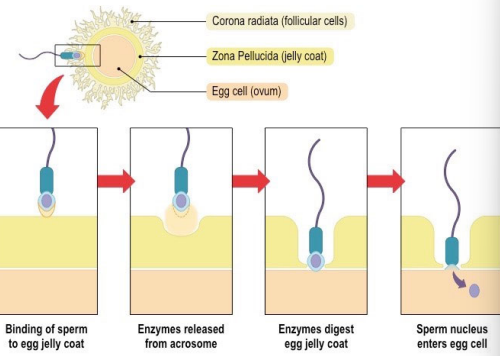
When a sperm touches the outer surface of an egg, receptor proteins in the sperm plasma membrane bind the sperm to the vitelline coat or zona pellucida
In most animals, only a sperm from the same species as the egg can recognize and bind to the egg surface
Species recognition is highly important in animals that carry out external fertilization, because the water surrounding the egg may contain sperm of many different species

Fertilization
Attachment of sperm to egg triggers the acrosomal reaction – enzymes in the acrosome are released from the sperm and digest a path through the egg coats
The sperm follows the path until its plasma membrane touches and fuses with the plasma membrane of the egg
Fusion introduces the sperm nucleus into the egg cytoplasm and activates the egg to complete meiosis and begin development
Fast block polyspermy
(sometimes in some invertebrates) occurs within a few seconds after fertilization
Fusion of egg and sperm opens ion channels in the plasma membrane of the egg, spreading a wave of electrical depolarization over the egg surface
Depolarization alters the egg plasma membrane’s potential from negative to positive so that it cannot fuse with any additional sperm – eliminating the possibility that more than one set of paternal chromosomes enters the egg
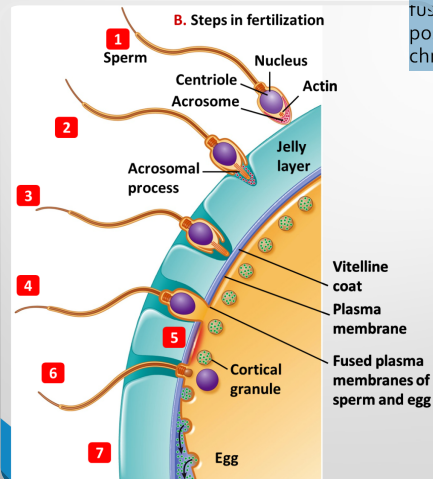
Slow block polyspermy
occurs within minutes after fertilization
Fusion of egg and sperm triggers release of Ca2+ ions from the egg’s ER into the cytosol
Ca2+ ions activate control proteins and enzymes that initiate intense metabolic activity in the fertilized egg
Ca2+ ions trigger the cortical reaction – cortical granules under the egg’s plasma membrane release their contents by exocytosis
Enzymes released from cortical granules alter the egg coats so no further sperm can penetrate to the egg
Fusion of nuclei
After the sperm nucleus enters the egg cytoplasm, microtubules move the sperm and egg nuclei together in the egg cytoplasm and they fuse
Chromosomes of the egg and sperm nuclei assemble together and enter mitosis, initiating the highly programmed events of embryonic development
Oviparous
animals lay eggs that contain nutrients needed for development of the embryo outside the mother’s body
egg outside → laid eggs.
Examples: Birds, most reptiles, amphibians, many fish.
Ovoviviparous
animals retain fertilized eggs within the body and the embryo develops in the egg – there is no uterus – eggs hatch inside the mother and offspring are released
egg inside → egg hatches inside.
Examples: Some sharks, snakes, and insects.
Viviparous
animals retain the embryo within the mother’s uterus and nourish it during at least early development
live → live birth with maternal nourishment.
Examples: Most mammals (humans, dogs, whales).
Placental mammals
(eutherians) have a that connects the embryo to the uterus – it facilitates transfer of nutrients from the mother’s blood to the embryo, and wastes from the embryo to the mother
Offspring are born well-developed
Young feed on milk after birth, but fully formed at birth
Examples: Humans, Dogs, Whales, Elephants
Marsupials
(metatherians) provide nutrients to the embryo during early stages of development via an attached membranous sac containing yolk – the embryo is born at an early stage and crawls to an abdominal pouch (marsupium) where it attaches to a nipple and continues development
are born very underdeveloped and continue developing in a pouch (marsupium)
Examples: Kangaroo, Koala, Opossum
Hermaphroditism
Definition: both mature egg‐ producing and mature sperm‐producing tissues are present in the same individual
Most hermaphroditic animals do not fertilize themselves – self‐fertilization is prevented by anatomical barriers, or by producing mature egg and sperm at different times
Simultaneous hermaphrodites: develop functional ovaries and testes at the same time
Example: Earthworms
Sequential hermaphrodites: change from one sex to the other
Example: clownfish (Finding Nemo) – Nemo is born male; if the dominant female dies, the largest male in the group changes into a female.
Sexual reproduction in humans
Human reproduction is typical of eutherian mammals:
Gonads produce gametes and secrete hormones responsible for sexual development and mating behavior
Eggs are fertilized in the oviduct and implant in the uterus, where they proceed through embryonic development
Nutrients from the mother and wastes from the embryo are exchanged through the placenta
After birth, the newborn is nourished with milk secreted by the mother’s mammary glands
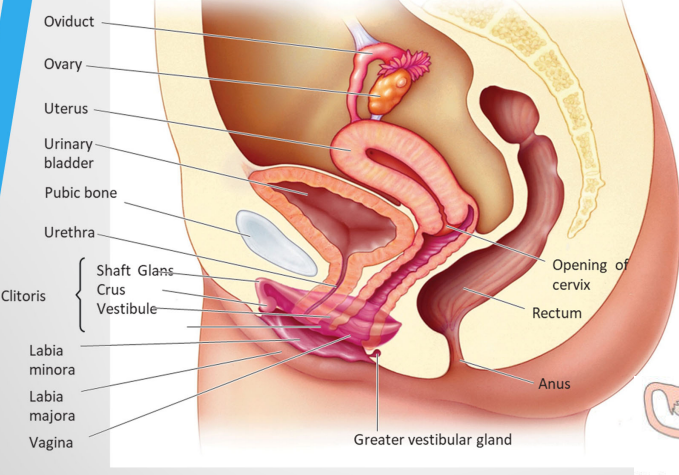
Internal female sex organs
An oviduct leads from each ovary to the uterus
The egg implants in the uterine lining (endometrium) – formed by layers of connective tissue with embedded glands and richly supplied with blood vessels
The lower end of the uterus (cervix) opens into the vagina, which receives sperm and acts as the birth canal
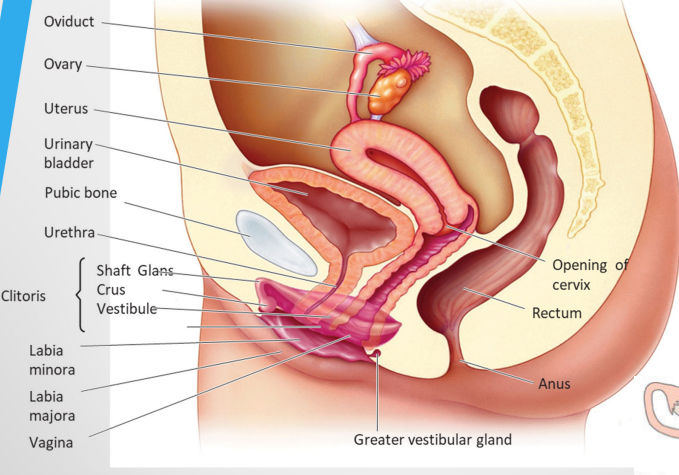
External female sex organs
collectively called the vulva and surrounds the opening of the vagina
Two sets of folded tissue: labia minora and labia majora
Erectile tissue: the clitoris
Greater vestibular glands secrete lubricating fluid
The hymen – a thin membrane that partially covers the opening of the vagina
The Monthly Reproductive Cycle
Reproduction in human females is under neuroendocrine control, involving complex interactions between the hypothalamus, pituitary, ovaries, and uterus
Cyclic events in the ovary, leading to ovulation about every 28 days from puberty to menopause, are the ovarian cycle
This cycle coordinates with the uterine cycle (menstrual cycle) that prepares the uterus to receive the egg if fertilization occurs
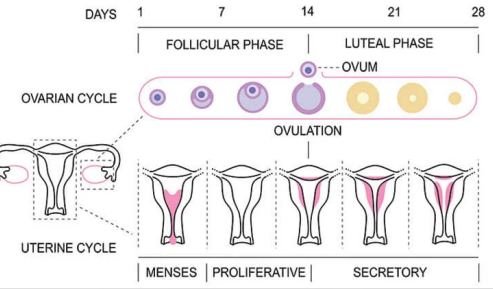
Menstrual Phase (Days 1–5)
What happens: The uterine lining (endometrium) sheds if there’s no pregnancy.
Signs: Bleeding occurs (period).
Hormones: Low levels of estrogen and progesterone.
Follicular Phase (Days 1–13, overlaps with menstruation)
Ovaries: Follicles in the ovary start maturing; one becomes dominant.
Hormones:
FSH (Follicle-stimulating hormone) stimulates follicle growth.
Estrogen rises, helping rebuild the uterine lining.
Egg: The dominant follicle prepares the egg for ovulation.
Ovulation (Day 14, mid-cycle)
What happens: The mature egg is released from the ovary into the fallopian tube.
Hormones:
LH surge (Luteinizing Hormone) triggers ovulation.
Estrogen peaks just before LH surge.
Fertilization: Egg can be fertilized by sperm within ~24 hours.
Luteal Phase (Days 15–28)
Ovaries: The ruptured follicle becomes the corpus luteum, which secretes progesterone (and some estrogen).
Uterus: Progesterone thickens the endometrium to prepare for possible implantation of a fertilized egg.
Hormones: Progesterone rises, estrogen moderate.
The Ovarian Cycle
The ovarian cycle begins with an increase in gonadotropin‐ releasing hormone (GnRH) released by the hypothalamus
GnRH stimulates the pituitary to release follicle‐stimulating hormone (FSH) and luteinizing hormone (LH)
FSH stimulates 6 to 20 primary oocytes in the ovaries to be released from prophase of meiosis I and continue meiosis
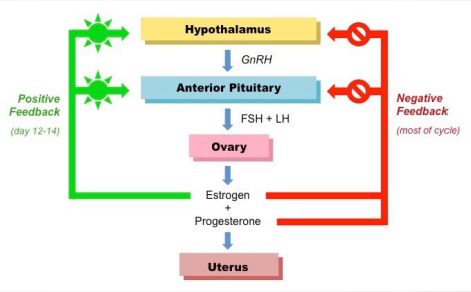
Ovarian cycle: Follicular Phase
Primary oocytes develop into secondary oocytes, which arrest in metaphase II, surrounded by cells that form a follicle
As the follicle enlarges, FSH and LH interact to stimulate the follicular cells to secrete estrogens, primarily estradiol
Secreted in low amounts, estrogens have a negative feedback effect on the pituitary, inhibiting its secretion of FSH
Estrogen secretion increases steadily, and its level peaks at about 12 days after follicle development begins
High estrogen level has a positive feedback effect on the hypothalamus and pituitary, increasing release of GnRH and stimulating the pituitary to release a burst of FSH and LH
The burst in LH secretion stimulates follicle cells to release enzymes that digest the wall of the follicle, causing it to burst and release the egg (ovulation)
Ovulation
At the birth of a female, each ovary contains about 1 million oocytes, arrested at the end of the first meiotic prophase
About 200,000 to 400,000 oocytes survive until a female becomes sexually mature
About 400 are ovulated (released into the oviducts) during the woman’s lifetime
The egg is pulled into the oviduct by the current produced by the beating of cilia lining the oviduct
The Ovarian Cycle: Luteal Cycle
LH also initiates the last phase of the menstrual cycle, the luteal phase
LH causes the follicle cells remaining at the surface of the ovary to grow into a corpus luteum, which secretes estrogens, large quantities of progesterone, and inhibin
Progesterone stimulates growth of the uterine lining and inhibits contractions of the uterus – it also inhibits secretion of GnRH, which inhibits release of FSH and LH
If fertilization does not occur, the corpus luteum gradually degenerates and its cells are phagocytized – in the absence of progesterone, menstruation begins
The Uterine Cycle
Menstrual flow results from the breakdown of the thickened endometrium – when flow ceases (day 4 ‐ 5 of the cycle) the endometrium begins to grow again (the proliferative phase)
Ovulation occurs about day 14 – if fertilization does not take place, the uterine lining continues to grow for another 14 days (the secretory phase)
At that time, lack of progesterone stops the blood supply, causing the lining to disintegrate – menstrual flow begins
Human Male Sexual Organs
Testes are suspended in the scrotum, which keeps them cooler than the body core
Mature sperm flow from the seminiferous tubules into the epididymis, a coiled storage tubule attached to the surface of each testis
Rhythmic muscular contractions of the epididymis move sperm into the vas deferens, which leads into the urethra
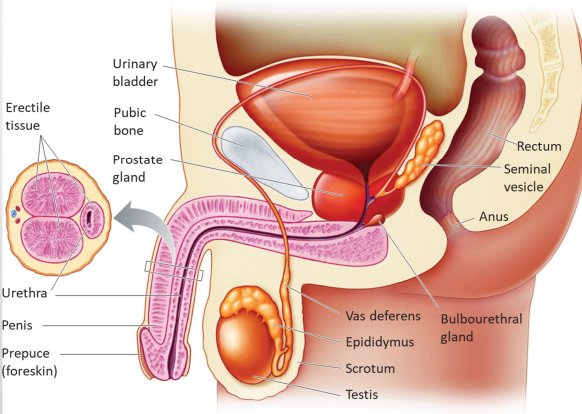
Why are the testes suspended in the scrotum?
To keep them cooler than the body core, which is necessary for proper sperm production.
Where do mature sperm go after forming in the seminiferous tubules?
They flow into the epididymis, a coiled storage tubule attached to each testis.
How do sperm move from the epididymis to the urethra?
Rhythmic muscular contractions of the epididymis push sperm into the vas deferens, which leads to the urethra.
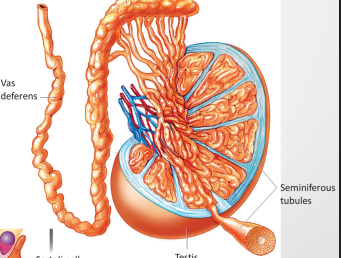
Where are sperm produced in males?
In the seminiferous tubules(in the testes) of the testes.
How long does spermatogenesis take, and how many sperm are produced daily?
The process takes 9–10 weeks from spermatogonium to mature sperm, producing about 130 million sperm per day.
What are Sertoli cells, and what do they do?
Found in the seminiferous tubules, surrounding developing spermatocytes.
Functions:
Provide nutrients to developing sperm.
Form the blood-testis barrier, isolating spermatocytes from the body’s immune system.
What are Leydig cells, and what do they do?
Located outside the seminiferous tubules, in the surrounding tissue.
Function: Produce male sex hormones (androgens), mainly testosterone, which is essential for sperm development and male secondary sexual characteristics.
Summarize the roles of seminiferous tubules, Sertoli cells, and Leydig cells in spermatogenesis.
Seminiferous tubules: site of sperm production
Sertoli cells: nourish sperm and protect them from the immune system
Leydig cells: produce testosterone to regulate spermatogenesis
What happens to sperm before they leave the body?
Sperm are mixed with secretions from three accessory glands, forming semen.
What do the seminal vesicles secrete, and what is its function?
Secrete a thick seminal fluid containing prostaglandins.
Function: Helps sperm move through the vasa deferentia.
What does the prostate gland do?
Adds an alkaline secretion to semen.
Functions:
Raises semen pH to counteract vaginal acidity.
Activates sperm motility.
Location: Surrounds where the vasa deferentia join the urethra.
What do the bulbourethral glands do?
- Secrete a clear, mucus-rich fluid into the urethra.
Functions:
Lubricates the tip of the penis.
Neutralizes residual urine acidity in the urethra.
How much of semen is made up of sperm vs accessory gland secretions?
Accessory gland secretions: >95% of semen volume
Sperm: <5% of semen volume
Male Accessory Glands
Seminal vesicles → energy & movement
Prostate → pH balance & sperm activation
Bulbourethral glands → lubrication & neutralization
What hormone does the hypothalamus secrete in sexually mature males, and what does it do?
GnRH (Gonadotropin-Releasing Hormone) → stimulates the anterior pituitary to secrete LH and FSH.
What does LH (Luteinizing Hormone) do in males?
Stimulates Leydig cells in the testes to produce testosterone.
What are the roles of testosterone in males?
Stimulates sperm production.
Controls growth and function of male reproductive structures (e.g., penis, testes, prostate).
Promotes male secondary sexual characteristics (e.g., facial hair, deep voice).
What does FSH (Follicle-Stimulating Hormone) do in males?
Stimulates Sertoli cells to secrete proteins and molecules required for spermatogenesis.
How are male reproductive hormone levels regulated?
By feedback mechanisms:
High testosterone inhibits GnRH, LH, and FSH release (negative feedback).
Low testosterone stimulates GnRH, LH, and FSH release.
Quick summary mnemonic of male rerpductive
GnRH → LH + FSH
LH → Leydig → Testosterone → sperm & male structures
FSH → Sertoli → supports spermatogenesis
Feedback keeps hormones in balance
Where can a human egg be fertilized?
Only in the third of the oviduct nearest the ovary.
How do sperm penetrate the egg’s protective layers?
Sperm use enzymes in their plasma membranes to penetrate the follicle cells surrounding the egg.
Many sperm release acrosomal enzymes together, increasing the chance of penetrating the zona pellucida, but only one sperm fertilizes the egg.
What is a zygote?
The single cell formed when the sperm and egg nuclei fuse.
Where does the first mitotic division of the embryo occur?
While the fertilized egg is still in the oviduct.
When and where does implantation occur?
About 7 days after ovulation, the embryo moves from the oviduct and implants in the uterine lining.
What role does hCG play after implantation?
Secreted by cells associated with the embryo.
Maintains the corpus luteum, preventing it from breaking down.
What happens around 10 weeks after implantation?
The placenta takes over progesterone production.
hCG drops, and the corpus luteum regresses.
The corpus luteum still secretes relaxin, which prevents uterine contractions until birth.
What is infertility?
The inability to conceive after 12 months of frequent, contraceptive-free intercourse.
Causes of male infertility?
Low sperm count or motility
Erectile dysfunction or duct blockage
Health and lifestyle factors
Causes of female infertility?
Inflammation of the Fallopian tubes
Hormone deficiencies
Environmental or lifestyle factors (e.g., athletes may have menstrual cycle irregularities)
What is the rhythm method?
Avoiding intercourse during the period of the month when the egg can be fertilized.
What is the withdrawal method?
Removing the penis from the vagina before ejaculation.
How does a condom prevent pregnancy?
Blocks sperm from entering the vagina; latex condoms may also prevent disease transmission.
What does a diaphragm do?
Blocks the cervix (used with spermicidal jelly) to prevent sperm from entering the uterus.
What is an intrauterine device (IUD)?
A long-term device placed in the uterus to prevent fertilization.
How is surgical contraception done?
Vasectomy: cutting and closing the vasa deferentia in males.
Tubal ligation: cutting and closing the oviducts in females.
How does the oral contraceptive pill prevent pregnancy?
Contains estrogen and progestin (or progestin alone) → inhibits FSH and LH secretion, preventing ovulation.
Side effect: increased risk of heart attack or stroke in smokers.
What is emergency contraception (“morning-after pill”)?
Progestin pill taken within 72 hours after intercourse to prevent pregnancy.