PHR 927 Block 4 IBD Etiology and Pathophysiology
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
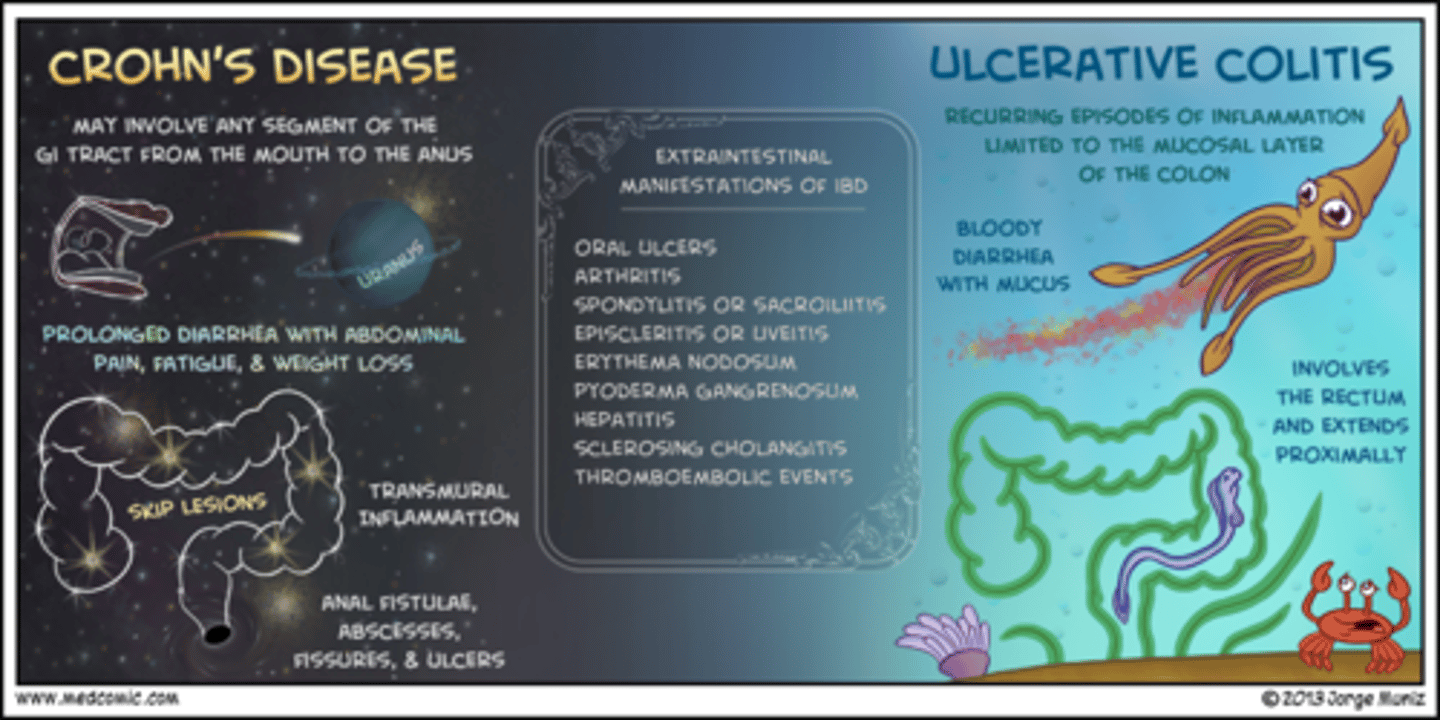
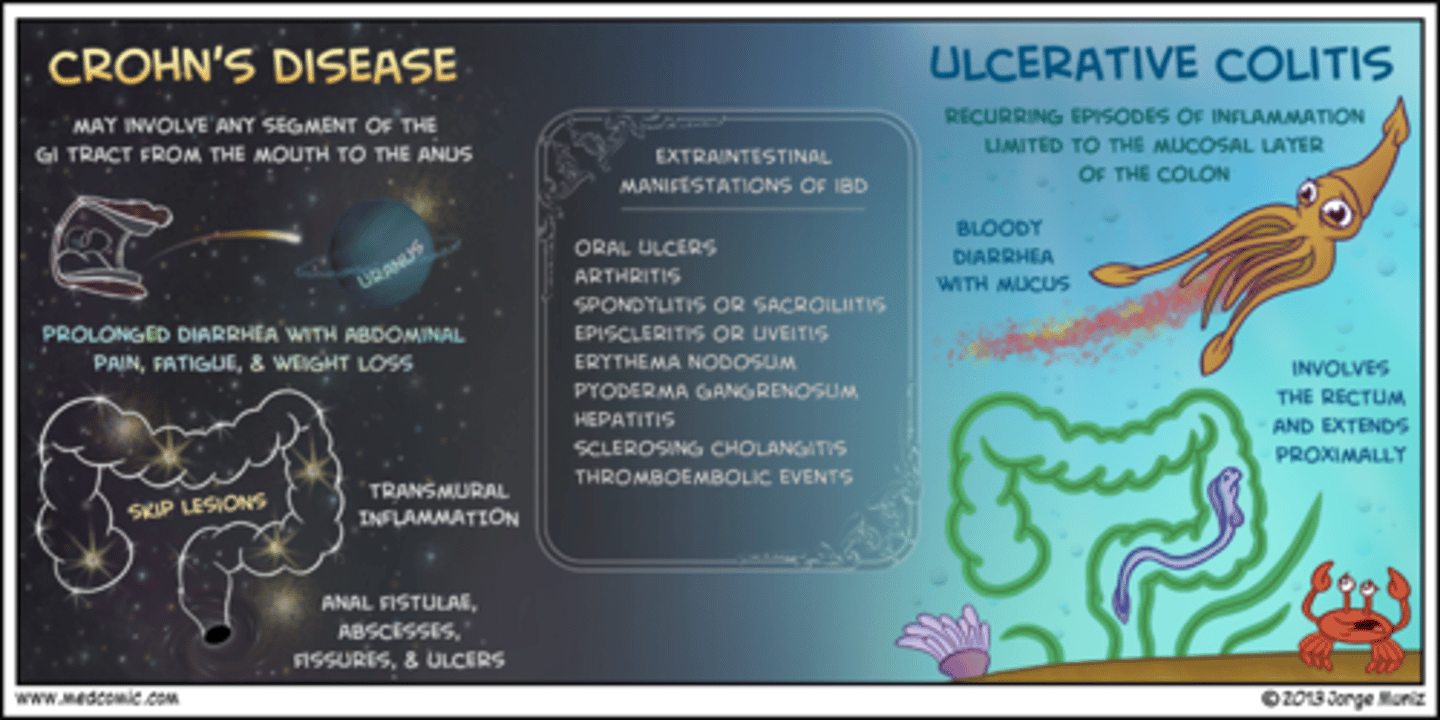
irritable bowel disease (IBD)
chronic inflammation of the bowel
two types: ulcerative colitis and crohn's disease
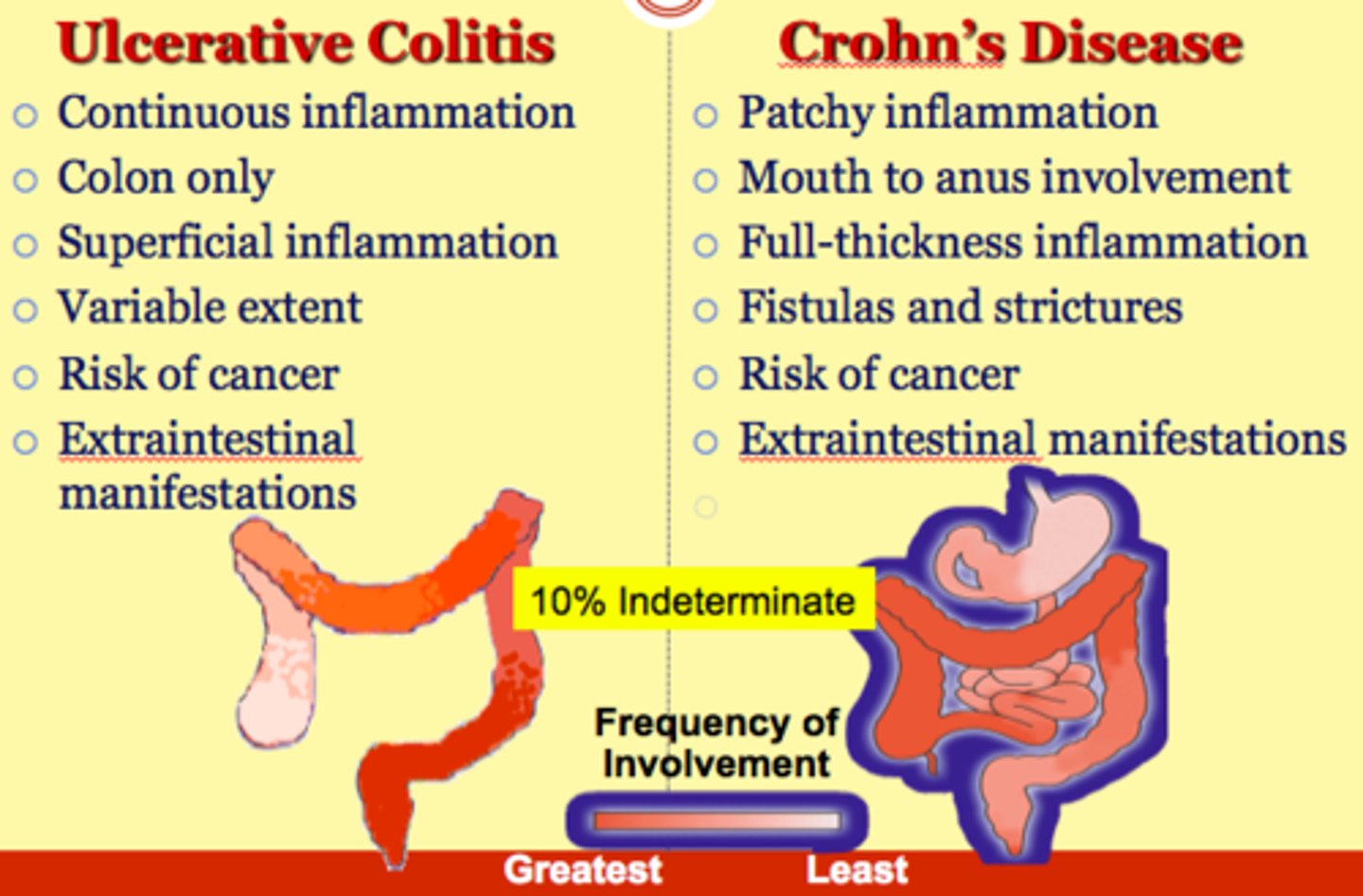
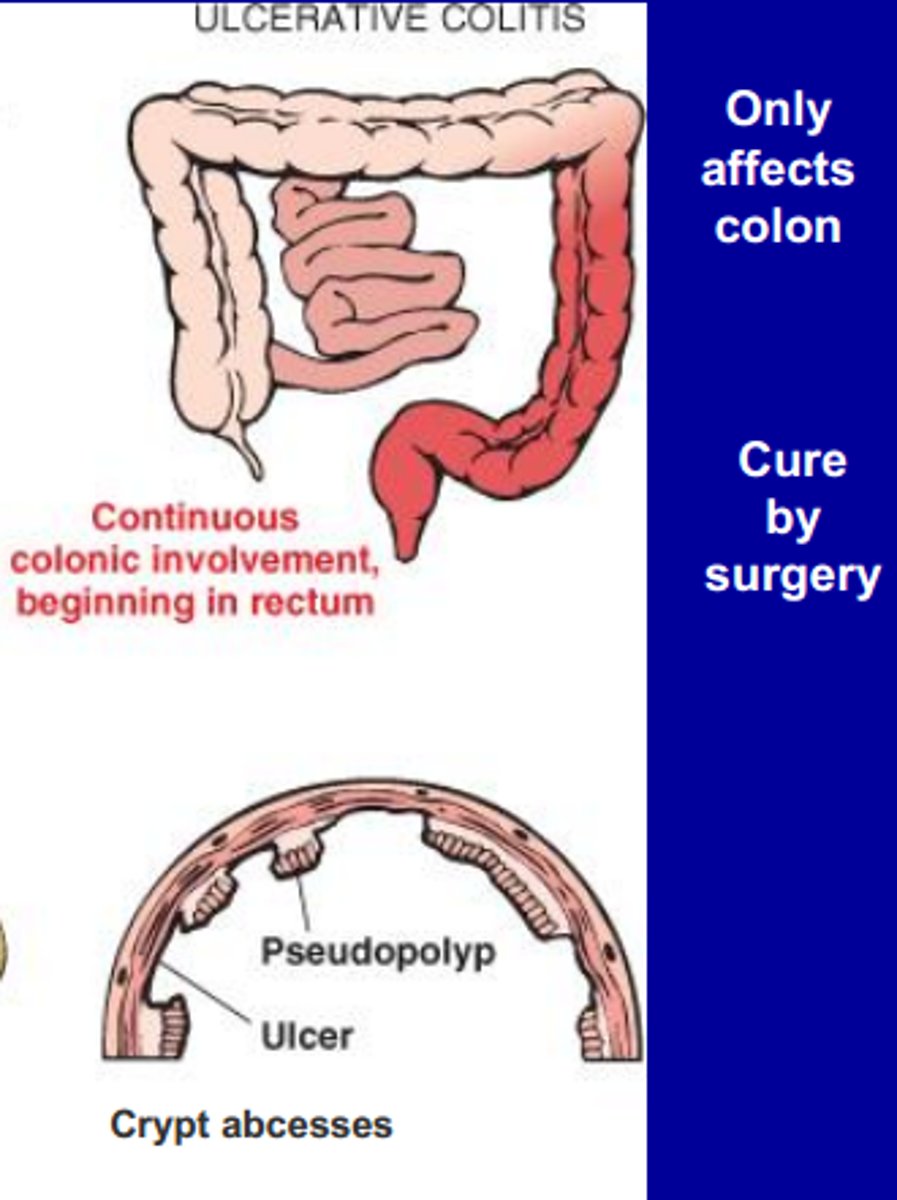
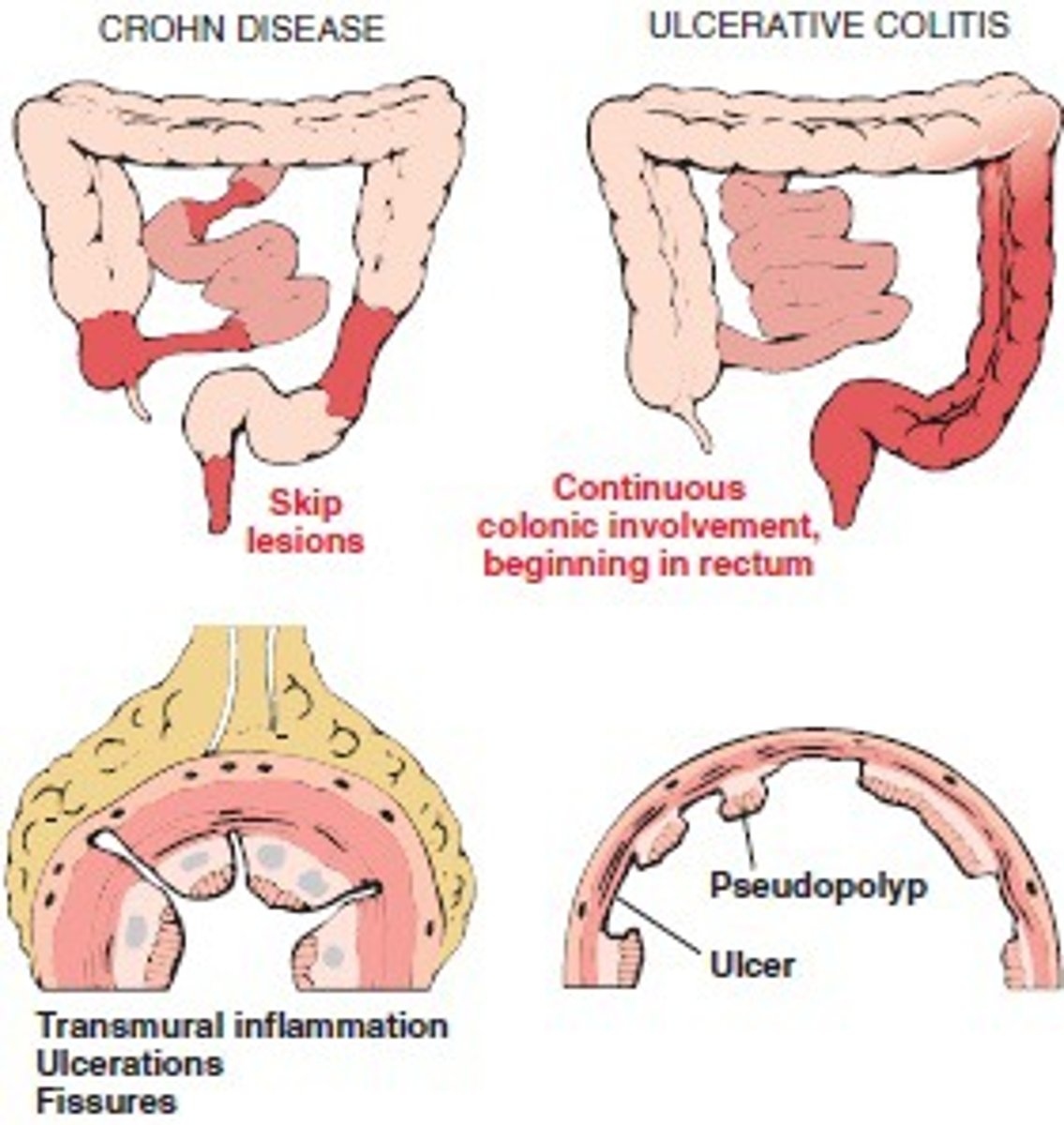
ulcerative colitis
(UC)
mucosal inflammatory condition
confined to rectum and colon
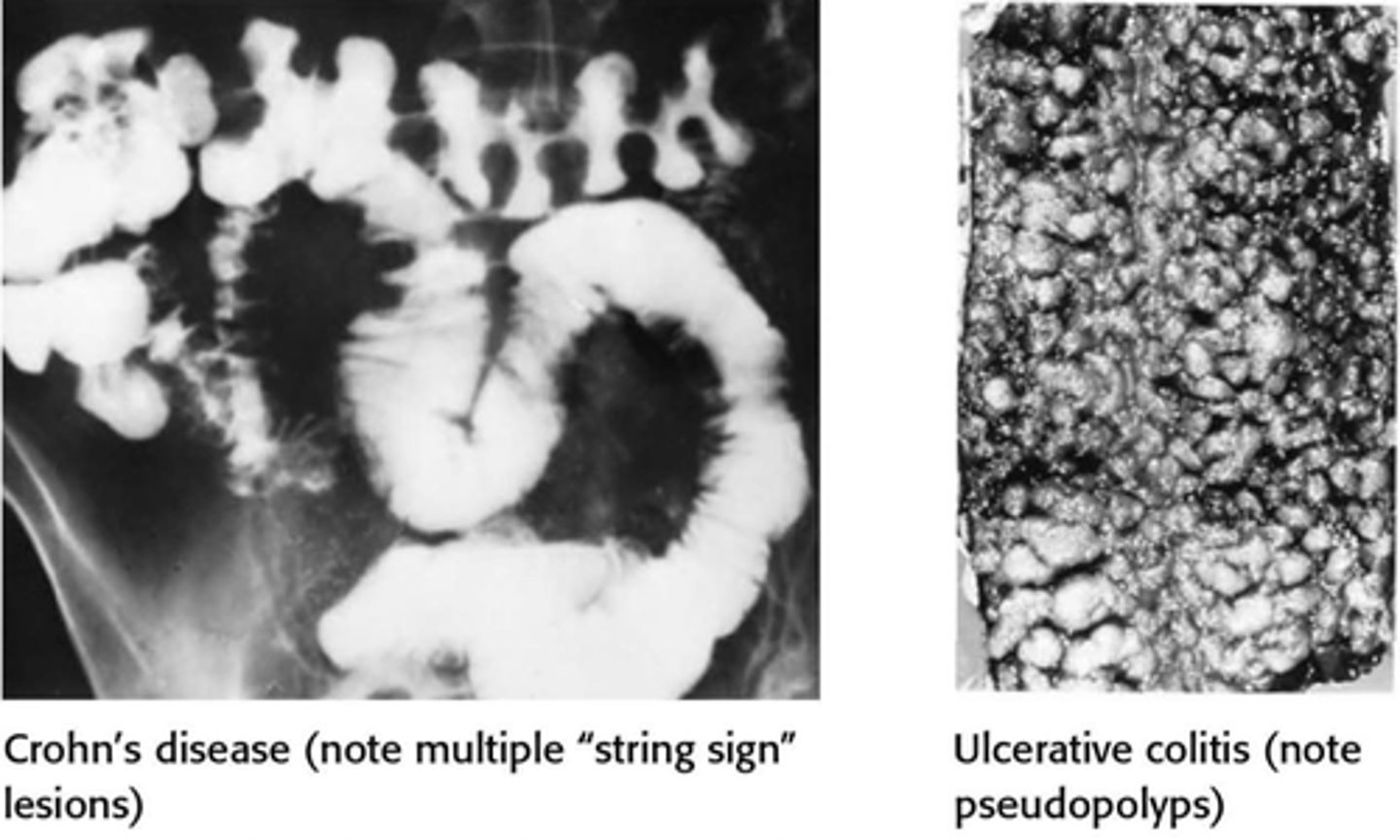
crohn's disease
(CD)
transmural inflammatory condition
can affect any part of the GI tract
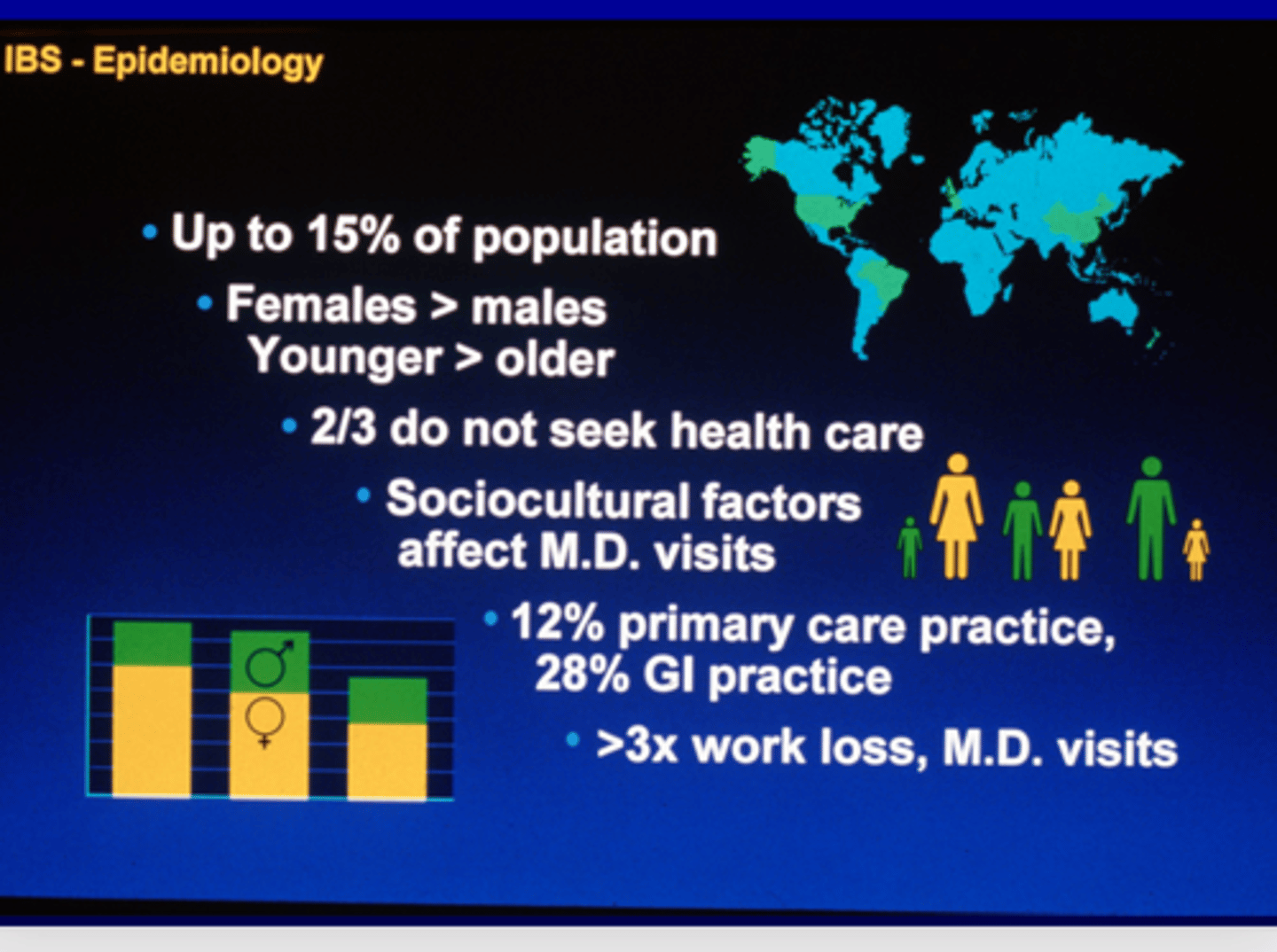
IBD epidemiology
- most common in USA and Northern Europe
- peak in 2nd - 3rd decade of life
- UC: more frequently in males
- CD: more frequently in women
- higher incidence in Jewish population
- more likely to develop if a relative has IBS
4 theories of IBD cause
1. immunologic
2. infectious: microbial dysbiosis; early exposure to antibiotics
3. genetics: 200+ genes associated with IBS
4. environmental:
- diet: ↓ dietary fiber, red meat, trans-unsaturated far, artificial sweeteners
- breastmilk: ↑ breastmilk ↓ UC development
- hygiene hypothesis: early exposure stimulates diversity and maturation of gut microbiome
- smoking: ↑ smoking ↓ UC development ↑ CD development
- NSAIDs: ↑ NSAIDs ↑ IBD onset (15+ days/month)
UC pathophysiology
- confined to rectum and colon: proctitis and left sided colitis are most common
- affects mucosal and submucosal layers
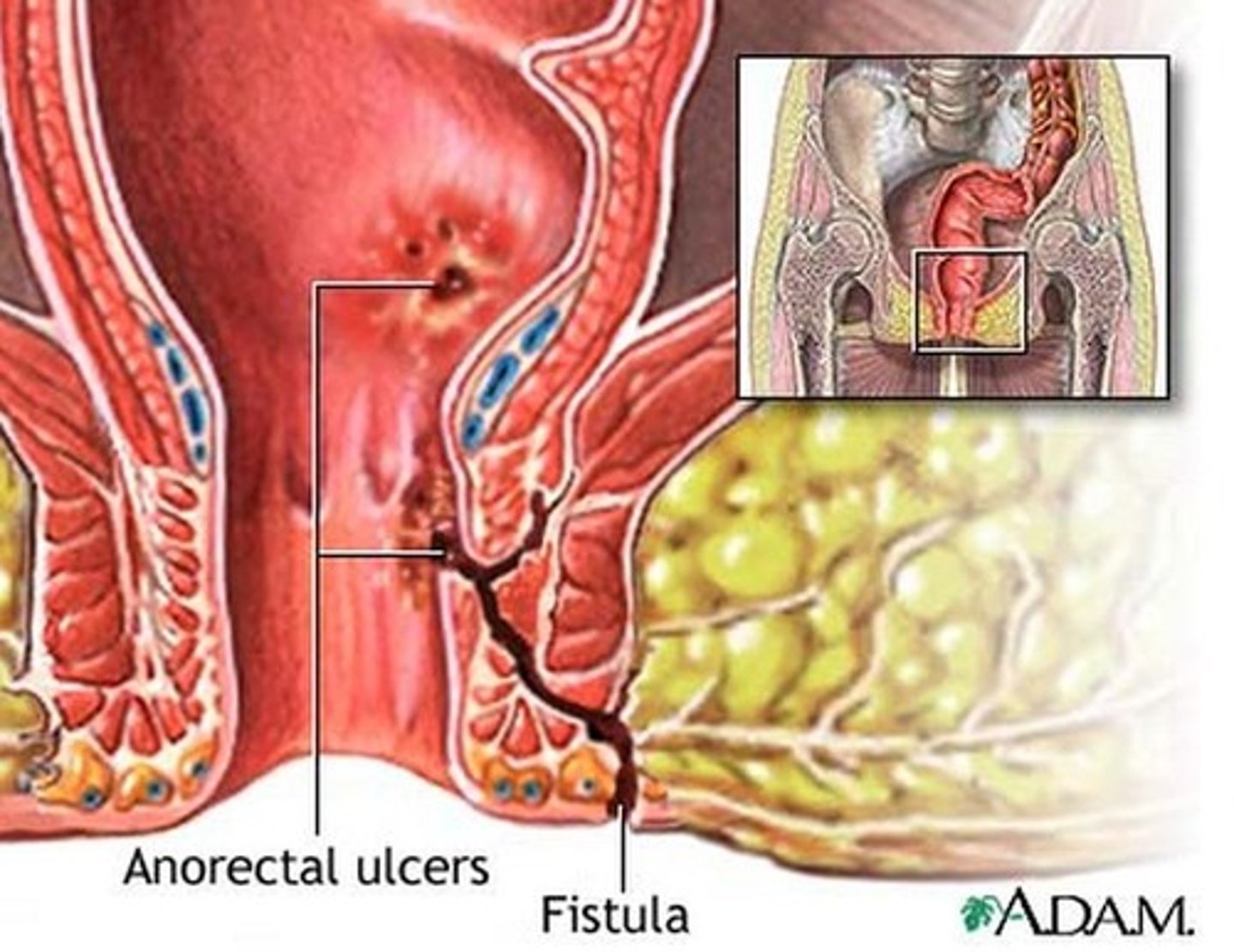
- fistula, perforation, or obstruction are uncommon
UC complications
local:
- hemorrhoids
- anal fissures
- perirectal abscess
- toxic megacolon
- colorectal carcinoma
- extra-intestinal manifestations
UC clinical features
common features:
- rectal bleeding
may be present:
- abdominal tenderness
rare/ uncommon:
- malaise/ fever
- abdominal pain
UC clinical presentation
1. distal disease: inflammation limited to areas distal to splenic flexure; "left sided disease"
2. extensive disease: inflammation extending proximal to the splenic flexure; majority of colon
3. proctitis: inflammation confined to the rectum
4. proctosigmoiditis: inflammation of the rectum and sigmoid colon
- onset: gradual (weeks to months)
- disease characterized by relapsing and remitting flares of mucosal inflammation
CD pathophysiology
- occurs anywhere in GI tract: mouth to anus
- terminal ileum most common
- transmural inflammatory process with deep ulcers
- fistula, perforation, or obstruction are more common
CD complications
fistulas (perianal, enterocutaneous, enteroenteric, enterovesicular, enterovaginal)
- lower risk of carcinoma than UC
- nutritional deficiencies
- extra-intestinal manifestations
CD clinical features
common:
- malaise/ fever
- rectal bleeding
- abdominal tenderness
- abdominal pain
- fistulas
- aphthous ulcers
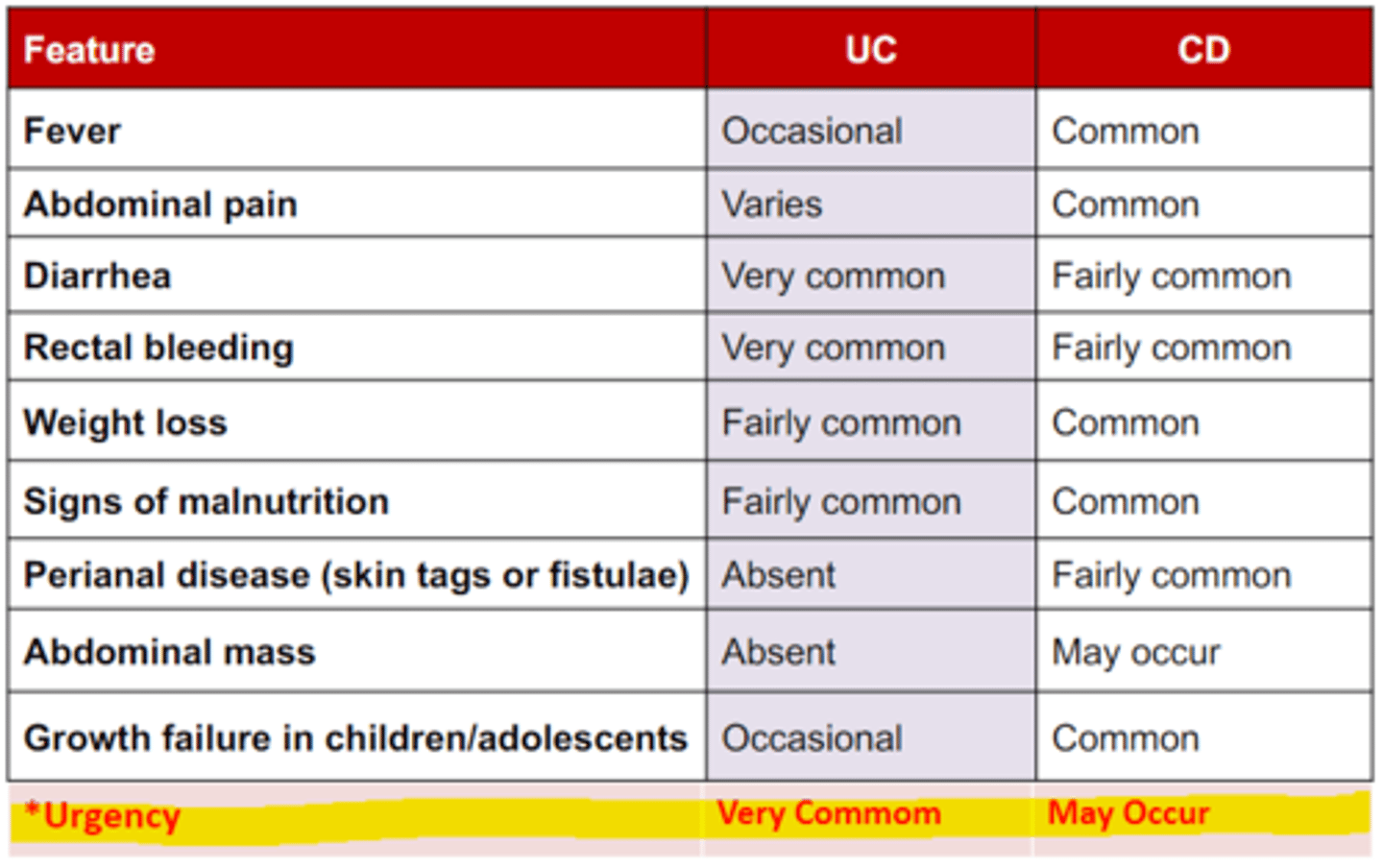
CD clinical presentation
S&S:
- malaise and fever
- abdominal pain
- frequent bowel movements
- hematochezia
- fistula
- weight loss and malnutrition
- arthritis
- bone fractures
- thromboembolism
physical exam & labs:
- abdominal mass and tenderness
- perianal fissure or fistula
- increased WBC, ESR, CRP, and fecal calprotectin
extraintestinal manifestations
symptoms affecting organs outside the intestines
- hepatobiliary
- joint arthralgias
- ocular
- dermatologic
- mucotaneous
- hematologic
- coagulation
- pulmonary
- metabolic
UC disease classification
Truelove and Witts: number of stools per day, blood in the stools, temperature, pulse, hemoglobin, and ESR
Mayo Score: from 0-12 , remission - severe disease
CD disease classification
no gold standard
Crohn's Disease Activity Index (CDAI): gauge response to therapy and determine remission
Harvey-Bradshaw Index (HBI): simpler than CDAI, but 93% with CDAI
- <150 to >450
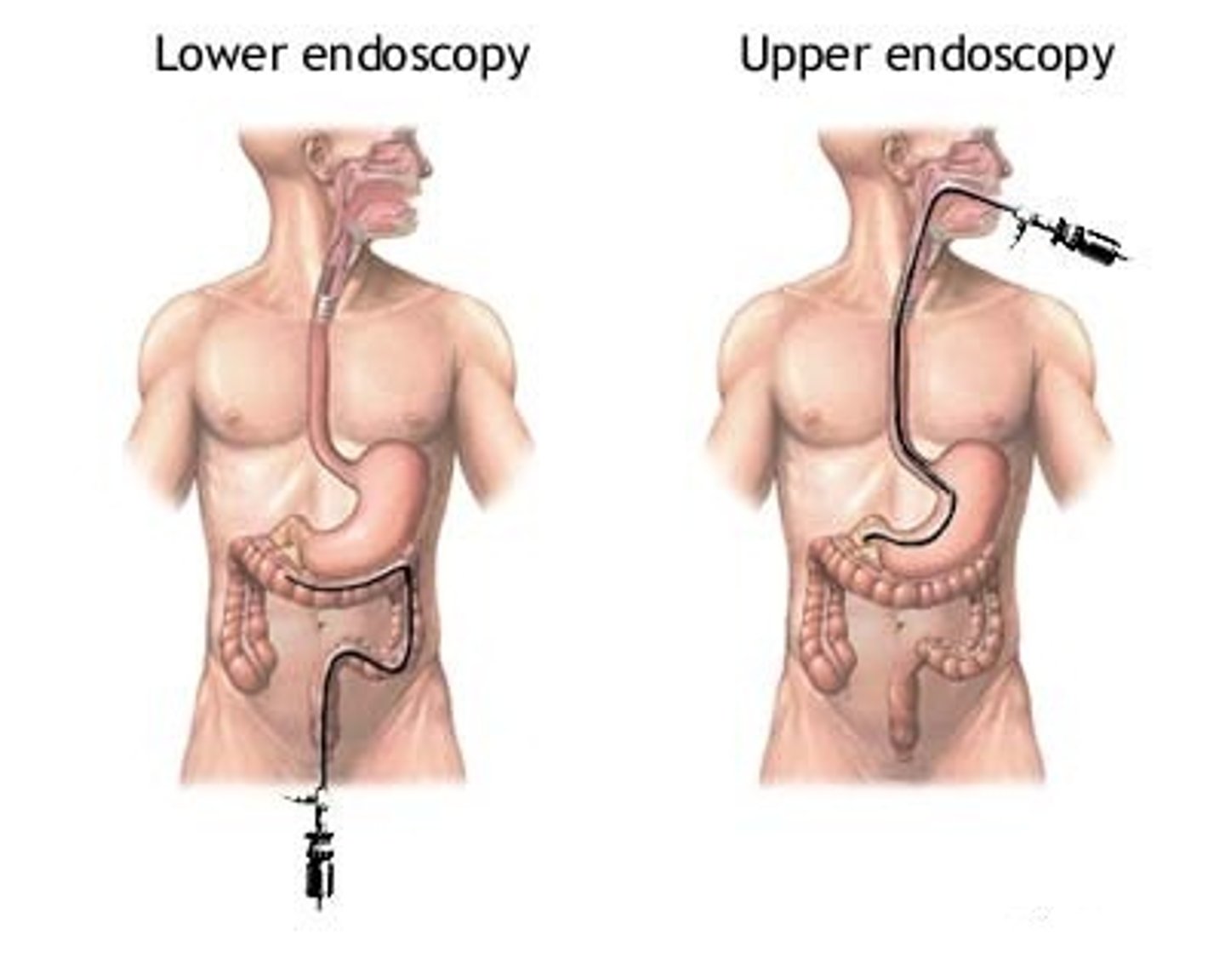
endoscopy
- ileocolonscopy with at least 2 biopsies should be performed in the assessment of patients with IBD
- disease distribution and severity should be documented
- upper endoscopy should only be performed in pts with upper GI signs and symptoms
- video capsule endoscopy may be useful in diagnosis of patients with small bowel CD
imaging studies
radiograph: for pts with concern for toxic megacolon, warranted to assess for colonic dilation
small bowel imaging: performed as initial diagnostic workup for pts with suspected CD
abdominal CT scan: often imaging of choice; thickening is seen in advanced disease
magnetic resonance enterography (MRE): useful in diagnosing chronic IBD; expensive and time consuming
transabdominal ultrasound: most sensitive in the ileum and sigmoid/ descending colon
- new, noninvasive, cheaper, well tolerated; operator dependent, may fail to detect superficial mucosal disease
routine laboratory investigation
complete blood count: anemia, elevated platelets
serum C-reactive protein (CRP): acute-phase reactant produced by the liver; short half life
erythrocyte sedimentation rate (ESR): non-specific measure of inflammation
stool studies for fecal pathogens: C. diff, viruses, parasites
fecal calprotectin and fecal lactoferrin
dehydration: electrolytes
malnutrition
monitoring disease activity
fecal markers: fecal calprotectin (>160 - predicts relapse)
serum CRP: monitor response in pts on infliximab
CTE and MRE: useful for pts with small bowel disease
mucosal healing: determined by endoscopy
- absence of ulceration, sustained remission, decreased surgery and hospitalization
serologic markers of IBD
routine use of serologic markers for the diagnosis or prognosis of IBD is not indicated
perinuclear antineutrophil cytoplasmic antibody (pANCA)
- positivity in up to 70% of pts with UC
- no relationship between pANCA and disease site/ activity/ treatment/ surgery
genetic testing
not indicated to establish diagnosis of IBD